Abstract
In recent years, various uncemented proximal metaphyseal hip stems were introduced for younger patients as a bone preserving strategy. Initial osteodensitometric analyses of the surrounding bone of short stems indicate an increase of bone mass with secondary bone ingrowth fixation as a predictor of long-term survival of these types of implants. We report the outcome of 151 modular Metha short hip stem implants in 148 patients between March 2005 and October 2007. The mean follow-up was 5.8±0.7 years and the mean age of the patients was 55.7±9.8 years. Along with demographic data and co-morbidities, the Harris Hip Score (HHS), the Hip dysfunction and Osteoarthritis Outcome Score (HOOS), and also the results of a patient-administered questionnaire were recorded pre-operatively and at follow-up. The mean HHS increased from 46±17 pre-operatively to 90±5 the HOOS improved from 55±16 pre-operatively to 89±10 at the final follow-up. A total of three patients have been revised, two for subsidence with femoral revision and one for infection without femoral revision (Kaplan Meier survival estimate 98%). The radiological findings showed no radiolucent lines in any of the patients. The modular Metha short hip stem was implanted in younger patients, who reported an overall high level of satisfaction. The clinical and radiographic results give support to the principle of using short stems with metaphyseal anchorage. However, long-term results are necessary to confirm the success of this concept in the years to come.
Key words: short stem, total hip arthroplasty, Metha, bone preserving
Introduction
The concept of uncemented proximal metaphyseal hip stem fixation is well accepted in total hip arthroplasty (THA) therapy. For younger patients, a bone-preserving strategy at the time of index surgery is also well accepted. Therefore, many short stems have been developed by various companies in the last years, following the initial ideas of the conservative short Mayo hip stem.1 There are, however, numerous concepts for short stems today: with shorter straight stems, short anatomical or neck shaped designs, or with dedicated metaphyseal force induction features. All concepts follow the idea of a proximal force induction in the metaphyseal and calcar region. The distal stem has a guiding role during implantation, and helps primary stabilization, but does not add secondary fixation by bony ingrowth.
The clinical results can only be presented as short term results for a minimum of five years.2-4 Within the class of short stem THA, one has to take different stem designs into account.5 Today there is a variety of newly-developed short stems, which in recent years were used for the first time with only a few published results.6 Short-term bone density observations of these implants gave evidence of an initial minimal decrease in metaphyseal periprosthetic bone mineral density compared to proximally anchored standard stems.7-11 These studies essentially confirm the short stem anchoring concept.
Short hip stems address younger patients with good proximal femur bone quality to preserve bone for potential revisions in the future. Furthermore, these implants favor minimally invasive techniques that enable younger patients to start rehabilitation earlier. Radiologically, a good secondary stabilization due to metaphyseal ingrowth could be observed. It is a prerequisite of the prosthesis’s long-term-survival. First osteodensitometric investigations could confirm that a proximal loading leads to an increase in bone mass and osseointegration of the implant.12
We introduced cementless short hip arthroplasty in our department in 2005 and have implanted more than 1600 short hip stems. They made up for 35% of all cementless hip arthroplasty in 2011.
In this study, we present the clinical and radiological results of the first 151 short hip stem THAs with an average follow-up of five years.
Materials and Methods
Between March 2005 and October 2007, a total of 151 uncemented THAs using the modular Metha short stem (B.Braun Aesculap, Tuttlingen, Germany) were performed on a series of 148 patients. Our indications for using this implant were: age below 70 years and adequate bone stock. Exclusion criteria included: avascular necrosis of the femoral neck including the metaphysis, and poor bone stock. We also included patients who received a short stem as femoral revision of a surface replacement.
The modular Metha short stem was made of titanium alloy with two-thirds of the bone interface covered with a plasma-sprayed surface coating (Plasmapore µ-CaP). Six different modular stem sizes were available, with 9 neck adapters with 130, 135 and 140 deg CCD and –7.5, 0, and +7.5 degree ante/retro-versions.
A direct lateral THA approach was used for all patients, in a supine position.13 After the neck osteotomy and the implantation of the cup, the femoral canal was prepared. After preparing the femoral canal, a trial reduction was carried out. Depending on the range of motion and the anatomical orientation of the proximal femur, different tapers can be implemented (relative ante/retroversion and CCD angle). Fluoroscopic control in two planes was used to ensure correct broach alignment and to minimize leg length discrepancy.
Patients were allowed full weight-bearing from the first post-operative day using two crutches for safety reasons during mobilization. Flexion was restricted to 80 degrees for 6 weeks using a special pillow for sitting. Abduction and rotation exercises were performed during the first 6 weeks.
All demographic data and co-morbidities were recorded. Additionally, the Harris Hip Score (HHS), the Hip dysfunction and Osteoarthritis Outcome Score (HOOS), and the results of a patient-administered questionnaire were recorded pre-operatively and at the follow-up.
Standardized standing antero-posterior (AP) and lateral radiographs of the proximal femur were taken pre-operatively, immediately post-operatively and at the follow-up. All radiographs were analyzed by a single observer in respect of the adapted Gruen zones around the short stem to identify subsidence, osteolysis, and bone resorption (Figure 1).14 Ossifications were analyzed according to the Brooker classification.15 Furthermore, leg-length discrepancy was measured including an AP view of the pelvis in the upright position and clinically during the follow-up examination. All data were analyzed statistically using the student t-test.
Figure 1.
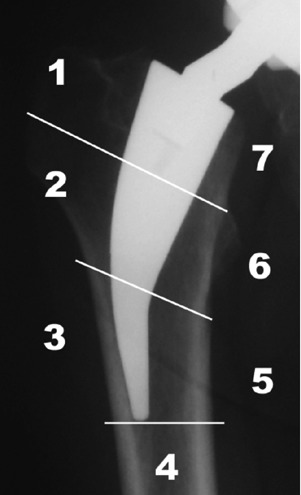
All radiographs were analyzed using the modified method of Gruen zones.
The study was approved by the local ethics committee.
Results
The average follow-up period was 5.8±0.7 years. There were 77 female and 74 male patients with an average age of 55.7±9.8 years. The main diagnoses were osteoarthritis in 88 patients (58%) (Figure 2), dysplastic osteoarthritis in 29 patients (19%), avascular necrosis of the femoral head in 15 patients (10%), after failed resurfacing in 6 patients (4%), and other reasons in 13 patients (9%) (Table 1).
Figure 2.
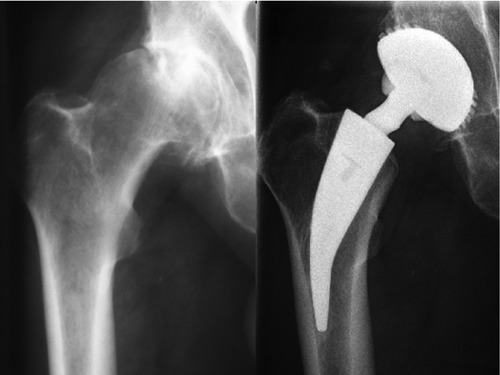
A 53-year-old male patient with osteoarthritis of the right hip joint. Radiograph at 5.1 years follow-up after short stem implantation combined with a threaded cup.
Table 1.
Patient characteristics of 151 hips in 148 patients.
| Variables | N. |
|---|---|
| Male | 74 |
| Female | 77 |
| Age in years (mean) Osteoarthritis |
55.7±9.8 88 |
| Dysplastic osteoarthritis | 29 |
| Avascular necrosis | 15 |
| Failure after resurfacing | 6 |
| Other indications | 13 |
The HHS improved from 46±17 pre-operatively to 90±5 at the latest follow-up. The HOOS improved from 55±6 pre-operatively to 89±10 (post-operative differentiation of the HOOS: symptoms 92±13, pain 92±12, activity 91±13, function/sports 89±17, and quality of life 89±24). Furthermore, the range of motion increased significantly for flexion, extension, abduction, internal rotation, and external rotation (P<0.05). At the latest follow-up, none of the patients reported severe or disabling thigh pain in the patient-administered questionnaire. None of the patients showed persistent Trendelenburg gait. Three patients used a cane for ambulation outdoors, but they attributed their need for a cane to other medical reasons. In three patients, a leg length discrepancy above 10 mm was recorded.
Eighty-one patients were given a 130 degree taper, and in 70 patients a 135 degree taper was used. Only five patients needed a modular taper with 7.5 degree anteversion and two patients required a taper with –7.5 degree retroversion. All other patients had a neutral modular taper.
Complications were found in three patients: one early infection was treated with a single-stage revision, and two subsidences were observed at 6 weeks and 8 weeks postoperatively due to undersizing, leading to mechanical problems that required a revision to a standard length hip stem. Heterotopic ossifications were identified in 2 patients, one classified as Brooker I and one as Brooker II. No further complications were observed. The Kaplan Meier survival estimate was 98.0% (Figure 3).
Figure 3.
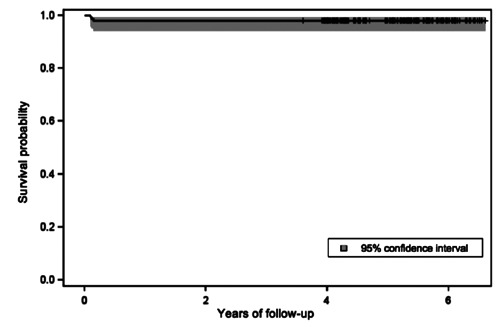
Kaplan Meier survival estimate of 98% after 5.8 years follow-up.
The radiographs were examined for all the patients. In terms of stem alignment, neutral alignment was attained in 138 (91%), valgus alignment in 6 (4%), and varus alignment in 7 (5%) hips. No radiolucent lines of more than 1 mm in thickness, osteolysis, bone resorption, or more subsidence than 3 mm in all Gruen zones were observed in any patients during the follow-up.
Discussion
During the last years the average age of THA patients decreased. Additionally, patient demands for faster rehabilitation and a higher level of functionality have increased.7,16 This has led to the development of short stems for THA.2,3,7,9,17 These prostheses can be implanted using a less- or minimally-invasive surgical approach to avoid muscle damage, preserve proximal bone, and to start rehabilitation earlier.3,9,18 A proximal anchorage of short stems may lead to the application of more physiological load.2,7,9,18 This was demonstrated by Morrey et al. in their 7-year survival rates of the Mayo short stem of 98%.3 The design and anchoring principle of the Metha short stem anchorage is similar to the Mayo short stem. They simply differ in the proximal shape of the implant, the surface coating and the modular set-up.
This study showed the successful implantation of the Metha short stem with good to excellent clinical results after an average follow-up of 5.8 years. As the implant was introduced in 2005, the follow-up period was shorter than in other studies of short stem implants,3,4,8,18 and comparable to recent clinical results of an average follow-up of 2,4 years of the same implant design.14 Our overall survival rate was over 98% to the time of follow-up. However, the results can be compared to recently published studies from Briem et al. 2011 with a survival rate of 99% in 155 cases after 6.2 years,19 Ettinger et al. with 100% after 5.2 years,20 and Wittenberg et al. with a survival rate of 96.7% after 4.9 years.21 Even in cases with osteonecrosis of the femoral head, this implant showed encouraging results.22 Compared to other uncemented standard stem designs with a similar age-group of patients, the 10-year survival rate is up to 98%.23
Radiographic evidence of good osseointegration of the short stem implant with no radiolucencies was rarely observed due to the short follow-up time. Other studies also describe the bone reactions in the Gruen zones which could be similar found in this study. There can usually found in the proximal or in the middle and distal parts of the implanted short stem.12,19,20,24,25 Complications such as aseptic loosening were not expected to be found in the first years after implantation of the stem, as early failures of cementless implants are mostly affected by an insufficient implantation technique. Only in two of our cases a significant subsidence >10 mm due to undersizing of the implant was recorded. This might be explained by the initial learning curve with this new implant.
Due to the modularity of the short stem design studied, the offset and rotation of the proximal femur can be addressed in order to respect the anatomy and reconstruct the biomechanics of each patient individually. Only in seven cases, a retro- or anteversion of the proximal femur was corrected by the modular taper. This is an advantage as especially younger patients scheduled for THA show anatomical deformities having lead to early osteoarthritis. Furthermore, younger patients have higher expectations concerning the range of motion due to their higher level of activity. To address anatomical deformities and the range of motion, we conclude that a modular system is helpful in some cases, but not mandatory for most patients receiving this particular short stem design.
Furthermore, the curved shape of this short stem supports less- and minimally-invasive hip approaches, such as the antero-lateral approach or the direct anterior approach.26,27 After cup implantation and the exposure of the femoral cavity, two curved awls open the femoral canal. The rasps also have curved handles to avoid damaging the muscle. These instruments enable a gentle and effective preparation of the femoral canal and implantation of the Metha short stem. Using different tapers with ante- and retroversion, a maximum range of motion and reconstruction of the offset can be achieved.
Metaphyseal anchorages of short stems provide undoubted advantages in terms of revision. In case of aseptic loosening, they allow a bone-preserving removal of the stem, often followed by implantation of a standard stem. Additionally, they represent an option for treating a failed resurfacing with a short stem and a large head.
In this study, the implantation of a short stem led to high levels of satisfaction in younger patients. The clinical and radiographic results encourage the principle of short stems providing a metaphyseal anchorage. It combines a minimally invasive implantation technique with bone-preservation, and easier revision. The short stem should be considered for younger patients after potential contraindications have been excluded (osteoporotic bone loss, avascular necrosis of the distal femoral neck/metaphysis, and a high degree of deformation). The implantation of a short stem in these cases may lead to early failure. However, long-term results are necessary to verify the concept in the years to come.
Conclusions
The modular Metha short hip stem reported an overall high level of satisfaction. The clinical and radiographic results give support to the principle of using short stems with metaphyseal anchorage. However, long-term results are necessary to confirm the success of this concept in the years to come.
References
- 1.Morrey BF.Short-stemmed uncemented femoral component for primary hip arthroplasty. Clin Orthop Relat Res 1989:169-75 [PubMed] [Google Scholar]
- 2.Ender SA, Machner A, Pap G, et al. Cementless CUT femoral neck prosthesis: increased rate of aseptic loosening after 5 years. Acta Orthop. 2007;78:616-21 [DOI] [PubMed] [Google Scholar]
- 3.Morrey BF, Adams RA, Kessler M.A conservative femoral replacement for total hip arthroplasty. A prospective study. J Bone Joint Surg Br. 2000;82:952-8 [DOI] [PubMed] [Google Scholar]
- 4.Pipino F, Keller A.Tissue-sparing surgery: 25 years experience with femoral neck preserving hip arthroplasty. J Orthopaed Traumatol. 2006;7:36-41 [Google Scholar]
- 5.Stukenborg-Colsman C.[Femoral neck prostheses]. Orthopade. 2007;36:347-52 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 6.Gulow J, Scholz R, Freiherr von Salis-Soglio G.[Short-stemmed endoprostheses in total hip arthroplasty]. Orthopade. 2007;36:353-9 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 7.Decking R, Rokahr C, Zurstegge M, et al. Maintenance of bone mineral density after implantation of a femoral neck hip prosthesis. BMC Musculoskelet Disord. 2008;9:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falez F, Casella F, Panegrossi G, et al. Perspectives on metaphyseal conservative stems. J Orthop Traumatol. 2008;9:49-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hube R, Zaage M, Hein W, Reichel H.[Early functional results with the Mayohip, a short stem system with metaphyseal-intertrochanteric fixation]. Orthopade. 2004;33:1249-58 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 10.Reiter A, Gellrich JC, Bachmann J, Braun A.[Changes of periprosthetic bone mineral density in cementless bicontact stem implantation; influence of different parameters—a prospective 4-year follow-up]. Z Orthop Ihre Grenzgeb. 2003;141:283-8 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 11.Roth A, Richartz G, Sander K, et al. [Periprosthetic bone loss after total hip endoprosthesis. Dependence on the type of prosthesis and preoperative bone configuration]. Orthopade. 2005;34:334-44 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 12.Gotze C, Ehrenbrink J, Ehrenbrink H.[Is there a bone-preserving bone remodelling in short-stem prosthesis? DEXA analysis with the Nanos total hip arthroplasty]. Z Orthop Unfall. 2010;148:398-405 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 13.Hardinge K.The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64:17-9 [DOI] [PubMed] [Google Scholar]
- 14.Braun A, Lazovic D, Zigan R.Modular short-stem prosthesis in total hip arthroplasty: implant positioning and the influence of navigation. Orthopedics. 2007;30:S148-52 [PubMed] [Google Scholar]
- 15.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr.Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629-32 [PubMed] [Google Scholar]
- 16.Chandler HP, Reineck FT, Wixson RL, McCarthy JC.Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426-34 [PubMed] [Google Scholar]
- 17.Huggler AH, Jacob HA, Bereiter H, et al. Long-term results with the uncemented thrust plate prosthesis (TPP). Acta Orthop Belg 1993;59 Suppl 1:215-23 [PubMed] [Google Scholar]
- 18.Thomas W, Lucente L, Mantegna N, Grundei H.[ESKA (CUT) endoprosthesis]. Orthopade. 2004;33:1243-8 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 19.Briem D, Schneider M, Bogner N, et al. Mid-term results of 155 patients treated with a collum femoris preserving (CFP) short stem prosthesis. Int Orthop. 2011;35:655-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ettinger M, Ettinger P, Lerch M, et al. The NANOS short stem in total hip arthroplasty: a mid term follow-up. Hip Int. 2011;21:583-6 [DOI] [PubMed] [Google Scholar]
- 21.Wittenberg RH, Steffen R, Windhagen H, et al. Five-year results of a cementless short-hip-stem prosthesis. Orthop Rev (Pavia). 2013;5:e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Floerkemeier T, Tscheuschner N, Calliess T, et al. Cementless short-stem hip arthroplasty METHA as an encouraging option in adults with osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2012;132: 1125-31 [DOI] [PubMed] [Google Scholar]
- 23.Ochs U, Eingartner C, Volkmann R, et al. [Prospective long-term follow-up of the cementless bicontact hip stem with plasmapore coating]. Z Orthop Unfall 2007;145 Suppl 1:S3-8 [Article in German]. [DOI] [PubMed] [Google Scholar]
- 24.Lerch M, von der Haar-Tran A, Windhagen H, et al. Bone remodelling around the Metha short-stem in total hip arthroplasty: a prospective dual-energy x-ray absorptiometry study. Int Orthop. 2012;36:533-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gill IR, Gill K, Jayasekera N, Miller J.Medium term results of the collum femoris preserving hydroxyapatite coated total hip replacement. Hip Int. 2008;18:75-80 [DOI] [PubMed] [Google Scholar]
- 26.Berger RA.The technique of minimally invasive total hip arthroplasty using the two-incision approach. Instr Course Lect. 2004;53:149-55 [PubMed] [Google Scholar]
- 27.Bertin KC, Rottinger H.Anterolateral mini-incision hip replacement surgery: a modified Watson-Jones approach. Clin Orthop Relat Res 2004:248-55 [PubMed] [Google Scholar]


