Abstract
A minimally invasive anterior approach (MIS) was compared to a standard lateral approach in primary total hip arthroplasty. Clinical and radiological outcomes were analyzed 6 weeks, 12 weeks, one year and two years after surgery. The duration of surgery was longer, mobility one week after surgery was better and time of hospitalization was shorter for minimally invasive-treated patients. They had less pain during movement, limping, better Harris Hip Score and satisfaction after 6 weeks, which remained after 12 weeks and 1 year, but not after two years. There were two deep infections in the MIS group. Radiological results were not affected. The infections might be a point of concern, but there were no other disadvantages of the MIS approach. In fact, early rehabilitation was facilitated and clinical results were improved. Our results encourage the continuous use of the MIS anterior approach instead of the lateral approach.
Key words: hip replacement, minimal invasive, anterior approach, early rehabilitation
Introduction
The usefulness of minimally invasive hip replacement has been thoroughly discussed, but no widely accepted definition of minimally invasive surgery with respect to total hip arthroplasty (THA) has been suggested. Several recent studies have focused on minimally invasive approaches in primary THA.1,2 Many so-called minimally invasive methods with an anterior, anterolateral, lateral or posterior approach are proposed to reduce surgical trauma,3-5 facilitate rehabilitation,6,7 and improve postoperative muscle strength.4 While some authors describe tremendous advantages of minimally invasive approaches,8 others have seen little effect, or even negative effects, on early outcome with an increased number of complications.9,10 Implant positioning and orientation might be compromised by the use of minimal invasive techniques11,12 and there is no data on the long-term survival available. Results seem to depend on case-load and surgical experience.13 The overall care of patients might contribute more to rehabilitation than the type of incision.14,15
The lateral transgluteal approach was standard at our hospital for more than 20 years,16 the last years used in a muscle sparing technique.17 It was replaced by a minimally invasive anterior approach in March 2009 with the aim to facilitate early rehabilitation and improve functional results without changing the overall clinical routines. In this prospective, consecutive cohort study, we aimed to evaluate the effect of the surgical approach on hospital stay, complications and early clinical and radiological results.
Materials and Methods
The institutional review board at the study center approved the study and all patients provided written informed consent for the surgery and postoperative follow-up. Data collection was begun in January 2008 for all patients. Until March 2009 a muscle sparing standard lateral transgluteal approach (STD) was clinical routine,16,17 thereafter, a minimally invasive anterior approach (MIS) was used.18
Criteria of inclusion
Only patients with elective unilateral primary hip replacement without previous surgery were included. Totally 357 primary THA were performed during the study period. Nine patients (hips) with previous surgery via lateral approach were re-operated via lateral approach and were excluded. Furthermore, we excluded 16 patients with bilateral procedures (32 hips), 33 patients (hips) treated for proximal femoral fractures and eleven patients (hips) with general complications during the hospitalization: five patients had cardiac problems (four STD/one MIS), three gastrointestinal (all MIS), one urological (STD), one pulmonary (MIS) and one for psychological deterioration (STD). Six patients declined participation. There was one early death not related to surgery and one exclusion due to mental sickness. Two patients treated after March 2009 were operated using the lateral approach due to obesity (BMI 41.6 and 33.9) and seven patients specifically requested a lateral approach during the time that the MIS approach was being introduced. After these exclusions a total of 255 hips were left for inclusion in the study; 142 operated using the STD and 113 operated using an anterior MIS approach.
Used implants
From January 2008 to January 2009, a cementless hip system (seleXys TH+ cup, CBC stem, ceramys head and inlay, Mathys, Bettlach, Switzerland) or a hybrid system (cementless RM Pressfit monobloc cup, cemented CCA stem, Bionit head, Mathys, Bettlach, Switzerland) was used. From January 2009 to September 2009, the twinSys stem (Mathys, Bettlach, Switzerland), either cementless or cemented, was implanted in combination with the same RM cups. From October 2009 onward, the cementless system consisted of an Allofit cup, Avenir stem, Sulox head and Durasul inlay (Zimmer, Winterthur, Switzerland), while the cemented hybrid system remained the same. In three cases, an acetabular reinforcement ring (Müller ring, Zimmer) or a polyethylene cemented cup was implanted. The used head sizes were 28 mm in 18% of the patients, 32 mm in 56% and 36 mm in 26%, respectively.
Surgical technique
All operations were performed in a standardized setting. Implant size, position and leg length were planned with a digital planning tool (AGFA Orthopaedic Tools, Agfa HealthCare N.V, Mortsel, Belgium). An image intensifier was used in all operations for intraoperative control of implant position and orientation. Leg-length was referred to the planning and the measured distance of the tip of the cone to the minor trochanter. The STD group was operated in supine position with a direct lateral approach, as described by Bauer,16 in a muscle sparing technique with a short split of the glutaeus medius muscle to avoid damage of the medial gluteal nerve (Figure 1).17 The MIS group was operated with an anterior MIS approach in supine position with the use of a standard trauma table (Maquet, Rastatt, Germany) as described by Matta and Shardar.18 The operated leg was draped and fixed in a leg holder, being hyperextended, adducted and external rotated for preparation of the femur without use of traction. Incision of the fascia was made about 2 cm lateral to the medial border of the tensor fascia lata muscle to avoid damage of the lateral cutaneal nerve (Figure 1) followed by a blunt dissection of the tensor on its medial border. A U-shaped capsulotomy was performed and the capsule was preserved. The branches of a retractor were placed ventrally in the capsule and dorsally in the femoral osteotomy to expose the acetabulum (Figure 2). For femoral exposure a cranio-dorsal capsular release was performed saving the tendon of the piriformis muscle and after elevation of the proximal femur it was kept in position with a curved retractor. Special instruments with offset handles were used for acetabular and femoral preparation. Patients received either general or spinal anesthesia in the STD group according to the preference of the patient and anesthesiologist and all received general anesthesia in the MIS group.
Figure 1.
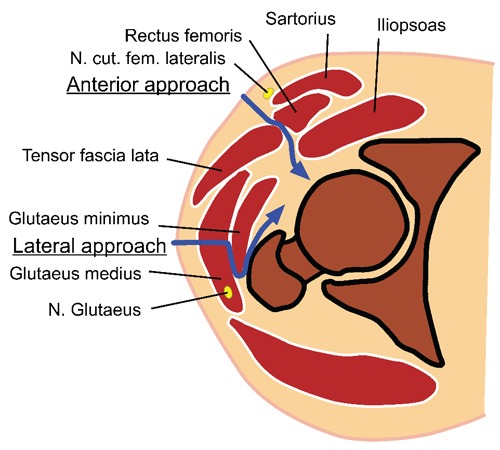
In the anterior approach the intermuscular space between rectus femoris and tensor fascia lata is developed, the lateral parts (musculus iliocapsularis) of the iliopsoas are lift off the capsule, no has to be refixed. The sensoric nervus cutaneaus femoris lateralis is close to the incision and might be damaged during preparation. In the lateral approach the musculus glutaeus medius is split and the musculus glutaeus minimus is lift off its insertion, they have to be refixed. In case of extended muscle split the motoric nervus glutaeus superior might be damaged.
Figure 2.
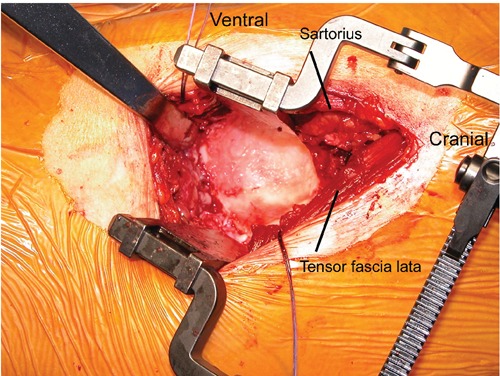
In the anterior approach the musculus sartorius and rectus femoris are mobilised anteriorly and the musculus tensor fascia lata posteriorly, respectively. They are kept under the retractor. The muscles can be mobilised cranially without risk of the innervation.
Postoperative treatment
Postoperative care followed a standardized protocol and was the same for both groups. Mobilization was initiated on the day after surgery and the drain was removed on the second or third day. Thereafter, independent mobilization was encouraged and full weight bearing was permitted, all patients were instructed on how to avoid dislocation.
Clinical follow-up
Patients were preoperatively assessed for hip function using a modified Harris Hip Score (HHS)19 and for their level of pain using a visual analogue scale (VAS). Study outcome parameters included the duration of surgery, number of complications and volume of blood loss. On the seventh day following surgery, wound healing (dry wound) was assessed and the following functional parameters were evaluated: the ability to independently get out of bed, the ability to walk with crutches, use of the toilet, the ability to climb stairs.
The length of hospital stay was recorded.
Patients were scheduled for follow-up examinations at six and 12 weeks, one and two years postoperatively. Assessments made at follow-up examinations included patients’ level of pain at rest and during movement as well as patient satisfaction using a VAS, limping and a modified HHS.
Radiological follow-up
Standardized radiographs of the pelvis (patient in supine position, centered on the symphysis, focus film distance 120 cm) were taken preoperatively and at one week, 12 weeks, one and two year postoperatively. The preoperative planning of the center of rotation was compared with the postoperative implant position in relation to the inter-teardrop line.20 Inclination of the cup was measured in reference to the interteardop line and anteversion was measured using the EBRA method.21
Statistics
Statistical analysis was performed with IBM SPSS Statistics 20 (IBM Corporation, Somers, New York). The distribution of each parameter was checked using the Kolmogorov-Smirnov test. In case of normally distributed data we used the t-test to compare data in two unpaired groups. If data were not normally distributed, a Mann-Whitney test was performed. Fisher’s exact test was used to compare parameters with binominal and ordinal results between the groups. A P-value <0.05 was considered statistically significant.
Results
All included patients had complete follow-up examinations. The main diagnosis was osteoarthritis (94.5%); 53% of the patients were male, the mean age was 70 years (range 40 to 93.2), the mean BMI was 27.4 (range 23 to 41), 83.1% had an American Society of Anesthesiologists (ASA) score of 2 or more. There was no difference in these demographic parameters for the two study groups. One hundred and twenty-eight of the 142 operations in the STD group, and all operations in the MIS group were performed or supervised by two consultants with special interest in hip surgery. All patients operated with the anterior approach received general anesthesia. In the standard group, 92 patients (64.8%) received general anesthesia and 50 patients received spinal anesthesia.
Perioperative parameters
The median duration of surgery was longer for MIS patients (119 vs 107 minutes, P<0.001). Median blood loss (700 vs 700 mL, P=0.291) and the need for transfusions (24.3% vs 25.7%, P=0.884) were similar for both groups.
Three patients had intraoperative fractures (all STD) and there were two early revisions due to hematoma (all STD), these patients were excluded from analysis of early and late functional results.
Hospital stay
Seven days after surgery the number of patients presenting with a dry wound (P<0.001), that were able to independently get out of bed (P=0.055, n.s.) and that were able to climb stairs (P=0.054, n.s.) were greater for the MIS group compared with the STD group. The ability of patients to walk with crutches (P=0.620) and use the toilet independently (P=0.500) was similar for both groups. The median duration of hospitalization was significantly shorter for patients in the MIS group (12.0 vs 11.0 days, P<0.001).
Clinical results
After six and 12 weeks, patients in the MIS group presented with significantly better outcomes for pain during movement, HHS and patient satisfaction (Table 1). In the MIS group there were more patients presenting with no limping at six weeks (47.3% vs 27.4% in STD, P<0.001) and 12 weeks (70.5% vs 48.1% in STD, P=0.002). There were no dislocations in both groups.
Table 1.
Clinical examination 6 weeks, 12 weeks, 1 year and 2 years after surgery.
| 6 weeks | 12 weeks | 1 year | 2 years | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STD | MIS | P | 95%CI* | STD | MIS | P | 95%CI* | STD | MIS | P | 95%CI* | STD | MIS | P | ||
| Median VAS pain at motion points (range) | 1.5 (0-8) |
1.0 (0-10) |
0.003 | 0.04-0.9 | 1.0 (0-8) |
0.0 (0-8) |
0.010 | 0.014-0.9 | 0.0 (0-7.2) |
0.0 (0-8.8) |
0.040 | -0.03-0.6 | 0.0 (0-10) |
0.0 (0-5) |
0.403 | |
| Median HHS points (range) | 77 (46-100) |
83 (42-100) |
0.003 | -7 to -1.4 | 91 (44-100) |
95 (51-100) |
0.009 | -5.9 to -0.3 | 96 (57-100) |
99 (73-100) |
0.005 | -6.2 to -1.9 | 99 (34-100) |
99 (56-100) |
0.509 | |
| Median VAS satisfaction (range) | 9.6 (2-10) |
10.0 (0-10) |
0.010 | -0.7-0.13 | 9.6 (0-10) |
10.0 (0-10) |
0.010 | -0.8-0.1 | 10.0 (2-10) |
10.0 (6-10) |
0.010 | -0.7 to -0.1 (3.7-10) |
10 (5-10) |
10 | 0.607 | |
Pain at motion, Harris Hip Score (HHS) and patients satisfaction 6 weeks, 12 weeks, 1 and 2 years postoperatively for the STD group and the MIS group. The P-values were calculated with the Mann-Whitney-Test (P-value of HHS after 6 weeks with the unpaired t-test).
*95% CI for group differences 6 weeks, 12 weeks and 1 year postoperatively.
During the first year of follow-up, there were three cases of aseptic cup loosening which needed to be revised (one in the MIS group and two in the STD group). There were two delayed infections, both in the MIS group, the implants were exchanged (1 one-stage-procedure and 1 two-stage-procedure). One patient (MIS) developed an acute hematogenous infection (sepsis with streptococci) after four months; it was treated with debridement and antibiotics. After one year, both groups had further improved in all parameters. All clinical parameters and the HHS still were significantly better for the MIS group as compared to the STD group. There were more patients with no limping in the MIS group (87.7%) than in the STD group (73.6%, P=0.038). At two years there was no more difference in the clinical parameters between both groups and the number of patients without limping was similar (MIS 82.5%, STD 80%, P=0.711) (Table 1).
Radiological results
Radiographs of two hips in the standard group and one hip in the MIS group could not be analyzed due to projection differences and poor quality and were excluded from the radiographic analysis. There was no difference between the groups in implant positioning for the horizontal position (P=0.669) and for the vertical position (P=0.190). Inclination was higher (P=0.011) and anteversion was lower (P=0.056, n.s.) among MIS-treated patients (Table 2), the number of cups with extreme inclination (less than 30° or more than 50°, P=0.326) and anteversion (less than 10° or more than 30°, P=0.531) was similar in both groups.
Table 2.
Radiological examination: postoperative positioning and orientation.
| STD | MIS | P | |
|---|---|---|---|
| Mean change of position Medially (SD) Range (mm) |
-1.7 4 -12.2 to 9.7 |
-1.9 3.6 -12.4 to 6.5 |
0.669 |
| Mean change of position Cranially (SD) Range (mm) |
0.9 4.1 -10.3 to 12.8 |
1.5 3.7 -7.3 to 11.4 |
0.190 |
| Mean inclination (SD) Range (°) |
37.7 (6.8) 18.3 to 55.3 |
39.8 (5.9) 24.9 to 52 |
0.011 |
| Mean anteversion (SD) Range (°) |
23.7 (7.5) 7 to 42 |
21.8 (8) 1 to 42 |
0.056 |
Change of position (medially and cranially) and cup orientation (inclination and anteversion) for the STD group and the MIS group (unpaired t-test). 95% CI for group differences for orientation: inclination, -3.8 to -0.5; anteversion, -0.1 to 3.8.
Discussion
More patients treated with the MIS anterior approach presented with a dry wound at one week and there was no evacuation of hematoma, but two patients in the MIS group were revised for delayed infection with implant exchange. The anterior skin is thinner and probably more delicate as compared to lateral or posterior skin areas and care has to be taken on disinfection and skin protection.22,23 There was a strong tendency that the ability to get out of bed and to climb stairs was better in the MIS group but did not reach a significant level. The function was superior for the MIS group after six and 12 weeks and even after one year, as evidenced by significantly better outcomes for pain during movement, limping, Harris Hip Score and patient satisfaction. Several studies show similar advantages of the MIS anterior approach in the early functional outcome.4,6,7 The direct anterior approach is the only approach using a true intermuscular interval, avoiding splitting of muscles and irritation of motor nerves.5 The glutaeus minimus and medius muscles are not exposed,4 occasional damage of the tensor fascia lata might have a minor effect on early rehabilitation. These differences disappear with time after surgery and were no more evident at 2 years.6
The only disadvantage of the MIS anterior approach that we found was a longer operation time. It is likely that this will shorten with increasing experience of the staff, including the handling of the trauma table.24
We introduced the MIS approach in a conservative, step-by-step fashion: the two responsible and experienced surgeons underwent extensive training, including external operation assistance, cadaver courses and anatomical studies. Stems with straight lateral edges were avoided and curved instruments were used for preparation. A consequent release of the postero-superior capsule for femoral preparation was performed and violent levering with retractors on the tip of the major trochanter was avoided. We could avoid trochanteric or femoral fractures and perforations in the MIS group which might have occured during the learning curve of the MIS anterior approach.13,22,23
The greater number of complications was observed in the STD group. This was in part due to the higher number of operating surgeons who, compared with the surgeons who performed the MIS hip replacements, had less experience with regard to the daily routine of hip replacement. The two delayed infections occurred in the MIS group. We have modified the intraoperative dressing by removing the plastic around the incision to keep the operation field dry. Short, heavy, and muscular males are more difficult for femoral exposure and obese patients with a belly covering the groin might not be suitable for the MIS approach.23 To avoid bias due to complications in the clinical results, these patients with complications were excluded from functional analysis.
We had no detailed look on palsy of the lateral femoral cutaneous nerve but numbness lateral and caudal to the incision occurred.1,23 Frequently it disappeared or patients got used to it, thus it did not remain a relevant problem. Lateral incision of the tensor fascia can reduce the incidence of this nerve affection.
Whereas all MIS patients received general anesthesia, only 64.8% of patients in the STD group received general anesthesia. Postoperatively, all patients of both groups followed the same treatment protocol. In fasttrack rehabilitation programs it is consensus that general anesthesia and opiates should be avoided as they lead to a prolonged early rehabilitation due to side effects.25 Nevertheless, in our study rehabilitation was facilitated for MIS-treated patients; they became mobile and independent earlier. This difference might even increase when more patients are operated under regional anesthesia.
The duration of stay in the hospital is affected by many factors like preoperative instruction of the patient, local resources for ambulant care and reimbursement of the treatment.15,26 During the study period, there were no changes in these socio-economic parameters, and payment of hospital care depended on the length of stay. Thus, there was no pressure for early discharge. The median length of hospital stay was shorter for MIS patients what might be explained by the facilitated early mobilization.7 But there might be a bias from the introduction of a new technique, the length of the incision and the knowledge of a minimal invasive operation might have had a psychological effect leading to a shorter stay too. More extensive preoperative instruction, better out-patient facilities and clear discharge management might have more impact in the length of hospital stay.
Blood loss and the need for transfusions were similar in both groups. Compared with reports from the literature, the rates were rather high.10,15 For both groups, no special care was taken to optimize preoperative hemoglobin levels. Blood loss and the need for transfusions may well decrease when introducing further precautionary measures. With the MIS approach, the acetabulum is easily exposed. The radiographic position was similar in both groups. We observed a broad range of orientation of the cup, which is frequently found in hip replacement.27,28 The cups in the MIS group had a slightly higher inclination and lower anteversion but the extrema were evenly distributed in both groups. Malorientation might be a problem in the use of MIS techniques,11,12 what can be avoided by the intraoperative use of an intensifier. The poor initial stability and early cup loosening of one specific implant (seleXys TH+ cup) was no problem of the used approach.
Stem preparation is more difficult when using an anterior MIS technique but we saw no increase in stem-related complications. Anteversion of the stem is difficult to assess and was not measured. As no dislocation occurred in both groups, we think that a satisfying cup and stem position and orientation can be reached with both methods. Patient instruction and the use of heads up to 36 mm might have avoided dislocations too and the anterior approach might further prevent posterior dislocation due to sparing of the posterior capsule. Leg length was not specifically assessed but leg length discrepancies did not appear to be a problem during follow-up.
One potential weakness of this study was the use of different implants during the study period. In order to facilitate the implantation of the stem using the MIS technique, the twinSys stem was introduced two months prior to the start of the MIS series, being oblique on the cranio-lateral edge, as compared to the previously used CBC and CCA stems, that have a bulky lateral shoulder. Later we observed problems with the primary stability of the spherical pressfit cup (seleXys TH+). Therefore, we introduced a new cup system and, in order to provide a complete implant system from one company, had to use another stem (Avenir) being very similar to the former one (twinSys). The introduction of the new implant system may have resulted in a negative influence on the results of the MIS group. Nevertheless, patients operated using the MIS technique presented with superior outcomes compared with patients who received the former implant system. Furthermore, all patients with cemented stems received the same cup (RM), and only differed in the stem (CCA cemented and later twinSys cemented stem). The outcomes for this subpopulation did not differ from the remaining patients. Thus, we believe that the choice of implant did not affect our clinical results.
The possibility of variation in the surgical technique was greater in the standard group since more surgeons performed operations in this group. As the lateral approach was routinely performed for many years prior to introduction of the MIS technique, more surgeons were familiar with it. In the MIS group, two surgeons with special interest in hip replacement joined all operations. Looking only on those patients operated by the two hip surgeons involved in both groups, the differences between groups remained the same, thus we believe that the surgeons did not influence the results.
We wanted to introduce the MIS approach to become probably the new standard. Using both approaches in the same time-period might cause a prolonged learning curve, risking more complications. Thus we preferred to use the approaches consecutively. In the setting of a public hospital we had no patient selection for the used approach besides the two exclusions from MIS due to obesity. Groups did not differ in patient parameters and our data should be valid even without randomization.
Conclusions
The introduction of the MIS anterior approach at our center was safe and led to improved early rehabilitation and clinical results relative to the STD lateral technique even one year postoperatively. But two deep infections in the MIS group were a point of concern. Radiological results were not affected by the new approach. The MIS anterior approach seemed not to be associated with specific disadvantages and we continue its use in routine clinical practice at our hospital. Additional adaptations and improvements in the clinical setup may further facilitate rehabilitation.
References
- 1.Smith TO, Blake V, Hing CB.Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop. 2011;35:173-84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pospischill M, Kranzl A, Attwenger B, et al. Minimally invasive compared with traditional transgluteal approach for total hip arthroplasty: a comparative gait analysis. J Bone Joint Surg Am. 2010;92:328-37 [DOI] [PubMed] [Google Scholar]
- 3.Bertin KC, Rottinger H.Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res 2004;248-55 [PubMed] [Google Scholar]
- 4.Bremer AK, Kalbere F, Pfirrmann CW, et al. Soft-tissue changes in hip abductor muscles and tendons after total hip replacement: comparison between the direct anterior and the transgluteal approaches. J Bone Joint Surg Br. 2011;93: 886-9 [DOI] [PubMed] [Google Scholar]
- 5.Kampa RJ, Prasthofer A, Lawrence-Watt DJ, et al. The internervous safe zone for incision of the capsule of the hip. A cadaver study. J Bone Joint Surg Br. 2007;89: 971-6 [DOI] [PubMed] [Google Scholar]
- 6.Restrepo C, Parvizi J, Pour AE, et al. Prospective randomized study of two surgical approaches for total hip arthroplasty. J Arthroplasty. 2010;25:671-9 [DOI] [PubMed] [Google Scholar]
- 7.Goebel S, Steinert AF, Schillinger J, et al. Reduced postoperative pain in total hip arthroplasty after minimal-invasive anterior approach. Int Orthop. 2012;36:491-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin DH, Jan MH, Liu TK, et al. Effects of anterolateral minimally invasive surgery in total hip arthroplasty on hip muscle strength, walking speed, and functional score. J Arthroplasty. 2007;22:1187-92 [DOI] [PubMed] [Google Scholar]
- 9.Wright JM, Crockett HC, Delgado S, et al. Mini-incision for total hip arthroplasty: a prospective, controlled investigation with 5-year follow-up evaluation. J Arthroplasty. 2004;19:538-45 [DOI] [PubMed] [Google Scholar]
- 10.Ogonda L, Wilson R, Archbold P, et al. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005;87:701-10 [DOI] [PubMed] [Google Scholar]
- 11.Williams SL, Bachison C, Michelson JD, et al. Component position in 2-incision minimally invasive total hip arthroplasty compared to standard total hip arthroplasty. J Arthroplasty. 2008;23:197-202 [DOI] [PubMed] [Google Scholar]
- 12.Meneghini RM, Smits SA.A Prospective, randomized study of component position in two-incision mis total hip arthroplasty: a preliminary study. Surg Technol Int 2011;XXI:255-60 [PubMed] [Google Scholar]
- 13.Lloyd JM, Wainwright T, Middleton RG.What is the role of minimally invasive surgery in a fast track hip and knee replacement pathway? Ann R Coll Surg Engl. 2012;94:148-51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berger RA, Sanders SA, Thill ES, et al. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res. 2009;467:1424-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Husted H, Holm G, Jacobsen S.Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79:168-73 [DOI] [PubMed] [Google Scholar]
- 16.Bauer R, Kerschbaumer F, Poisel S, et al. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg. 1979;95:47-9 [DOI] [PubMed] [Google Scholar]
- 17.O’Brien DA, Rorabeck CH.The mini-incision direct lateral approach in primary total hip arthroplasty. Clin Orthop Relat Res. 2005;441:99-103 [DOI] [PubMed] [Google Scholar]
- 18.Matta JM, Shahrdar C, Ferguson T.Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115-24 [DOI] [PubMed] [Google Scholar]
- 19.Haddad RJ, Cook SD, Brinker MR.A comparison of three varieties of noncemented porous-coated hip replacement. J. Bone Joint Surg Br. 1990;72:2-8 [DOI] [PubMed] [Google Scholar]
- 20.Ilchmann T.Radiographic assessment of cup migration and wear after hip replacement. Acta Orthop Scand Suppl. 1997;276:1-26 [DOI] [PubMed] [Google Scholar]
- 21.Krismer M, Bauer R, Tschupik J, et al. EBRA: a method to measure migration of acetabular components. J Biomech 1995;28:1225-36 [DOI] [PubMed] [Google Scholar]
- 22.Jewett BA, Collis DK.High complication rate with anterior total hip arthroplasties on a fracture table. Clin Orthop Relat Res. 2011;469:503-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lovell TP.Single-incision direct anterior approach for total hip arthroplasty using a standard operating table. J Arthroplasty. 2008;23:64-8 [DOI] [PubMed] [Google Scholar]
- 24.D’Arrigo C, Speranza A, Monaco E, et al. Learning curve in tissue sparing total hip replacement: comparison between different approaches. J Orthop Traumatol. 2009;10: 47-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Husted H, Holm G.Fast track in total hip and knee arthroplasty—experiences from Hvidovre University Hospital, Denmark. Injury 2006;37 Suppl 5:S31-5 [DOI] [PubMed] [Google Scholar]
- 26.Mears DC, Mears SC, Chelly JE, et al. THA with a minimally invasive technique, multi-modal anesthesia, and home rehabilitation: factors associated with early discharge? Clin Orthop Relat Res. 2009;467:1412-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Callanan MC, Jarrett B, Bragdon CR, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469:319-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Laffosse JM, Accadbled F, Molinier F, et al. Anterolateral mini-invasive versus posterior mini-invasive approach for primary total hip replacement. Comparison of exposure and implant positioning. Arch Orthop Trauma Surg. 2008;128:363-9 [DOI] [PubMed] [Google Scholar]


