Abstract
Background:
No organized school oral health program is existent in India.
Aim:
The aim of this study is to test the feasibility and efficacy of an economical school oral health promotional intervention with educational and preventive components.
Settings and Design:
School oral health promotional intervention carried out in one of the randomly selected school and evaluated through short duration prospective model.
Materials and Methods:
A total of 100 children with an age range of 10-12 years with no previous history of dental intervention were enrolled. Interventions comprised of oral health education (delivered through lecture and demonstrations by an undergraduate dental student) and topical antibacterial therapy (fluoride varnish and povidone iodine). Outcomes consisted of Knowledge and practices (KAP) regarding oral health, clinical oral health related parameters such as plaque index (PI), gingival index (GI) and caries activity as per Modified Snyder's test. These were reported at baseline, 3 weeks and 6 months follow-up examination by a calibrated examiner.
Statistical Analysis:
McNemar Bowker's test, Student's t-test, Pearson Chi-square tests were used.
Results:
Highly significant (P < 0.001) improvements in KAP scores, PI scores, GI scores and caries activity were reported at 3 weeks and 6 months follow-up examination.
Conclusion:
This small economical school oral health program positively influenced oral health related practices and parameters of oral health such as oral cleanliness, gingival health and caries activity.
Keywords: Fluoride varnish, oral health education, preventive oral health program, school oral health program, topical povidone iodine
Introduction
Although dental caries prevalence and severity has shown a tremendous decline world-wide in past decades, oral health in many developing countries including India is still in compromising state.[1,2,3] A previous study has reported prevalence of as high as 92.11% among 9 year old and a mean dynamical mean field theory of 4.61 ± 3.14, higher than World Health Organization (WHO) goal for Healthy people (2000).[3] This worrisome prevalence and severity was attributed to lack of use of fluoride toothpaste (80%), lack of knowledge about the etiology of dental caries (98%) and ≥5 sugar exposures/day (30%).[3] To add to the problem, the community oral health care delivery services in urban India are not sufficiently organized to successfully deliver curative services to this huge burden of oral diseases.
Oral health education aims to promote oral health principally by providing information to improve awareness leading to adoption of a healthier life-style, positive attitudes and good oral health behavior. Improvement in knowledge as a result of oral health education program has been known to influence not only self-reported oral health related practices and behavior in a favorable way, but also improve clinical parameters of oral health such as oral hygiene, gingival health and dental caries.[4,5] These implications are not only short term but long-term retention of favorable oral health related behaviors and maintenance of improved oral health as well has been reported.[6]
Favorable health related behaviors are best established in pre-adolescent[7,8] and adolescent[9,10] age group and once established offer a promise to be sustained during adulthood as well. Further, schools provide an ideal setting to deliver oral health education in combination with preventive services to achieve oral health promotion. World-wide, schools have been recognized as a perfect set up to deliver oral health education and preventive services in an efficient and effective way.[11,12,13] Moreover, school based approach has been reported to be more efficient in delivering preventive and curative services than community based approach.[14]
Prevalent gingivitis and dental caries characterize the poor oral health of Indian school children.[3,15] In spite of this no oral health promotional program is existent. Policy makers need a cost-effective efficient school based oral health promotional program (SOHPP), but evidence to endorse any school based oral health intervention is scarce in India. Keeping this in mind, the present cluster trial was conducted to evaluate the effectiveness of an oral health promotional program comprising of educational and preventive arms on oral health related knowledge, behavior (practices) and oral health status such as oral hygiene, gingival health and caries activity.
Null hypothesis
There would be no difference in knowledge, behavior (practices) and oral health status such as oral hygiene, gingival health and caries activity before and after conducting SOHPP in the study population.
Materials and Methods
Study location
The present study was conducted in Chandigarh located in Northern India and spread in an area of 114 km2 , with community water supply fluoridated at 0.3 ppm. The total population of the city is 900,635 Census of India, 2011.
Sample selection and recruitment
The sample consisted of 100 children aged 10-12 years studying in a randomly selected private high school out of school list (n = 18, private high schools in Chandigarh). Principal of school was contacted by the investigator through written communication explaining the importance of good oral health and emphasizing the need for school based oral health promotional intervention. Permission was sought to allow investigator (AG) to carry out oral health promotional intervention program. A similar letter explaining the condition and seeking consent was circulated among parents/guardians. Cohorts of children born in year 2000-2002 attending the selected school in academic year 2011-12 were included in the study. Schools for children with special health care needs were excluded.
Inclusion and exclusion criteria
Children aged 10-12 years with no history of previous dental intervention either preventive or curative were enrolled. History of antibiotic intake in past 2 weeks and ongoing orthodontic treatment resulted in exclusion from trial.
Furthermore, absenteeism on the day of examination and failure to obtain written informed consent from parents resulted in exclusion from the study.
Evaluation parameters
Knowledge, attitude and practices regarding oral health
Oral hygiene
Gingival health
Dental caries activity.
Time points of observation
Evaluations were carried out at baseline, 3 weeks and 6 months post-intervention.
Methods of evaluation
Knowledge and practices
A questionnaire was drafted by AG and face validation was carried out by four experienced pediatric dentists. The questionnaire was pilot tested as well. It comprised of 18 items; 12 knowledge and 6 practice questions. The questionnaire was administered by AG. The outcome was reported as correct/incorrect response to knowledge questions and favorable/unfavorable response to practice questions. Positive outcome was defined as correct response to knowledge and favorable response to practice questions.
Oral hygiene
Silness and Loe Plaque Index (PI); 1964 (PI)[16] was used for recording dental plaque as a measure of oral hygiene. Prior to recording dental plaque, the child was asked to rinse thoroughly with plain water. If no plaque was detected visibly on a particular surface, a probe tip was run across the surface to ascertain its presence/absence. The mean PI was calculated and on the basis of mean scores, the oral hygiene was described as excellent (0), good (0.1-1.0), fair (1.1-2.0) or poor (2.1-3.0).
Gingival health
Gingival health status was recorded on 6 index teeth viz. 16, 12, 24, 36, 32 and 44 using Loe and Sillness Index; 1963 (Gingival index [GI]).[17] For recording GI, facial gingiva around each tooth was divided into three units such as distal, middle and mesial while lingual gingiva was recorded as a single unit. Thus, GI was recorded for four gingival units/tooth. The recording was done after gently drying the teeth and gingivae with chip blower. Initially the blunt probe tip was gently pressed all around free gingival margin to check for spontaneous bleeding. If no bleeding point was observed, the blunt probe tip being held parallel to long axis of the tooth was walked in the gingival sulcus all around the tooth to check for bleeding on slight provocation. The firm pen grasp was used to probe the gingival sulcus with due care being taken to avoid traumatizing gingival tissues. The mean GI was calculated and on the basis of mean scores obtained gingival health was graded as mild gingivitis (mean GI = 0.0-1.0), moderate gingivitis (mean GI = 1.1-2.0) and severe gingivitis (mean GI = 2.1-3.0).
Caries activity
Modified Snyder's test was used to assess caries activity at various time points of observation.
Preparation of test media
The preparation of Snyder medium was done using commercially available B-C-G dextrose agar (Snyder Test Agar: HiMedia Laboratories Pvt Ltd, Mumbai). A total of 65 g of the snyder test agar was suspended in 1 L of distilled water. The mixture was boiled to dissolve the powder completely.
Each snyder test-tube was dispensed with 10 mL of media and autoclaved at 121°C at 15 lbs for 15 min. The contents of the tube were allowed to solidify before storage in the refrigerator. The snyder tubes were carried to school in controlled storage temperature in ice boxes.
Salivary sample collection
Prior to saliva collection, snyder tubes were rolled between hands to bring the temperature close to body temperature. Following this, the tube was uncapped and the open-end was momentarily exposed to flame to sterilize the tube opening and prevent any untoward sample contamination. Unstimulated saliva was collected by making the subject to drool directly into the tube in sufficient amount to just cover the superior surface of the medium. Samples were collected around 11.00 am on all successive days.
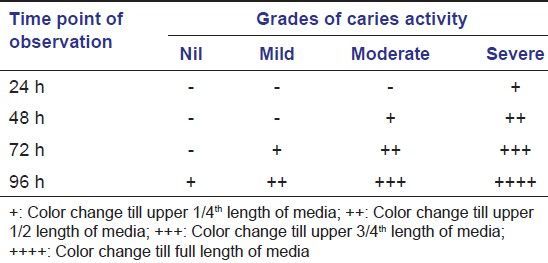
Incubation and evaluation of media
Following saliva collection, the tubes were incubated at 37°C. Color changes from blue-green to yellow, if any, were noted every 24 h, 48 h, 72 h and 96 h according to the method described by Alban 1970. The caries activity was divided into 4 categories based on color changes obtained in the snyder tube in 96 h [Table 1].
Table 1.
Interpretation of caries activity on the basis of modified Snyder test results†
Study settings and examination
The present study was carried out in school premises. Children were examined by AG in well-lit class rooms in sufficient natural light. A mirror and probe were used for examination. Children were made to rinse with plain water prior to the examination. PI was recorded prior to recording GI. Plaque was not disclosed for recording PI.
Schools were informed of date of baseline examination in advance, but, this information was not dispersed among subjects.
Training and calibration of examiner
The examiner (AG) was calibrated by training sessions by an experienced faculty (ISB) which were carried out during the routine patient evaluations at Department of Community Dentistry at Dr. HSJ Institute of Dental Sciences, Chandigarh, India. K > 0.6 for inter-examiner agreement between AG and gold standard examiner was a prerequisite to let AG start with the study.
Oral health promotional intervention
It was conducted after baseline evaluation. The interventional program comprised of educational and preventive arms.
Oral health educational program
It comprised of information about etiology and prevention of dental caries and gingivitis. The school children were taught about intelligent use of sugars (restriction of sugar <3 times/day) and use of fluoride tooth paste. Effective removal of dental plaque was taught and Fone's method of brushing was demonstrated.
Mode of delivery of oral health educational program
The educational program was delivered by first author (AG) via Microsoft powerpoint® presentation (Microsoft Corp, 2007, Redmond, Washington, USA) and lecture. Brushing technique was demonstrated using acrylic models and toothbrush.
Preventive services
These comprised of topical application of 0.5 ml povidone iodine (10%) and 0.5 ml of sodium fluoride varnish with a concentration of 22,600 ppm (Fluoritop-SR® ICPA, Gujarat, India). Povidone iodine applications were done at baseline, 2 months, 4 months and 6 months.
Methods of record keeping
Information about subject's demographic characteristics, outcome on KAP questionnaire, PI, GI and caries activity was recorded on preprinted proformas by AG.
Statistical analysis
The collected data were first fed into Microsoft excel (Microsoft Corp, 2007, Redmond, Washington, USA) and then imported to the statistical package for the social sciences (SPSS) package version 17.0 (SPSS Inc., Chicago, IL, USA). Descriptive data were expressed as number (%) for qualitative variables and mean ± standard deviation for quantitative variables. For quantitative variables following normal distribution as depicted by results of Kolmogorov-Smirnov test, comparative analysis of variables at baseline versus follow-up examination was carried out using Student's t-test. For comparative evaluation of qualitative variables at same time points of observation, McNemar-Bowker test was used. Pearson Chi-square was used to assess correlation among dependent variables of interest. Significance was set at a P ≤ 0.05.
Results
Basic demographics
Attrition of sample
A total of 3/100 (3%) children were lost to follow-up during the final examination at 6 months because of fitness reasons.
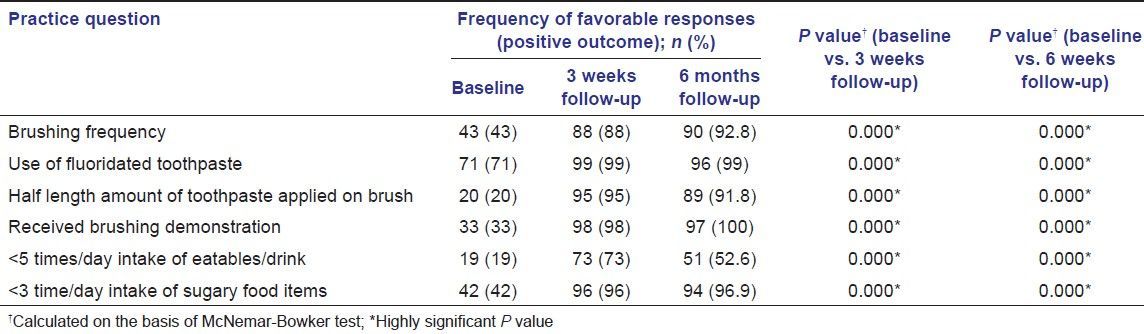
Outcome to KAP questionnaire
A highly significant (P < 0.001; McNemar-Bowker Test) improvement in positive outcome for KAP questionnaire was reported at 3 week follow-up. This change was reported to be retained at 6 months follow-up (P < 0.001; McNemar-Bowker Test) [Tables 2 and 3].
Table 2.
Frequency of positive outcome to knowledge questionnaire
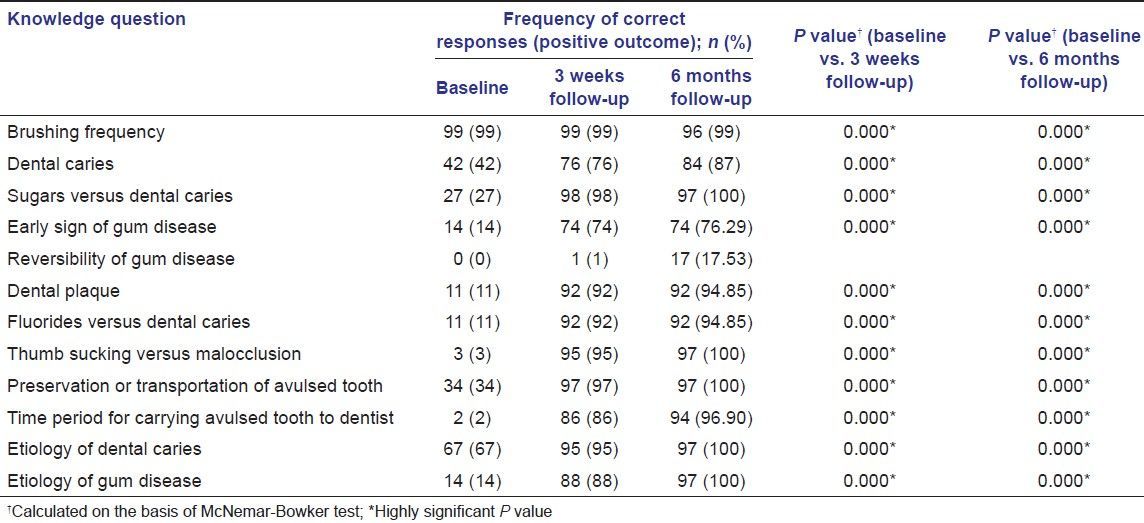
Table 3.
Frequency of positive outcome to knowledge and practice questionnaire
Oral hygiene status (PI scores); gingival health (GI scores) [Tables 4 and 5]
Table 4.
Plaque index and gingival index scores at various time points of observation
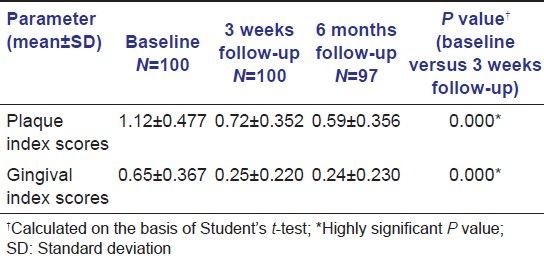
Table 5.
Distribution of subjects with different grades of oral hygiene and gingivitis at various time points of observation
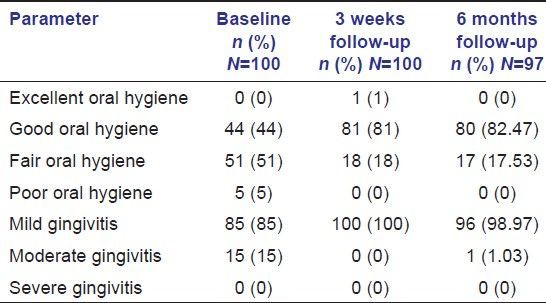
Highly significant reduction in PI and GI scores was reported (P < 0.001, Student's t-test) at 3 weeks follow-up and in addition to maintenance of low PI and GI scores, further minor reduction (P > 0.5, NS for PI and P < 0.05, SS for GI; Student's t-test) was reported for these at 6 months follow-up.
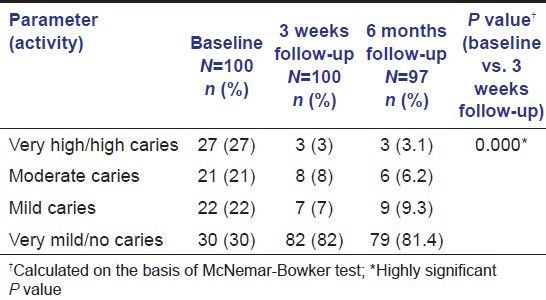
Caries activity
A highly significant increase in number of subjects with very low caries activity was reported at 3 weeks follow-up (P < 0.001; McNemar-Bowker Test) [Table 6]. This change was sustained at 6 months follow-up.
Table 6.
Distribution of subjects according to caries activity at various time points of observation
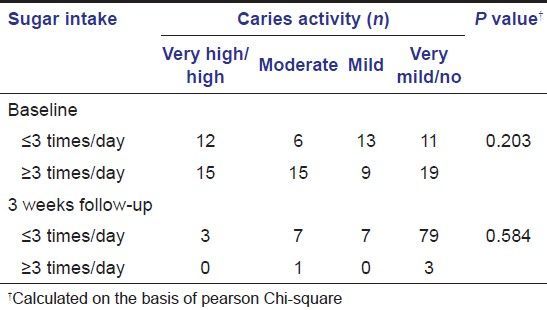
Association between dependent variables
Insignificant association was found between caries activity and daily sugar intake at baseline (Pearson Chi-Square 4.609, P = 0.203) as well as at 3 weeks follow-up (Pearson Chi-Square 1.947, P = 0.584) [Table 7].
Table 7.
Association between sugar consumption and caries activity at various time points of observation
Discussion
There are no organized SOHPP in India at regional/national level. Furthermore, there is scarcity of published literature on feasibility and efficacy of pilot projects on SOHPP in Indian setting. There is a need to have sound evidence based SOHPP, which can help policy makers develop and administer school dental health services. This pilot project aimed to develop a feasible, efficient and cost-effective SOHPP for Indian school children.
We named this project school oral health promotional intervention as in addition to educational intervention, preventive services in form of topical fluoride application and antibacterial therapy with topical povidone iodine application were provided. The present study clearly demonstrated that an inexpensive, easy to organize, school based oral health educational intervention coupled with basic preventive services is efficient in enhancement of overall oral health such as cleanliness, gingival health and caries activity.
Educational programs with health messages delivered in an environment conducive to learning such as school can induce a lasting change in health related behavior.[6,18] Dentist-led strategy to deliver health messages with an intention to induce behavior change is supposed to be the best method when compared with teacher-led, peer-led or self-learning modalities.[19] Although this strategy is condemned owing to limited availability of dentists in underserved areas; it is an efficient method. In the present study, the oral health education was delivered by an undergraduate dental student and it proved to be efficient. By making participation of dental students in community/school dental health a compulsory aspect of undergraduate curriculum, the shortage of community dentists can be overcome.
In the present study, we used a communication-behavior change model[20] applied through transfer of oral health information. Positive changes in health related behavior as a result of such efforts have been reported to be sustained for short term[21] as well as long term.[6,22] In corroboration with this evidence, we reported positive outcome in knowledge as well as practices at 3 weeks follow-up as well as at 6 months follow-up even when no reinforcement was provided after lecture at the start of this study.
Key components of educational intervention to seek positive behavior change were immediate gains from good oral hygiene[9] (such as fresh breath; clean, teeth; and attractive appearance). Further, importance of good oral health and its relationship was emphasized. Children were made aware of etiological basis of oral diseases. As a result of this educational intervention, positive changes were reported in oral health related practices.
Individuals have their own characteristic learning styles and abilities to acquire and retain information.[23] Microsoft Office powerpoint presentations are commonly used to deliver curriculum lectures in schools these days and school children are familiar with this mode of education. This familiar mode of instruction was combined with one-to-one instructions for tooth brushing. Combination of communication and audiovisual aid has been recognized as an effective method to deliver oral health related information.[24,25]
Owing to favorable oral health practices established as a result of our SOHPP, improvement in oral health such as cleanliness, gingival health and caries activity was reported. Significant improvements were reported at 3 weeks follow-up and further improvements were reported at 6 months follow-up. This finding has an important oral health implication in underserved communities. These positive oral health changes were sustained even without reinforcements. It has been reported that exposure to dental inspections and responding to oral health related questionnaire, even when no health messages are delivered might result in improved oral health related behavior especially oral cleanliness.[26] This could possibly explain lasting positive effects at second follow-up.
We used PI and GI, which are reliable tools[27,28] to measure oral cleanliness and gingival health as outcomes for oral health. Further, the examiner was calibrated and consistent recordings were expected at follow-up examinations and at baseline as shown by intra-examiner kappa value of 0.83.[29] Although we developed a prospective model for evaluation of our SOHPP, the follow-up period was small (6 months) and unrealistic to measure caries increment as an outcome. This is the reason modified Snyder's test was used as a measure of caries activity. Modified Snyder's test has long been reported as a reliable prediction tool for caries increment.[30,31] Poor correlation was reported between sugar consumption and caries activity during all time points of measurements throughout the study period. This implies that reduction in caries activity as result of our SOHPP was possibly due to antibacterial topical fluoride varnish[32] and povidone iodine therapy.[32,33] However, a suitable statistical model is needed to extrapolate this possible assumption.
We do not clearly know what arms of this intervention resulted in positive outcome in this trial. Further trials with randomized cluster designs and suitable statistical models are needed. There are few more limitations in this study such as inclusion of homogenous study population, absence of control group and relatively small sample size. However, this pilot project has important oral health implications with suggestions that such economical SOHPP utilizing minimal resources can benefit oral health of masses in underserved population.
Conclusion
This small economical SOHPP positively influenced oral health behavior and parameters of oral health such as oral cleanliness, gingival health and caries activity.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lauris JR, da Silva Bastos R, de Magalhaes Bastos JR. Decline in dental caries among 12-year-old children in Brazil, 1980-2005. Int Dent J. 2012;62:308–14. doi: 10.1111/j.1875-595x.2012.00124.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marthaler TM. Changes in dental caries 1953-2003. Caries Res. 2004;38:173–81. doi: 10.1159/000077752. [DOI] [PubMed] [Google Scholar]
- 3.Goyal A, Gauba K, Chawla HS, Kaur M, Kapur A. Epidemiology of dental caries in Chandigarh school children and trends over the last 25 years. J Indian Soc Pedod Prev Dent. 2007;25:115–8. doi: 10.4103/0970-4388.36559. [DOI] [PubMed] [Google Scholar]
- 4.Sheiham A, Watt R. Oral health promotion and policy. In: Murray JJ, Nunn JH, Steele JG, editors. Prevention of Oral Disease. 4th ed. Oxford: Oxford University Press; 2003. pp. 241–58. [Google Scholar]
- 5.Kay EJ, Locker D. Is dental health education effective. A systematic review of current evidence? Community Dent Oral Epidemiol. 1996;24:231–5. doi: 10.1111/j.1600-0528.1996.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 6.Tai BJ, Jiang H, Du MQ, Peng B. Assessing the effectiveness of a school-based oral health promotion programme in Yichang City, China. Community Dent Oral Epidemiol. 2009;37:391–8. doi: 10.1111/j.1600-0528.2009.00484.x. [DOI] [PubMed] [Google Scholar]
- 7.de Farias IA, de Araújo Souza GC, Ferreira MA. A health education program for Brazilian public schoolchildren: The effects on dental health practice and oral health awareness. J Public Health Dent. 2009;69:225–30. doi: 10.1111/j.1752-7325.2009.00127.x. [DOI] [PubMed] [Google Scholar]
- 8.Amalia R, Schaub RM, Widyanti N, Stewart R, Groothoff JW. The role of school-based dental programme on dental caries experience in Yogyakarta Province, Indonesia. Int J Paediatr Dent. 2012;22:203–10. doi: 10.1111/j.1365-263X.2011.01177.x. [DOI] [PubMed] [Google Scholar]
- 9.Yazdani R, Vehkalahti MM, Nouri M, Murtomaa H. School-based education to improve oral cleanliness and gingival health in adolescents in Tehran, Iran. Int J Paediatr Dent. 2009;19:274–81. doi: 10.1111/j.1365-263X.2009.00972.x. [DOI] [PubMed] [Google Scholar]
- 10.Honkala S, Honkala E, Rimpelä A, Vikat A. Oral hygiene instructions and dietary sugar advice received by adolescents in 1989 and 1997. Community Dent Oral Epidemiol. 2002;30:124–32. doi: 10.1034/j.1600-0528.2002.300206.x. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. WHO Information Series on School Health. Document 8. Geneva: WHO; 2003. Oral health promotion through schools. [Google Scholar]
- 12.Flanders RA. Effectiveness of dental health educational programs in schools. J Am Dent Assoc. 1987;114:239–42. doi: 10.14219/jada.archive.1987.0033. [DOI] [PubMed] [Google Scholar]
- 13.Pine CM. Designing school programmes to be effective vehicles for changing oral hygiene behaviour. Int Dent J. 2007;57:377–81. [Google Scholar]
- 14.Larsen CD, Larsen MD, Handwerker LB, Kim MS, Rosenthal M. A comparison of urban school- and community-based dental clinics. J Sch Health. 2009;79:116–22. doi: 10.1111/j.1746-1561.2008.00395.x. [DOI] [PubMed] [Google Scholar]
- 15.Grewal H, Verma M, Kumar A. Prevalence of dental caries and treatment needs amongst the school children of three educational zones of urban Delhi, India. Indian J Dent Res. 2011;22:517–9. doi: 10.4103/0970-9290.90283. [DOI] [PubMed] [Google Scholar]
- 16.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 17.Loe H, Silness J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 18.Petersen PE, Peng B, Tai B, Bian Z, Fan M. Effect of a school-based oral health education programme in Wuhan City, Peoples Republic of China. Int Dent J. 2004;54:33–41. doi: 10.1111/j.1875-595x.2004.tb00250.x. [DOI] [PubMed] [Google Scholar]
- 19.Haleem A, Siddiqui MI, Khan AA. School-based strategies for oral health education of adolescents-A cluster randomized controlled trial. BMC Oral Health. 2012;12:54. doi: 10.1186/1472-6831-12-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGuire WJ. Public communication as a strategy for inducing health-promoting behavioral change. Prev Med. 1984;13:299–319. doi: 10.1016/0091-7435(84)90086-0. [DOI] [PubMed] [Google Scholar]
- 21.Hausen H. Oral health promotion reduces plaque and gingival bleeding in the short term. Evid Based Dent. 2005;6:31. doi: 10.1038/sj.ebd.6400325. [DOI] [PubMed] [Google Scholar]
- 22.Tewari A, Gauba K, Goyal A. Evaluation of KAP of oral hygiene measures following oral health education through existing health and educational infrastructure. J Indian Soc Pedod Prev Dent. 1992;10:7–17. [PubMed] [Google Scholar]
- 23.Yoder ME. Preferred learning style and educational technology: Linear vs. interactive video. Nurs Health Care. 1994;15:128–32. [PubMed] [Google Scholar]
- 24.Lees A, Rock WP. A comparison between written, verbal, and videotape oral hygiene instruction for patients with fixed appliances. J Orthod. 2000;27:323–8. doi: 10.1093/ortho/27.4.323. [DOI] [PubMed] [Google Scholar]
- 25.Lim LP, Davies WI, Yuen KW, Ma MH. Comparison of modes of oral hygiene instruction in improving gingival health. J Clin Periodontol. 1996;23:693–7. doi: 10.1111/j.1600-051x.1996.tb00595.x. [DOI] [PubMed] [Google Scholar]
- 26.Baranowski T, Allen DD, Mâsse LC, Wilson M. Does participation in an intervention affect responses on self-report questionnaires? Health Educ Res. 2006;21(Suppl 1):98–109. doi: 10.1093/her/cyl087. [DOI] [PubMed] [Google Scholar]
- 27.Macgregor ID. Comparison of the Silness-Loe (1964) Index with gravimetric measurement of dental plaque. Clin Prev Dent. 1987;9:9–12. [PubMed] [Google Scholar]
- 28.McClanahan SF, Bartizek RD, Biesbrock AR. Identification and consequences of distinct Löe-Silness gingival index examiner styles for the clinical assessment of gingivitis. J Periodontol. 2001;72:383–92. doi: 10.1902/jop.2001.72.3.383. [DOI] [PubMed] [Google Scholar]
- 29.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 30.Snyder ML, Arbor A. A simple colorimetric method for diagnosis of caries activity. J Am Dent Assoc. 1941;28:44–9. [Google Scholar]
- 31.Sánchez-Pérez L, Golubov J, Irigoyen-Camacho ME, Moctezuma PA, Acosta-Gio E. Clinical, salivary, and bacterial markers for caries risk assessment in schoolchildren: A 4-year follow-up. Int J Paediatr Dent. 2009;19:186–92. doi: 10.1111/j.1365-263x.2008.00941.x. [DOI] [PubMed] [Google Scholar]
- 32.Milgrom PM, Tut OK, Mancl LA. Topical iodine and fluoride varnish effectiveness in the primary dentition: A quasi-experimental study. J Dent Child (Chic) 2011;78:143–7. [PubMed] [Google Scholar]
- 33.Simratvir M, Singh N, Chopra S, Thomas AM. Efficacy of 10% Povidone Iodine in children affected with early childhood caries: An in vivo study. J Clin Pediatr Dent. 2010;34:233–8. doi: 10.17796/jcpd.34.3.l552816527xtv122. [DOI] [PubMed] [Google Scholar]


