Abstract
Objective
To evaluate the effectiveness of a Cognitive-Behavioral therapy (CBT) for suicide prevention in decreasing suicidal ideation and hopelessness in a sample of depressed 12 to 18 year-old adolescents who had at least one previous suicidal attempt.
Methods
In a clinical trial, 30 depressed adolescents who attempted suicide in the recent 3 months were selected using simple sampling method and divided randomly into intervention and wait-list control groups. Both groups received psychiatric interventions as routine. The intervention group received a 12 session (once a week) of CBT program according to the package developed by Stanley et al, including psychoeducational interventions and individual and family skills training modules. All of the patients were evaluated by Scale for Suicidal Ideation, Beck's hopelessness Inventory, and Beck's Depression Inventory before the intervention and after 12 weeks.
Findings
There were significant differences between the two groups regarding the scores of the above mentioned scales after 12 weeks. Fifty-four to 77 percent decreases in the mean scores of the used scales were observed in the invention group. There were no significant changes in the scores of the control wait-list group. The differences between pre- and post-intervention scores in the intervention group were significant.
Conclusion
CBT is an effective method in reducing suicidal ideation and hopelessness in the depressed adolescents with previous suicidal attempts.
Keywords: Suicide, Cognitive-Behavioral Therapy, Depression, Adolescents, Hopelessness, Suicidal Idea
Introduction
None of the psychiatric emergencies are as important as suicide. Suicide is one of the leading causes of death in the adolescents and its incidence is increasing in the recent years[1]. Suicide is one of the ten leading causes of death in the world. It has significant impacts on the well-being of the patients and causes significant mortality and morbidity and has similar negative consequences on the family member, society, and health systems[2].
Suicidal attempts are 10 to 40 times more prevalent than committed (completed) suicide. Suicide is still a taboo in the Islamic societies and most of deaths due to suicide in these countries are reported as accidents[3]. It has been reported that about 9 percent of the adolescents had at least one suicidal attempt in the year before the study. Suicide is the third cause of death in the United States[4]. Depressive disorders have been reported in up to 95 percent of the adolescents who attempt suicide[5]. Hopelessness is the most important factor in the depressed patients and has a predictive value in suicidal ideation, suicidal attempt and committed suicide[6].
Suicidal behaviors have different characteristics in different periods of individual's life cycle[7]. For example, in the adolescents, identificational suicide (i.e. attempting suicide because somebody in the peer group or some famous people did so) may be an important factor that predicts suicidal behaviors[8].
Unfortunately, there is no empirically supported method to specifically prevent suicidal attempts[1]. It has been shown that interventions that are aimed to decrease some risk factors such as depression, suicidal ideation, and impulsivity may be helpful in prevention further suicidal attempts[9]. It has been mentioned that Cognitive-Behavioral Therapy (CBT) can challenge maladaptive beliefs, and improve problem solving skills and social competence[8]. All of the above mentioned problems usually exist in the patients who attempt suicide or have suicidal ideations.
Considering the above mentioned notes, and high frequency of depressive disorders in the adolescents who attempted suicide, the researchers decided to evaluate the effectiveness of CBT in decreasing suicidal ideation, hopelessness and depression (as predecessors of suicidal attempts) in adolescents who had at least one suicidal attempt in the past 3 months, by helping them to improve their social competence, problem solving skills, and challenging maladaptive and erroneous cognitive schemas.
Subjects and Methods
Study design
The Present study is an open labeled clinical trial that was designed to evaluate the effectiveness of CBT in decreasing suicidal ideation and hopelessness in the 12 to 18 year-old depressed adolescents who had a positive history of previous suicidal attempt in the past 3 months. Although in most psychiatric studies it has been noted that a 30 percent decrease in the used scales can be interpreted as efficacy of the used intervention, the researchers decided to compare only the mean scores of the used instruments.
Participants
Thirty 12 to 18 year-old adolescents who had a previous suicidal attempt in the past 3 months and were admitted in Namazi, Shooshtari, and Hafez Hospitals, Shiraz, Iran during summer 2011 to winter 2012 were selected suing simple sampling method. The participants were divided randomly into intervention and wait list control groups. Only the patients with suicidal attempts in the past 90 days, with mild to moderate major depressive disorder (MDD) were selected and the patients with bipolar mood, psychotic, pervasive developmental, severe depressive disorder (that needed prompt hospitalization) or substance use disorders, or the patients who received electroconvulsive therapy (ECT), were excluded from the study. The patients who attempted suicide as a means for tension release or attention seeking without a real suicidal intention, the patients who could not participate in the psychotherapy sessions or did not mention any current suicidal idea were also excluded from the study. Patients in both groups received routine psychiatric interventions and follow-ups. All of the patients gave oral consent to participate in the study and finished it. The study was approved by the Committee of Ethics of Shiraz University of Medical Sciences.
Instruments
Scale for Suicidal Ideation (SSI): This instrument, which was introduced by Beck et al in 1979[10], includes 19 items each of which has 3 choices (active suicidal intention, distinct plans for suicide, and passive suicidal intention). Each item is scored from 0 to 2 with a total score of 0 to 38. It has a relatively high internal consistency, with a Chronbach's alpha of 84 to 89 percent. Its reliability and validity have been proven for outpatients.
Beck's Hopelessness Inventory (BHI): This inventtory consists of 20 items that measure three major aspects of hopelessness: feelings about the future, loss of motivation, and expectations. It has a reliability coefficient of 93 percent and a total coefficient ratio of 39 t0 76 percent. The answers are in a true-false format and higher scores on the inventory mean higher probability of hopelessness[11].
Beck's Depression Inventory (BDI): This Inventory includes 21 items each one having 4 choices that score between 0 and 4. Higher scores denote higher severity of depression. The Persian version of this inventory has validity coefficient equal to 70%, reliability coefficient of 77%and internal consistency of 91%[12].
Intervention
The Intervention group received a package of 12 sessions of CBT for suicidal ideation as follow. The patients in the control group were placed on the wait list condition. All of the patients were evaluated with the mean of the above-mentioned instruments before starting the study. The patients in the intervention group were evaluated in the final session. Considering that the intervention took about 3 months to be completed, the patients in the control group were evaluated after 3 months. All of the patients received appropriate pharmacotherapy if needed.
The intervention according to the Stanley et al model[4] includes 3 phases. The initial phase lasting 3 sessions consists of five main components: chain analysis, safety planning, psychoeducation, developing reasons for living and hope, and case conceptualization. The last 2 components occur during the 3rd session. Parents are allowed to participate in the first session. The middle phase of the treatment lasts from 4th to 9th session and includes optional individual (including behavioral activation and increasing pleasurable activities, mood monitoring, emotion regulation and distress tolerance techniques, cognitive restructuring, problem solving, goal setting, mobilizing social support, and assertiveness skills) and family (including family behavioral activation, family emotion regulation, family problem solving, family communication, and family cognitive restructuring) skills training modules. The termination phase that lasts from the 10th to 12th session includes a relapse prevention task that embraces five steps: (a) Preparation, (b) Review of the indexed attempt or suicidal crisis, (c) Review of the attempt or suicidal crisis using skills, (d) Review of a future high risk scenario, and (e) Debriefing and follow-up.
Statistical Analysis
The obtained data were analyzed by Student t- and chi square tests using the statistical software SPSS Win 16.0 when appropriate. The significance level determined to be equal to 0.05.
Findings
All 30 patients (15 patients in each group) finished the study. Females were dominant in each group (14 cases in intervention and 13 cases in control group, P=0.5). The mean age and SSI, BHI, and BDI score of the patients in the two groups before the intervention had no significant differences as shown in Table 1. There were no significant differences between the two groups regarding age and sex distribution.
Table 1.
Demographic and mean scores of different scales in the studied groups
| Parameter | Intervention (n = 15) (Mean ± SD) | Control (n = 15) (Mean ± SD) | P. value |
|---|---|---|---|
| Age | 16.1(1.6) | 16(1.2) | 0.8 |
| Pretreatment SSI | 20.8(3.27) | 19.53(4.3) | 0.3 |
| Pretreatment BHI | 12.6(4.7) | 11(3.58) | 0.3 |
| Pretreatment BDI | 30.58(5.35) | 27.78(4.11) | 0.2 |
| Post-treatment SSI | 4.6(4.12) | 20.33(6.13) | <0.001 |
| Post-treatment BHI | 3.2(2.33) | 11.67(4.7) | <0.001 |
| Post-treatment BDI | 14.42(3.89) | 33.6(8.56) | <0.001 |
SD: Standard Deviation SSI: Scale for Suicidal Ideation; BHI: Beck's Helplessness Inventory; BDI: Beck's Depression Inventory
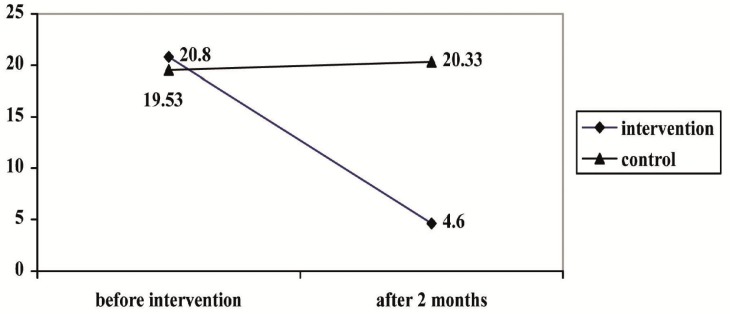
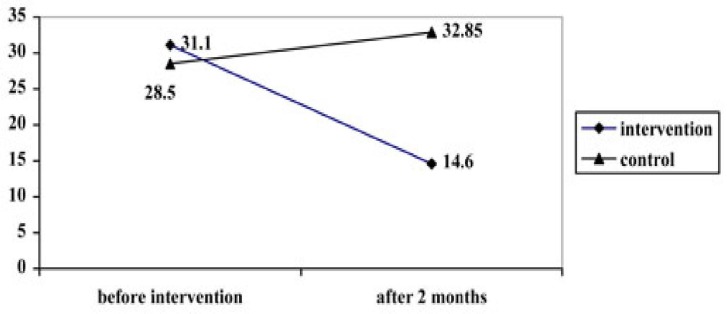
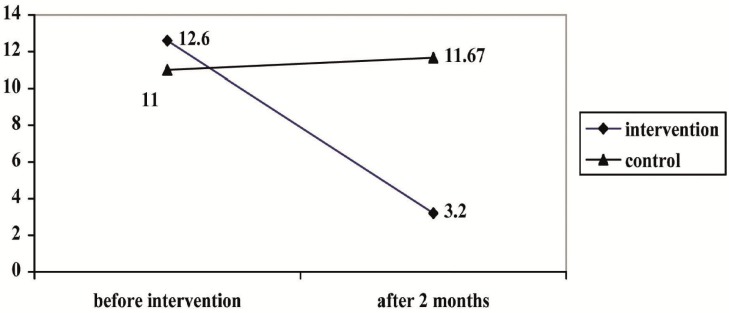
The scores of the above-mentioned inventories in the control group after 3 months did not change significantly (in all of them P > 0.05; Figs. 1–3) but the scores in all of these inventories decreased significantly in the intervention group (in all of them P < 0.001; Figs. 1–3). The differences between the 2 groups after 3 months were also significant.
Fig. 1.
Mean scale for suicidal ideation scores in the studied groups before and after the intervention
Fig. 3.
Mean Beck's Depression Inventory scores in the studied groups before and after the intervention
Fig. 2.
Mean Beck's Hopelessness Inventory scores in the studied groups before and after the intervention
Discussion
This study was performed to evaluate the efficacy of a 12 sessions CBT package on the suicidal ideation, helplessness depression of the 12 to 18 year-old adolescents who had a previous suicidal attempt in the past 3 months. The patients in the control group were enrolled in a wait-list and received the intervention after the second evaluation in 3 months.
There were no statistically significant differences in the mean scores of SSI, BHI, and BDI between the intervention and control group in beginning of the study. The mean age and sex distribution of the two groups were not statistically different, too. This means that the two groups were similar and comparable and the observed differences after the intervention can be attributed to the designed intervention.
The mean SSI, BHI, and BDI scores of the two groups were different after 3 months. This was similar to findings of Spirito et al[13], Stanley et al[4], and Bateman et al[14]. All of these studies used CBT approaches for different patients and reported this method as being effective in decreasing suicidal ideation. Considering that the performed intervention was adopted from a package developed by Stanley et al[4], the similarity between the present study and these studies may be an expected finding. It also seems that observing the current changing trends in social values in Iranian community and some universal similarities in youths’ conflicts, similar interventions may have similar efficacy in cognitive reconstruction and rehabilitation.
However, in a study performed by Wood et al[15] comparing group psychotherapy and conventional support for suicidal adolescents, there were no significant differences between the two groups regarding severity of depression and suicidal thoughts following the intervention. They also combined dialectic behavioral therapy and group psychodynamic approach in their treatment program that are different from the methods used in the present study. They observed some benefits in self-harm behaviors and improved school performance in the intervention group but failed to do so in depressive symptoms, helplessness, or suicidal ideation. The difference between the mentioned study and present study may be due to different approaches used in the two studies. The reason for different results may also be due to the fact that suicidal adolescents benefit more from individualized formats of treatment that consider individual characteristics and family system.
In the present study, like the study performed by Barbe et al[16], Stanley et al[4], Bapiri et al[17], and Hanasabzade et al[18] CBT was effective in decreasing hopelessness and depression scores of the suicidal adolescents. However Wood et al failed to show any efficacy of CBT in decreasing severity of depression[15]. As it was discussed before, the main reason for this difference may be inclusion of the suicidal adolescents. However, Wood et al[14] failed to show any efficacy of CBT in decreasing severity of depression. As it was discussed before, the main reason for this difference may be the group psychotherapy or different treatment format of the mentioned study.
Limitations: Lack of motivation to participate in a CBT program is a key problem in the adolescent age group specifically in the patients who are suicidal. We chose an empathic approach and tried to maintain an appropriate and friendly rapport to overcome this limitation. Trying to draw parental cooperation, trust and considering their psycho-education in the program was another objective to maintain adolescent motivation to participate in the study. Small sample size is another limitation of this study.
Conclusion
Considering the results of the present study and the results of similar studies, and considering the differences of cognitive abilities of the adults and adolescents and higher flexibility of the adolescent cognitive structures, it can be concluded that CBT is an effective, appropriate, and acceptable treatment modality for the adolescents with recent suicidal attempts and current suicidal ideas. On the other hand, one of the major predisposing factors in the suicidal adolescents is lack of enough problem solving skills. Therefore, a significant emphasis on this aspect of adolescents’ life seems to be necessary. The effect of conflictual family systems, inappropriate parenting styles, changing social standards, emotional problem on adolescents’ life must be taken into consideration in any successful treatment intervention.
Acknowledgment
This study was a part of fulfillment for MS degree of B Sharifi and it was done by using funds from and published by permission of Shiraz University of Medical Sciences. The authors wish to thank all of the participants of the study. They also wish to express their gratitude to the staff of Namazi, Shooshtari, and Hafez Hospitals for their kind collaboration in the study and referring the patients.
Conflict of Interest
None
References
- 1.Azar M, Nouhi S, Shafiei Kandejani A. Suicide. Tehran: Arjmand publications; 2006. [In Persian] [Google Scholar]
- 2.Keyvanara M, Mousavi SG, Malekian A, et al. Suicide prevention: the experiences of recurrent suicide attempters (a phenomenological study) Iran J Psychiatry Behav Sci. 2010;4(1):4–12. [In Persian] [Google Scholar]
- 3.Seghatoleslam T, Rezaee M, Sajadfar F, et al. A study on psycho-social factors related to children's suicide. Iran Red Crescent Med J. 2010;12(6):660–3. [Google Scholar]
- 4.Stanley B, Brown G, Brent AD, et al. Cognitive-behavioral therapy for suicide prevention (CBT-SP): treatment model, feasibility and acceptability. J Am Acad Child Adolesc Psychiatry. 2009;48(10):1005–13. doi: 10.1097/CHI.0b013e3181b5dbfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zamani G, Mehdizadeh M, Sadeghi P. Attempt to suicide in young ages with epilepsy. Iran J Pediatr. 2012;22(3):404–7. [PMC free article] [PubMed] [Google Scholar]
- 6.Rudd MD, Joiner TE, Hasan Rajab M. Tehran: Roshd Publication; 2007. Treating suicidal behavior: an effective, time-limited approach (Treatment Manuals for Practitioners), 2001. Translated by: Foroughan M. [Google Scholar]
- 7.Daniel SS, Goldstone BD. Intervention for suicidal youth: a review of the literature and developmental consideration. Suicide Life Threat Behav. 2009;39(3):252–68. doi: 10.1521/suli.2009.39.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaplan H, Sadock B. Synopsis of Psychiatry. 10th ed. Philadelphia: Lippincot Williams and Wilkins; 2007. [Google Scholar]
- 9.Sokero TP, Melartin TK, Rytsälä HJ, et al. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. 2003;64(9):1094–100. doi: 10.4088/jcp.v64n0916. [DOI] [PubMed] [Google Scholar]
- 10.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343–52. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 11.Beck AT. Beck Hopelessness Scale. The Psychological Corporation; 1988. [Google Scholar]
- 12.Kaviani H, Mousavi AS. Psychological interview and tests. Tehran: Mehr-e Kavian; 2009. pp. 180–9. [in Persian] [Google Scholar]
- 13.Spirito A, Esposito-Smythers C, Wolff J, et al. Cognitive-behavioral therapy for adolescents depression and suicidality. Child Adolesc Psychiatr Clin N Am. 2011;20(2):191–204. doi: 10.1016/j.chc.2011.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bateman K, Hansen L, Turkington D, et al. Cognitive behavioral therapy reduces suicidal ideation in schizophrenia: results from a randomized controlled trial. Suicide Life threat Behav. 2007;37(3):284–90. doi: 10.1521/suli.2007.37.3.284. [DOI] [PubMed] [Google Scholar]
- 15.Wood A, Trainor G, Rothwell J, et al. Randomized trial of group therapy for repeated deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1246–53. doi: 10.1097/00004583-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Barbe PR, Bridge J, Birmaher B, et al. Suicidality and its relationship to treatment outcome in depressed adolescents. Suicide Life Threat Behav. 2004;34(1):44–55. doi: 10.1521/suli.34.1.44.27768. [DOI] [PubMed] [Google Scholar]
- 17.Bapiri OA, Bahamin GH, Feyzelahi A. Impact of group problem solving training on some psychological characteristics of adolescents attempting suicide. J Ilam Univ Med Sci. 2010;18(1):16–22. [In Persian] [Google Scholar]
- 18.Hanasabzade M, Yazdandoost R, Asgharnejad Farid A, et al. Mindfulness based cognitive therapy (MBCT) on suicidal depressed patients: A qualitative study. J Behav Sci. 2011;5(1):33–8. [In Persian] [Google Scholar]