Abstract
Background:
The maintenance of balance is an essential requirement for the performance of daily tasks and sporting activities and muscular fatigue is a factor to impair postural control, so this study was done to compare the effect of selected muscle groups fatigue on postural control during bipedal stance in healthy subjects.
Materials and Methods:
Fifteen healthy female students (24.3 ± 2.6 years) completed three testing session with a break period of at least 2 days. During each session, postural control was assessed during two 30-s trials of bipedal stance with eyes close before and after the fatigue protocol. Fatigue protocols were performed by 60% of their unfatigued Maximum Voluntary Contraction of unilateral ankle plantar flexors, bilateral lumbar extensors and bilateral neck extensors. One of the three fatigue protocols was performed on each session.
Results:
The result showed that fatigue had a significant effect on COP velocity and it increase COP velocity but there was not found any difference in postural sway between muscle groups.
Conclusion:
Localized muscle fatigue caused deficits in postural control regardless of the location of fatigue. Authors suggest the possibility of the contributions of central mechanisms to postural deficits due to fatigue and it seems that difference was not between muscle groups due to central fatigue.
Keywords: Center of pressure, fatigue, postural control
INTRODUCTION
Muscle fatigue is related to a decrease in capacity or force production following repeated muscle contraction. The onset of fatigue may be attributed to metabolical or neurological factors controlled peripherally and centrally by the neuromuscular systems. It is demonstrated that fatigue affects the neuromuscular control. Neuromuscular control can be evaluated in several levels including brain, spinal cord or muscle as well as the muscular activation pattern and postural control.1 The maintenance of balance is an essential requirement for the performance of daily activities.2 Postural control involves multiple sensory systems (visual, vestibular and somatosensory), the motor systems, and sensory motor integration.3 Most studies have reported increased postural sway with localized muscle fatigue (LMF) at isolated muscle groups,4,5,6,7,8,9 and little attention has been paid to comparison of the effect of LMF at different sites. Bizid et al., reported that fatigue of the knee extensors can affect postural performance more than that of the ankle plantar flexor muscles.10 Gribble and Hertel examined the effects of isokinetic muscle fatigue of the hip and ankle on postural control during single leg stance. There was an adverse effect of localized fatigue on postural control maintenance and the effect was greater for fatigue of the hip musculatures compared to the ankle ones.11 Salavati et al., found similar results following fatigue of the hip and ankle musculature.2 Dickin and Doan did not observe any difference between the fatigue effects of the knee and ankle musculature in impairment of postural control.12 Lin et al., indicated that acute effects of fatigue differed between muscle groups, and the most effect was seen at the lower back and then by the ankle. Neither the knee nor the shoulder fatigue resulted in significant effects on the postural control.3 Most of the studies have been limited to lower extremity musculature, and there is little evidence to compare the effect of the axial muscle fatigue and lower extremities fatigue on the postural control. This study aimed to compare the effect of fatigue of three muscle groups: The back extensor, neck extensor, and ankle plantar flexor on the postural control”. It was hypothesized that fatigue-related decrease in postural control would differ in severity in different fatigue sites.
MATERIALS AND METHODS
Fifteen healthy female (age 24.3 ± 2.7 year, height 163 ± 4 cm, body weight 54.9 ± 5.5 kg, mean ± SD) university students studying in the School of Rehabilitation Sciences of Shiraz University of Medical Sciences were selected through non-randomized sampling to participate in this study. All the participants gave informed consent to the experimental procedure and the study was approved by the Shiraz University of Medical Sciences Ethic Committee. The participants were excluded if they had any history of lower extremity or spine injuries within the last year, any deformity, pain or surgery in the lower extremity or spine, neuro-musculoskeletal disorders, and visual and vestibular problems. They were also excluded if they had professional sports participation in the past 6 months. 2, 3.
Measurements of maximum voluntary contraction (MVC) and fatigue protocols were performed by dynamometer (MIE, LTD, UK). In order to measure postural control, we used the force platform (Kistler Switzerland, type 9286 AA). COP data were collected with the sample frequency of 120 Hz.
There were three separated experimental sessions with a break interval of at least 2 days. One of the three fatigue protocols was performed on each session, and the order of protocols was randomized between the participants. During each session, postural control was assessed before and after completing an isometric fatigue protocol. For all the subjects, fatigue protocol of the ankle plantar flexors was applied on the dominant lower extremity (dominant lower extremity was determined by using the test of kicking a ball).10
The maximum voluntary contraction (MVC) protocol consisted of three maximum contractions of 5-second duration, with 1-min rest between contractions. The greatest value of all trials was taken to represent the subject's MVC (Davidson, Madigan ML, & Nussbaum, 2004). The level of contraction throughout the fatigue procedures was set at 60% of MVC.6 Contraction continued until the torque output for the participants dropped below 60% of peak torque.13 Then the subjects were removed from dynamometer and tested for postural control with a delay of no more than 20s.
Ankle plantar flexors: The participants were placed in long sitting posture (90° shank/foot flexion, 90° hip flexion) and performed isometric contraction with the ankle plantar flexors.
Neck and lumbar extensors: MVC for the lumbar and cervical erector spine was determined by using an apparatus which was designed to seat the subject so that the upper body was perpendicular to the walkway surface. To remove the potential effect of the hip extensor activity contributing to the MVC of the lumbar extensors, the apparatus seat height was adjusted so that the trunk thigh angle was at 135° and the shank-thigh at 90°. Orientation of the upper and lower body in this position assisted in maintaining equilibrium at the hip level and neutral lumbar lordosis. MVC for lumbar erector spine (LES) was measured using a strap connected in series with a fixed vertical post and a chest harness. An adjustable beam attached to the fixed post supported the pelvic to ensure the hips remained stationary; this configuration created a force couple between the pelvis and trunk when the subject pulled him/herself to the direction of posterior via the chest harness and resulted in contraction of the LES [Figure 1]. Procedure to measure MVC of the cervical erector spine (CES) were similar; however, a head harness used in place of the chest harness, and the adjustable support beam previously stabilizing the pelvis was placed over the sternum, so that a force couple was created between the upper thoracic region and the head [Figure 2].
Figure 1.
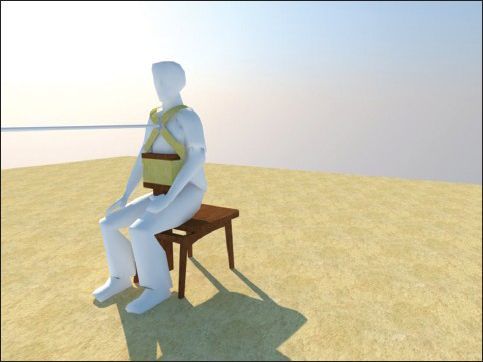
Method used to measure isometric maximum voluntary contraction of lumbar extensors
Figure 2.
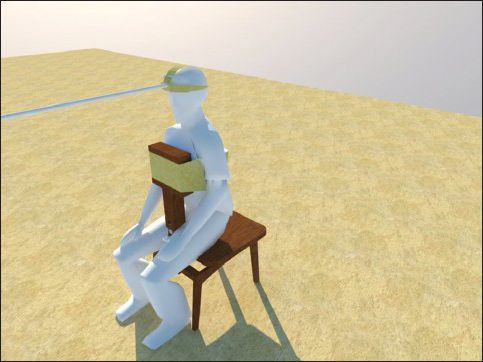
Method used to measure isometric maximum voluntary contraction of neck extensors
In order to measure postural control, the subjects were asked to maintain a double leg stance on the platform while barefoot, arms at their sides, feet together, head pointed straight ahead, and eye closed.6 Two trials of 30s were performed before and after the fatigue protocol with 10s rests between the trials.14
COP signals were smoothed using a fourth-order zero-lag Butterworth filter with a 15-Hz low-pass cut-off frequency before computing the mean COP velocity (mm s-1).15 The mean COP velocity was sum of the cumulated COP displacements divided by the total time.
Statistical analysis
Statistical analysis was performed using SPSS software version 16.0. The means of the two pre-trials and two post-trials were used for all analysis. Kolmogorov-Smirnov test was used to confirm normal distribution of data. Post-fatigue changes in COP velocity in the three groups were compared using univariate Two-way ANOVA. The independent factors were muscle groups (with three levels: Neck, lumbar, ankle) and condition (with two levels: Pre-fatigue and post-fatigue), and the dependent factor was COP velocity. The level of significance was considered P < 0.05 for all analysis.
RESULTS
The results showed that the “condition” had a significant effect on COP velocity (F = 5.07; P = 0.027) [Figure 3]. It means that muscle fatigue caused an increase in the COP velocity. The statistical analysis revealed no significance for the main effect of “muscle groups” (F = 1.45, P = 0.23), nor for “condition x” muscle groups interaction [F (1,2) = 0.08; P = 0.92]. It means that there were no differences in postural sway with regard the three muscle groups used in this study. Because main effect for “condition” (two levels of factor) was significant then post-hoc was not necessary.
Figure 3.
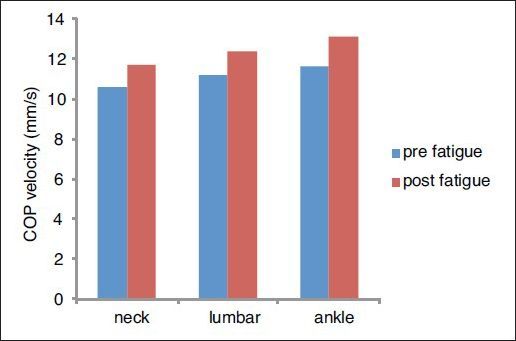
Mean values and standard deviations of COP velocity for the three groups muscle in pre and post-fatigue steps
DISCUSSION
The results of this study suggest that localized muscle fatigue of the ankle plantar flexors, neck extensors and lumbar extensors reduces the postural control in healthy young women. Although the postural control was impaired as a function of fatigue, there were no significant differences between the three muscle groups. Developing fatigue in a working muscle can be achieved by requiring the muscle to perform isometric, eccentric and concentric movements or a combination of the three forms of muscle actions. The current study utilized activities that involved isometric actions for all three protocols; therefore, similar type of contraction may be one of the causes of obtained non-significant differences between the three groups. The results of the current study are consistent with Dickin and Doan's study12 in which lower extremity muscle groups (knee or ankle) and overall fatigue of the dominant leg affected the balance system. Both joint-localized fatigue and overall fatigue were found to induce impairments in the postural control, no differences in the postural sway were found between fatigue locations or across any interactions between sway and fatigue locations. In contrast, Lin et al.,3 reported that immediate effects of fatigue differed in different joints, with the most substantial effects evident at the lower back, followed by the ankle. Neither the knee nor shoulder fatigue resulted in significant effects on the postural control. The participants performed submaximal isotonic fatiguing exercise (using Biodex Medical Systems) involving the unilateral knee extensors, ankle plantar flexors, and shoulder flexors, and bilateral lumbar extensors. In their investigation, the muscle groups were fatigued by using different fatigue protocols and different types of contraction. Corbeil et al.,16 reported no increased COP variability in either the sagittal or frontal planes of movement during double-limb stance when the plantar flexors were fatigued. Perhaps different results are related to the use of different protocols. They used repeated plantar flexion for fatigue protocol, whereas in our method we used isometric fatiguing protocol. Babault et al.,17 reported that isometric actions induce central fatigue first, followed by peripheral fatigue. These authors reported that metabolite concentration might be higher during isometric fatiguing procedure compared with concentric fatiguing (the intermittent nature of the concentric procedure may favour blood flow and, therefore, the evacuation of metabolic products) and would first increase the inhibitory effect of small diameter afferents (groups III and IV) and involve α-motor neuron inhibition at the spinal level. More precisely, a high metabolite concentration induces recurrent inhibition, presynaptic inhibition of 1a afferents, stretch-reflex disfacilitation and responsiveness of Golgi tendons organs, hence, a high metabolite concentration generates a decrease in the contribution of proprioceptive input and, thus, would affect the efficiency of the postural regulation mechanism. In practice, this phenomenon could involve deterioration of the postural control.
The limitations of this study were that applying fatigue protocol on both lower extremities by the existing dynamometer was impossible; moreover, the authors interpreted that central fatigue probably caused impaired postural control, but it was not investigated. Our results suggest that LMF caused deficits in the postural control regardless of the location of fatigue. When muscles are in fatigued state, they become less efficient at providing joint stability within the sensorimotor system.
ACKNOWLEDGMENTS
The authors would like to thank Shiraz University of Medical Sciences for the support during the course of this research. We also thank the volunteer participants for their time and support. This article is extracted from a Master of Sciences thesis Fatemeh Nikhalat, MSc, proposal number 5233). The authors would like to thank Dr. Nasrin Shokrpour at Center for Development of Clinical Research of Nemazee Hospital for editorial assistance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gribble PA, Hertel J. Effect of lower-extremity muscle fatigue on postural control. Arch Phys Med Rehabil. 2004;85:589–92. doi: 10.1016/j.apmr.2003.06.031. [DOI] [PubMed] [Google Scholar]
- 2.Salavati M, Moghadam M, Ebrahimi I, Arab AM. Changes in postural stability with fatigue of lower extremity frontal and sagittal plane movers. Gait Posture. 2007;26:214–8. doi: 10.1016/j.gaitpost.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Lin D, Nussbaum MA, Seol H, Singh NB, Madigan ML, Wojcik LA. Acute effects of localized muscle fatigue on postural control and patterns of recovery during upright stance: Influence of fatigue location and age. Eur J Appl Physiol. 2009;106:425–34. doi: 10.1007/s00421-009-1026-5. [DOI] [PubMed] [Google Scholar]
- 4.Vuillerme N, Anziani B, Rougier P. Trunk extensor muscles fatigue affects undisturbed postural control in young healthy adults. Clin Biomech (Bristol, Avon) 2007;22:489–94. doi: 10.1016/j.clinbiomech.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Vuillerme N, Pinsault N, Vaillant J. Postural control during quiet standing following cervical muscular fatigue: Effects of changes in sensory inputs. Neurosci Lett. 2005;378:135–9. doi: 10.1016/j.neulet.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 6.Davidson BS, Madigan ML, Nussbaum MA. Effects of lumbar extensor fatigue and fatigue rate on postural sway. Eur J Appl Physiol. 2004;93:183–9. doi: 10.1007/s00421-004-1195-1. [DOI] [PubMed] [Google Scholar]
- 7.Vuillerme N, Nougier V, Prieur J. Can vision compensate for a lower limbs muscular fatigue for controlling posture in humans? Neurosci Lett. 2001;308:103–6. doi: 10.1016/s0304-3940(01)01987-5. [DOI] [PubMed] [Google Scholar]
- 8.Schieppati M, Nardone A, Schmid M. Neck muscle fatigue affects postural control in man. Neuroscience. 2003;121:277–85. doi: 10.1016/s0306-4522(03)00439-1. [DOI] [PubMed] [Google Scholar]
- 9.Yaggie JA, McGregor SJ. Effects of isokinetic ankle fatigue on maintenance of balance and postural limits. Arch Phys Med Rehabil. 2002;83:224–8. doi: 10.1053/apmr.2002.28032. [DOI] [PubMed] [Google Scholar]
- 10.Bizid R, Margnes E, Francois Y, Jully JL, Gonzalez G, Dupui P, et al. Effects of knee and ankle muscle fatigue on postural control in the unipedal stance. Eur J Appl Physiol. 2009;106:375–80. doi: 10.1007/s00421-009-1029-2. [DOI] [PubMed] [Google Scholar]
- 11.Gribble PA, Hertel J. Effect of hip and ankle muscle fatigue on unipodal postural control. J Electromyogr Kinesiol. 2004;14:641–6. doi: 10.1016/j.jelekin.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Dickin DC, Doan JB. Postural stability in altered and unilateral sensory environments following fatiguing exercise of lower extremity joints. Scand J Med Sci Sports. 2008;18:765–72. doi: 10.1111/j.1600-0838.2007.00760.x. [DOI] [PubMed] [Google Scholar]
- 13.Kavanagh JJ, Morison S, Barret RS. Lumbar and cervical erector spinae fatigue elicit compensatory postural responses to assist in maintaining head stability during walking. J Apple Physiol. 2006;101:1118–26. doi: 10.1152/japplphysiol.00165.2006. [DOI] [PubMed] [Google Scholar]
- 14.Duarte M, Freitas SM. Revision of posturography based on force plate for balance evaluation. Rev Bras Fisioter. 2010;14:183–92. [PubMed] [Google Scholar]
- 15.Karlsson A, Frykberg G. Correlations between force plate measures for assessment of balance. Clin Biomech (Bristol, Avon) 2000;15:365–9. doi: 10.1016/s0268-0033(99)00096-0. [DOI] [PubMed] [Google Scholar]
- 16.Corbeil P, Blouin J, Bégin F, Nougier V, Teasdale N. Perturbation of the postural control system induced by muscular fatigue. Gait Posture. 2003;18:92–100. doi: 10.1016/s0966-6362(02)00198-4. [DOI] [PubMed] [Google Scholar]
- 17.Fabre MS, Michaut A, Pousson M. Neuromuscular fatigue development during maximal concentric and isometric knee extensions. J Appl Physiol. 2006;100:780–5. doi: 10.1152/japplphysiol.00737.2005. [DOI] [PubMed] [Google Scholar]


