Abstract
Sarcoidosis is classified as an acquired systemic granulomatous disease. Because of the fact that sarcoidosis affects multiple tissues and organs, it is characterized by many potential signs and symptoms, as well as by the presence of non-caseating granulomas in the organs involved. Although oral sarcoidosis is relatively rare, it may however, present in the oral cavity. This report presents a rare case of sarcoidosis with the initial presenting symptom as severe generalized gingival enlargement. The gingival enlargement was treated by gingivectomy. After histopathological examination of gingival biopsy and certain special investigations, a diagnosis of sarcoidosis was made.
Keywords: Gingival enlargement, gingivectomy, sarcoidosis
Introduction
Sarcoidosis is a systemic non-caseating granulomatous disease of unknown etiology. Jonathan Hutchinson, an English surgeon-dermatologist, reported the first case of sarcoidosis in 1875, but the term sarcoidosis was introduced later by Boeck in 1899 (James, 1997)[1] which in Greek means, “flesh-like condition” (Chesnutt, 1995).[2] Sarcoidosis affects all individuals regardless of race, sex or age. There is a worldwide difference in incidence rates of sarcoidosis.[3] It is more frequent among Africans than Caucasians (Reich and Johnson, 1996).[4] One-third of the patients with sarcoidosis can present with non-specific constitutional symptoms such as fever, fatigue, malaise or weight loss (English et al., 2001).[5] The most common presentation of sarcoidosis consists of pulmonary infiltration and hilar lymphadenopathy, dermal and ocular lesions (Hunninghake et al., 1999).[6] Head and neck lesions of sarcoidosis are manifested in 10-15% of patients.[7,8] In the maxillofacial region, the salivary glands are frequently involved, while sometimes, xerostomia and bilateral parotid swelling are present. Lesions that occur in the soft tissues of the oral cavity and/or in the jaws are rare.[9]
This article reports a case of generalized severe gingival enlargement which was the presenting symptom in a patient with sarcoidosis.
Case Report
A 36-year-old female patient reported to the Department of Periodontics, in our institute, with the chief complaint of generalized overgrowth of gums. Patient had noticed it from the past 10 years, which has gradually increased to the present state. Medical history was not significant. Patient was asked about endocrine abnormality (to rule out pregnancy gingivitis), intake of drugs like nifedipine, cyclosporine and phenytoin (to rule out drug induced gingival enlargement) and history of any allergy. All of which were negative. To rule out hereditary gingival fibromatosis, she was asked about family history, with particular importance to family dental history, which was negative. Her socioeconomic condition was poor and she was uneducated, belonged to a village. She gave a significant dental history of similar gingival overgrowth 12 years back which was treated by a local dental surgeon, then. Patient could not recollect the details regarding treatment given to her at that time. Two years after the treatment, patient noticed a recurrence of gingival enlargement and has been gradually increasing to the present state, much severe than previous one. Patient had difficulty in eating and pain in gums while brushing teeth, with occasional bleeding. Clinically she had severe generalized gingival enlargement, soft and spongy, reddish pink which bled on touching, particularly in lower anterior region where the enlargement almost covered the clinical crowns [Figure 1]. Her oral hygiene status was fair (Greene and Vermillion Index).[10] She had missing teeth – 18, 35, 45, 48 (FDI Federation Dentaire Internationale System). She did not give any history about extraction of these teeth.
Figure 1.

Pretreatment photograph showing generalized severe gingival enlargement
An orthopantomograph was taken which showed mild alveolar bone loss in upper and lower anterior teeth and missing (congenitally) 18, 35, 45, 48 [Figure 2].
Figure 2.
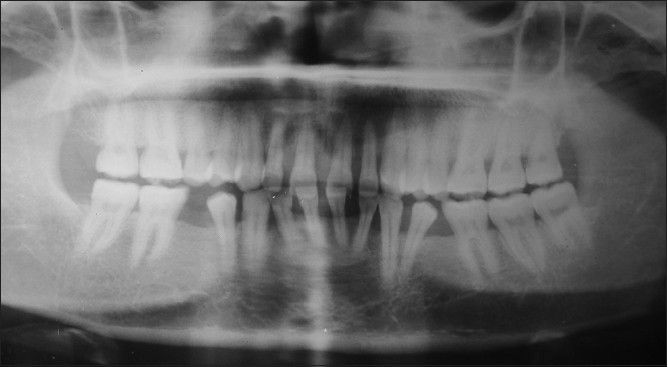
Orthopantomograph showing mild alveolar bone loss in relation to upper and lower anterior teeth. Also evident are missing teeth
Treatment consisted of oral prophylaxis (scaling and polishing procedures) and oral hygiene instructions. She was advised to rinse twice daily with 0.2% chlorhexidine mouthwash, 10 ml, 1:1 dilution for 15 days. After 1 month, on reevaluation, it was observed that the enlargement had not reduced in severity, size, clinical appearance and consistency and was same as 1 month back. Hence, the inflammatory cause of gingival enlargement was also ruled out and she was posted for surgical excision.
Informed consent was taken prior to the surgical procedure. Lower anterior region was chosen for first surgical session as the enlargement was severest in this region. Surgical excision was performed under local anesthesia using the external bevel gingivectomy technique [Figure 3]. The excised tissue was submitted for histopathological examination which demonstrated non-caseating epithelioid cell granulomas, typical of granulomatous conditions, using hematoxylin and eosin staining [Figure 4]. Multinucleated giant cells were evident throughout the granuloma. Based on the histological findings, a number of special investigations were undertaken, to rule out various granulomatous diseases. Mantoux test and Sputum test was negative for tuberculosis. Complete blood count reports showed eosinophil count -24% (normal range 0-4%). Serum angiotensin converting enzyme (sACE) levels were - 1038.5 nkat/L (normal range lesser than 670 nkat/L). Chest X-ray showed hilar lymphadenopathy. Based on the histopathological examination, elevated sACE levels, increased eosinophil count and chest X-ray findings, diagnosis of sarcoidosis was made. The patient was referred to the physician for further investigations and treatment. Since she did not have symptomatic pulmonary involvement she was not given any medications for sarcoidosis and was kept under regular follow-up by the physician for 5 months. She did not show any symptoms of the disease and was referred back for treatment of gingival enlargement.
Figure 3.

Immediately after gingivectomy of lower anterior teeth
Figure 4.
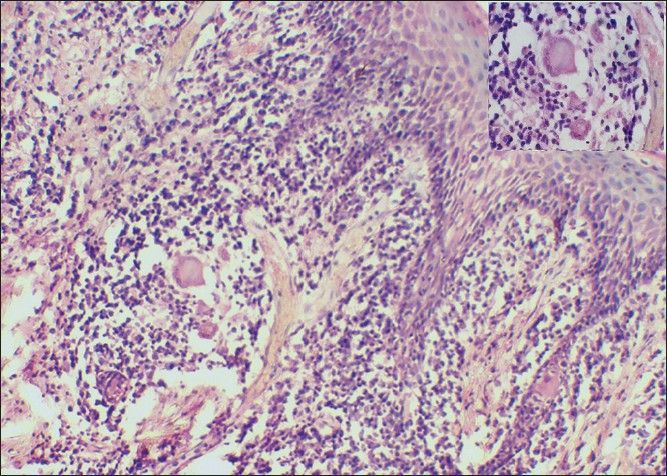
Photomicrograph showing granulomas with lymphocytes and epitheloid cells with Langhans giant cells (inset: Langhans giant cells)
Other areas of gingival enlargement were treated by external bevel gingivectomy. Patient was followed-up by us for 1 month after completion of full mouth gingivectomy and showed good healing with no signs of recurrence of gingival enlargement [Figure 5] after which the patient went back to her village and has not reported again for follow-up.
Figure 5.

Post-operative picture, 1 month after completion of full mouth gingivectomy
Discussion
Sarcoidosis is a multiorgan disorder. The clinical symptoms depend on the ethnicity, chronicity of illness, site and extent of involvement of the organ and activity of the granulomas. The most common presentation consists of pulmonary infiltration and hilar lymphadenopathy, dermal and ocular lesions (Hunninghake et al., 1999).[6]
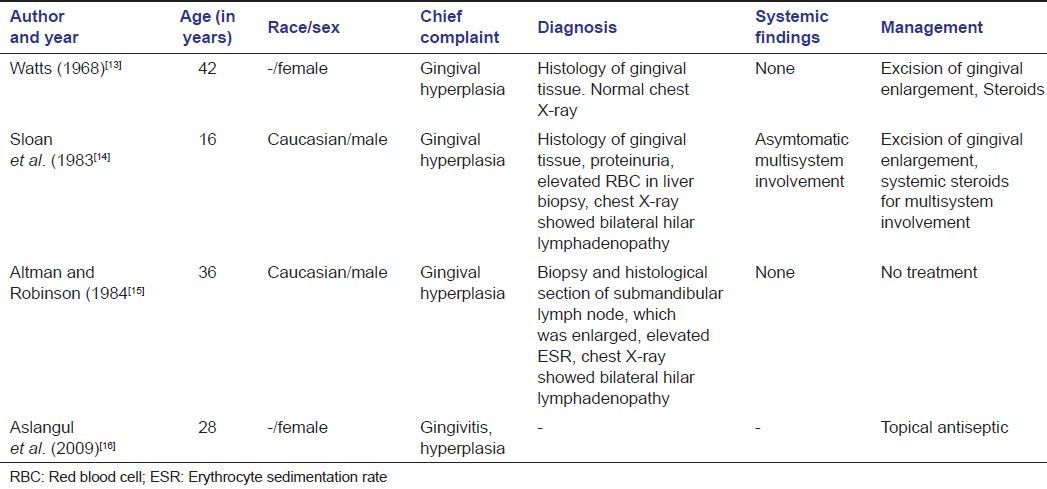
Oral involvement in sarcoidosis is uncommon. Schroff (1942)[11] reported the first suspected case of sarcoid granulomas in the oral mucosa. Since then, there have been only 70 well-documented cases of oral sarcoidosis reported in literature (jaw bones and salivary glands involvements being excluded), where the initial presentation is of oral sarcoidosis, of which only four cases presented as gingival enlargement (Table 1, as adapted from Suresh and Radfar, 2005[3] and Bouaziz et al., 2012[12])]
Table 1.
Sarcoidosis presenting as gingival enlargement (adapted from Suresh and Radfar, 2005[3] and Bouaziz et al., 2012[12])
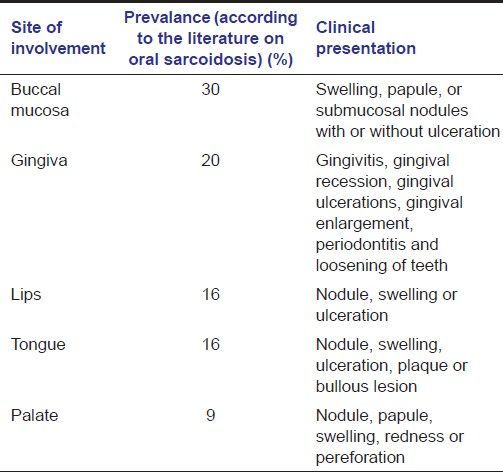
Clinically, the disease can affect any site of the mouth with a variety of clinical presentations (Table 2, as adapted from Bouaziz et al., 2012[12])]
Table 2.
Prevalence and clinical presentation of oral sarcoidosis according to the site (adapted from Bouaziz et al., 2012[12])
The etiology of sarcoidosis is not well understood. Genetic predisposition may be a factor. Viral and bacterial infections (mycobacteria, Epstein-Barr virus), external environmental factors and occupational exposures such as mold and material used in pesticides have also been suggested as causative factors.[17]
The mechanism by which sarcoidosis develops is a form of immunological response to one or more of these factors which lead to the formation of the non-caseating granulomas.
There are no specific tests for sarcoidosis. Diagnosis of sarcoidosis is mainly based on exclusion of other non-caseating granulomas forming conditions. The diagnosis of sarcoidosis is established when clinical features are supported by histopathological evidence of typical non-caseating epithelioid granulomas and other laboratory tests (Samtsov 1992;[7] Newman et al., 1997).[8]
The sACE level has been studied extensively as a laboratory marker in sarcoidosis. Secretion of ACE by granuloma-forming epithelioid cells results in high serum levels in 80-90% of patients with sarcoidosis. sACE activity has been used as an indicator of the clinical course and severity of sarcoidosis.[18]
Treatment is not required for all patients with sarcoidosis. The American Thoracic Society, European Respiratory Society and World Association of Sarcoidosis and Other Granulomatous Disorders have identified specific conditions, which require treatment (Hunninghake et al., 1999).[6] These include the sarcoidosis of the heart and nerves, hypercalcemia and ocular involvement that do not respond to local therapy.
Asymptomatic pulmonary involvement does not require treatment, while treatment is indicated in symptomatic pulmonary sarcoidosis with worsening pulmonary function tests (Baughman and Lynch, 2003).[19] Corticosteroids have remained as the mainstay in the treatment of sarcoidosis. Antimalarial drugs in combination with low dose corticosteroids and certain immunosuppressant drugs have been shown to be beneficial in the treatment of sarcoidosis. Concerning oral sarcoidosis treatment, the available information is poor and mainly comes from scattered case reports. The choice of treatment mainly depends on severity and extent of the disease. Different treatments have been employed ranging from no specific therapy to surgical excision.[3,12]
Prognosis of sarcoidosis correlates with mode of onset, initial clinical course, hosts’ characteristics, extent and severity of disease.[7] The prognosis in patients with hilar lymphadenopathy is good, but in patients with radiological signs of irreversible fibrosis is the worst.
Many of those affected remain asymptomatic and remission sometimes occurs spontaneously (Shams et al., 2007).[20] In a few patients, progressive disease may lead to death (English et al., 2001).[5] Hence, it is important to enforce a periodic follow-up of these patients in order to evaluate the status and course of the disease.
Conclusion
The case presented demonstrates a rare presentation of sarcoidosis which was treated by gingivectomy. No systemic treatment was given to the patient as she did not have symptomatic pulmonary involvement. Regular monitoring is important in such cases to know the progress of the disease, as in some cases remissions may occur spontaneously or the disease may progress still further. This case report supports the literature regarding oral sarcoidosis, that, although rare, granulomatous conditions like sarcoidosis can manifest as gingival enlargement and should be considered as a differential diagnosis of gingival enlargement.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.James DG. Descriptive definition and historic aspects of sarcoidosis. Clin Chest Med. 1997;18:663–79. doi: 10.1016/s0272-5231(05)70411-1. [DOI] [PubMed] [Google Scholar]
- 2.Chesnutt AN. Enigmas in sarcoidosis. West J Med. 1995;162:519–26. [PMC free article] [PubMed] [Google Scholar]
- 3.Suresh L, Radfar L. Oral sarcoidosis: A review of literature. Oral Dis. 2005;11:138–45. doi: 10.1111/j.1601-0825.2005.01014.x. [DOI] [PubMed] [Google Scholar]
- 4.Reich JM, Johnson RE. Incidence of clinically identified sarcoidosis in a northwest United States population. Sarcoidosis Vasc Diffuse Lung Dis. 1996;13:173–7. [PubMed] [Google Scholar]
- 5.English JC, 3rd, Patel PJ, Greer KE. Sarcoidosis. J Am Acad Dermatol. 2001;44:725–43. doi: 10.1067/mjd.2001.114596. [DOI] [PubMed] [Google Scholar]
- 6.Hunninghake GW, Costabel U, Ando M, Baughman R, Cordier JF, du Bois R, et al. ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other granulomatous disorders. Sarcoidosis Vasc Diffuse Lung Dis. 1999;16:149–73. [PubMed] [Google Scholar]
- 7.Samtsov AV. Cutaneous sarcoidosis. Int J Dermatol. 1992;117:203–7. doi: 10.1111/j.1365-4362.1992.tb02664.x. [DOI] [PubMed] [Google Scholar]
- 8.Newman LS, Rose CS, Maier LA. Sarcoidosis. N Engl J Med. 1997;336:1224–34. doi: 10.1056/NEJM199704243361706. [DOI] [PubMed] [Google Scholar]
- 9.Kolokotronis AE, Belazi MA, Haidemenos G, Zaraboukas TK, Antoniades DZ. Sarcoidosis: Oral and perioral manifestations. Hippokratia. 2009;13:119–21. [PMC free article] [PubMed] [Google Scholar]
- 10.Greene JC, Vermilion JR. The oral hygiene index. A method for classifying oral hygiene status. J Am Dent Assoc. 1960;61:172–9. [Google Scholar]
- 11.Schroff J. Sarcoid of the face (Besnier-Boeck-Schumann) disease: eport of a case. J Am Dent Assoc. 1942;29:2208–11. [Google Scholar]
- 12.Bouaziz A, Le Scanff J, Chapelon-Abric C, Varron L, Khenifer S, Gleizal A, et al. Oral involvement in sarcoidosis: Report of 12 cases. QJM. 2012;105:755–67. doi: 10.1093/qjmed/hcs042. [DOI] [PubMed] [Google Scholar]
- 13.Watts KD. Sarcoid of the gingivae: A case report. Br J Oral Surg. 1968;6:108–13. doi: 10.1016/s0007-117x(68)80007-1. [DOI] [PubMed] [Google Scholar]
- 14.Sloan PJ, O’Neil TC, Smith CJ, Holdsworth CD. Multisystem sarcoid presenting with gingival hyperplasia. Br J Oral Surg. 1983;21:31–5. doi: 10.1016/0007-117x(83)90028-8. [DOI] [PubMed] [Google Scholar]
- 15.Altman K, Robinson PD. Sarcoidosis with oral involvement. Br Dent J. 1984;157:310–1. doi: 10.1038/sj.bdj.4805478. [DOI] [PubMed] [Google Scholar]
- 16.Aslangul E, Gadhoum H, Badoual C, Szwebel T, Perrot S, Le Jeunne C. A chronic gingival hypertrophy. Rev Med Interne. 2009;30:260–1. doi: 10.1016/j.revmed.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 17.Moller DR, Chen ES. What causes sarcoidosis? Curr Opin Pulm Med. 2002;8:429–34. doi: 10.1097/00063198-200209000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Ueda E, Kawabe T, Tachibana T, Kokubu T. Serum angiotensin-converting enzyme activity as an indicator of prognosis in sarcoidosis. Am Rev Respir Dis. 1980;121:667–71. doi: 10.1164/arrd.1980.121.4.667. [DOI] [PubMed] [Google Scholar]
- 19.Baughman RP, Lynch JP. Difficult treatment issues in sarcoidosis. J Intern Med. 2003;253:41–5. doi: 10.1046/j.1365-2796.2003.01076.x. [DOI] [PubMed] [Google Scholar]
- 20.Shams MG, Motamedi MH, Azizi T. Orofacial granulomatosis of the lower lip and cheek: Report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e42–4. doi: 10.1016/j.tripleo.2007.05.012. [DOI] [PubMed] [Google Scholar]


