Abstract
Informed consent implies that the person undergoing an intervention thoroughly understands its pros and cons. We conducted a randomized control trial to evaluate patients’ recall of complications after day case hand surgery and how this can be influenced by age and/or socioeconomic factors. Patients’ wishes on the extent and type of provided information were also evaluated. A total of 124 cases were recruited. Ten cases were excluded because they presented for follow up more than 2 weeks after surgery. The other patients were randomized into 2 groups: the first one (48) received only verbal information, while the second one (66) also received written information sheets. No statistically significant difference was noted in the recall between the two groups. No difference among gender, age or socioeconomic status was noted. Most patients preferred both written and verbal information. Preference for knowledge of rates of complications increased when surgery was dangerous. Our results don’t show any significant difference in patients’ recall depending on the type of consenting method. Nevertheless, we still propose that patients should receive as much information as possible before undergoing any intervention.
Key words: informed consent, recall, day case surgery
Introduction
The Oxford Online Dictionaries define consent as permission for something to happen or agreement to do something and informed consent as permission granted in full knowledge of the possible consequences, typically that which is given by a patient to a doctor for treatment with knowledge of the possible risks and benefits.1 The term informed consent was first coined by Paul G. Gebhard in 1957 in a medical malpractice case in which a clinician at Stanford University Hospital was accused of not fully revealing the risks involved in a treatment procedure.
Gaining informed consent is an integral part of clinical practice and its nature and definition changes from region to region. It is the right of the patients to be fully aware of the intervention and a morale obligation of doctors that their patients understand what they have been told. Although a clinician would have spent immense time and effort along with all possible resources, it is still debatable as to how much patients actually understand and can recall.2
In the National Health Services, UK, there is a wide variability in the mode of consenting for surgical procedures and there is no inter or intra hospital and inter- or intra-departmental uniformity. Some patients are consented for the proposed surgical procedure on the initial consultation, some on the day of surgery and some attend a separate consenting clinic before surgery.
The recognition of the fact that patients do not lay down memory when consented for surgery is alarming and emphasizes the need for meticulous notes keeping.3 All these efforts are made to make sure that the patient fully understands the procedure and that in case of a complication and associated litigations, the treating doctor has evidence that patient was provided with all possible information.
We analyzed patient’s recall of complications undergoing day case procedures involving hand surgery. We aimed to assess the difference in recall, if patients were also delivered with written information in addition to verbal information in day case procedures. We also assessed the impact of gender, age and socioeconomic conditions on patients recall and patient’s preferences for consenting methods and the amount of information patient’s would like to have whilst being consented. Although there are studies available in the literature carried out in various specialties, but to our knowledge, this is the only study which also investigates the extent to which patient’s want to know about the risks of surgery.
Materials and Methods
This was a single center prospective randomized control trial for which prior approval was gained from the local quality evaluation and clinical governance department. Help was sought from our local statistician and consecutive patients undergoing elective day case procedures in our hand firm over a period of 6 months were recruited into the study after their consent. Those patients who were unable to consent for themselves were excluded from this study.
Patients were randomized into 2 groups by a sealed envelope method by one investigator only (AES) to eradicate any bias. The first group of patients received verbal information only including the operation itself, benefits of the procedure, alternative treatment options and associated complications. A trust approved consent form was then signed by the patient and a copy provided to the patients based on their wishes. The second group in addition to all this also received an A4 sized document, explaining all the risks involved. All the patients were consented by primary author to eradicate any bias.
General and regional anesthesia where required, was delivered by a consultant anesthetist and local anesthesia in all cases by the operating surgeon. All surgical procedures were performed by either the senior author or other authors under supervision of the senior author. All patients were discharged home the same day and reviewed in clinic for their first post operative visit and removal of sutures in a fortnight as per unit policy. At this stage, an A4 size questionnaire was provided to the patient’s assessing their recall of the risks mentioned on the day of surgery. It also asked them about their age, gender, socioeconomic background and preference for the method of consenting along with patient preference for knowledge pertaining to the extent of surgery and its complications. In order to eliminate bias, all questionnaires were filled in by the patients alone in waiting areas.
Our primary outcome measure was to analyze the impact of type of consenting on patient’s recall of risks after surgery. Secondary outcome measures were the effect of gender, age and socioeconomic background on patient’s recall. T tests were used for statistical analysis.
Results
A total of 124 cases were recruited during the study catchment period. Ten cases were excluded because they presented for follow up more than 2 weeks after surgery which was our catchment time for this study. Of the remaining, 48 cases were segregated into group 1 (verbal) and 66 into group 2 (verbal and written). All of the 10 excluded cases belonged to group 1.
Carpal tunnel decompression was carried out in 55 cases, Palmar fasciectomies for Duputryens contracture in 27 cases, excision of soft tissue lumps in 18 cases and 7 each of Trapeizectomies and trigger finger releases were included. Fifty four procedures were performed on left hand and 60 on the contralateral side. No bilateral cases were involved in the study. Majority of the patients had local anesthetic (62), whilst 48 had general anesthetic, 2 had a regional block and similar number had a combination of general anesthetic and regional block.
The mean percentage of risks recalled by groups 1 and 2 were 79% and 85% respectively. This difference was not statistically significant (P=0.1). Patients in both the groups had a similar pattern of recall of complications (Figure 1).
Figure 1.
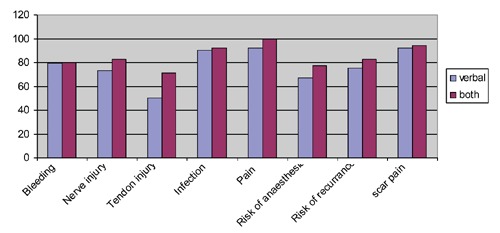
Patient recall of complications post operatively, showing no significant difference between the 2 methods of consenting (P=0.1).
Overall, most commonly recalled risks were pain, infection and scar tenderness. Tendon injury was the least recalled complication. More patients in group 2 recalled every one of the complications. Four patients were not well satisfied with information given, of whom 3 belonged to group 1 and 1 to group 2. No reasons were mentioned for this by the patients.
Age and gender
Seventy-five cases were aged more than 50 years and 37 were younger than 50. Two patients didn’t want to disclose their ages. Patients aged less than 50 and 50 and above remembered 87% and 81% of the complications respectively. This difference again was not statistically significant (P=0.2). Furthermore, when these 2 age groups were subcategorized into group 1 (verbal) and group 2 (verbal and written), no significant differences in their ability to recall complications was noted. Majority of patients in both age groups preferred to have both verbal and written information pre operatively (Figures 2 and 3). No significant difference in recall was noted between different genders.
Employment status
One hundred patients revealed their employment status. Half of them were employed (Group A) and half were either unemployed or retired or housewives (Group B). Group A and B recalled 86% and 79% of the risks respectively, which was again insignificant when these patients were sub grouped depending on the type of information they received (P=0.1).
Patients’ preferences
Majority of patients preferred to have both verbal and written information pertaining to the risks of surgery (Figure 3). When asked about the extent of information revealed to patients related to the risks associated with surgery, the preference decreased if risks were less than 1 in 100 and so on (Figure 4).
Figure 3.
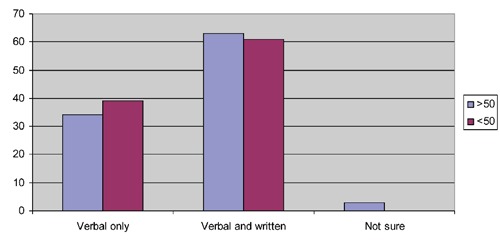
Majority of patients in both age groups demonstrating a preference for verbal and written consent together.
Figure 4.
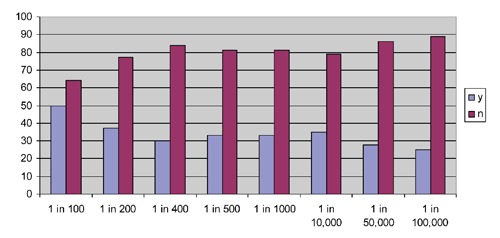
Patients demonstrated a decreasing interest to be informed of a complication associated with surgery as its incidence decreases from 1 percent.
Discussion
It has been noted by the medico-legal field that patients do not lay down memory when they are consented for surgery.3 In the court of law it is difficult to prove whether a patient wasn’t given information about a procedure and its complications or is it simply a case of forgotten details. Hence, the onus of proof falls on the clinician. Certainly, some patients will be able to comprehend and retain more information than others, which is simply a matter of different backgrounds and this is the scenario where tailor made information should be provided.
Exactly how much should be explained to the patient and how much they can comprehend is very subjective. A clinician was found negligent when he failed to warn the patient of a risk where its incidence was 1 in 14,000. Some other studies have reported that risks as low as one in 2 million should be explained to patients to reduce the risk of any medico legal action.3-5 It is also interesting to note here that bulk information can lead to less recall and comprehension in comparison to small amounts.6,7
Hutson and many others have shown that recollection of risks and benefits of surgery decreases with time. They also mentioned that patients tend to recall benefits more than complication.8 In order to improve patients recall of the whole informed consenting procedure, various adjuncts have been employed and tested along with the standard procedure including audiovisual and paper formats.8-11 These and many other studies have been conducted in different specialties checking for recall at variable periods and again showing variable results.12
We conducted this trial on day case procedures in hand surgery which to the author’s knowledge have not been conducted so far. Our results show that the percentage of risks recalled was higher in the group of patients who received both written and verbal information in comparison to the group who received only verbal information, although statistically not significant. This result is both in contrast and similar to some of the aforementioned studies. Robinson employed videotaping whilst consenting patients for thoracic surgery and again found significant discrepancies in recall.13 Numerous explanations have been proposed for the difference in recall but no solid evidence has been found. We propose a cool off period during the consenting process, where patients after being told in the clinic that they need surgery, should be seen, if possible, in a pre assessment clinic where they are consented and given ample opportunity to enquire. Later on the day of surgery, the consent form should be re confirmed with patients having another opportunity to ask anything, if needed. This, if logistically possible, would give ample time to patients to digest all the information and make well informed decisions. This ideally should increase there comprehension as well.
We also analyzed the effect of gender, age and employment status on patient recall. Although, there were minimum differences of percentage of recall noted between various subgroups, but none of them were statistically significant. This is in contradiction to a study which shows that recall was negatively influenced by older age.14 Our sample included only 5 patients above the age of 80, which might explain the reason for no difference.
We could not find any evidence in literature of the effect of gender and employment status on recall, but nonetheless, this was noted to be insignificant in our study. There is some evidence though that level of education and reading skills does affect both recall and comprehension.14 Our sample size was a case mix of different socioeconomic backgrounds, but mainly deprived background, which might have nullified the effect of one class over the other. Hence, geographical and demographic situation of the parent institution can affect the results.
All of our patients had English as their first language so our results were not biased by language barrier. Certainly there is evidence that patients belonging to different ethnic groups where English may not be the first language, level of comprehension and recall will be low.15 This proves the importance of geographical location and ethnicity of patient sample in patient recall and comprehension.
The standards of communication skills of the clinician delivering the information also affect the quality of patient information. Junior doctors may focus on technical terms and medical jargon during information giving and overlook certain other facts. More experienced clinicians are expected and proved to provide more elaborate information to patients.15,16 In our study, all patients were consented by one senior investigator to reduce any bias. We also checked for patient satisfaction with the consenting procedure, and only 4 patients out of the whole sample were not well satisfied. No reason was mentioned for this in the return questionnaire so we cannot make any comments. Certainly, with the introduction of European Working times directives, it will become increasingly difficult for junior doctors to master the art of informed consenting and almost impossible for a consultant to consent every single patient on the operating list. This is where printed information booklets can come in handy.
We also looked into patients’ preferences for consenting, and patients in all age groups and genders preferred to have both written and verbal information about their surgery and its risks. The preference of patients for awareness of risks associated with surgery was more if the associated risk was 1 in 100 or more. This steadily decreased with the decrease in the associated risk. This challenges the situation where it’s mentioned to reveal risks as low as 1 in 2 million in order to reduce the risk of medico legal action.3-5 If a clinician basis his or her practice based on this, they will spend a number of hours to touch base on every possible risk. This for all practical purposes is not possible and it has been proven that a bundle of information decreased patient recall and comprehension as medical jargon will invariably take over the communication, which becomes a bit too much for the patient.6,7
Conclusions
Lantos said that, if the goal of informed consent is risk management, consent forms should be encyclopedic.17 Unfortunately, in the current medico legal climate, this is in a way true. The burden of proof in any case in the court of law lies with the clinician. Whether some methods of information enhance patient’s comprehension and recall is debatable because of the effect of numerous variables. Nevertheless, it is a morale and legal duty of a clinician to exhaust all possible resources to ensure that patients fully understand what is being done to them otherwise any operation can count towards physical assault which can be liable to damages. Regardless of the type of material used during consenting, it is advised that meticulous documentation of this should be made in patient’s notes. This is unfortunately not what Leigh, a senior Solicitor, has noticed as he mentions I regularly advise doctors that their skills are for their patient and their notes are for themselves. My words fall on ears which are as deaf as the surgical patient.3
Figure 2.
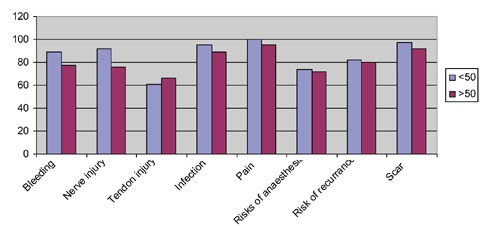
No statistically significant difference in recall found in patients less then 50 years and more than 50 years age groups.
References
- 1.Oxford Online Dictionaries. Available from: http://oxforddictionaries.com/definition/consent#m_en_gb0173250.007 [Google Scholar]
- 2.Shankar J.Patients’ memory for medical information. J R Soc Med. 2003;96:520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leigh B.Consent- an event or a memory? J Bone Joint Surg Br 2006;88-B:16-8 [DOI] [PubMed] [Google Scholar]
- 4.Whitaker RV.67 ALJR 47. Australian High Court. 1992 [Google Scholar]
- 5.Knapp TA, Huff RL.Emerging trends in the physicians’ duty to disclose: an update of Canterbury V Spence. J Leg Med (NY). 1975;1:41-5 [PubMed] [Google Scholar]
- 6.Dawes PJ, O’Keefe L, Adcock S.Informed consent: using a structured interview changes patients’ attitudes toward informed consent. J Laryngol Otol. 1993;107:775-9 [DOI] [PubMed] [Google Scholar]
- 7.Inglis S, Farnill D.The effects of providing preoperative statistical anaesthetic-risk information. Anaesth Intensive Care. 1993;21:799-05 [DOI] [PubMed] [Google Scholar]
- 8.Hutson MM, Blaha JD.Patients’ recall of preoperative instruction for informed consent for an operation. J Bone Joint Surg Am. 1991;73:160-2 [PubMed] [Google Scholar]
- 9.Shurnas PS, Coughlin MJ.Recall of the risks of forefoot surgery after informed consent. Foot Ankle Int. 2003;24:904-8 [DOI] [PubMed] [Google Scholar]
- 10.Krupp W, Spanehl O, Laubach W, Seifert V.Informed consent in neurosurgery: patients recall of preoperative discussion. Acta Neurochir (Wien). 2000;142:233-8 [DOI] [PubMed] [Google Scholar]
- 11.Fleischman M, Garcia C.Informed consent in dermatologic surgery. Dermatol Surg. 2003;29:952-5 [DOI] [PubMed] [Google Scholar]
- 12.Lemaire R.Informed consent: a contemporary myth? J Bone Joint Surg Br. 2006;88:2-7 [DOI] [PubMed] [Google Scholar]
- 13.Robinson G, Merav A.Informed consent: recall by patients tested postoperatively. Ann Thorac Surg. 1976;22:209-12 [DOI] [PubMed] [Google Scholar]
- 14.Sugarman J, McCrory DC, Hubal RC.Getting meaningful informed consent from older adults: a structured literature review of empirical research. J Am Geriatr Soc. 1998;46:517-24 [DOI] [PubMed] [Google Scholar]
- 15.Pette M, Pachaly J, David M.Turkish and German patients recall of diagnosis and therapy before and following informed consent. Ethn Health. 2004;9:213-23 [DOI] [PubMed] [Google Scholar]
- 16.Perez-Castanedo J, Hernando Robles P, Canellas Argesol M, et al. Information about operative risk: opinions of the physicians and patients involved. Rev Esp Anestesiol Reanim. 2004;51:20-7 [PubMed] [Google Scholar]
- 17.Lantos J.Informed consent: the whole truth for patients? Cancer 1993;72 Suppl 9:2811-5 [DOI] [PubMed] [Google Scholar]


