Abstract
Background:
Supracondylar fractures are the commonest elbow injury in children. Most displaced Supracondylar fractures are manipulated and held with a medial/lateral entry or two lateral Kirschner wires. It was the purpose of this study to investigate the treatment of this injury in this unique patient population.
Materials and Methods:
This study was conducted in the Department of Orthopaedic surgery in M. M. Medical College from July 2005 to July 2010. One hundred seventy patients were recruited from Emergency and outpatient department having closed displaced Supracondylar fractures of humerus in children. They were treated either with medial-lateral pin fixation (n = 85) or with 2-lateral pin fixation (n = 85). All patients were operated under general anaesthesia. All patients were followed for 6 months. Results were analysed using Flynn's criteria.
Statistical Analysis Used:
Chi Square Test. Chi Square calculator was used as a software.
Results:
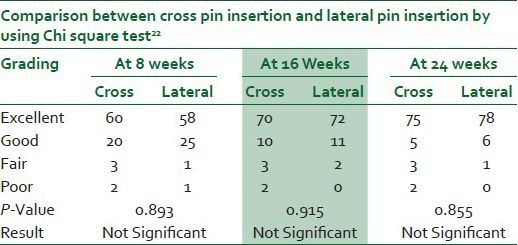
All children achieved union in a mean time of 4 weeks (range: 3-6 weeks). Post-operatively, eight patients (4.70%) got ulnar nerve injury and six (3.52%) patients got pin tract infection. Comparison between two groups such as cross K-wire group (85) and lateral K-wire group (n = 85) by using the Chi Square Test showed that in case of 8 weeks with (P-values = 0.89), in 16 weeks (P = 0.91) and 24 weeks (P = 0.85) with respective excellent, good, fair and poor categories were not found statistically significant.
Conclusion:
The lateral percutaneous pinning technique of displaced Supracondylar fractures of the humerus offers a viable alternative to the crossed pinning group as it offers the same stability without the incipient risk of iatrogenic ulnar nerve injury.
Keywords: Close reduction, chi square test, humerus, percutaneous pinning, supracondylar fracture
INTRODUCTION
Supracondylar fractures of the humerus represent 50-70% of all elbow fracture in children in the first decade of life.1 Current method of treatment of this fracture is based on Gartland classification. Flynn et al., reported the incidence of cubitus varus deformity after treatment was 5%, whereas Arino et al., reported that it was almost 21%, ulnar nerve deficit was found in 15% of patients who were treated with medial and lateral pin as per the report of chai.2,3,4,5 Many different methods are described such as close reduction and long arm cast or slab, Dunlop skin traction, olecranon traction, but all of these methods had large complication rate.1,2,6,7,8,9,10,11,12 The current preferred method of treatment for displaced Supracondylar fracture has been close reduction and percutaneous pin fixation. This method has given excellent results reported by various authors.10,11,12,13,14,15 Thus, I conducted this retrospective study to compare whether lateral pin construct, if placed properly, can provide the same stability like medial and lateral pin fixation, at the same time avoiding the possibility of iatrogenic ulnar nerve palsy.16,17,18
MATERIALS AND METHODS
This retrospective study was carried out at Orthopaedics Department of M. M. Medical College from July 2005 to July 2010. Institutional medical ethics committee approved it. A written informed consent was obtained from all the patients (by their parents).19,20 In this study, 170 children with Grade III close Supracondylar fractures of humerus were included. The patients were aged between 1.5 years and 13 years with the mean age of 7.76 years. The time of operation ranges from the 1st day of injury to the 8th day of injury with the mean time of operation being 4.6 days. The patients were evaluated as described by Flynn and the results compared with the contra lateral normal elbow.2 Under general anaesthesia, using c-arm fluoroscopy closed reductions were done.21 When satisfactory reduction had been achieved, then fixations were done by K-wires of 1.5 or 2.0 mm size and well-padded above-elbow posterior back-slabs were applied. [Figures 1a-c] [Figures 2a-c]. The patients were carefully observed for 12-72 hours (average 58 hours) and then discharged. The above-elbow plaster of paris (POP) back slabs were kept for two to three weeks and the pins and slab were removed in the outpatient (OPD) clinic. Elbow Range of motion (ROMS) was started after removing the POP back slab. The follow-ups were arranged as follows: The first follow-up on the 7th day to inspect the wound; the second follow-up on the second week for wound inspection or suture removal and to see the pin configuration. It is a retrospective study. Within 2-3 weeks, x-rays were taken to see the callus formation; if callus is formed, then we remove the pop and pins and to start physiotherapy; the third follow-up on the 4th week and the fourth follow-up on the 8th week post-operatively to see the ROM and carrying angle of the elbow, and the final follow-up on the 6 months post-operatively to see the final result of the study.
Figure 1.
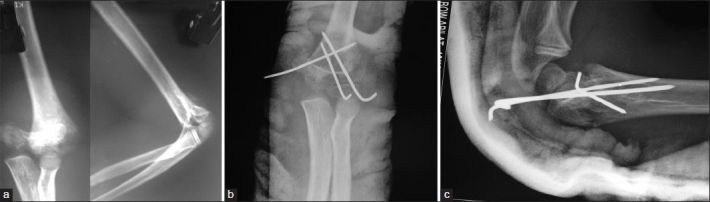
(a) Pre-operative A-P and Lateral radiographs showing Supracondylar fracture of humerus of 4-year-old child, (b) Post-operative anteroposterior radiographs of Supracondylar fracture of humerus showing with Crossed K-wire fixation, (c) Post-operative Lateral radiographs of Supracondylar fracture of humerus showing with crossed K-wire fixation
Figure 2.

(a) Pre-operative A-P radiograph showing Supracondylar fracture of humerus of 6-year-old child, (b) Pre-operative Lateral radiograph showing Supracondylar fracture of humerus of 6-year-old child, (c) Post-operative A-P and Lateral radiographs of Supracondylar fracture of humerus showing with 2 lateral K-wire fixation
Ethics
The protocol was approved by Institutional ethics committee and thus meets the standards of the Declaration of Helsinki in its revised version of 1975 and amendments made to it in 1983, 1989 and 1996 (JAMA 1997;277:925-6).
RESULTS
There were 170 children in this study, 97 children were male and 73 children were females. The children were aged 1.5-13 years. There were 103 left-sided and 67 right-sided fractures. Among 170 children, 102 children had injury during playing, 44 children had met with a road traffic accident and 24 had a fall from a height. All were closed fractures. The extension types were 158 (92.94%) and flexion types 12 (7.05%). 85 (50%) cases were treated by two lateral parallel K-wires and 85 (50%) by cross K-wires. Preoperatively, six cases had nerve injuries (median nerve three, ulnar nerve two and radial nerve one) and there were no cases of vascular injuries. Post-operatively, eight patients (4.70%) got ulnar nerve injury in the crossed K-wire group (n = 85). Six (3.52%) patients got pin tract infection, four in the crossed K-wire group (n = 85), and two in the lateral K-wire group (n = 85), which were superficial and healed after removing pins and oral antibiotic administration. All nerve injuries recovered within 3.5 months post-operatively. There were no ulnar nerve injuries in the patient treated by inserting only lateral two K-wires. Callus formations were seen in all patients at the 2-3 weeks post-operatively before removing the K-wires. The fractures united in all cases at the 4th week post-operatively. Results were analysed using Flynn's criteria.2 All patients were followed at 8th week, 16th week and the 24th week, postoperatively. However, comparison between two groups showed that all categories such as 8 weeks, 16 weeks and 24 weeks with respective excellent, good, fair and poor were not found statistically significant. In cases of ulnar nerve injuries and pin tract infections also not found statistically significant22 [Table 1]. All patients achieved complete radiographic healing at a mean of 4 weeks (range: 3-6 weeks). In a subjective measure of outcome at follow-up, in the crossed K-wire group (n = 85), the results were excellent in 88.23% and good in 5.88% patients, and in the lateral K-wire group, the results were excellent in 91.75% and good in 7.05% patients. No patients or parents reported their out-come as not satisfied. At follow-up, all patients went on to osseous union and regained a full range of movement after rehabilitation. During this study, complications like vascular injury, compartment syndrome, myositis ossifications, significant mal-union and non-union were not red. Distal pin migration was seen in five (2.94%) patients, loss of reduction was seen in six (3.52%), which was not significant and did not require re-reduction and re-pinning. Comparison between two groups such as cross K-wire group (85) and lateral K-wire group (n = 85) by using the Chi Square Test showed that in case of 8 weeks with (P-values = 0.89), in 16 weeks (P = 0.91) and 24 weeks (P = 0.85) with respective excellent, good, fair and poor categories were not found statistically significant. The mean Baumann angle loss in the medial-lateral pin fixation group and the 2-lateral pin fixation group was 5.96Ο and 5.30Ο, respectively. Analyses of the Baumann angle loss showed no significant difference between medial lateral pin fixation and 2-lateral pin fixation.
Table 1.
Results of the evaluation of the 170 patients according to the Flynn criteria
DISCUSSION
Management of displaced extension type III Supracondylar fracture of humerus treated by close reduction and percutaneous pin fixation has consistently given satisfactory result compared to other method of treatment. However, controversy persists regarding the adequate pin fixation technique comparing medio-lateral and lateral pin fixation. In this study, not much difference between both fixation methods in terms of stability was found but there is an evidence of iatrogenic ulnar nerve injury (4.70%) in medio-lateral pin fixation group. Iatrogenic ulnar nerve injuries in this study were most likely neuropraxia (Sunderland type 1) since all of them recovered without exploration or repair within 3.5 months post-operatively. Complete transaction of the nerve or neurotmesis was not seen in this study. In cases of ulnar nerve injuries and pin tract infections also not found statistically significant.22 The medio-lateral pin fixation method supposed to have the advantage of better fracture stability, although iatrogenic ulnar injury can occur with this technique. Pin fixation from lateral side has the advantage of avoiding ulnar nerve injury but this construct has been thought to be biomechanically less stable. Lee SS et al., and Ziouts et al., reported that medial and lateral entry provides greater torsional rigidity than lateral entry pin fixation does.19,20 The total strength of this construct is not only related to pin entry but mainly to divergence of the pins in different column and number of pins. The greater strength seen with the divergence of the pins was related to the location of the interaction of the two pins and the fact that the greater amount of divergence between the two pins allow for some purchase in the medial and lateral column.19,20 There are some authors who advocated the use of the third wire to prevent the displacement of the distal fragment.23,24 The use of a third pin requires the medial pin to enter the joint and thus increases the risk of joint penetration and infection. The use of two pins laterally was preferred to decrease the risk of infection. Skaggs et al.,13 found no ulnar nerve palsy and no reduction was lost in 124 children managed with only lateral-entry pins. In an other study of Skaggs et al.,14 of 204 children who had a Gartland type-3 fracture, 51 were treated with lateral pins only and 153 were treated with crossed pins. The configuration of the pins did not affect the Baumann's angle in Gartland type 3 fractures. Reynolds and Jackson25 found no differences in results between the two different methods. The most common complication in the treatment of closed reduction and percutaneous pinning of displaced Supracondylar fractures of the humerus is iatrogenic ulnar nerve palsy with the use of medial pin.18,26,27,28,29 The rate of ulnar nerve injuries varies in different studies. Lyons et al.,29 have reported this number as 6%, Royce et al.,27 as 3%, Agus et al.,28 as 58%. It is found that postoperative nerve palsies after percutaneous pinning was with direct injury to the nerve, not after manipulation of closed reduction.11,26,27,30 Skaggs et al.,14 noted the incidence of ulnar nerve injury as 4% in patients whom the pins were applied without hyper flexion of the elbow and as 15% in whom the medial pin was applied with the elbow hyperflexed. Different techniques are performed to decrease the rate of ulnar nerve injury. It is also showed that lateral-pins decrease the rate of ulnar nerve injury when compared with medial-pins. In the present study, there was no incidence of ulnar nerve injury where pinning was done from the lateral side; and I did not find any difference in bone healing and stability between lateral-pin insertion and cross-pin insertion as the same treatment protocol was followed for both the groups. Skaggs found that the use of lateral-entry pins alone was effective for even the most unstable Supracondylar humeral fractures and they saw no iatrogenic ulnar nerve injuries, and no reduction was lost.13,14 In the present study, iatrogenic nerve injury was seen in eight patients (4.70%) where pinning was done from cross pin insertion. Although most of the ulnar nerve injuries recover spontaneously between 4 months and 6 months, permanent damage has been reported in the literature.27,31 Lyons et al.,18 observed spontaneous functional recovery after the removal of medial pin. However, Rasool31 advocated the early exploration of the nerve. Clawing of the fingers may occur rarely after ulnar nerve injuries. Pathological electromyographic measurements can be detected in most of ulnar nerve injuries during the early postoperative period. In this study, the results of both lateral and cross pin insertion groups at 8th post-operative week showed excellent results in around 70% of patients. At the final follow-up, these excellent results were seen in around 90% of the cases. In post-operative period, physiotherapy plays a significant role in increasing the ROM of the elbow joint. Those patients who had good or fair results were having severe soft tissue injuries or repeated closed reduction. Khan obtained 88% excellent, 4% good and 4% poor results in his study.32 Tiwari observed 88% satisfactory results, among which 42% were excellent, in his series of late-presenting Supracondylar fractures of humerus in children.33 These two studies are comparable to our study. Cubitus varus deformity is the most common problem seen after the treatment of Supracondylar fractures. The cause of the deformity is coronal rotation, or tilting of the distal fragment.34 Some investigators believed that varus deformity is due to epiphyseal growth disturbance or rotation of the distal fragment.35 Smith suggested that residual medial tilt after reduction is the most important factor in varus angulations, with isolated rotational deformities being corrected by compensatory rotation at the shoulder.36 This concept has become popular in understanding the sequel of alteration in carrying angle.37 In this series, six patients (3.52%) had nerve injury preoperatively, out of which three had median, two ulnar and one radial. Eight patients got ulnar nerve injuries post-operatively, which is 4.70% of the total number. All the nerve injuries recovered within 14 weeks postoperatively. The incidence of postoperative has been estimated to range from 5% to 19%.38 Culp recommends that initial observation and supportive therapy for neural injury associated with a closed, displaced, Supracondylar fracture of the humerus; and that if there is no clinical or electromyography evidence of return of neural function at five months after injury, exploration and neurolysis should be performed. If the nerve is in continuity, the prognosis after neurolysis is excellent.39 In my study, six (3.52%) patients developed pin-tract infections, which were superficial and healed after removing pins and administration of oral antibiotics. No deep infection or septic arthritis was found. Pirone found superficial pin-tract infection in 2% of cases with no deep infection and septic arthritis.40 In the present series, the distal pin migration was seen in five (2.94%) patients and loss of reduction in six (3.52%), which were not significant and so required no re-reduction and re-pinning. Gordon observed pin-tract migration in 6% of cases and Lee noticed the loss of reduction in 7% of cases.12,19 Lee et al.,41 stated that the lateral pinning technique was found to be more beneficial than the medial and lateral crossed pinning technique for Supracondylar fractures of the humerus in children, on the basis of current evidences. However, the results were sensitive to the data of ulnar nerve injury. Avoiding the worst clinical scenario (permanent ulnar nerve palsy) might be more important and affordable than obtaining favourable clinical results (stable fixation) at the potential cost of disastrous complications. Dua et al.,42 proposed that closed reduction and crossed pinning of displaced Supracondylar fractures of humerus in children is a safe and effective method even with delayed presentation. Erpelding et al.,43 stated that Open treatment of distal humeral fractures with an extensor mechanism-on approach results in excellent healing, a mean elbow flexion-extension arc exceeding 100°, and maintenance of 90% of elbow extension strength compared with that of the contra lateral, normal elbow. Woratanara et al.,44 stated that lateral pinning is preferable to cross pinning for fixation of pediatric Supracondylar humerus fractures as a result of decreased risk of ulnar nerve injury. The main goal of the treatment of displaced paediatric Supracondylar humerus fractures is to achieve an anatomic reduction. This reduction should be supported by a fixation with a good stability and less morbidity. When all these are taken into consideration, we believe that closed reduction and percutaneous lateral pinning is an efficient, reliable and safe method.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Herring JA, editor. Tachdjian's Pediatric Orthopaedics. 3rd ed. Vol. 3. Philadelphia: W.B. Saunders; 2002. Fracture about the elbow; pp. 2139–221. [Google Scholar]
- 2.Flynn JC, Mattews JG, Benoit RL. Blind pinning of displaced Supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am. 1974;56:263–72. [PubMed] [Google Scholar]
- 3.Arino VL, Llurch EE, Ramriez AM, Ferrer J, Rodriguez L, Baixauli F. Percutaneous fixation of Supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1977;59:914–6. [PubMed] [Google Scholar]
- 4.Chai KK. Master thesis. University of Malaya; 2000. A prospective study on Supracondylar fractures of the humerus in children: Comparing the results of closed manipulation and plaster cast with close manipulation and percutaneous cross K wiring for the treatment of displaced fractures. [Google Scholar]
- 5.Wilkins KE. Supracondylar fracture of the distal humerus. In: Rockwood CA, Wilkins KE, Beaty JH, editors. Fractures in children. 4th ed. Vol. 3. Philadelphia: Lippincott-Raven; 1996. pp. 669–752. [Google Scholar]
- 6.Dogde HS. Displaced supracondylar fractures of humerus in children – Treatment by Dunlop's traction. J Bone Joint Surg Am. 1972;54:1408–18. [PubMed] [Google Scholar]
- 7.Dunlop J. Transcondylar fractures of the humerus in childhood. J Bone Joint Surg. 1939;21:59–73. [Google Scholar]
- 8.Worlock PH, Colton C. Severely displaced Supracondylar fractures of humerus in children: A simple method of treatment. J Pediatr Orthop. 1987;7:49–53. doi: 10.1097/01241398-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Smith FM. Kirschner's wire traction in elbow and upper arm injuries. Am J Surg. 1947;74:700–87. doi: 10.1016/0002-9610(47)90235-3. [DOI] [PubMed] [Google Scholar]
- 10.Mazda K, Boggione C, Fittoussi F, Pemecot GF. Systemic pinning of displaced extension-type supracondylar fractures of humerus in children. A prospective study of 116 consecutive patients. J Bone Joint Surg Br. 2001;83:888–93. doi: 10.1302/0301-620x.83b6.11544. [DOI] [PubMed] [Google Scholar]
- 11.Shannon FJ, Mohan P, Chacko J, D’Souza LG. ‘Dorgan's’ Percutaneous lateral cross-wiring of Supracondylar fractures of humerus in children. J Pediatr Orthop. 2004;24:376–9. doi: 10.1097/00004694-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Gordon JE, Patton CM, Luhmann SJ, Bassett GS, Schoenecker PL. Fracture stability after pinning of displaced Supracondylar fractures of humerus in children. J Pediatr Orthop. 2001;21:313–8. [PubMed] [Google Scholar]
- 13.Skaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of Supracondylar fractures of humerus in children. J Bone Joint Surg Am. 2004;86:702–7. doi: 10.2106/00004623-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of Supracondylar fractures of humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83:735–40. [PubMed] [Google Scholar]
- 15.Fowles JV, Kassab MT. Displaced Supracondylar fractures of the elbow in children. A report on the fixation of extension and fixation fractures by two lateral percutaneous pins. J Bone Joint Surg Br. 1974;56:490–500. [PubMed] [Google Scholar]
- 16.Belhan O, Karakurt L, Ozdemir H, Yilmaz E, Kaya M, Serin E, et al. Dynamic of the ulnar nerve after percutaneous pinning of Supracondylar humerus fractures in children. J Pediatr Orthop B. 2009;18:29–33. doi: 10.1097/BPB.0b013e32831960fa. [DOI] [PubMed] [Google Scholar]
- 17.Brown IC, Zinar DM. Traumatic and iatrogenic neurological complications after Supracondylar humerus fractures in children. J Pediatr Orthop. 1995;15:440–3. doi: 10.1097/01241398-199507000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Lyons JP, Ashley E, Hoffer MM. Ulnar nerve palsies after percutaneous cross-pinning of Supracondylar fractures in children's elbows. J Pediatr Orthop. 1998;18:43–5. [PubMed] [Google Scholar]
- 19.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced paediatric Supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22:440–3. [PubMed] [Google Scholar]
- 20.Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix Supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76:253–6. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Bloom T, Robertson C, Mahar A, Pring M, Newton PO. Hollywood, FL: Read at the Annual Meeting of the Pediatric Orthopaedic society of North America; 2007. May 23-26, Comparison of Supracondylar humeral fracture is not anatomically reduced. [Google Scholar]
- 22.Nikulin MS. Chi-squared test for normality. Proceedings of the International Vilnius Conference on Probability Theory and Mathematical. Statistics. 1973;2:119–22. [Google Scholar]
- 23.Eralp L, Demirhan M, Dikici F, Onen M. Radiologic comparison of crossed K-wires and three K-wires configurations in the treatment of displaced Supracondylar humerus fractures. Acta Orthop Traumatol Turc. 2000;34:278–83. [Google Scholar]
- 24.Karapinar L, Ozturk H, Altay T, Kose B. Closed reduction and percutaneous pinning with three Kirschner wires in children with type III displaced Supracondylar fractures of the humerus. Acta Orthop Traumatol Turc. 2005;39:23–9. [PubMed] [Google Scholar]
- 25.Reynolds RA, Jackson H. Concept of treatment in Supracondylar humeral fractures. Injury. 2005;36(Suppl 1):A51–6. doi: 10.1016/j.injury.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Devnani AS. Late presentation of Supracondylar fracture of the humerus in Children. Clin Orthop Relat Res. 2005:36–41. doi: 10.1097/01.blo.0000152439.43810.11. [DOI] [PubMed] [Google Scholar]
- 27.Royce RO, Dutkowsky JP, Kasser JR, Rand FR. Neurologic complications after K-wire fixation of Supracondylar humerus fractures in children. J Pediatr Orthop. 1991;11:191–4. doi: 10.1097/01241398-199103000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Agus H, Kelenderer O, Kayali C. Closed reduction and percutaneous pinning results in children with Supracondylar humerus fractures. Acta Orthop Traumatol Turc. 1999;33:18–22. [Google Scholar]
- 29.Ippolito E, Caterini R, Scola E. Supracondylar fractures of the humerus in children. Analysis at maturity of fifty-three patients treated conservatively. J Bone Joint Surg Am. 1986;68:333–44. [PubMed] [Google Scholar]
- 30.Green DW, Widmann RF, Frank JS, Gardner MJ. Low incidence of ulnar nerve injury with crossed pin placement for paediatric Supracondylar humerus fractures using a mini-open technique. J Orthop Trauma. 2005;19:158–63. doi: 10.1097/00005131-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 31.Rasool MN. Ulnar nerve injury after K-wire fixation of Supracondylar humerus fractures in children. J Pediatr Orthop. 1998;18:686–90. doi: 10.1097/00004694-199809000-00027. [DOI] [PubMed] [Google Scholar]
- 32.Khan AQ, Goel S, Abbas M, Sherwani MK. Percutaneous Kwiring for Gartland type III Supracondylar humerus fractures in children. Saudi Med J. 2007;28:603–6. [PubMed] [Google Scholar]
- 33.Tiwari A, Kanojia RK, Kapoor SK. Surgical management for late presentation of Supracondylar humeral fracture in children. J Orthop Surg (Hong Kong) 2007;15:177–82. doi: 10.1177/230949900701500211. [DOI] [PubMed] [Google Scholar]
- 34.Kallio PE, Foster BK, Paterson DC. Difficult Supracondylar elbow fractures in children: Analysis of percutaneous pinning technique. J Pediatr Orthop. 1992;12:11–5. [PubMed] [Google Scholar]
- 35.Smith L. Deformity following Supracondylar fractures of the humerus. J Bone Joint Surg Am. 1960;42:235–52. [PubMed] [Google Scholar]
- 36.Smith L. Supracondylar fractures of the humerus treated by direct observation. Clin Orthop Relat Res. 1967;50:37–42. [PubMed] [Google Scholar]
- 37.Mann TS. Prognosis in supracondylar fractures. J Bone Joint Surg Br. 1963;45:516–22. [PubMed] [Google Scholar]
- 38.McGraw JJ, Akbarnia BA, Hanel DP, Keppler L, Burdge RE. Neurological complications resulting from Supracondylar fractures of the humerus in children. J Pediatr Orthop. 1986;6:647–50. doi: 10.1097/01241398-198611000-00001. [DOI] [PubMed] [Google Scholar]
- 39.Culp RW, Osterman AL, Davidson RS, Skirven T, Bora FW., Jr Neural injuries associated with Supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1990;72:1211–5. [PubMed] [Google Scholar]
- 40.Pirone AM, Graham HK, Krajbich JI. Management of displaced extension-type Supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1988;70:641–50. [PubMed] [Google Scholar]
- 41.Lee KM, Chung CY, Gwon DK, Sung KH, Kim TW, Choi IH, et al. Medial and lateral crossed pinning versus lateral pinning for Supracondylar fractures of the humerus in children: Decision analysis. J Pediatr Orthop. 2012;32:131–8. doi: 10.1097/BPO.0b013e3182471931. [DOI] [PubMed] [Google Scholar]
- 42.Dua A, Eachempati K, Malhotra R, Sharma L, Gidaganti M. Closed reduction and percutaneous pinning of displaced Supracondylar fractures of humerus in children with delayed presentation. Chin J Traumatol. 2011;14:14–9. [PubMed] [Google Scholar]
- 43.Erpelding JM, Mailander A, High R, Mormino MA, Fehringer EV. Outcome following distal humeral fracture fixation with an extensor mechanism-on approach. J Bone Joint Surg Am. 2012;94:548–53. doi: 10.2106/JBJS.J.01785. [DOI] [PubMed] [Google Scholar]
- 44.Woratanarat P, Angsanuntsukh C, Rattanasiri S, Attia J, Woratanarat T, Thakkinstian A. Meta-analysis of pinning in Supracondylar fracture of the humerus in children. J Orthop Trauma. 2012;26:48–53. doi: 10.1097/BOT.0b013e3182143de0. [DOI] [PubMed] [Google Scholar]


