Abstract
Reconstruction of the posterior cruciate ligament (PCL) by a tibial press-fit fixation of the patellar tendon with an accessory bone plug is a promising approach because no foreign materials are required. Until today, there is no data about the biomechanical properties of such press-fit fixations. The aim of this study was to compare the biomechanical qualities of a bone plug tibial inlay technique with the commonly applied interference screw of patellar tendon PCL grafts. Twenty patellar tendons including a bone block were harvested from ten human cadavers. The grafts were implanted into twenty legs of adult German country pigs. In group P, the grafts were attached in a press-fit technique with accessory bone plug. In group S, the grafts were fixed with an interference screw. Each group consisted of 10 specimens. The constructs were biomechanically analyzed in cyclic loading between 60 and 250 N for 500 cycles recording elongation. Finally, ultimate failure load and failure mode were analyzed. Ultimate failure load was 598.6±36.3 N in group P and 653.7±39.8 N in group S (not significant, P>0.05). Elongation during cyclic loading between the 1st and the 20th cycle was 3.4±0.9 mm for group P and 3.1±1 mm for group S. Between the 20th and the 500th cycle, elongation was 4.2±2.3 mm in group P and 2.5±0.9 mm in group S (not significant, P>0.05). This is the first study investigating the biomechanical properties of tibial press-fit fixation of the patellar tendon with accessory bone plug in posterior cruciate ligament reconstruction. The implant-free tibial inlay technique shows equal biomechanical characteristics compared to an interference screw fixation. Further in vivo studies are desirable to compare the biological behavior and clinical relevance of this fixation device.
Key words: posterior cruciate ligament reconstruction, tibial press-fit fixation, interference screw, biomechanical properties
Introduction
Ruptures of the posterior cruciate ligament (PCL) are more rare than ruptures of the anterior cruciate ligament (ACL). They are often caused by traffic accidents like the classical dashboard injury, and sports injuries. The majority of patients remains asymptomatic and is treated conservatively.1 Some patients show significant symptoms with joint instability and subsequent articular deterioration, therefore being of potential benefit from reconstruction of the PCL.2,3 The appropriate management of PCL injuries remains controversial, with interventions extending from conservative treatment with physiotherapy to reconstruction of the PCL with a large variety of described techniques, expecting prevention of future osteoarthritic joint changes by regaining joint stability.3
A biomechanical study investigating the PCL-deficient knee revealed increased abnormal forces in the medial and patellofemoral compartment, predisposing to premature and severe arthritis.4 The Cochrane review from 2005 found no randomized controlled studies comparing effectiveness and safety of surgical and conservative interventions for PCL injuries in adults.3
By virtue of the complex anatomical structure of the PCL with its two bundles,3,5,6 the decision regarding graft choice and its fixation remains a contentious issue. Autografts like hamstrings, quadriceps tendon, or bone-patellar tendon-bone remain the gold standard for PCL reconstruction. Allografts like Achilles tendon are appropriate for revision surgery,7 whereas synthetic grafts should be avoided by reason of their drawbacks.8
The benefit of the bone-patellar tendon-bone (BPTB) graft is a rapid bone-to-bone healing into the tunnel within six weeks. However, BPTB grafts can produce more serious donor site morbidity and lead to a weakening of the pulley.9,10 Most surgeons still use hardware like intererence screws for fixation of the graft in the drill holes,11,12 even though this leads to artifacts during postoperative magnetic resonance imaging and the necessity of implant removal in case of revision surgery.13,14 Bioabsorbable poly-L-lactic acid interference screws are reducing their volume by around two thirds after two years.13,15,16
A hardware-free press-fit fixation device with bone plugs on either end of the patellar tendon graft can avoid these limitations. The classical tibial inlay procedure is based on anatomical insertion of the bone block into the sulcus at the posterior side of the tibial plateau at the origin of the native PCL. This technique prevents the so-called killer turn with its risk of graft failure by decreasing posterior translation and graft abrasion compared to the transtibial reconstruction of the PCL.17-19 Furthermore, the tibial inlay technique prevents transphyseal drilling in PCL reconstructions in children and adolescents.20,21
The disadvantages of the tibial inlay technique include increased operating time and an increased risk to the posterior neurovascular structures.22 A recent evidence-based systematic review from 2010 found a lack of objective data comparing the outcomes of transtibial versus inlay PCL reconstruction.23 The most recent systematic review from 2011 investigating both biomechanical and clinical studies found no certain advantage of arthroscopic transtibial PCL reconstruction compared to the open inlay technique.24 It suggested the further development of an arthroscopic tibial inlay technique, which may combine the advantages of the open inlay and the arthroscopic transtibial technique.24
The purpose of this study was to evaluate the biomechanical properties of tibial press-fit graft fixation combined with an additional bone block to interference screw fixation in PCL reconstruction with patellar tendon grafts.
Materials and Methods
The experimental setup was chosen analogously to a prior study investigating the fixation strength of tibial PCL fixations.25 Twenty patellar tendons including a 10 mm bone block from the tibial tuberosity were harvested from ten human cadavers. There were no signs of degeneration. The grafts were implanted into twenty legs of German country pigs. The pigs were adult, one year old, and had a weight between 100 and 120 lbs. The distal tibia was cut off and the shaft was cemented into an aluminium holder using cold-curing methyl-methacrylate resin (Technovit 4071, Heraeus Kulzer GmbH, Wehrheim, Germany).
In group P, the graft was attached in a press-fit technique with accessory bone plug (Figure 1A, B). The grafts in group S were fixed with an interference screw (Figure 1A, C). Each group consisted of 10 specimens.
Figure 1.

A) Tibial inlay procedure based on inserting the bone block of the graft anatomically into the sulcus at the posterior side of the tibial plateau at the origin of the native PCL; B) in group P, the graft was attached in a press-fit technique with accessory bone plug; C) the grafts in group S were fixed with an interference screw.
The constructs were analyzed in cyclic loading between 60 and 250 N for 500 cycles. Finally, an ultimate failure load with 1 mm/sec was performed. Elongation, failure mode and ultimate failure load were analyzed (Figure 2).
Figure 2.

Macroscopic view of the experimental biomechanical setting.
Statistical analysis
All mean values are reported with standard deviations. Normality and Equal Variance Tests were conducted. Comparison of two groups was conducted using a non-parametric T-test. All operations were performed using Sigma Stat 15.0 (SPSS company, Chicago, IL, USA). A significance level of P<0.05 was assumed.
Results
Elongation during cyclic loading between the 1st and the 20th cycle was 3.4±0.9 mm for group P and 3.1±1 mm for group S. Between the 20th and the 500th cycle, elongation was 4.2±2.3 mm in group P and 2.5±0.9 mm in group S (not significant, P>0.05; Figure 3A).
Figure 3.
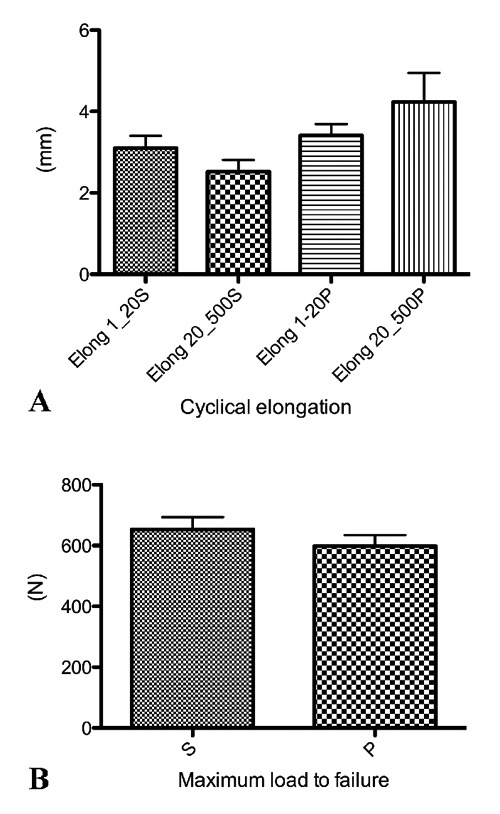
A) Elongation during cyclic loading between the 1st and the 20th cycle was 3.4±0.9 mm for group P and 3.1±1 mm for group S. Between the 20th and the 500th cycle, elongation was 4.2±2.3 mm in group P and 2.5±0.9 mm in group S (not significant, P>0.05); B) ultimate failure load was 598.6±36.3 N in group P and 653.7±39.8 N in group S (not significant, P>0.05).
Ultimate failure load was 598.6±36.3 N in group P and 653.7±39.8 N in group S (not significant, P>0.05; Figure 3B). In the moment of failure, 10/10 constructs failed due to a rupture of the tendon close to the bone lock in group P. In group S 9/10 constructs failed because of a tendon rupture close to the bone block and 1/10 failed because of a fracture of the proximal tibia.
Discussion
The most important finding of the study was that a tibial inlay press-fit fixation provides comparable biomechanical properties to interference screw fixation in PCL reconstruction.
Posterior laxity of the knee remains a challenge in orthopedic surgery. Combined joint instability patterns are common and reported as 85%.17 Associated injuries typically include posterolateral rotatory instability and combined anterior cruciate ligament injuries.10 As a prevention for graft failure resulting from abnormal lateral opening of the tibiofemoral joint, associated posterolateral rotatory instability should be corrected simultaneously during PCL reconstruction.7
In a biomechanical human cadaveric study by Markolf et al.26 from 2002, the acute angle in the tibial tunnel group lead to graft failure before finishing cyclic loading in 32%, while 100% of the tibial inlay group survived cyclic loading. Mean reduction of thickness of the graft was 40.6% in the tibial tunnel group and 12.5% in the tibial inlay group. They also found significantly less graft elongation in the tibial inlay group.26
Contradictory to the findings of Markolf et al.,26 McAllister et al.18 reported no significant differences concerning knee laxity between the tibial tunnel and tibial inlay techniques over the entire flexion range.18 Accordingly, Oakes et al.27 did not find differences between the tibial tunnel technique and the inlay technique for PCL reconstruction with bone-patellar tendon-bone grafts regarding generation of graft forces.27
To prevent high stress on the graft potentially leading to failure due to the sharp angle at the tibial tunnel entrance, the inlay technique consists of placement of a bone plug from the graft anatomically on the back of the tibia.11 Attempting to minimize graft-tunnel wall abrasion, a patellar BTB tibial inlay reconstruction of the PCL has been previously described by Berg in 1995.19 In his clinical case series, the quadriceps active drawer in 70 degrees of flexion was decreased by an average of 4 mm and improved patellofemoral symptoms.
Cooper et al. found convincing 2- to 10-year follow-up clinical results for bone-patellar tendon-bone grafts using tibial inlay fixation repairs of the PCL.17 Bergfeld et al. performed a human cadaver study comparing tibial PCL tunnel reconstruction with inlay reconstruction. The inlay technique showed less posterior translation with less graft degradation than the tunnel technique.11
The tibial inlay attachment in the double-bundle technique with use of Achilles tendon allografts yields satisfying results in PCL revision surgery.7
Several limitations apply to this study. First, this in vitro study provides no information about any dynamic biomechanical properties concerning kinematics. Second, the data presented in this study only pictures the time zero properties without any knowledge concerning the biological healing response.
Conclusions
This is the first study investigating the biomechanical properties of tibial press-fit fixation of the patellar tendon with accessory bone plug in posterior cruciate ligament reconstruction. The implant-free tibial inlay technique yields equal biomechanical characteristics compared to an interference screw fixation. Further in vivo studies are desirable to compare the biological behavior and clinical relevance of this fixation device.
Acknowledgements
the authors would like to thank Dr. Fabian Goede for excellent drawing of Figure 1.
References
- 1.Shelbourne KD, Clark M, Gray T.Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med 2013;41:1526-33 [DOI] [PubMed] [Google Scholar]
- 2.Fanelli GC, Beck JD, Edson CJ.Current concepts review: the posterior cruciate ligament. J Knee Surg 2010;23:61-72 [DOI] [PubMed] [Google Scholar]
- 3.Peccin MS, Almeida GJ, Amaro J, et al. Interventions for treating posterior cruciate ligament injuries of the knee in adults. Cochrane database Syst Rev 2005:CD002939. [DOI] [PubMed] [Google Scholar]
- 4.Boynton MD, Tietjens BR.Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med 1996;24:306-10 [DOI] [PubMed] [Google Scholar]
- 5.Amis AA, Gupte CM, Bull AM, Edwards A.Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc 2006;14: 257-63 [DOI] [PubMed] [Google Scholar]
- 6.Krudwig WK.[Functional anatomy of the posterior cruciate ligament]. Unfallchirurgie 1996;22:49-56 [Artice in German] [PubMed] [Google Scholar]
- 7.Lee SH, Jung YB, Lee HJ, et al. Revision posterior cruciate ligament reconstruction using a modified tibial-inlay double-bundle technique. J Bone Joint Surg Am 2012;94:516-22 [DOI] [PubMed] [Google Scholar]
- 8.Frank CB, Jackson DW.The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am 1997;79: 1556-76 [DOI] [PubMed] [Google Scholar]
- 9.Lobenhoffer P.[Chronic instability after posterior cruciate ligament injury. Tactics, techniques, and results]. Unfallchirurgie 1999;102:824-38 [Artice in German] [DOI] [PubMed] [Google Scholar]
- 10.Strobel MJ, Weiler A, Eichhorn HJ.[Diagnosis and therapy of fresh and chronic posterior cruciate ligament lesions]. Chirurg 2000;71:1066-81 [Artice in German] [DOI] [PubMed] [Google Scholar]
- 11.Bergfeld JA, McAllister DR, Parker RD, et al. A biomechanical comparison of posterior cruciate ligament reconstruction techniques. Am J Sports Med 2001;29:129-36 [DOI] [PubMed] [Google Scholar]
- 12.Brand J Jr, Hamilton D, Selby J, et al. Biomechanical comparison of quadriceps tendon fixation with patellar tendon bone plug interference fixation in cruciate ligament reconstruction. Arthroscopy 2000;16:805-12 [DOI] [PubMed] [Google Scholar]
- 13.Drogset JO, Grontvedt T, Myhr G.Magnetic resonance imaging analysis of bioabsorbable interference screws used for fixation of bone-patellar tendon-bone autografts in endoscopic reconstruction of the anterior cruciate ligament. Am J Sports Med 2006;34:1164-9 [DOI] [PubMed] [Google Scholar]
- 14.Noyes FR, Barber-Westin SD.Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J Bone Joint Surg Am 2001;83:1131-43 [DOI] [PubMed] [Google Scholar]
- 15.Jagodzinski M, Geiges B, von Falck C, et al. Biodegradable screw versus a press-fit bone plug fixation for hamstring anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med 2010;38:501-8 [DOI] [PubMed] [Google Scholar]
- 16.Apostolopoulos A, Nikolopoulos D, Polyzois I, et al. Pretibial cyst formation after anterior cruciate ligament reconstruction with poly-L acid screw fixation: a case report presentation and review of the literature. J Surg Orthop Adv 2012;21:151-6 [DOI] [PubMed] [Google Scholar]
- 17.Cooper DE, Stewart D.Posterior cruciate ligament reconstruction using single-bundle patella tendon graft with tibial inlay fixation: 2- to 10-year follow-up. Am J Sports Med 2004;32:346-60 [DOI] [PubMed] [Google Scholar]
- 18.McAllister DR, Markolf KL, Oakes DA, et al. A biomechanical comparison of tibial inlay and tibial tunnel posterior cruciate ligament reconstruction techniques: graft pretension and knee laxity. Am J Sports Med 2002;30:312-7 [DOI] [PubMed] [Google Scholar]
- 19.Berg EE.Posterior cruciate ligament tibial inlay reconstruction. Arthroscopy 1995;11: 69-76 [DOI] [PubMed] [Google Scholar]
- 20.Warme WJ, Mickelson D.All-epiphyseal semitendinosus PCL reconstruction in a 10-year-old child. J Pediatr Orthop 2010;30: 465-8 [DOI] [PubMed] [Google Scholar]
- 21.Bovid KM, Salata MJ, Vander Have KL, Sekiya JK.Arthroscopic posterior cruciate ligament reconstruction in a skeletally immature patient: a new technique with case report. Arthroscopy 2010;26:563-70 [DOI] [PubMed] [Google Scholar]
- 22.Papalia R, Osti L, Del Buono A, et al. Tibial inlay for posterior cruciate ligament reconstruction: a systematic review. Knee 2010;17:264-9 [DOI] [PubMed] [Google Scholar]
- 23.May JH, Gillette BP, Morgan JA, et al. Transtibial versus inlay posterior cruciate ligament reconstruction: an evidence-based systematic review. J Knee Surg 2010;23:73-9 [DOI] [PubMed] [Google Scholar]
- 24.Panchal HB, Sekiya JK.Open tibial inlay versus arthroscopic transtibial posterior cruciate ligament reconstructions. Arthroscopy 2011;27:1289-95 [DOI] [PubMed] [Google Scholar]
- 25.Ettinger M, Wehrhahn T, Petri M, et al. The fixation strength of tibial PCL press-fit reconstructions. Knee Surg Sports Traumatol Arthrosc 2012;20:308-14 [DOI] [PubMed] [Google Scholar]
- 26.Markolf KL, Zemanovic JR, McAllister DR.Cyclic loading of posterior cruciate ligament replacements fixed with tibial tunnel and tibial inlay methods. J Bone Joint Surg Am 2002;84:518-24 [DOI] [PubMed] [Google Scholar]
- 27.Oakes DA, Markolf KL, McWilliams J, et al. Biomechanical comparison of tibial inlay and tibial tunnel techniques for reconstruction of the posterior cruciate ligament. Analysis of graft forces. J Bone Joint Surg Am 2002;84:938-44 [DOI] [PubMed] [Google Scholar]


