Abstract
Background:
Cervical cancer is the most common genital cancer and one of the leading causes of death among female population. Fortunately, this cancer is preventable by screening for premalignant lesions but this is rarely provided and hardly utilised. We assessed the knowledge, attitude and utilisation of cervical cancer screening among market women in Sabon Gari, Zaria.
Materials and Methods:
This was a cross-sectional study to evaluate the knowledge, attitude and practice of cervical cancer screening among market women. A total of 260 women were administered with questionnaires which were both self and interviewer administered. These were analysed using SPSS version 11.
Results:
Respondents exhibited a fair knowledge of cervical cancer and cervical cancer screening (43.5%); however, their knowledge of risk factors was poor. There was generally good attitude to cervical cancer screening (80.4%), but their level of practice was low (15.4%).
Conclusions:
There was a fair knowledge of cervical cancer and cervical cancer screening among Nigerian market women in this study, their practice of cervical cancer screening was poor.
Keywords: Cervical, cancer, screening, Zaria
INTRODUCTION
Invasive cervical cancer is the second-most common cancer in women worldwide, but 80% of cases occur in developing countries.1 Although readily detectable in its premalignant stage, cervical cancer remains the second most common cancer in Nigeria2 and fifth in the United Kingdom.2 Among the female population in Nigeria, it is the most common cancer.3,4,5 In 2007, it was reported that 36.59 million women aged ≥15 years in Nigeria are at risk of developing cervical cancer. There are 9922 cases diagnosed annually with 8030 deaths. Human papilloma virus (HPV) prevalence is 24.8%. Incidence of cervical cancer in Nigeria is 250/100,000 women.6
Market women constitute an important group/economic driving force in the country and therefore it is important to know whether knowledge, attitude and practice of cervical cancer screening among female market population is associated with or determined by certain socio-demographic factors.
MATERIALS AND METHODS
This was a descriptive cross-sectional, questionnaire-based study carried out to assess the knowledge, attitude and utilisation of cervical cancer screening among market women, aged 15 years and above, in Sabon Gari Local Government Area of Kaduna State. Only female shop owners/attendants aged 15 years and above in Sabon Gari Main Market who gave their consent were included in this study.
Sample size
Sampling size for the study was calculated based on the formula below.7
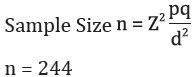
Deliberate over-sampling was done to the tune of 10% to make up for incomplete responses. Therefore, a sample size of 269 was used.
Epitable of EPI INFO 2002 statistical package was used to generate 270 random numbers, assuming that there would be an average of one female of 15 years and above per shop. Questionnaires were administered for data collection. Questions were both closed ended and open ended, providing information about basic demographic data and items sold, pregnancy history and gynaecological history like menstrual history, vaginal discharge, and pain during intercourse, post-coital bleeding, etc. Knowledge about the risk factors of cervical cancer and screening methods, attitude and utilisation of cervical cancer screening were assessed.
Data analysis
Data were analysed using SPSS version 11. The results were summarised into tables, charts and graphs and were subjected to test of statistical significance, where necessary. The knowledge, attitude and practice of cervical cancer screening were scored using the responses from the questions asked, with each correct answer having one point and wrong responses scoring zero. Knowledge score ranged from 0-20, attitude 0-7 and practice 0-4. Knowledge score was categorised thus: Poor (0-9) and Good (10-20). Attitude score categorisation was: Poor (0-3) and Good (4-7); while practice score categorised as Poor (0-2), and Good (≥3).
RESULTS
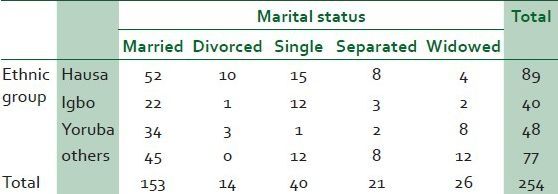
There were 269 questionnaires given, out of which 260 were analysable. Most of the respondents were aged 15-44 years with a mean of 33.2 +/- 11.7 years; there were 135 (51.9%) Christians and 121 (46.5%) Muslims [Table 1]. Most of the respondents were married (60.2%), only 15.7% were single. Major tribe of the respondents is Hausa. This is depicted in Table 2. Most of the respondents have some form of education; only 21.2% have no formal education.
Table 1.
Frequency distribution of age and religion of respondents
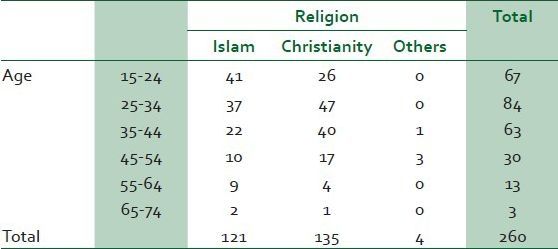
Table 2.
Distribution of respondents marital status and ethnic groups
Most respondents (77.7) had conceived previously. Of this, only 8.8% primiparous and majority of the respondents (66.9%) have heard of cervical cancer. The knowledge score of cervical cancer screening showed that there was a fair knowledge (43.5%) of cervical cancer screening among respondents.
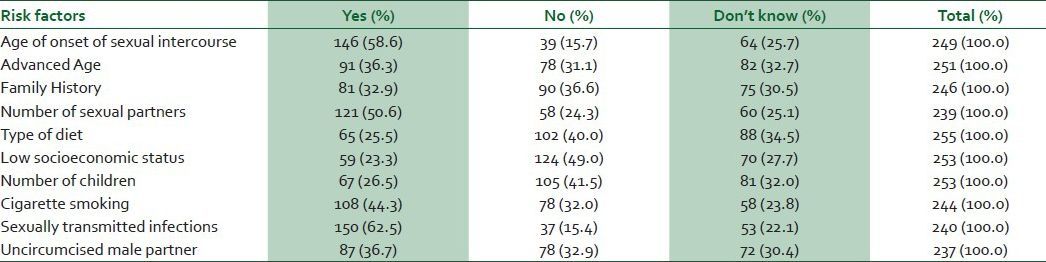
Their knowledge of risk factors for cervical cancer was generally is poor; although 62.5% of them were aware that sexually transmitted infection ware a risk factor. Although their knowledge of symptoms of cervical cancer was fair [Tables 3-5], their attitude towards cervical cancer screening was poor (19.6%). Some patients would go to seek care after noticing symptoms in hospitals (72.1%), traditional healers (10.5%), religious healers (7.4%), while 10.1% would not go anywhere. Better facilities, provision of more female staff at screening centres and offering service at cheaper cost would enhance utilisation of cervical cancer screening [Table 6].
Table 3.
Distribution of respondents by educational status
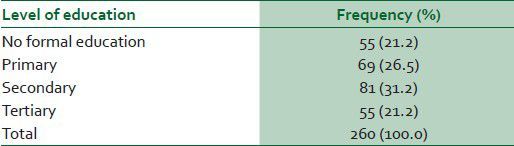
Table 5.
Knowledge of symptoms by the respondents
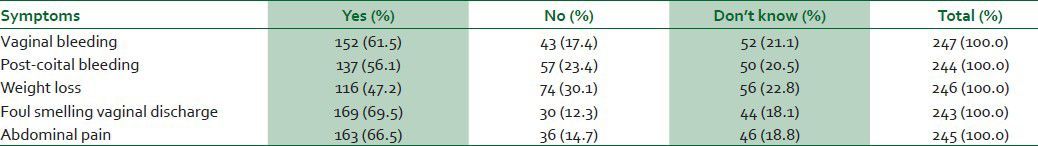
Table 6.
Factors that will enhance utilisation of screening services
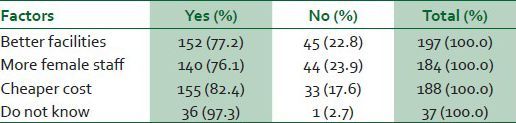
Table 4.
Knowledge of risk factors by the respondents
Many (32.7%) of the women had never heard of cervical cancer screening before, but 32.7% others had been screened for cervical cancer. Of those who had been screened, 80.6% did so voluntarily 68.2% had advised a friend/relation in the past to take up cervical cancer screening. Respondents identified fear of outcome of screening, lack of information and public awareness, lack of health worker request, high cost of screening and lack of personnel at the screening centres as the reasons why people do not patronise cervical screening.
DISCUSSION
Cervical cancer is a preventable non-communicable disease of public health importance. Invasive cervical cancer is the second most common cancer in women worldwide, but 80% of cases occur in developing countries.1 Women often become aware of cervical cancer and screening in the course of their interaction with other each other.8
It is important to note that that only 21.2% lack formal education. This is similar to study done in Ezem in Eastern Nigeria and Ogunbode et al in Ibadan.8,9 Most of the respondents (77.7%) had a history of previous conception. About 8.8% of the respondents that had a history of conception are primiparous. Multiparity is one of the risk factors for developing cervical cancer. Ogunbode et al.,8 recorded most women in their series to be in their third and fourth decades and 48% were either multiparous or grand multiparous. Parity is higher in this study probably because most respondents are of Hausa ethnic group where the practice of early marriage is high and practice of modern contraception is low.
Only 66.9% of respondents ever heard of cervical cancer, and of these 68.6% have heard of cervical cancer screening. This contrasts most reports from Nigerian communities who found that majority of respondents never heard of cervical cancer or cervical cancer screening. Ogunbode et al.,9 carried out a study among market women in Ibadan and only 19.7% were aware of cervical cancer screening. Similarly, in a study in Aba10 only 16% of respondents had knowledge of screening services. However, studies done among hospital workers had similar reports to this study.11,12,13,14 A study among female health workers in Ilorin11 showed the level of awareness to be 69.8%, another study in Nnewi recorded 87%. The high level of awareness in this study may be due to the fact that community health outreach programs usually target market women and of recent a group of American cancer experts visited the market. They discussed issues of cancer prevention, particularly screening. They also offered cervical cancer screening service at the nearby Sabon Gari Comprehensive Health Centre.
Most of the respondents in the present report heard about this from healthcare personnel and few heard from friends, family and media. This is also in contrast to previous reports by Ayinde et al.,15 who found that most respondents get information from radio, family and friends. Most of the respondents (43.5%) had some good knowledge of cervical cancer screening as in a report by Mutyaba et al.,16 in Uganda.
Many respondents opined that better facilities, provision of more female staff and offering service at cheaper cost at the screening centres will enhance utilisation. Adefuye14 reported that lack of physicians’ referrals and ignorance about location of service centers were the two most frequent reasons for failure of utilisation. According to Aboyeji et al.,11 and others,9,13,17,18 the reasons for why women avoided screening included outright rejection, fear of detection of cancer and religious beliefs.
Our finding agrees with earlier studies that reported low level of practice even when the good knowledge is good.9,15,19,20 Studies by Aboyeji et al.,11, Gharoro et al.,20 and Adefuye14 reported other reasons to include ignorance, misconceptions and religious beliefs. These were similar to the reasons adduced in our study.
CONCLUSIONS
The general knowledge of cervical cancer screening was good and the attitude was fair, however, this did not translate to good practice. High cost of screening, lack of female health workers and fear of outcome were some of the reasons responsible for low screening patronage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Holland WW, Stewart S. Nuffield: Nuffield provincial Trust; 1990. Screening in adult women, screening in health care; pp. 155–172. [Google Scholar]
- 2.Goroll AH, May LA, Mulley AG. Primary care medicine: Office evaluation and management of the adult patient. Screening for cervical cancer. 1995:588–590. [Google Scholar]
- 3.Parkin DM, Ferlay J, Hamdi-Cherif M, Sitas F, Thomas JO, Wabinga H, et al., editors. Lyon: IARC Press; 2003. Cancer in Africa: Epidemiology and Prevention. IARC Scientific Publications No. 153. [Google Scholar]
- 4.Rafindadi AH, Ahmed SA. Lagos: Proceedings of the Association of Pathologists in Nigeria Scientific Conference; 2005. Cancer in women and children in Zaria. [Google Scholar]
- 5.Mohammed A, Ahmed SA, Oluwole OP, Avidime S. Malignant tumours of the female genital tract in Zaria, Nigeria: Analysis of 513 cases. Ann Afr Med. 2006:93–96. [Google Scholar]
- 6.Pisani P, Parkin DM, Bray F, Ferley J. Estimates of the worldwide mortality from 25 cancers in 1990. Int J Cancer. 1999;83:870–3. doi: 10.1002/(sici)1097-0215(19991210)83:6<870::aid-ijc35>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 7.Kish L. New York: John Wiley and Sons; 1965. Survey sampling; p. 20. [Google Scholar]
- 8.Ogunbode OO, Ayinde OA. Awareness of cervical cancer and screening in a Nigerian female market population. Ann Afr Med. 2005;4:160–3. [Google Scholar]
- 9.Ezem BU. Awareness and uptake of cervical cancer screening in Owerri, South-Eastern Nigeria. Ann Afr Med. 2007;6:94–8. doi: 10.4103/1596-3519.55727. [DOI] [PubMed] [Google Scholar]
- 10.Feyi-Waboso PA, Kamanu C, Aluka C. Awareness and risk factors for cervical cancer among women in Aba, south-eastern Nigeria. Trop J Obstet Gynae. 2005;22:25–6. [Google Scholar]
- 11.Aboyeji PO. Knowledge, attitude and practice of cervical smear as a screening procedure for cervical cancer in Ilorin, Nigeria. Trop J Obstet Gynae. 2004;21:114–7. [Google Scholar]
- 12.Nwobodo EI, Malami SA. Knowledge and practice of cervical cancer screening among female health workers in Sokoto, North Western Nigeria. Niger Postgrad Med J. 2005;12:255–7. [PubMed] [Google Scholar]
- 13.Udigwe GO. Knowledge, attitude and practice of cervical cancer screening (Pap Smear) among female nurses in Nnewi, South Eastern Nigeria. Nig J Clin Pract. 2006;9:40–3. [PubMed] [Google Scholar]
- 14.Adefuye PO. Knowledge and practice of cervical cancer screening among female professional health workers in a sub-urban district of Nigeria. Nig Med Pract. 2006;50:19–22. [Google Scholar]
- 15.Ayinde OA, Ogunbode OO. Determinants of cervical cancer knowledge and its utilization of screening among a Nigerian female population. Trop J Obstet Gynae. 2005;22:21–4. [Google Scholar]
- 16.Mutyaba T, Mmiro FA, Weiderpass E. Knowledge, attitudes and practices on cervical cancer screening among the medical workers of Mulago Hospital, Uganda. BMC Med Educ. 2006;6:13. doi: 10.1186/1472-6920-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wellensiek N, Moodley M, Moodley J, Nkwanyana N. Knowledge of cervical cancer screening and use of cervical screening facilities among women from various socioeconomic backgrounds in Durban, Kwazulu Natal, South Africa. Int J Gynaecol Cancer. 2002;12:376–82. doi: 10.1046/j.1525-1438.2002.01114.x. [DOI] [PubMed] [Google Scholar]
- 18.McFarland DM. Cervical cancer and Pap Smear screening in Botswana: Knowledge and perceptions. Int Nurs Rev. 2003;50:167–75. doi: 10.1046/j.1466-7657.2003.00195.x. [DOI] [PubMed] [Google Scholar]
- 19.Chukwuali LI. Cervical cancer screening in Enugu, Nigeria. Trop J Obst Gynae. 2003;20:79–81. [Google Scholar]
- 20.Gharoro EP, Ikeanyi EN. An appraisal of the level of awareness and utilization of the Pap smears as a cervical cancer screening test among female health workers in a tertiary institution. Int J Gynaecol Cancer. 2006;16:1063–8. doi: 10.1111/j.1525-1438.2006.00579.x. [DOI] [PubMed] [Google Scholar]


