Abstract
Background and Aim:
Differences in patient characteristics due to race or ethnicity may influence the incidence of difficult airway. Our purpose was to determine the incidence of difficult laryngoscopy and intubation, as well as the anatomical features and clinical risk factors that influence them, in the Indian population.
Methods:
In 330 adult patients receiving general anaesthesia with tracheal intubation, airway characteristics and clinical factors were determined and their association with difficult laryngoscopy (Cormack and Lehane grade 3 and 4) was analysed. Intubation Difficulty Scale score was used to identify degree of difficult laryngoscopy.
Results:
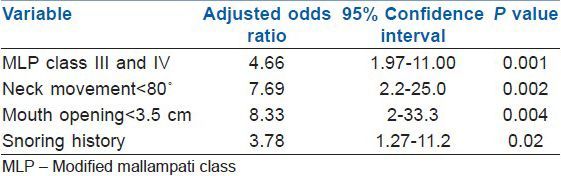
The incidence of difficult laryngoscopy and intubation was 9.7% and 4.5%, respectively. Univariate analysis showed that increasing age and weight, male gender, modified Mallampati class (MMC) 3 and 4 in sitting and supine positions, inter-incisor distance (IID) ≤3.5 cm, thyromental (TMD) and sternomental distance, ratio of height and TMD, short neck, limited mandibular protrusion, decreased range of neck movement, history of snoring, receding mandible and cervical spondylosis were associated with difficult laryngoscopy. Multivariate analysis identified four variables that were independently associated with difficult laryngoscopy: MMC class 3 and 4, range of neck movement <80°, IID ≤ 3.5 cm and snoring.
Conclusions:
We found an incidence of 9.7% and 4.5% for difficult laryngoscopy and difficult intubation, respectively, in Indian patients with apparently normal airways. MMC class 3 and 4, range of neck movement <80°, IID ≤ 3.5 cm and snoring were independently related to difficult laryngoscopy. There was a high incidence (48.5%) of minor difficulty in intubation.
Keywords: Airway evaluation, difficult intubation, difficult laryngoscopy, intubation difficulty scale
INTRODUCTION
Difficulty in airway management is a major cause of morbidity and mortality in anaesthetic practice. The ability to identify patients at risk of difficult tracheal intubation is important especially in patients with apparently normal airways. Difficult laryngoscopy (poor glottis visualization) is considered a surrogate indicator of difficult intubation. Preoperative assessment of various anatomic and clinical features helps in identifying potentially difficult laryngoscopy. The diagnostic accuracy of these screening tests varies between different studies. This is attributed to difference in incidence of difficult laryngoscopy, inadequate statistical power, different test thresholds and differences in patient characteristics.[1]
Differences in patient characteristics due to race or ethnicity may influence the incidence of difficult laryngoscopy and difficult intubation. The majority of studies of difficult laryngoscopy and intubation have been performed in the American or European population.[1,2,3,4,5,6] Anthropometrically, Indians are different compared to the Americans or Europeans. Adequate data of normal values in a given population may help the clinician to identify patients who are outside the range and therefore potentially challenging. Moreover, most studies do not provide a ‘measure’ of difficult intubation in patients with difficult laryngoscopy. To address this issue, we undertook a prospective study to determine: (1) the incidence of difficult laryngoscopy and difficult intubation; (2) the anatomic and clinical risk factors associated with difficult laryngoscopy; (3) to characterise the degree of difficulty in tracheal intubation in the Indian patient population.
METHODS
After obtaining approval from the local ethics committee and written informed consent from patients, 330 adult ASA physical status I and II adult patients scheduled for elective surgery under general anaesthesia requiring tracheal intubation were included in this prospective study. Patients with obvious abnormality of the airway where intubation under general anaesthesia would be contraindicated, those at increased risk of aspiration, inter-incisor distance <2.5 cm and unstable cervical spine were excluded from the study.
The following airway characteristics were assessed preoperatively by one investigator to reduce inter-observer variability: (1) modified Mallampati class (MMC)[2] of oropharyngeal view obtained with the patient sitting and also in the supine position (tongue protruding, without phonation); (2) inter-incisor distance (IID) < or > 3.5 cm with the mouth fully open (inter-gingival distance in edentulous patients); (3) thyromental distance (TMD) and sternomental distance (SMD) obtained by measuring the straight distance from thyroid notch and sternal notch to the inner mentum, respectively, with the head in extension; (4) range of head and neck movement < or > 80° as described by Wilson et al.;[3] (5) mandibular protrusion limitation; the lower incisors can be brought in front of the upper incisors or the lower incisors can be advanced only to the level of upper incisors or cannot reach the level of the upper incisors; (6) ratio of height (cm) and TMD (cm) [RHTMD] and body mass index (BMI), kg/m2 was calculated; (7) dentition: Loose, missing, protruding teeth or edentulous; (8) other features such as history of snoring, hypertension or diabetes, short muscular neck, beard or cervical spondylosis were noted. All patients fasted overnight and received oral alprazolam 0.25 mg/0.5 mg (< or > 50 kg body weight, respectively) the night before and on the morning of surgery.
In the operating room, standard monitoring was established (electrocardiogram, non-invasive blood pressure, pulse oximetry, capnography). A difficult airway cart was kept at hand.
The height of the operating table was adjusted such that the plane of the patient's face was at the level of xiphisternum of the anaesthesiologist performing laryngoscopy and intubation. Anaesthesia was induced with fentanyl 2 μg/kg and propofol 2-2.5 mg/kg until loss of verbal contact. Intubation was facilitated by vecuronium 0.1 mg/kg. The lungs were ventilated with O2, N2O and isoflurane 0.6% for 3 minutes. Degree of difficulty with mask ventilation was graded as easy, difficult or impossible.[4]
Intubation was performed using Macintosh size 3 blade with the patients’ head in sniffing position by anaesthesiologists with more than five years experience in anaesthesia who were unaware of the airway measurements. Tracheal tubes size 7 and 8 were used in female and male patients, respectively. Laryngoscopic view was graded by Cormack and Lehane grading[5] without external laryngeal pressure (ELP). Cormack grade 3 and 4 were regarded as difficult laryngoscopy. ELP was permitted to facilitate intubation and the Cormack grade obtained following ELP was also noted. Intubation difficulty was assessed by the Intubation Difficulty Scale (IDS) score.[6] The number of attempts and operators, alternate intubation techniques used, Cormack grade, lifting force used, need for external laryngeal pressure and vocal cord position were noted. Alternative techniques included patient repositioning, change of blade or tracheal tube, use of stylet, laryngeal mask airway (LMA), intubating LMA, fibreoptic intubation or intubation through LMA. IDS score = 0 represented easy intubation, IDS score = 1-5 represented slight difficulty and IDS score >5 represented moderate to major difficulty in intubation.[6] Duration of laryngoscopy was recorded. The stance of the anaesthesiologist performing laryngoscopy and intubation (upright or leaning backwards, bending at the knee or stooping) was also noted. The study ended after successful tracheal intubation was confirmed by assessment of chest movement, auscultation and capnography.
Assuming an incidence of difficult laryngoscopy of 8%[7] and an error of 3%, a sample size of 327 patients would be required to find significant differences between patients with easy and difficult laryngoscopy. We included 330 patients. Descriptive statistics in the form of mean, standard deviation for interval variables and frequency and percentage for categorical variables have been performed. Student's t-test was performed to see significant differences between easy and difficult laryngoscopy for interval variables. Chi-square tests with Yates correction factor were used to see association between the two groups for categorical variables. All significant and important variables were selected for multivariate logistic regression analysis. Stepwise forward multivariate logistic regression analysis was performed to see important risk factors for difficult laryngoscopy. Adjusted odds ratio and 95% confidence interval were presented. A P value 0.05 (two-tailed) was considered to be of statistically significant level. SPSS 19.0 statistical package was used for the analysis.
RESULTS
A total of 330 patients were included in the study. The demographic and airway characteristics of the study population are presented in Table 1. Mask ventilation was easy in 293 (88.8%), difficult in 36 (10.9%) and impossible in 1 (0.3%) of 330 patients. There was no significant difference between the Easy and Difficult laryngoscopy groups with regard to difficulty in mask ventilation (P = 0.312). The incidence of difficult laryngoscopy was 9.7%. The duration of laryngoscopy was 13.4 ± 5.5 and 28.2 ± 21.5 s in patients with easy and difficult laryngoscopy, respectively (P = 0.000). There were no failed intubations.
Table 1.
Overall patient data
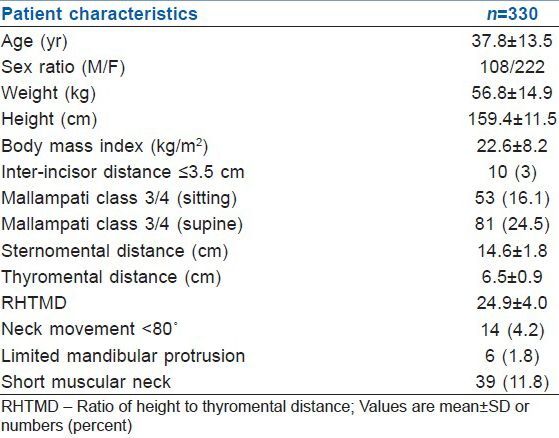
The distribution of airway characteristics between the Easy (Cormack grade 1 and 2) and Difficult (Cormack grade 3 and 4) laryngoscopy groups are shown in Tables 2 and 3. The incidence of MMC zero airway was 1.7% (5 of 330 patients; 3 females and 2 males). The supine position worsened the MMC view [Table 1]. Both MMC in the sitting position and supine position were statistically significantly related to difficult laryngoscopy (P = 0.000 and 0.004, respectively).
Table 2.
Demographic data of patients in the easy and difficult laryngoscopy groups
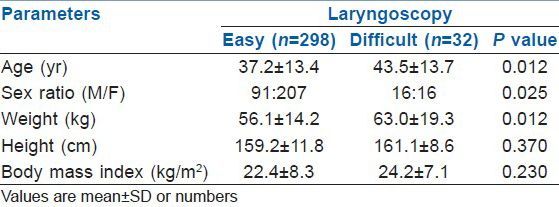
Table 3.
Airway characteristics in the easy and difficult laryngoscopy groups
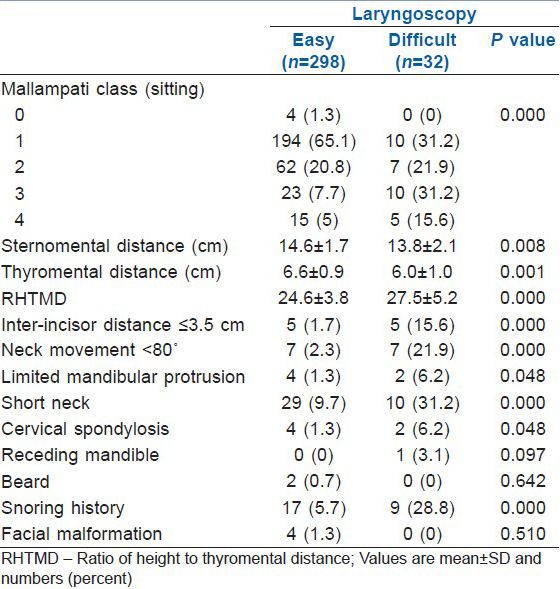
Univariate analysis demonstrated several risk factors that were associated with difficult laryngoscopy: increasing age, weight, male gender, modified Mallampati class 3 and 4 in sitting and supine positions, TMD, RHTMD, SMD, short neck, limited mandibular protrusion, decreased range of neck movement, history of snoring, receding mandible and cervical spondylosis [Tables 2 and 3]. Multivariate analysis identified four variables that were independently associated with difficult laryngoscopy [Table 4]. These were modified Mallampati class 3 and 4, range of neck movement <80°, IID ≤ 3.5 cm and a history of snoring.
Table 4.
Predictors of difficult laryngoscopy through multivariate logistic regression with forward selection
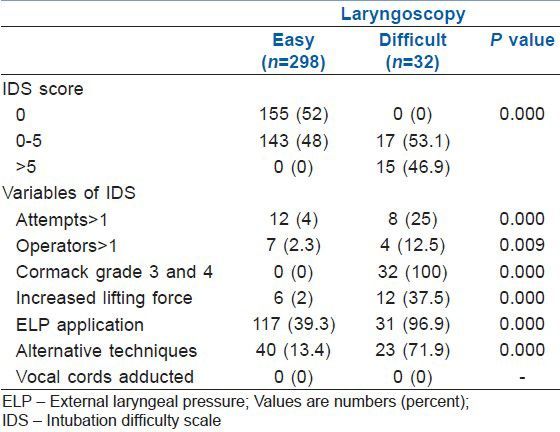
The distribution of Cormack and Lehane grades without and with external laryngeal pressure (ELP) are presented in Table 5. IDS scores ranged between 0 and 16. Intubation was judged to be easy (IDS score = 0) in 155 (47%) and minor difficulty (IDS score 1-5) was experienced in 160 (48.5%) of 330 patients. Moderate to major difficulty (IDS score >5) was seen in 15 of 330 patients (4.5%). The distribution of IDS scores and its variables between the two groups are depicted in Table 6. Use of stylet was the most commonly employed alternative technique (13.6%), followed by change in patient position (0.9%) and laryngoscope blade (0.9%).
Table 5.
Distribution of Cormack and Lehane grades without and with external laryngeal manipulation between the easy and difficult laryngoscopy groups
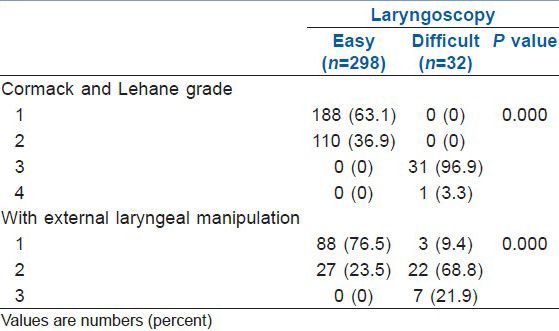
Table 6.
Intubation difficulty scale score and variables of IDS
There was a statistically significant difference between the two groups in the stance adopted by the anaesthesiologists performing laryngoscopy and intubation; in 50% (16 of 32 patients) of cases in the difficult laryngoscopy group, the anaesthesiologist leaned backwards, bent at the knee or stooped to bring the face closer to the patient during laryngoscopy and intubation to obtain the best laryngeal view compared with 18.9% (56 of 278 patients) in the easy laryngoscopy group (P <0.001).
DISCUSSION
We found an incidence of 9.7% and 4.5% for difficult laryngoscopy and difficult tracheal intubation (IDS score >5), respectively. Difficult laryngoscopy was independent of degree of difficulty in mask ventilation. We identified four risk factors associated with difficult laryngoscopy: Mallampati class 3-4, range of head and neck movement <80°, IID ≤ 3.5 cm and history of snoring. There was a high incidence of minor (IDS score1-5) intubation difficulty (48.5%). External laryngeal pressure (ELP) and use of alternative techniques (stylet, change in patient position or blade) were used in decreasing frequency to facilitate intubation.
Our data demonstrate that increasing age, weight and male gender were associated with difficult laryngoscopy. An association between difficult laryngoscopy and older[8,9,10] and heavier patients has been reported.[10] Osteoarthritic changes and poor dentition may be responsible for the age-related increase in difficult laryngoscopy.[11] A significant proportion of difficult tracheal intubations has been found in males,[11] attributed to differences in neck fat deposition between the sexes.[12] Obesity has been found to be a risk factor for difficult intubation.[8,11] while other investigators[13] found no such association. Though patients in difficult laryngoscopy group were heavier than those in the easy laryngoscopy group, we did not find BMI to be a risk factor for difficult laryngoscopy. Savva[14] did not report any difference in age, sex, weight or height between easy and difficult laryngoscopy groups.
TMD in the difficult laryngoscopy group was significantly shorter (6.0 ± 1.0 cm) compared with that in the easy (6.6 ± 0.9 cm) laryngoscopy group. A positive correlation between short TMD and difficult laryngoscopy has been reported[9,15,16,17,18] while others have found no such correlation.[11,19] Cut-off values of TMD for predicting difficult laryngoscopy range from 5.5 to 7.0 cm.[18] Mean TMD in our patients was 6.5 ± 0.9 cm in contrast to 7.9 ± 1.2 cm reported by Schmitt et al.[18] TMD is related to body size and proportion. The mean height of our patients (159 ± 12 cm) is shorter than that reported in the study by Schmitt et al. (171 ± 9 cm).[18] Therefore, RHTMD is considered a better indicator of difficult intubation than TMD.[18,20,21] Mean RHTMD in our study was 24.9 ± 4 that compares with 22.1 ± 3.0 reported by Schmitt et al.[18] Cut-off values for RHTMD recommended for predicting difficult laryngoscopy are 25 in Caucasians,[18] 24 in Iranian patients[19] and 23.5 in Thai patients.[20] Krishna et al.[21] used a cut-off value suggested by Schmitt et al.[18] (≥25) in their study. In our study RHTMD was significantly higher in patients in the difficult laryngoscopy group (27.5 ± 5.2) compared with that in the easy laryngoscopy group (24.6 ± 3.8).
Sternomental distance (SMD) is an indicator of head and neck mobility.[10] No study has addressed the correlation between SMD and difficult laryngoscopy in the Indian population. There was a statistically significant difference between SMD in the easy and difficult laryngoscopy groups (14.6 ± 1.7 cm and 13.8 ± 2.1 cm, respectively). The cut-off point of SMD suggested for predicting difficult laryngoscopy is 12.5 cm[14] and 13.5 cm.[10] Our aim was to evaluate anatomical measurements commonly used to predict a difficult airway in the Indian population, thereby revealing differences with measurement values obtained in non-Indian patients. We did not attempt to define cut-off values for TMD, SMD or RHTMD in this study as the sample size was not large enough to determine the cut-off threshold values. It is important to note that no single anatomical factor determines the ease of difficult laryngoscopy and therefore no single anatomic factor can be used to predict a difficult intubation.
The incidence of difficult laryngoscopy (Cormack grade 3-4) differs in various studies; it was reported to be 3.4% in West African population,[17] 8.2% in a predominantly Chinese population[22] and 23.1% in Iranian population.[19] Amongst studies in the Indian population, Krishna et al.[21] reported an incidence of 8.5%. However, they graded Cormack scores as the best view obtained with optimal laryngeal manipulation. In contrast, in a predominantly Kashmiri population, the incidence of difficult laryngoscopy was only 3.3%.[16] In our study, the incidence of difficult laryngoscopy was 9.7% without ELP; the incidence decreased to 2.1% following ELP application.
On multivariate analysis, Mallampati class 3 and 4, range of neck movement <80°, IID ≤ 3.5 cm and snoring were independently related to difficult laryngoscopy. Previous studies have identified Mallampati class 3 and 4,[11,15,16,20] decreased range of neck movement,[9,16,19,20] decreased IID[3,15,17,18,19] and snoring[23] as predictors of difficult laryngoscopy.
The incidence of modified Mallampati class zero was 1.7% in our study which is comparable with that reported by Ezri et al.[11] (1.8%) and Hegde et al.[24] (1.7%). All patients with class zero airway had a Cormack grade 1laryngoscopic view. MMC zero per se is not associated with difficult laryngoscopy.[24] While Mallampati class obtained in the sitting position is standard, at times airway examination in the sitting position may not be convenient, possible or advisable. Elderly, very sick and bed-ridden patients, those requiring emergency tracheal intubation or patients with prolapsed disc and fracture spine may not be able to sit up for assessment.[25] MMC class 3-4 was observed in more patients in the supine position compared with sitting position (24.5% versus 16.1%, respectively) as has been reported previously.[25,26,27] There was a statistically significant association between MMC in the supine position with difficult laryngoscopy (P = 0.004), but less so than MMC in the sitting position (P = 0.000). Airway evaluation in both the positions almost equally predicts for difficult laryngoscopy.[25,26]
We found snoring to be an independent risk factor for difficult laryngoscopy. Snoring occurs more frequently in males, overweight patients, worsens with age and is associated with obstructive sleep apnoea which possibly explains its association with difficult laryngoscopy.[23] Diabetes is known to be associated with difficult laryngoscopy as was also seen in this study. An interesting finding of our study is that hypertensive patients were found to have a significant association with difficult laryngoscopy on univariate analysis.
There are anthropometric differences between the Indian population and the American or European population. The average height of an American adult male and female (1.776 m and 1.632 m, respectively)[28] is considerably greater than that of an Indian male and female (1.612 m and 1.521 m, respectively).[29] This probably translates into differences in the anatomical indices that are commonly used to predict difficult laryngoscopy. Naguib et al.[30] found the mean TMD of patients in the easy and difficult laryngoscopy groups of 7.6 ± 0.9 and 6.45 ± 1.6 cm, respectively, that is greater compared to that found in our study (6.6 ± 0.9 and 6.0 ± 1.0, respectively). Likewise, the mean TMD in European patients with easy and difficult mask ventilation reported by Langeron et al.[4] is 8.9 ± 1.6 and 8.5 ± 1.3 cm, respectively, considerably greater than TMD in our study. Safavi et al.[31] concluded that the cut-off point for RHTMD for prediction of direct laryngoscopy is race dependent and recommend calculating cut-off point for each population separately.
Most previous studies in the Indian population have considered difficult laryngoscopy as indicative of difficult intubation.[16,21,32] Although, difficult laryngoscopy is an important component of difficult intubation, the two may not always be necessarily correlated.[33] The incidence of moderate to major difficult tracheal intubation (IDS >5) was 4.5% in our study. We found a high incidence of minor difficulty in intubation (48.5%). Similarly, Adnet et al.[15] reported minor intubation difficulty in 37% and moderate to major difficulty in 8% of patients. Likewise, Schmitt et al.[18] found 55% of patients to have no difficulty, 37.3% minor difficulty and 7.7% to have major difficulty in intubation.
Few studies have used the IDS score to assess tracheal intubation in the Indian population. Prakash et al.[7] reported an 8% incidence of difficult laryngoscopy and found easy intubation in 60.4%, minor difficulty in 38.2% and moderate to major difficulty in 1.5% patients. In contrast, Ambardekar et al.[34] reported difficult laryngoscopy in only 1.67% and moderate to major intubation difficulty in 0.67% patients. Gangadhar et al.[35] reported a positive correlation between MMC class 1/2 and easy intubation, an incidence of Cormack grade 3/4 of 8.3% and difficulty in 35% of intubations in 60 patients undergoing tracheal intubation with cricoid pressure in the emergency department.
The anaesthesiologists in the easy laryngoscopy group adopted an erect posture in 81.1% of cases. In contrast, in 50% of cases in the difficult laryngoscopy group, the anaesthesiologists bent at their knees, stooped or leaned their upper body backwards to align the line of vision and the laryngeal axis.
CONCLUSION
We found an incidence of 9.7% and 4.5% for difficult laryngoscopy and difficult intubation, respectively, in Indian patients with apparently normal airways. Mallampati class 3-4, range of neck movement < 80°, inter-incisor distance ≤ 3.5 cm and snoring were independently related to difficult laryngoscopy. Our results reveal that there are differences in anatomical measurements commonly used to predict a difficult airway between the Indian and non-Indian population. This implies that standard threshold values for predicting a difficult airway may not apply in the Indian population.
Footnotes
Source of Support: Institutional
Conflict of Interest: None declared.
REFERENCES
- 1.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 3.Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61:211–6. doi: 10.1093/bja/61.2.211. [DOI] [PubMed] [Google Scholar]
- 4.Langeron O, Masso E, Huraux C, Guggiari M, Bianchi A, Coriat P, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–36. doi: 10.1097/00000542-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 6.Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The Intubation Difficulty Scale (IDS): Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–7. doi: 10.1097/00000542-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Prakash S, Rapsang AG, Mahajan S, Bhattacharjee S, Singh R, Gogia AR. Comparative Evaluation of the Sniffing Position with Simple Head Extension for Laryngoscopic View and Intubation Difficulty in Adults Undergoing Elective Surgery. Anesthesiol Res Pract 2011. 2011 doi: 10.1155/2011/297913. 297913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rose DK, Cohen MM. The airway: Problems and predictions in 18,500 patients. Can J Anaesth. 1994;41:372–83. doi: 10.1007/BF03009858. [DOI] [PubMed] [Google Scholar]
- 9.Nath G, Sekar M. Predicting difficult intubation: A comprehensive scoring system. Anaesth Intensive Care. 1997;25:482–6. doi: 10.1177/0310057X9702500505. [DOI] [PubMed] [Google Scholar]
- 10.Ramadhani SA, Mohamed LA, Rocke DA, Gouws E. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. Br J Anaesth. 1996;77:312–6. doi: 10.1093/bja/77.3.312. [DOI] [PubMed] [Google Scholar]
- 11.Ezri T, Gewürtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, et al. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58:1111–4. doi: 10.1046/j.1365-2044.2003.03412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ. Neck soft tissue and fat distribution: Comparison between normal men and women by magnetic resonance imaging. Thorax. 1999;54:323–8. doi: 10.1136/thx.54.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meyer RJ. Obesity and difficult intubation. Anaesth Intensive Care. 1994;22:314–5. [PubMed] [Google Scholar]
- 14.Savva D. Prediction of difficult tracheal intubation. Br J Anaesth. 1994;73:149–53. doi: 10.1093/bja/73.2.149. [DOI] [PubMed] [Google Scholar]
- 15.Adnet F, Racine SX, Borron SW, Clemessy JL, Fournier JL, Lapostolle F, et al. Acta A survey of tracheal intubation difficulty in the operating room: A prospective observational study. Anaesthesiol Scand. 2001;45:327–32. doi: 10.1034/j.1399-6576.2001.045003327.x. [DOI] [PubMed] [Google Scholar]
- 16.Gupta AK, Ommid M, Nengroo S, Naqash I, Mehta A. Predictors of difficult intubation: Study in Kashmiri population. British Journal of Medical Practitioners. 2010;3:307–12. [Google Scholar]
- 17.Merah NA, Foulkes-Crabbe DJ, Kushimo OT, Ajayi PA. Prediction of difficult laryngoscopy in a population of Nigerian obstetric patients. West Afr J Med. 2004;23:38–41. doi: 10.4314/wajm.v23i1.28079. [DOI] [PubMed] [Google Scholar]
- 18.Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient's height to thyromental distance improves prediction of difficult laryngoscopy. Anaesth Intensive Care. 2002;30:763–5. doi: 10.1177/0310057X0203000607. [DOI] [PubMed] [Google Scholar]
- 19.Farzi F, Mirmansouri A, Forghanparast K, Abdolahzade M, Nahvi H. Difficult laryngoscopy; the predictive value of ratio of height to thyromental distance versus other common predictive tests of upper airway. Prof Med J. 2012;19:6. [Google Scholar]
- 20.Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: Four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–5. doi: 10.1213/01.ANE.0000181000.43971.1E. [DOI] [PubMed] [Google Scholar]
- 21.Krishna HM, Agarwal M, Dali JS, Rampal P, Dua CK. Prediction of difficult laryngoscopy in Indian population: Role of patient's height to thyromental distance. J Anaesth Clin Pharmacol. 205;;1:257–60. [Google Scholar]
- 22.Butler PJ, Dhara SS. Prediction of difficult laryngoscopy: An assessment of the thyromental distance and Mallampati predictive tests. Anaesth Intensive Care. 1992;20:139–42. doi: 10.1177/0310057X9202000202. [DOI] [PubMed] [Google Scholar]
- 23.Dabbagh A, Rad MP, Daneshmand A. The relationship between night time snoring and Cormack and Lehane grading. Acta Anaesthesiol Taiwan. 2010;48:172–3. doi: 10.1016/j.aat.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Hegde HV, Prasad KC, Bhat MT, Hegde JS, Santhosh Mysore Cb, Yaliwal VG, et al. Airway difficulty in Mallampati ‘class zero’ patients: A prospective double-blind observational study. Eur J Anaesthesiol. 2012;29:338–42. doi: 10.1097/EJA.0b013e3283542407. [DOI] [PubMed] [Google Scholar]
- 25.Khatiwada S, Bhattarai B, Pokharel K, Acharya R, Ghimire A, Baral DD. Comparison of modified Mallampati test between sitting and supine positions for prediction of difficult intubation. Health Renaiss. 2012;10:12–5. [Google Scholar]
- 26.Kim DS, Kim KH. Assessment of the modified mallampati classification on supine position. Korean J Anesthesiol. 2000;38:789–94. [Google Scholar]
- 27.Singhal V, Sharma M, Prabhakar H, Ali Z, Singh GP. Effect of posture on mouth opening and modified Mallampati classification for airway assessment. J Anesth. 2009;23:463–5. doi: 10.1007/s00540-009-0761-4. [DOI] [PubMed] [Google Scholar]
- 28.McDowell MA, Fryar CD, Ogden C, Flegal KM. National Health Statistics Reports 10. National Center for Health Statistics; [Last accessed on 2008 Oct 22]. Anthropometric Reference Data for Children and Adults: United States, 2003–2006. Available from: http://www.cdc.gov/nchs/data/nhsr/nhsr010.pdf . [PubMed] [Google Scholar]
- 29.Mamidi RS, Kulkarni B, Singh A. Secular trends in height in different states of India in relation to socioeconomic characteristics and dietary intakes. Food Nutr Bull. 2011;32:23–34. doi: 10.1177/156482651103200103. [DOI] [PubMed] [Google Scholar]
- 30.Naguib M, Malabarey T, AlSatli RA, Damegh SA, Samarkandi AH. Predictive models for difficult laryngoscopy and intubation. A clinical, radiologic and three-dimensional computer imaging study. Can J Anaesth. 1999;46:748–59. doi: 10.1007/BF03013910. [DOI] [PubMed] [Google Scholar]
- 31.Safavi M, Honarmand A, Zare N. A comparison of the ratio of patient's height to thyromental distance with the modified Mallampati and the upper lip bite test in predicting difficult laryngoscopy. Saudi J Anaesth. 2011;5:258–63. doi: 10.4103/1658-354X.84098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mishra SK, Bhat RR, M. Nagappa SK, Badhe A. Comparison of upper lip bite test with modified Mallampati classification for prediction of difficult obstetric intubation. Internet J Anesthesiol. 2009;19:6. [Google Scholar]
- 33.García-Guiral M, García-Amigueti F, Ortells-Polo MA, Muiños-Haro P, Gallego-González J, Carral-Olondris JN. Relationship between laryngoscopy degree and intubation difficulty. Rev Esp Anestesiol Reanim. 1997;44:93–7. [PubMed] [Google Scholar]
- 34.Ambardekar M, Pandya S, Ahuja P. Comparison of the sniffing position with simple head extension for laryngoscopic view in elective surgical patients. Internet J Anesthesiol. 2008;17:15. [Google Scholar]
- 35.Gangadharan L, Sreekanth C, Vasnaik MC. Prediction of difficult intubations using conventional indicators; Does rapid sequence intubation ease difficult intubations? A prospective randomized study in a tertiary care teaching hospital. J Emerg Trauma Shock. 2011;4:42–7. doi: 10.4103/0974-2700.76836. [DOI] [PMC free article] [PubMed] [Google Scholar]


