Abstract
Most studies on the prevalence and determinants of resistant hypertension (RH) do not account for white coat hypertension, medication non-adherence, or use of suboptimal treatment dosages. We studied the characteristics, drug combinations, and dosages of patients on at least three antihypertensives of different classes who had uncontrolled blood pressure on 24-hour ambulatory blood pressure monitoring and high medication adherence measured by electronic monitoring. The data were collected as part of the baseline measures of a hypertension control trial. Of 140 monitored primary care patients, all with uncontrolled office blood pressure, 69 (49%) were on at least three antihypertensives of different classes. Of these 69, 15 (22%) were controlled on ambulatory blood pressure monitoring, 20 (29%) were uncontrolled and non-adherent, leaving only 34 (49%) adherent to their medications and having uncontrolled ambulatory hypertension (uncontrolled RH). Thirty-one (91%) of the 34 uncontrolled RH patients were prescribed a diuretic, of which 24 were on hydrochlorothiazide 25 mg. Less than half of the patients on angiotensin-converting enzyme inhibitor, angiotensin receptor blocker, or calcium channel blocker were prescribed maximal doses of these agents. Half of the RH can be attributed to white coat effect and poor medication adherence, and all of the remaining patients were on apparently suboptimal drug combinations and/or dosages. Primary care physicians need to be educated regarding the optimal treatment of RH.
Keywords: Resistant hypertension, white-coat hypertension, medication adherence, electronic monitoring, drug dosage
Introduction
Resistant hypertension (RH), defined as blood pressure (BP) that remains above goal in spite of the concurrent use of three antihypertensive agents of different classes, is an important clinical problem.1 Patients with RH have high cardiovascular risk and high prevalence of target organ damage.2 The prevalence of RH has been reported to range from 12% to 15% in the treated hypertensive population.3,4 However, most studies on the prevalence and determinants of RH do not account for white coat hypertension,3,5–8 poor medication adherence (MA),3,4,7,9,10 or use of suboptimal treatment dosages.3,4,6–9,11 In a recent study including a large cohort of treated hypertensive patients from the Spanish Ambulatory Blood Pressure Monitoring (ABPM) registry, 37.5% of RH patients had normal 24-hour BP.9 Therefore, a considerable number of RH patients have a “white coat syndrome” and do not have true RH. Another group of patients that should be excluded are those with poor MA. Poor MA, an important cause of poor BP control,12 is common in treated hypertensives.13,14 Finally, patients with suboptimal drug combinations and/or dosages should not be included in the group of true RHs.
As part of a study on improving hypertension control, we had baseline data including drug regimens and doses, 24-hour ABPM, and adherence as measured by Medication Event Monitoring System (MEMS) bottle caps for patients who were uncontrolled based on office BP measurements in 10 Primary Care (PC) settings in a southwestern United States (US) city. We described the characteristics, antihypertensive regimens, and dosages of patients on at least three antihypertensives of different classes who had uncontrolled BP based on 24-hour ABPM and high MA measured by MEMS. We compared them with patients on at least three drugs whose BP was controlled based on 24-hour ABPM.
Methods
Study Population
Data for this study were collected as part of a cluster-randomized trial on clinical inertia and BP control in 10 PC clinics between 2006 and 2007. The details of the trial have been reported.15,16 Eligible patients had to be over 21 years and have at least two clinic visits in the previous 12 months, with BP on the most recent two consecutive visits of ≥140 mm Hg systolic (SBP) or ≥90 mm Hg diastolic (DBP), or if diabetic, ≥130 mm Hg SBP or 80 mm Hg DBP. Since the trial was aimed at improving BP control in established hypertensives, some evidence of prior diagnosis and/or treatment of hypertension was required. Research assistants identified potential study participants by screening the medical records of patients who presented for a routine PC appointment. Patients with cognitive impairment, renal insufficiency (recent serum creatinine >2.0), or a serious concomitant illness such as cancer, recent myocardial infarction, or unstable angina, were excluded. Informed consent was obtained from both the patient and provider.
A random subsample of patients at baseline underwent a 24-hour ABPM and an electronic bottle cap monitoring. The Aardex Medication Event Monitoring System (MEMS 6 Track Cap, Sion, Switzerland) was used to record the date and time of each bottle cap opening during the monitoring period. Up to three antihypertensive medications were monitored for 30 days. Standardized quality control procedures included testing each device before it was dispensed to the participant (eg, checking battery status, visually examining the devices for defects and malfunctions, etc), educating participants in the proper use of the devices, debriefing participants when they return devices, and cleaning and analyzing the data. The 24-hour ABPM was performed using the Oscar 2 (Suntech Medical, Morrisville, NC) monitor, programmed to take a reading every 20 minutes during the day, and every 45 minutes at night. Valid registries had to fulfill a series of pre-established criteria, including 80% of both SBP and DBP successful recordings during the daytime and nighttime periods, 24-hour duration, and at least one BP measurement per hour.
Data on age, gender, race/ethnicity, employment status, smoking status, comorbidities, and years of education completed were collected at baseline. Patients were also asked to list all of their current antihypertensive medications, and indicate the number and timing of their prescribed doses. This information was compared with the orders written by the patient’s physician in the medical records, and any discrepancies were resolved by further querying the patient or the physician. Combination pills were counted according to the number of different drugs they contained.
Of 248 patients selected to participate in the ABPM and MEMS monitoring substudy,116 completed both ABPM and MEMS monitoring as part of the baseline data collection of a trial. During follow-up in the intervention clinics, an additional 24 patients not included in the baseline sample completed ABPM and MEMS monitoring on referral from their provider, and we included their data in our study. For these 24 patients, data on drug combinations and dosages prescribed at the time of ABPM and MEMS monitoring was collected in the study clinic.
Controlled hypertension was defined as ambulatory BP <135/85 mm Hg (weighted average day and night time) or <125/75 mm Hg if diabetic. Using a widely accepted definition, participants were classified as nonadherent if they took <80% of all prescribed doses, averaged across all monitored antihypertensives.17,18
Statistical Analysis
Descriptive statistics and frequencies were calculated. Characteristics of patients with uncontrolled resistant and white-coat hypertension were compared using Fisher exact tests and Mann-Whitney U tests (proportions and medians, respectively). All statistical tests were two-sided at α = .05. Data were analyzed using SPSS (version 20) for Windows (SPSS, Inc., Chicago, IL).
Results
There were 665 patients in the baseline sample of the clinical trial. In this study, we included 140 patients who completed 24-hour ABPM and electronic bottle cap monitoring (including 116 randomly selected at baseline and 24 patients who were referred for monitoring by their physicians in the intervention clinics). In general, characteristics of the monitored sample were similar to those of the 665 patients enrolled in the clinical trial.
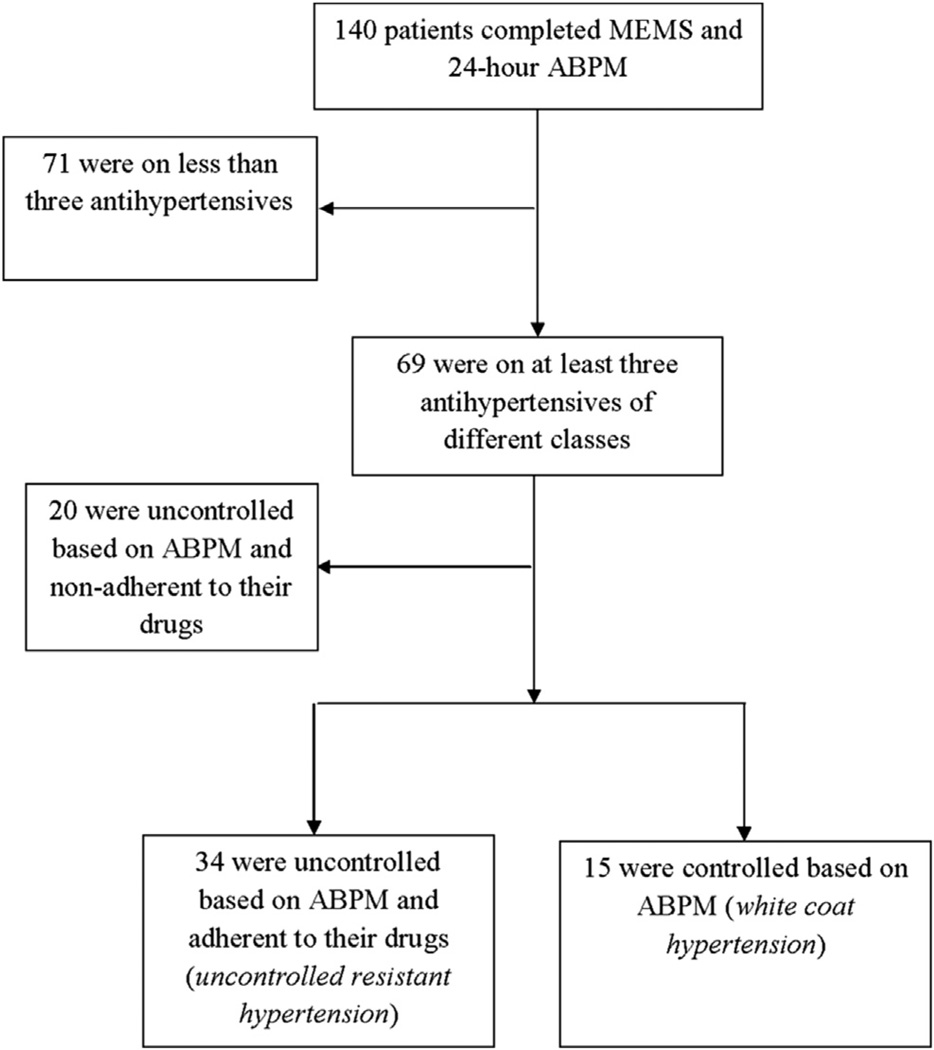
Of 140 patients monitored, 23 (16%) were on one antihypertensive drug, 48 (34%) were on two drugs, and 69 (50%) were on at least three drugs of different classes (Figure 1). This group of 69 patients would be classified as RH in some studies where more data were not available. Of these 69 patients, 15 (22%) were controlled based on ABPM (white coat hypertension). An additional 20 (29%) were uncontrolled but non-adherent, leaving only 34 (49%) adherent to their antihypertensive medications and having uncontrolled ambulatory hypertension (uncontrolled resistant hypertension [URH]; Figure 1).
Figure 1.
Flow chart describing patient selection for analyses. ABPM, Ambulatory blood pressure monitoring; MEMS, Medication Event Monitoring System.
Table 1 shows differences in characteristics between patients with URH and white-coat hypertension patients on at least three drugs. The median age of the URH patients was 59 years, the median body mass index (BMI) was 33 (kg/m2); the median 24-hour ambulatory SBP was 145 and DBP was 77. Compared with white-coat hypertension patients, those having URH were more likely to have diabetes (P =.002). Both 24-hour SBP and 24-hour DBP were significantly higher in URH patients (criteria for definition of groups). URH and white-coat hypertension patients did not differ significantly on age, gender, race/ethnicity, smoking status, BMI, employment status, and education (Table 1). Similar results were obtained when we restricted the analysis only to the patients selected at baseline.
Table 1.
Differences in characteristics between uncontrolled resistant hypertensive patients and patients with white-coat hypertension
| Uncontrolled Resistant (n = 34) | White-coat Hypertension (n = 15) | P value* | |
|---|---|---|---|
| Age | 59 (33–81) | 54 (35–74) | .063 |
| Female gender | 24 (71) | 10 (67) | .784 |
| African Americans | 21 (62) | 12 (80) | .324 |
| Current smoker | 8 (24) | 5 (33) | .500 |
| Diabetes | 24 (71) | 3 (20) | .002 |
| Employed | 10 (29) | 9 (60) | .059 |
| Less than high school education | 16 (47) | 5 (33) | .533 |
| BMI | 33 (22–52) | 31 (22–48) | .573 |
| Number of antihypertensives | 3 (3–5) | 3 (3–5) | .505 |
| 24-hour SBP | 145 (117–195) | 121 (101–134) | <.001 |
| 24-hour DBP | 77 (49–119) | 71 (55–81) | .031 |
BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Values are presented as number (percentage), or median (range).
P values refer to Fisher exact test for nominal variables and Mann-Whitney U tests for continuous variables.
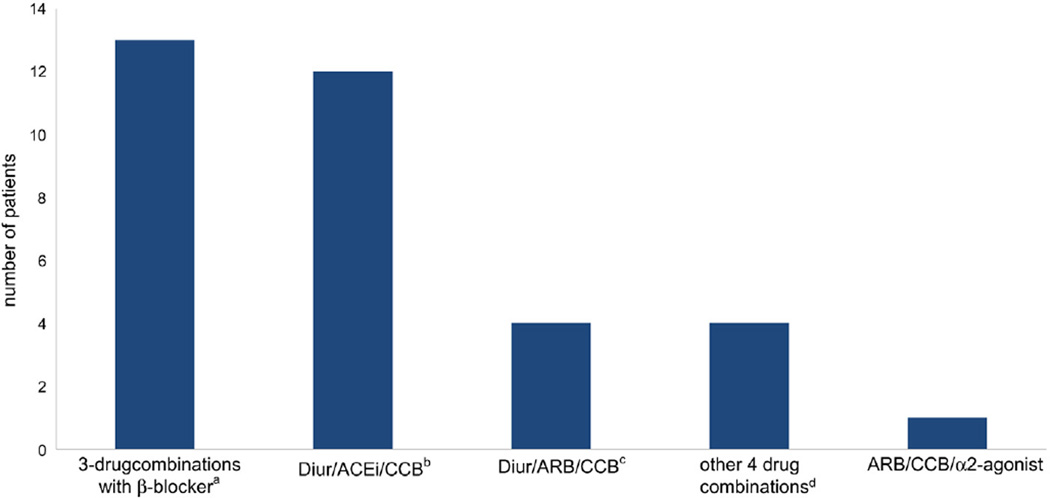
Figure 2 shows drug combinations of the URH patients. Of the 34 patients with URH, 23 were on three antihypertensives of different classes, eight were on four drugs, and three were on five drugs. Thirty-one (91%) of the 34 URH patients were prescribed a diuretic, of which 24 were on hydrochlorothiazide (HCTZ) 25 mg, four were prescribed Furosemide 40 mg, one Furosemide 80 mg, one HCTZ 50 mg, and one HCTZ-Triamterene 50 mg–75 mg. None of the patients was on spironolactone or eplerenone. Of the 25 patients on angiotensin-converting enzyme inhibitor (ACEi), 10 (40%) were prescribed the maximum dosage. Of the 10 patients on angiotensin receptor blocker (ARB), four were prescribed the maximum dosage, and of the 20 patients on calcium channel blockers (CCB), only three (15%) were prescribed the maximum dosage.
Figure 2.
Drug combinations of 34 patients with uncontrolled resistant hypertension. aIncluding eight patients on diuretic/ACEi/β-blocker; two on diuretic/ARB/β-blocker; one on diuretic/CCB/β-blocker; one on ACEi/CCB/β-blocker; and one on ARB/β-blocker/direct vasodilator. bIncluding eight patients on a three-drug combination of diuretic/ACEi/CCB; two on four-drug combination of diuretic/ACEi/CCB/β-blocker; and two on a five-drug combination of diuretic/ACEi/CCB/β-blocker/α2-agonist. cIncluding one patient on a three-drug combination of diuretic/ARB/CCB; two on a four-drug combination of diuretic/ARB/CCB/β-blocker; and one on diuretic/ARB/CCB/ACEi/β-blocker. dIncluding two patients on diuretic/ACEi/ARB/β-blocker; one on diuretic/CCB/β-blocker/α2-agonist; and one on diuretic/ACEi/β-blocker/α2-agonist. ACEi, Angiotension-converting enzyme inhibitor; ARB, angiotensin receptor blocker; CCB, calcium-channel blocker.
Thirteen patients (38%) were prescribed a three-drug combination with a beta-blocker (Figure 2). Sixteen (47%) of the URH patients were prescribed a combination of diuretic plus ACEi or ARB plus CCB, of which twelve patients were on diuretic plus ACEi plus CCB and four on diuretic plus ARB plus CCB (Figure 1).
Discussion
To the best of our knowledge, this is the first study that systematically excluded patients with both white coat hypertension based on 24-hour ABPM and poor adherence measured by MEMS from estimates of the fraction of hypertensives who could be classified as “resistant,” and the first to describe treatment dosages of PC patients with RH. In many investigations, ABPM and MEMS monitoring have been considered the gold standard for adherence assessment19 and BP measurement,20 respectively. We found that of the patients with RH (defined as uncontrolled office BP while being treated with at least three antihypertensives of different classes), 22% were misclassified due to the “white coat effect,” 29% had poor MA, and all of the remaining 49% were on apparently suboptimal drug combinations and/or dosages. Thirteen (38%) of the 34 URH patients were prescribed a three-drug combination with a beta-blocker, which might not be an optimal third agent for hypertension control.10,21,22 Use of beta-blockers as part of the treatment strategy was independently associated with RH in the study by Barochiner et al.10 In the multivariate analysis, the risk of RH was four times higher for those who used beta-blockers as part of the three-drug antihypertensive regimen, one of them being a diuretic.10
None of the URH patients were on chlorthalidone or an aldosterone antagonist, despite evidence-based recommendations to use these diuretics for RH patients.1 Only two of the 26 patients on HCTZ received 50 mg, despite superior BP reduction with 50 mg of HCTZ compared with 25 mg based on 24-hour ambulatory BP.23 Similarly, less than half of the patients on ACEi, ARB or CCB were prescribed maximal doses of these agents.
Our findings are in line with previous studies where white coat hypertension was present in 20% to 40% of patients attended in referral units.4,24 In terms of studies that examined primary care patients with resistant hypertension compared with referral center studies, our estimate of prevalence of white coat hypertension (22%) is somewhat lower than the prevalence reported by de la Sierra and colleagues (37.5%).4 This difference can be attributed to the lower cutoff of ambulatory BP for controlled hypertension in diabetic patients in our study. We obtained a similar estimate (33%) when we used the same cutoff value (130/80) in all patients on at least three drugs, one of them being a diuretic. Our study is the first that looked at rate of white coat hypertension in fairly unselected US primary care patients uncontrolled on at least three drugs.
Poor MA was another important contributing factor to RH in our study. This is in agreement with a study where observed drug taking (“tablet feed”), followed by office and ambulatory BP monitoring, identified a high proportion (about two-thirds) of RH patients whose elevated BP levels were due to poor MA.25
Use of suboptimal regimens and/or dosages was the third important contributing factor to RH in our study. National claims data describing the overall use of antihypertensives in the RH population also found that very low percentages of the patients were on chlorthalidone or on aldestorone antagonists (3% and 6%, respectively), and minimally efficacious combinations of antihypertensives were often prescribed.11
We did not find significant differences for age, gender, race/ethnicity, smoking status, BMI, employment status, and education between patients with URH and patients with white coat hypertension. These results are similar to comparisons presented by Acelajado et al, where patients with refractory hypertension (defined as hypertension that is uncontrolled in spite of maximal medical therapy) were compared with controlled group treated with a comparable number of antihypertensive medications.5 In contrast to the study by Acelejado et al, we did find a significant difference for diabetes, which can be explained by the lower cutoff of ambulatory BP for controlled hypertension in diabetic patients in our study. The difference for diabetes was no longer significant when we used the same cutoff value in all patients.
A limitation of our study is the lack of detailed data on clinical and biochemical parameters. We excluded patients with renal insufficiency or recent myocardial infarction; therefore, our results may not be generalizable to this population. A strength of our study is that we used gold standard methods for adherence assessment and BP measurement. Another limitation is that our sample included patients from two health care systems in a large city and may not be representative of the overall US population. However, our sample, comprised of socioeconomically and ethnically diverse hypertensive patients undergoing routine care in public and private PC clinics, is more likely to be typical of PC patients than a sample of volunteers.
Our results suggest that 24-hour ABPM and MA assessment may be an important step before further investigating or treating patients with RH. ABPM is crucial in identifying not only white coat hypertension, but also the possibility of masked hypertension in controlled patients.26 Improving MA would further reduce the prevalence of RH in primary care. In contemporary treated hypertensive patients, those classified as nonadherent are most commonly partially adherent.27,28 In our recent study, examining patterns of nonadherence to multiple antihypertensives, we found that most dose omissions were of short duration and could potentially be compensated for with long-acting antihypertensives.29 Encouraging full adherence remains an important public health priority. Our results also indicate a need for improvement regarding the treatment regimens and dosages. Maximizing the dose of diuretic therapy is an important treatment strategy in RH.11 Most of the URH patients might have been controlled if maximum recommended doses of diuretics and other agents had been prescribed.
In conclusion, half of the RH in our study can be explained by white coat effect and poor MA, and all of the remaining patients were on apparently suboptimal drug combinations and/or dosages. PC physicians need to be educated regarding the optimal treatment of RH, particularly with regard to diuretic use.
Acknowledgments
This study was supported by grant R01 HL078589 from the National Heart, Lung, and Blood Institute, National Institutes of Health.
Footnotes
No conflict of interests to declare.
References
- 1.Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistant hypertension: diagnosis, evaluation, and treatment: a scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Circulation. 2008;117:e510–e526. doi: 10.1161/CIRCULATIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 2.Cuspidi C, Macca G, Sampieri L, Michev I, Salerno M, Fusi V, et al. High prevalence of cardiac and extracardiac target organ damage in refractory hypertension. Journal Hypertens. 2001;19:2063–2070. doi: 10.1097/00004872-200111000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–1080. doi: 10.1161/HYPERTENSIONAHA.111.170308. [DOI] [PubMed] [Google Scholar]
- 4.de la Sierra A, Segura J, Banegas JR, Gorostidi M, de la Cruz JJ, Armario P, et al. Clinical features of 8295 patients with resistant hypertension classified on the basis of ambulatory blood pressure monitoring. Hypertension. 2011;57:898–902. doi: 10.1161/HYPERTENSIONAHA.110.168948. [DOI] [PubMed] [Google Scholar]
- 5.Acelajado MC, Pisoni R, Dudenbostel T, Dell’Italia LJ, Cartmill F, Zhang B, et al. Refractory hypertension: definition, prevalence, and patient characteristics. J Clin Hypertens (Greenwich) 2012;14:7–12. doi: 10.1111/j.1751-7176.2011.00556.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Irvin MR, Shimbo D, Mann DM, Reynolds K, Krousel-Wood M, Limdi NA, et al. Prevalence and correlates of low medication adherence in apparent treatment-resistant hypertension. J Clin Hypertens (Greenwich) 2012;14:694–700. doi: 10.1111/j.1751-7176.2012.00690.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KC. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation. 2011;124:1046–1058. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012;125:1635–1642. doi: 10.1161/CIRCULATIONAHA.111.068064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de la Sierra A, Banegas JR, Oliveras A, Gorostidi M, Segura J, de la Cruz J, et al. Clinical differences between resistant hypertensives and patients treated and controlled with three or less drugs. J Hypertens. 2012;30:1211–1216. doi: 10.1097/HJH.0b013e328353634e. [DOI] [PubMed] [Google Scholar]
- 10.Barochiner J, Alfie J, Aparicio LS, Cuffaro PE, Rada MA, Morales MS, et al. Prevalence and clinical profile of resistant hypertension among treated hypertensive subjects. Clin Exp Hypertens. 2012 doi: 10.3109/10641963.2012.739236. (in press). [DOI] [PubMed] [Google Scholar]
- 11.Hanselin MR, Saseen JJ, Allen RR, Marrs JC, Nair KV. Description of antihypertensive use in patients with resistant hypertension prescribed four or more agents. Hypertension. 2011;58:1008–1013. doi: 10.1161/HYPERTENSIONAHA.111.180497. [DOI] [PubMed] [Google Scholar]
- 12.Yiannakopoulou E, Papadopulos JS, Cokkinos DV, Mountokalakis TD. Adherence to antihypertensive treatment: a critical factor for blood pressure control. Eur J Cardiovasc Prev Rehabil. 2005;12:243–249. doi: 10.1097/00149831-200506000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Grigoryan L, Pavlik VN, Hyman DJ. Predictors of antihypertensive medication adherence in two urban health-care systems. Am J Hypertens. 2012;25:735–738. doi: 10.1038/ajh.2012.30. [DOI] [PubMed] [Google Scholar]
- 14.Ogedegbe G, Chaplin W, Schoenthaler A, Statman D, Berger D, Richardson T, et al. A practice-based trial of motivational interviewing and adherence in hypertensive African Americans. Am J Hypertens. 2008;21:1137–1143. doi: 10.1038/ajh.2008.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pavlik VN, Greisinger AJ, Pool J, Haidet P, Hyman DJ. Does reducing physician uncertainty improve hypertension control? rationale and methods. Circ Cardiovasc Qual Outcomes. 2009;2:257–263. doi: 10.1161/CIRCOUTCOMES.109.849984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyman DJ, Pavlik VN, Greisinger AJ, Chan W, Bayona J, Mansyur C, et al. Effect of a physician uncertainty reduction intervention on blood pressure in uncontrolled hypertensives–a cluster randomized trial. J Gen Intern Med. 2012;27:413–419. doi: 10.1007/s11606-011-1888-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sica DA. Fixed-dose combination antihypertensive drugs. Do they have a role in rational therapy? Drugs. 1994;48:16–24. doi: 10.2165/00003495-199448010-00003. [DOI] [PubMed] [Google Scholar]
- 18.Okano GJ, Rascati KL, Wilson JP, Remund DD, Grabenstein JD, Brixner DI. Patterns of antihypertensive use among patients in the us department of defense database initially prescribed an angiotensin-converting enzyme inhibitor or calcium channel blocker. Clin Ther. 1997;19:1433–1445. doi: 10.1016/s0149-2918(97)80017-3. discussion 1424-35. [DOI] [PubMed] [Google Scholar]
- 19.Choo PW, Rand CS, Inui TS, Lee ML, Cain E, Cordeiro-Breault M, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37:846–857. doi: 10.1097/00005650-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Verdecchia P, Reboldi G, Porcellati C, Schillaci G, Pede S, Bentivoglio M, et al. Risk of cardiovascular disease in relation to achieved office and ambulatory blood pressure control in treated hypertensive subjects. J Am Coll Cardiol. 2002;39:878–885. doi: 10.1016/s0735-1097(01)01827-7. [DOI] [PubMed] [Google Scholar]
- 21.Wiysonge CS, Bradley HA, Volmink J, Mayosi BM, Mbewu A, Opie LH. Beta-blockers for hypertension. Cochrane Database Syst Rev. 2012;8 doi: 10.1002/14651858.CD002003.pub3. CD002003. [DOI] [PubMed] [Google Scholar]
- 22.De Caterina AR, Leone AM. The role of beta-blockers as first-line therapy in hypertension. Curr Atheroscler Rep. 2011;13:147–153. doi: 10.1007/s11883-010-0157-9. [DOI] [PubMed] [Google Scholar]
- 23.Messerli FH, Makani H, Benjo A, Romero J, Alviar C, Bangalore S. Antihypertensive efficacy of hydrochlorothiazide as evaluated by ambulatory blood pressure monitoring: a meta-analysis of randomized trials. J Am Coll Cardiol. 2011;57:590–600. doi: 10.1016/j.jacc.2010.07.053. [DOI] [PubMed] [Google Scholar]
- 24.Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am J Hypertens. 2001;14:1263–1269. doi: 10.1016/s0895-7061(01)02193-8. [DOI] [PubMed] [Google Scholar]
- 25.Bunker J, Callister W, Chang CL, Sever PS. How common is true resistant hypertension? J Hum Hypertens. 2011;25:137–140. doi: 10.1038/jhh.2010.108. [DOI] [PubMed] [Google Scholar]
- 26.Schmieder RE, Lehmann MV, Schmidt S. Optimizing blood pressure control in hypertension: The need to use abpm. Blood Press. 2013;22:65–72. doi: 10.3109/08037051.2012.727253. [DOI] [PubMed] [Google Scholar]
- 27.Rose AJ, Berlowitz DR, Manze M, Orner MB, Kressin NR. Intensifying therapy for hypertension despite suboptimal adherence. Hypertension. 2009;54:524–529. doi: 10.1161/HYPERTENSIONAHA.109.133389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rose AJ, Glickman ME, D’Amore MM, Orner MB, Berlowitz D, Kressin NR. Effects of daily adherence to antihypertensive medication on blood pressure control. J Clin Hypertens (Greenwich) 2011;13:416–421. doi: 10.1111/j.1751-7176.2011.00427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grigoryan L, Pavlik VN, Hyman DJ. Patterns of nonadherence to antihypertensive therapy in primary care. J Clin Hypertens (Greenwich) 2013;15:107–111. doi: 10.1111/jch.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]