Abstract
Objectives
The purpose of this study was to examine use and describe outcomes of radial access for percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI).
Background
Transradial PCI (TRI) is associated with reduced risk of bleeding and vascular complications, as compared with femoral access PCI (FPCI). Studies have suggested that TRI may reduce mortality among patients with STEMI.
Methods
We examined 294,769 patients undergoing PCI for STEMI at 1,204 hospitals in the CathPCI Registry between 2007 and 2011. Patients were grouped according to access site used for PCI. The temporal trend in the rate of radial versus femoral approach was determined. For minimization of confounding, an inverse probability weighting analysis incorporating propensity scores was used to compare procedural success, post-PCI bleeding, door-to-balloon times, and in-hospital mortality between radial and femoral access.
Results
Over the 5-year period, the use of TRI versus FPCI in STEMI increased from 0.9% to 6.4% (p < 0.0001). There was no difference in procedural success. TRI was associated with longer median door-to-balloon time (78 vs. 74 min; p < 0.0001) but lower adjusted risk of bleeding (odds ratio [OR]: 0.62; 95% CI: 0.53 to 0.72; p < 0.0001) and lower adjusted risk of in-hospital mortality (OR: 0.76; 95% CI: 0.57 to 0.99; p = 0.0455).
Conclusions
In this large national database, use of radial access for PCI in STEMI increased over the study period. Despite longer door-to-balloon times, the radial approach was associated with lower bleeding rate and reduced in-hospital mortality. These data provide support to execute an adequately powered randomized controlled trial comparing radial and femoral approaches for PCI in STEMI.
Keywords: bleeding, mortality, PCI, radial access, STEMI
Treatment of acute ST-segment elevation myocardial infarction (STEMI) has improved substantially, and the mortality rates from this condition have continued to decline (1). Despite these positive trends, bleeding rates remain high, particularly in the setting of primary or rescue percutaneous coronary intervention (PCI) (2,3). In this context, strategies that reduce bleeding risk appear to be associated with a lower rate of net adverse clinical events (4). Studies have indicated that a large proportion of bleeding among patients with STEMI undergoing primary PCI was related to the vascular access site (5). Outside of the setting of acute STEMI, transradial PCI (TRI) has been shown in many studies to reduce post-procedural bleeding and major vascular complications (6–8). Because there is a learning curve and subsequently increased procedure duration associated with TRI (9), the radial approach for primary PCI may worsen outcomes due to the clinical importance of rapid reperfusion. On the other hand, the lower rate of adverse outcomes associated with TRI has the potential to improve outcomes in high-risk patients such as those with STEMI. Studies that have examined these issues have reported conflicting results. Small single-center studies have shown that door-to-balloon times with a radial approach are similar to those with the femoral approach. A larger meta-analysis of randomized and observational studies showed that TRI was associated with longer procedural times (10,11). Similarly, studies have conflicted in reporting bleeding and mortality outcomes associated with vascular access sites (radial vs. femoral). Some studies have shown lower rates, whereas 2 randomized trials have different conclusions. In the STEMI subgroup of the RIVAL (Radial vs Femoral Access for Coronary Intervention Trial) study, there was no difference in major bleeding between the radial and femoral groups, but there was an association between TRI and reduced 30-day mortality (12). In contrast, 2 meta-analyses have shown a reduction in bleeding and mortality with transradial primary PCI (11,13).
The National Cardiovascular Data Registry (NCDR) is the largest ongoing contemporary database of PCI procedures, which provides an ideal opportunity to explore the prevalence and in-hospital outcomes of TRI in STEMI. Accordingly, we examined the temporal trends of TRI in STEMI, compared patient and hospital characteristics by access site, and evaluated the association between TRI for STEMI and in-hospital outcomes.
Methods
Data source and study sample
The NCDR CathPCI Registry is an initiative of the American College of Cardiology (ACC) Foundation and the Society for Cardiovascular Angiography and Interventions. Descriptions of the NCDR and CathPCI Registry have been previously published (14–15). Demographic, clinical, procedural, and institutional data elements from diagnostic catheterization and PCI procedures were collected at more than 1,315 participating centers. Data were entered via either a secure Web-based platform or software provided by ACC-certified vendors. Data quality assurance included automatic system validation and reporting of data completeness, random on-site auditing of participating centers, and education and training for site data managers (16). All data elements and definitions were prospectively defined by a committee of the ACC. A comprehensive description of NCDR data elements and definitions is available at http://www.ncdr.com/webncdr/cathpci/home/datacollection.
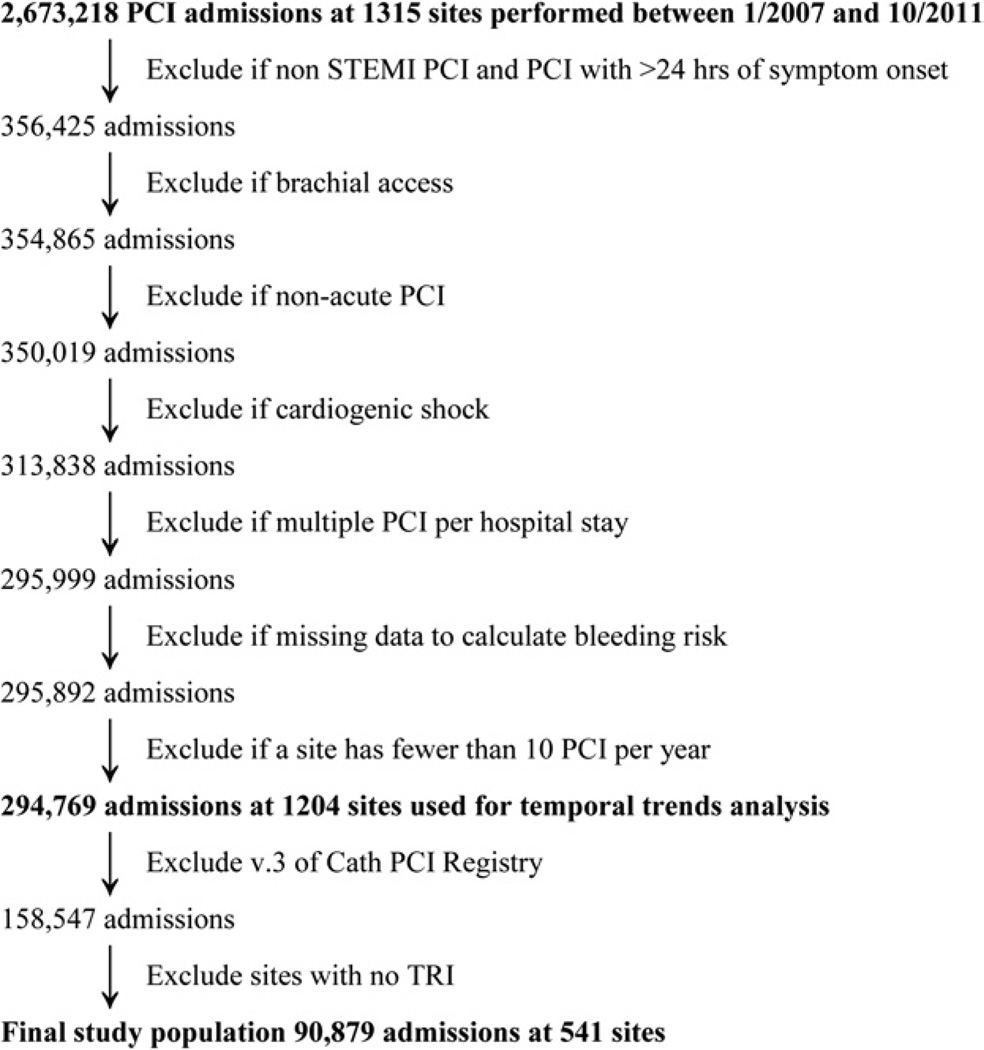
The study population consisted of patients with STEMI treated with immediate primary PCI or rescue PCI from January 1, 2007, to September 30, 2011. Patients were excluded if they had cardiogenic shock, more than 1 PCI during hospitalization, PCI through access of a nonfemoral and nonradial artery (i.e., ulnar, brachial), or unknown data on bleeding events. After these exclusions (Fig. 1), 294,769 patients from 1,204 sites were included in the analysis of prevalence and temporal trends of TRI for STEMI. For comparison of patient and hospital characteristics by approach (radial vs. femoral) and determination of the association between TRI for STEMI and in-hospital outcomes, further exclusions were made. Patients with sufficient data to calculate in-hospital mortality and bleeding risk according to CathPCI Registry version 4 models, from sites with at least 1 radial PCI for STEMI, were included for analysis, resulting in a final study population of 90,879 patients from 541 sites.
Figure 1. The CONSORT Diagram.
Patient population from CathPCI Registry selected for the study, displayed as a CONSORT diagram. The population was initially selected to allow analysis of prevalence and temporal trends of transradial percutaneous coronary intervention (TRI) for ST-segment elevation myocardial infarction (STEMI). For comparison of patient and hospital characteristics by approach (radial vs. femoral) and determination of the association between TRI for STEMI and in-hospital outcomes, further exclusions were made. PCI = percutaneous coronary intervention.
Endpoints and definitions
The primary endpoint for this analysis was in-hospital mortality. Other endpoints were procedural success (defined as the number of lesions dilated divided by the number of lesions attempted) and bleeding. Bleeding was defined as the presence of 1 or more of the following within 72 h of PCI: overt access site bleeding, retroperitoneal hemorrhage, intracranial hemorrhage, gastrointestinal or genitourinary bleeding, cardiac tamponade, non–bypass surgery–related blood transfusion in patients with a pre-procedure hemoglobin ≤8 g/dl, or an absolute decrease in hemoglobin ≥3 g/dl from pre- to post-PCI in patients with a pre-procedure hemoglobin value <16 g/dl.
Ethical considerations
This study was approved by the Duke University Medical Center institutional review board and was determined to meet the definition of research not requiring informed consent.
Statistical analysis
For determination of the temporal trends in the use of TRI for STEMI over the study period from 2007 to 2011, the quarterly proportion of TRI cases out of all PCI cases for STEMI (radial plus femoral) was calculated.
Patient and hospital characteristics were compared by approach (radial vs. femoral and overall). Patient characteristics, including demographics, history and risk factors, coronary anatomy, PCI procedure, lesions and devices, laboratory values, intraprocedure and post-procedure events, discharge, and hospital characteristics, were compared. Categorical variables are presented as frequencies (percentages), and differences between the 2 groups were assessed using the chi-square test when the sample size was sufficient, otherwise using an exact test. Continuous variables are presented as median (Q1, Q3) and were compared using the Wilcoxon rank-sum test.
For the development of a propensity score model for TRI versus femoral PCI, a logistic regression model was fit-adjusted for patient characteristics before catheterization. Variables were selected a priori from the CathPCI Registry version 4 in-hospital mortality and bleeding models to include variables that were related to the outcomes (17). Specifically, sex, age, body mass index, cerebrovascular disease, peripheral vascular disease, chronic lung disease, prior PCI, diabetes, ejection fraction, renal failure (glomerular filtration rate <30 or dialysis), glomerular filtration rate, cardiogenic shock, PCI status (emergency/salvage vs. urgent), New York Heart Association heart failure class, cardiac arrest, and pre-procedure hemoglobin (as a continuous linear spline with 1 knot at 13) were included in the propensity score model. The overlap of the distributions of propensity scores by radial and femoral patients was assessed by looking at histograms of propensity scores and descriptive statistics. Pre- and post-inverse probability of treatment weighting (IPTW) balance of the covariates between radial and femoral patients was checked (18,19).
For determination of the association between TRI and in-hospital outcomes, logistic regression with generalized estimating equations was used to account for within-hospital clustering. Propensity score was developed and used to adjust for confounding by the IPTW method. For maximization of efficiency, weights were stabilized by using the marginal probability of TRI (20,21). For radial patients, weights were calculated by dividing the marginal probability of radial by the individual patient’s propensity score, and weights for femoral patients were calculated by dividing (1 minus the marginal probability of radial) by (1 minus the individual patient’s propensity score). A limitation of this method is that one cannot adjust for unmeasured confounding. Along with the adjusted odds ratio (OR), the number needed to treat (NNT) is presented with 95% CIs, estimated from 200 bootstrap samples.
Propensity score model
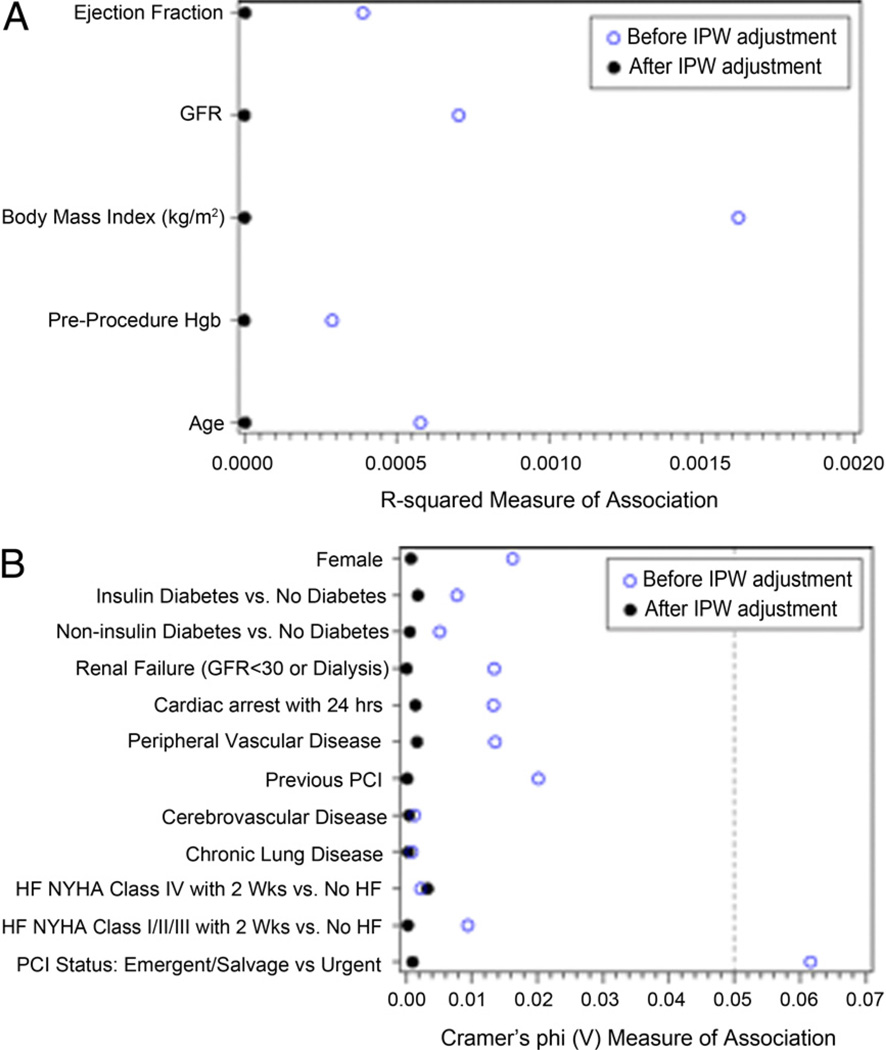
The adequacy of the propensity score model was assessed by checking the distribution of propensity scores by treatment for reasonable overlap and the pre- and post-IPTW balance of the covariates. Percentiles of propensity scores were similar between femoral (first = 0.033, 50th = 0.063, 99th = 0.151) and radial patients (first = 0.037, 50th = 0.067, 99th = 0.173). Pre- and post-IPTW balance of the covariates between treatment groups was assessed using Cramer’s phi for categorical variables and R2 for continuous variables. Values closer to zero indicated better balance. After IPTW adjustment, the r2 measure for each continuous variable was <0.0001, and it was <0.004 for each categorical variable, which indicates reasonable balance (Fig. 2).
Figure 2. Balance of Continuous and Categorical Variables After Adjustment.
Pre- and post-inverse probability of treatment weighting (IPW) balance of the covariates between radial and femoral patients was checked. IPW improved the balance for all variables. Continuous variables were reasonably balanced even before IPW (all R2 < 0.004). (A) Continuous variables. (B) Categorical variables. GFR = glomerular filtration rate; HF = heart failure; Hgb = hemoglobin; NYHA = New York Heart Association; other abbreviation as in Figure 1.
Results
Population characteristics and treatment
Among 90,879 patients undergoing immediate primary or rescue PCI for STEMI, 6,159 patients (6.8%) received TRI, whereas 84,720 patients (93.2%) received facilitated PCI (FPCI). Baseline demographic and clinical history characteristics (Table 1) were different between the TRI and FPCI groups. Those undergoing TRI were younger and heavier and were more likely to be male, be white, have peripheral vascular disease, and have recent heart failure; they were less likely to have prior MI, PCI, and coronary artery bypass graft, or be on hemodialysis.
Table 1.
Demographic and Clinical Characteristics of the Study Population (N = 90,879)
| Variable | Radial (N = 6,159) |
Femoral (N = 84,720) |
p Value |
|---|---|---|---|
| Mean age, yrs | 59.37 ± 12.51 | 60.61 ± 12.95 | <0.0001 |
| Male | 75.27 | 72.38 | <0.0001 |
| White | 89.24 | 88.09 | 0.0074 |
| Body mass index, kg/m2 | 30.11 ± 6.88 | 29.12 ± 6.04 | <0.0001 |
| Previous MI | 16.97 | 19.70 | <0.0001 |
| Diabetes | 22.83 | 22.81 | 0.9833 |
| Cerebrovascular disease | 6.90 | 6.77 | 0.6848 |
| Peripheral vascular disease | 6.95 | 5.69 | <0.0001 |
| Chronic lung disease | 9.34 | 9.44 | 0.7761 |
| Hypertension | 64.56 | 65.62 | 0.0914 |
| Current/recent smoker | 45.30 | 43.93 | 0.0379 |
| Dyslipidemia | 61.81 | 63.45 | 0.0096 |
| Family history of CAD | 25.05 | 20.73 | <0.0001 |
| Previous PCI | 17.92 | 21.19 | <0.0001 |
| Previous CABG | 1.93 | 5.87 | <0.0001 |
| Currently on dialysis | 0.54 | 0.89 | 0.0035 |
| Heart failure within 2 weeks | 6.59 | 5.97 | 0.0491 |
Values are mean ± SD or %. p Values are based on Pearson chi-square tests for all categorical variables and on chi-square rank-based group means score statistics for all continuous/ordinal variables. p < 0.05 indicates that the summary measures (i.e., medians for continuous variables and proportions for categorical variables) differ significantly between the radial and femoral access groups.
CABG = coronary artery bypass graft; CAD = coronary artery disease; MI = myocardial infarction; PCI = percutaneous coronary intervention.
Procedural characteristics were different between the TRI and FPCI groups (Table 2). Fluoroscopy time was longer with TRI, but the volume of contrast used was less compared with FPCI. Intra-aortic balloon pump insertion was more frequent in patients receiving FPCI; however, there was no difference in the use of PCI without stenting between the groups. There was no difference in the use of drug-eluting stents. Both bivalirudin and glycoprotein IIb/IIIa inhibitors were used more frequently in the FPCI group. There was no difference in the frequency of bifurcation lesion treatment, lesion length, or location between the groups. ACC/American Heart Association high/C lesion risk was encountered less frequently in patients with TRI (63.99% vs. 66.08%; p = 0.0007), but there was no difference in the procedural success rate. Median door-to-device time was 4 min shorter in FPCI compared with TRI (74 vs. 78 min; p < 0.0001).
Table 2.
Procedural Characteristics in Patients With STEMI Treated With Radial and Femoral Access PCI
| Variable | Radial (N = 6,159) |
Femoral (N = 84,720) |
p Value |
|---|---|---|---|
| Fluoroscopy time, min | 12.80 | 10.40 | <0.0001 |
| Contrast volume, ml | 180.00 | 185.00 | <0.0001 |
| Left heart catheterization | 85.87 | 85.17 | 0.5367 |
| IABP | 1.69 | 5.21 | <0.0001 |
| Drug-eluting stent | 51.97 | 52.46 | 0.0699 |
| No stent used | 9.09 | 9.80 | 0.0699 |
| Bivalirudin | 30.00 | 34.65 | <0.0001 |
| Low-molecular-weight heparin | 7.85 | 5.83 | <0.0001 |
| Glycoprotein IIb/IIIa (any) | 58.14 | 61.09 | <0.0001 |
| High/C lesion risk | 63.99 | 66.08 | 0.0007 |
| Bifurcation lesion | 12.71 | 12.37 | 0.4254 |
| Single lesion treated | 80.55 | 78.90 | 0.0542 |
| Lesion successfully dilated | 94.82 | 94.04 | 0.0254 |
| Door-to-device time, min | 78.00 | 74.00 | <0.0001 |
Values are %.
IABP = intra-aortic balloon pump; STEMI = ST-elevation myocardial infarction; other abbreviation as in Table 1
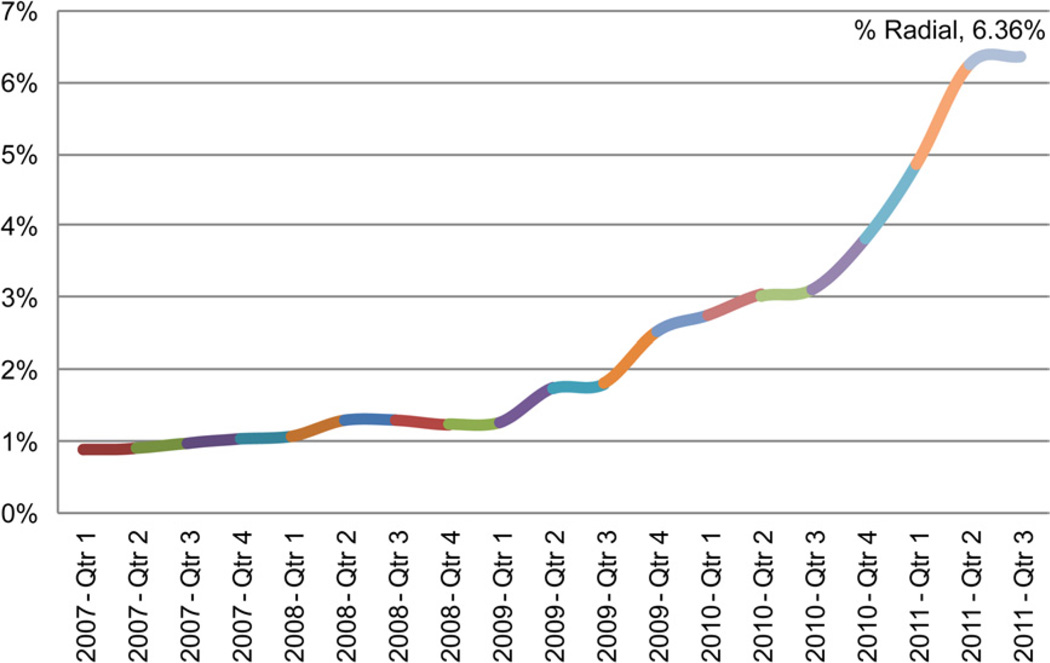
Temporal trends in the use of TRI
Use of TRI in STEMI increased over the study period, from 0.9% of patients receiving TRI in the first quarter of 2007 to 6.4% of patients receiving TRI in the third quarter of 2011 (p < 0.0001) (Fig. 3).
Figure 3. Temporal Trend in Use of TRI for STEMI PCI from 2007 to 2011.
Time line in quarters is presented on the x-axis, and use of radial access (%) is presented on the y-axis. Abbreviations as in Figure 1.
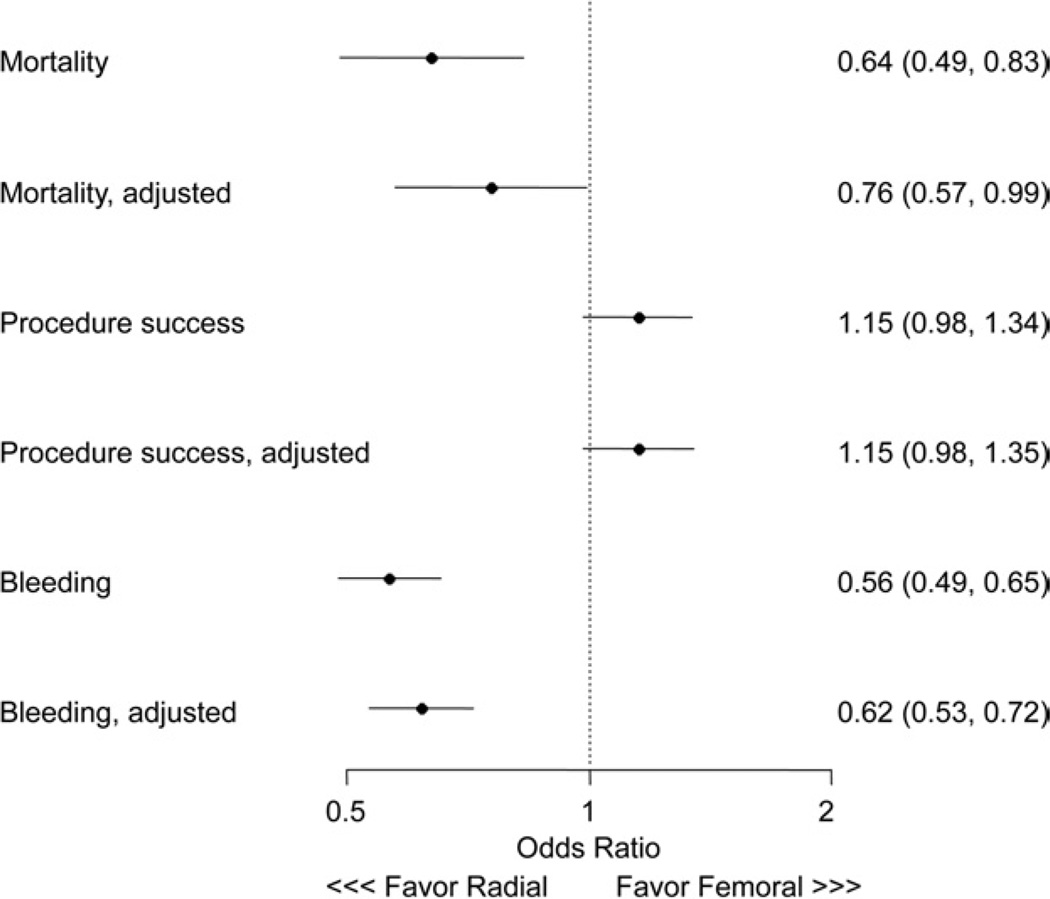
Association between TRI for STEMI and in-hospital outcomes
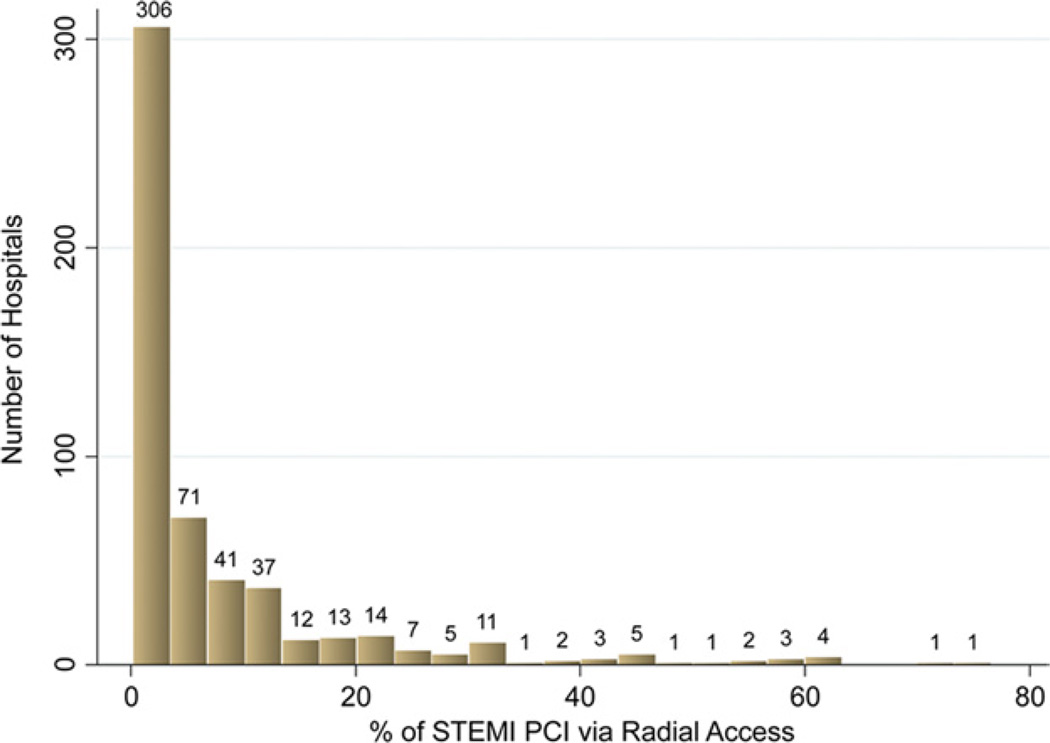
Vascular complications requiring procedural care were less common in TRI patients compared with FPCI patients (0.13% vs. 0.49%; p < 0.001). TRI was associated with in-hospital outcomes (Fig. 4). There was no difference in procedural success. Unadjusted rates of bleeding and in-hospital mortality were lower with TRI. After IPTW multivariable adjustment, TRI was associated with lower risk of bleeding (OR: 0.62; 95% CI: 0.53 to 0.72) and lower risk of in-hospital mortality (OR: 0.76; 95% CI: 0.57 to 0.99). NCDR version 4–defined bleeding was lower in the TRI group, as compared with the FPCI group: 6.88% versus 11.59% (p < 0.0001). NNT to prevent 1 bleeding event with TRI was 25; NNT to prevent 1 death with TRI was 207. The proportion of TRI use in patients with STEMI among the hospital sites varied from 0.2% to 76.6% (median 2.7%) (Fig. 5).
Figure 4. In-Hospital Outcomes of TRI in STEMI.
Association between radial versus femoral access PCI and in-hospital outcomes, displayed as the relative risk between groups (solid diamonds) with 95% CIs (horizontal lines). Abbreviations as in Figure 1.
Figure 5. Frequency of TRI Use.
Distribution of frequency in radial access use during STEMI PCI by 541 hospital sites contributing to the National Cardiovascular Data Registry. The percent of radial access is on the x-axis, and the number of hospitals is on the y-axis. Abbreviations as in Figure 1.
Discussion
Using data from a broadly representative contemporary PCI registry, we reported several important observations. First, although the rate of adoption of radial access for emergent PCI in the United States is low, there is a trend of its increased use from 0.9% to 6.4% in the course of 5 years. Second, we found that radial access was associated with slightly longer door-to-device time compared with femoral access. Third, despite this longer time, there was an association between TRI and reduced in-hospital mortality in patients with STEMI undergoing PCI. Fourth, there was also a significant association with reduced bleeding in the TRI group.
Primary reperfusion with PCI is a well-established standard of care in patients with STEMI (1). Although catheter-based therapy offers better outcomes compared with thrombolytic therapy (22), bleeding and other arteriotomy site complications are potential limiting factors. Indeed, studies have indicated that the rate of bleeding was higher among patients undergoing primary PCI for STEMI compared with those undergoing PCI for other indications (4,23). A large proportion of these bleeding events were related to the vascular access site (5). In this high-risk population, strategies that reduce bleeding, such as use of bivalirudin, were associated with reduced mortality (4). Because radial access substantially reduces access site bleeding compared with femoral access, its use during primary and rescue PCI is of great interest.
Prior trials have examined the association between TRI and outcomes among patients with STEMI (11,24). In aggregate, these studies have shown a reduction in mortality, but not bleeding, with either slightly reduced door-to-balloon times (13) or longer procedure times. Based on these studies, the explanation for the mortality reduction with transradial primary PCI remains elusive. On the other hand, observational studies have consistently shown an association between TRI and both reduced bleeding and mortality. An observational study by Chase et al. (25) showed that the reduction in 1-year mortality among patients undergoing TRI was largely explained by a reduction in the need for post-procedure transfusion after transradial procedures. Recently, the RIFLE STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) randomized trial confirmed these findings by showing a reduction in 30-day mortality with transradial primary PCI of similar magnitude to the reduction in Bleeding Academic Research Consortium type ≥2 bleeding. Our study corroborated these studies and extends them by examining a large contemporary multicenter registry of PCI. Importantly, our study was able to account for current antithrombotic strategies such as bivalirudin.
Overall, there was no difference in procedural success between the FPCI and TRI cases, but TRI was associated with slightly longer door-to-device time. Shorter door-to-balloon times have been linked to improved survival (26). In this context, ambulance and hospital systems participating in acute infarct angioplasty function under significant time pressure, with publicly reported quality metrics. Any strategy that delays acute reperfusion requires careful consideration. Concerns about the difficulty with radial access, navigation of the tortuous arm vasculature to engage the coronary arteries, and inability to use larger thrombectomy catheters may be potential reasons why radial access is as rare in clinical practice as documented by our study. The association between TRI and reduced mortality despite longer door-to-device time may be reflective of competing risks—the risk associated with major bleeding after STEMI PCI may be greater than that conferred by a 4-min increase in reperfusion time. Other factors, such as immediate ability to ambulate and reduce stress afforded by TRI, may play a role, but they were not examined.
Study limitations
Some limitations of our study should be considered. As with any other observational study, associations between treatments and outcomes cannot prove causality. A limitation of the adjustment methodology is that there is always a chance of unmeasured confounding. There might be residual factors that are not known or not captured by the registry that may bias the results in favor of the femoral or radial access. However, operators and hospital systems in the United States are much more familiar with femoral access (as reflected by the longer fluoroscopy times in the TRI group), and any advantage of the radial access shown by providers early in the learning curve would likely become more evident with more experience in radial procedures. Finally, bleeding events can be underreported. Although an auditing program was used to verify data accuracy in the registry, outcomes were not adjudicated; thus, there may be underreporting of complications other than mortality. It is likely that the associations between radial access and reduced bleeding would be greater with higher reported bleeding rates.
Conclusions
There was a trend of increased use of radial access for STEMI PCI from 0.9% to 6.4% in the course of 5 years, between 2007 and 2011. Compared with femoral access, use of radial access for STEMI PCI was associated with slightly longer door-to-device time and fluoroscopy times but reduced bleeding and in-hospital mortality. These data suggest that wider adoption of TRI for STEMI may significantly improve outcomes; however, these results should be confirmed in an adequately powered prospective randomized trial.
Abbreviations and Acronyms
- FPCI
facilitated percutaneous coronary intervention
- PCI
percutaneous coronary intervention
- STEMI
ST-segment elevation myocardial infarction
- TRI
transradial percutaneous coronary intervention
Footnotes
All authors have reported that they have no relationships relevant to the contents of this paper to disclose.
REFERENCES
- 1.Roe MT, Messenger JC, Weintraub WS, et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010;56:254–263. doi: 10.1016/j.jacc.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Suh JW, Mehran R, Claessen BE, et al. Impact of in-hospital major bleeding on late clinical outcomes after primary percutaneous coronary intervention in acute myocardial infarction the HORIZONS-AMI (Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction) trial. J Am Coll Cardiol. 2011;58:1750–1756. doi: 10.1016/j.jacc.2011.07.021. [DOI] [PubMed] [Google Scholar]
- 3.Gershlick AH, Stephens-Lloyd A, Hughes S, et al. Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction. N Engl J Med. 2005;353:2758–2768. doi: 10.1056/NEJMoa050849. [DOI] [PubMed] [Google Scholar]
- 4.Stone GW, Witzenbichler B, Guagliumi G, et al. Bivalirudin during primary PCI in acute myocardial infarction. N Engl J Med. 2008;358:2218–2230. doi: 10.1056/NEJMoa0708191. [DOI] [PubMed] [Google Scholar]
- 5.Rao SV, Cohen MG, Kandzari DE, Bertrand OF, Gilchrist IC. The transradial approach to percutaneous coronary intervention: historical perspective, current concepts, and future directions. J Am Coll Cardiol. 2010;55:2187–2195. doi: 10.1016/j.jacc.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 6.Sciahbasi A, Pristipino C, Ambrosio G, et al. Arterial access-site-related outcomes of patients undergoing invasive coronary procedures for acute coronary syndromes (from the Comparison of Early Invasive and Conservative Treatment in Patients With Non-ST-Elevation Acute Coronary Syndromes [PRESTO-ACS] vascular substudy) Am J Cardiol. 2009;103:796–800. doi: 10.1016/j.amjcard.2008.11.049. [DOI] [PubMed] [Google Scholar]
- 7.Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–140. doi: 10.1016/j.ahj.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Rao SV, Ou FS, Wang TY, et al. Trends in the prevalence and outcomes of radial and femoral approaches to percutaneous coronary intervention: a report from the National Cardiovascular Data Registry. J Am Coll Cardiol Intv. 2008;1:379–386. doi: 10.1016/j.jcin.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 9.Ball WT, Sharieff W, Jolly SS, et al. Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv. 2011;4:336–341. doi: 10.1161/CIRCINTERVENTIONS.110.960864. [DOI] [PubMed] [Google Scholar]
- 10.Pancholy S, Patel T, Sanghvi K, Thomas M, Patel T. Comparison of door-to-balloon times for primary PCI using transradial versus transfemoral approach. Catheter Cardiovasc Interv. 2010;75:991–995. doi: 10.1002/ccd.22425. [DOI] [PubMed] [Google Scholar]
- 11.Joyal D, Bertrand OF, Rinfret S, Shimony A, Eisenberg MJ. Meta-analysis of ten trials on the effectiveness of the radial versus the femoral approach in primary percutaneous coronary intervention. Am J Cardiol. 2012;109:813–818. doi: 10.1016/j.amjcard.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Jolly SS, Yusuf S, Cairns J, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377:1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 13.Vorobcsuk A, Kónyi A, Aradi D, et al. Transradial versus transfemoral percutaneous coronary intervention in acute myocardial infarction Systematic overview and meta-analysis. Am Heart J. 2009;158:814–821. doi: 10.1016/j.ahj.2009.08.022. [DOI] [PubMed] [Google Scholar]
- 14.Weintraub WS, McKay CR, Riner RN, et al. The American College of Cardiology National Database: progress and challenges. American College of Cardiology Database Committee. J Am Coll Cardiol. 1997;29:459–465. doi: 10.1016/s0735-1097(96)00545-1. [DOI] [PubMed] [Google Scholar]
- 15.Brindis RG, Fitzgerald S, Anderson HV, Shaw RE, Weintraub WS, Williams JF. The American College of Cardiology—National Cardiovascular Data Registry (ACC-NCDR): building a national clinical data repository. J Am Coll Cardiol. 2001;37:2240–2245. doi: 10.1016/s0735-1097(01)01372-9. [DOI] [PubMed] [Google Scholar]
- 16.CathPCI Registry Companion Guide to Your NCDR Data Quality Report. Washington, DC: American College of Cardiology Foundation; 2008. [Google Scholar]
- 17.Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163:1149–1156. doi: 10.1093/aje/kwj149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–1234. [Google Scholar]
- 20.Robins JM. Marginal structural models. 1997 Proc Am Stat Assoc. 1998;1998:1–10. [Google Scholar]
- 21.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–560. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 23.Lopes RD, Alexander KP, Manoukian SV, et al. Advanced age, antithrombotic strategy, and bleeding in non-ST-segment elevation acute coronary syndromes: results from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2009;53:1021–1030. doi: 10.1016/j.jacc.2008.12.021. [DOI] [PubMed] [Google Scholar]
- 24.Jang JS, Jin HY, Seo JS, et al. Transradial versus transfemoral approach for primary percutaneous coronary intervention in patients with acute myocardial infarction: a systematic review and meta-analysis. Euro-Intervention. 2012;8:501–510. doi: 10.4244/EIJV8I4A78. [DOI] [PubMed] [Google Scholar]
- 25.Chase AJ, Fretz EB, Warburton WP, et al. Association of the arterial access site at angioplasty with transfusion and mortality: the M.O.R.T.A.L study (Mortality Benefit of Reduced Transfusion After Percutaneous Coronary Intervention via the Arm or Leg) Heart. 2008;94:1019–1025. doi: 10.1136/hrt.2007.136390. [DOI] [PubMed] [Google Scholar]
- 26.Rathore SS, Curtis JP, Nallamothu BK, et al. Association of door-to-balloon time and mortality in patients ≥65 years with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2009;104:1198–1203. doi: 10.1016/j.amjcard.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]