Abstract
Efficacious treatments for seasonal affective disorder include light therapy and a seasonal affective disorder-tailored form of cognitive-behavioral therapy. Using data from a parent clinical trial, these secondary analyses examined the relationship between cognitive change over treatment with cognitive-behavioral therapy, light therapy, or combination treatment and mood outcomes the next winter. Sixty-nine participants were randomly assigned to 6-weeks of cognitive-behavioral therapy, light therapy, or combination treatment. Cognitive constructs (i.e., dysfunctional attitudes, negative automatic thoughts, and rumination) were assessed at pre- and post-treatment. Dysfunctional attitudes, negative automatic thoughts, and rumination improved over acute treatment, regardless of modality; however, in participants randomized to solo cognitive-behavioral therapy, a greater degree of improvement in dysfunctional attitudes and automatic thoughts was uniquely associated with less severe depressive symptoms the next winter. Change in maladaptive thoughts during acute treatment appears mechanistic of solo cognitive-behavioral therapy’s enduring effects the next winter, but is simply a consequence of diminished depression in light therapy and combination treatment.
Keywords: Seasonal affective disorder, light therapy, cognitive-behavioral therapy, cognitive mechanisms, treatment durability
Winter seasonal affective disorder (SAD) is a subtype of recurrent depression characterized by a regular seasonal pattern of major depressive episodes during the fall and/or winter months (Rosenthal et al., 1984). SAD is associated with impaired psychosocial functioning during the winter months (Schlager, Froom, & Jaffe, 1995) with symptoms such as a depressed mood, anhedonia, a significant change in sleep length, eating and weight changes, fatigue, and difficulty concentrating (Rosenthal et al., 1984).
Light therapy is empirically-supported and currently the gold standard treatment for acute SAD, prescribed as exposure to bright artificial light in the morning hours, daily through the fall and winter months (Lewy, Sack, Miller, & Hoban,1987; Lewy et al., 1998; Terman, Terman, Lo, & Cooper, 2001; Terman & Terman, 2005). Preliminary studies suggest that a form of cognitive-behavioral therapy (CBT)1 tailored specifically for SAD (Rohan, 2008) is comparably efficacious to light therapy in the acute treatment of SAD (Rohan, Tierney Lindsey, Roecklein, & Lacy, 2004; Rohan et al., 2007). Additionally, acute CBT treatment also appears to buffer against relapse the following winter, as evident by fewer SAD episode recurrences and less severe patient- and interviewer-rated depressive symptoms during the next winter relative to patients who received initial treatment with light therapy (Rohan, Roecklein, Lacy, & Vacek, 2009). Theoretically, CBT for SAD targets a psychological vulnerability involving maladaptive cognitions (e.g., negative core beliefs, dysfunctional attitudes, rumination), behavioral disengagement, and emotional reactivity to winter- and low-light stimuli (Rohan, Roecklein, & Haaga, 2009; Tierney Lindsey, Rohan, Roecklein, & Mahon, 2011). The 12-session SAD-tailored CBT protocol includes restructuring negative cognitions, increasing behavioral activation, and relapse prevention for subsequent fall/winter seasons.
Although light therapy research and preliminary CBT studies have shown both are efficacious in treating SAD, these two treatments have very different proposed mechanisms of action underlying their antidepressant effects. Indeed, light therapy and CBT are designed to target different vulnerabilities (i.e., physiological vs. psychological) to SAD, respectively (see Rohan, Roecklein, & Haaga, 2009 for a review). Correction of a misaligned circadian rhythm in nocturnal melatonin release (Lewy, Lefler, Emens, & Bauer, 2006) is hypothesized as the mediator of light therapy’s antidepressant effects, whereas cognitive mediation is proposed to underlie CBT’s antidepressants effects. In examining mechanisms of action underlying SAD treatments, several time points are of interest. Assessing process measures across acute treatment provides information on mechanisms that underlie improvements in depression while SAD treatment is actively underway. Measurement through treatment endpoint is particularly important to elucidate mechanisms of action for a palliative SAD treatment, one that suppresses symptoms as long as treatment is being administered (Hollon, Stewart, & Strunk, 2006).
In the case of SAD, linking changes in process measures across acute treatment during the initial winter of study to depression outcomes in the next winter season provides information on treatment-related changes that may fortify an individual against SAD recurrence (i.e., a wholly new winter depressive episode following a spontaneous spring/summer remission). This type of longitudinal prediction is especially relevant for highlighting mechanisms of action in a prophylactic SAD treatment, one that changes underlying vulnerability processes in a lasting way that serves to prevent depression recurrence after treatment has ended (Hollon et al., 2006). The current study capitalizes on the predictable pattern of SAD episodes in an effort to examine the association between changes in cognitive constructs over 6-weeks of acute treatment with CBT, light therapy, or combined treatment and symptom severity at a follow-up the next winter.
To date, there is no research on whether cognitive constructs change over the course of CBT for SAD or whether the degree of cognitive change over treatment relates to outcomes during the next winter. However, research in the field of nonseasonal unipolar depression has found that cognitive constructs change over the course of cognitive therapy (for a recent review please see Garratt, Ingram, Rand, & Sawalani, 2007). This research has focused on the depressive cognitive constructs derived by Beck (1967; 1976), (i.e., dysfunctional attitudes, negative automatic thoughts, and cognitive reactivity), as well as, ruminative response style (Nolen-Hoeksema, 1991).
Beck’s cognitive theory for depression proposes three levels of thinking that are involved in the onset and maintenance of depression: core beliefs or schema, intermediate cognitions (i.e., attitudes, rules, and assumptions), and automatic thoughts (Beck, 1967; Beck, Rush, Shaw, & Emery, 1979). Dysfunctional attitudes are the rules and assumptions activated by underlying schemas or core beliefs, which guide negative automatic thoughts or brief, conscious moment-to-moment cognitions (Beck, 1967, 1976; Beck, Rush, Shaw, & Emery, 1979). In addition to cognitive constructs derived from Beck’s cognitive model, studies have also examined treatment-related change in rumination, or a tendency to focus on one’s symptoms of distress and the causes and consequences of them when in a depressed mood (Nolen-Hoeksema, 1987).
Unipolar depression research has examined treatment-related change in dysfunctional attitudes and negative automatic thoughts across treatment modalities (i.e., cognitive therapy, group CBT, pharmacotherapy, other psychotherapy interventions, or a combination of modalities) and has found that these cognitive constructs decrease from pre- to post-treatment (Barber & DeRubeis, 2001; Bowers, 1990; DeRubeis et al., 1990; Dingle, Oei, & Young, 2010; Dozois et al., 2009; Imber et al., 1990; Jones, Siegle, & Thase, 2008; Kwon & Oei, 2003; Oei, Bullbeck, & Campbell, 2006; Oei & Sullivan, 1999; Oei & Yeoh, 1999; Schmaling, Dimidjian, Katon, & Sullivan, 2002; Seligman, Schulman, DeRubeis, & Hollon, 1999; Simons, Garfield, & Murphy, 1984; Stravynski et al., 1994; Westra, Dozois, & Boardman, 2002). Two studies in the unipolar depression field examined the temporal relationship between change in these cognitive constructs and depression. The findings from these studies indicate that early change in dysfunctional attitudes and negative automatic thoughts is associated with subsequent improvements in depression (Coleman, Cole, & Wuest, 2010; DeRubeis et al., 1990). In one of these studies, DeRubeis and colleagues (1990) examined change in dysfunctional attitudes over treatment with either cognitive therapy or pharmacotherapy (i.e., imipramine) in 64 depressed individuals. Change early in treatment (i.e., from pre- to mid-treatment) in dysfunctional attitudes predicted subsequent improvement in depression scores (i.e., from mid- to post- treatment) in the cognitive therapy group only, suggesting that cognitive change acts as a mechanism for subsequent improvement in depression in cognitive therapy specifically.
Current literature on cognitive mechanisms underlying cognitive therapy has been limited to the field of nonseasonal unipolar depression, with no research on cognitive change over SAD treatment. The present study explores this question in a secondary analysis of our published clinical trials for SAD (Rohan et al., 2004; Rohan et al., 2007; Rohan, Roecklein, Lacy, et al., 2009). The aim of the current study is to examine whether the degree of change in dysfunctional attitudes, negative automatic thoughts, rumination, and distraction over the 6-weeks of acute treatment with light therapy, CBT, or their combination predicts depression severity during the next winter season. A positive predictive relationship between treatment-related cognitive change and mood outcomes in the next winter would imply the presence of a mediation effect underlying long-term treatment outcomes. We hypothesize that cognitive change over acute treatment is mechanistic only for treatments involving CBT (solo or combined with light therapy), and that any cognitive change that occurs over acute light therapy is incidental to general improvements in depression rather than a necessary component underlying light therapy’s efficacy. Therefore, we hypothesize that cognitive change over treatment will uniquely relate to next winter outcomes in treatments that include CBT because CBT is presumed to be a preventive treatment that changes underlying cognitive vulnerability processes to fortify an individual with SAD against recurrences.
Method
Participant Eligibility and Screening
This research is based on data from a parent clinical trial testing the efficacy of treatments for SAD, including an initial feasibility study (Rohan et al., 2004), a subsequent controlled, randomized clinical trial (Rohan et al., 2007), and the next winter follow-up outcomes (Rohan et al., 2009). The studies were conducted at a research-based seasonality clinic at the Uniformed Services University of the Health Sciences and were approved by the university’s institutional review board. Participants were recruited from the metropolitan Washington, DC area through community advertisements. The feasibility study took place over one fall/winter season (2000/2001), and the controlled trial was conducted over the course of three consecutive fall/winter seasons with initial recruitment in 2001/2002. Screening and enrollment procedures were the same across these two studies and have been detailed elsewhere (Rohan et al., 2004; Rohan et al., 2007).
Participants in both studies (a) were aged 18 or older, (b) met DSM-IV criteria for major depression, recurrent, with a seasonal pattern on the Structured Clinical Interview for DSM-IV Axis I Disorders–Clinician Version (SCID; First, Spitzer, Gibbon, & Williams, 1995), and (c) met criteria, described under Outcome Measures, for a current winter SAD episode as assessed by the Structured Interview Guide for the Hamilton Rating Scale for Depression–Seasonal Affective Disorder Version (SIGH-SAD; Williams, Link, Rosenthal, Amira, & Terman, 1992). Exclusion criteria for both studies included (a) current psychological or psychiatric treatment (i.e., psychotropic medications, psychotherapy, light therapy) or plans to initiate such treatment, (b) presence of any current comorbid Axis I disorder on the SCID, (c) plans for major vacations or absences through March, and (d) bipolar-type SAD. The exception to (a) was a small subsample of participants in the feasibility study (n = 3) that otherwise satisfied all study criteria, but were taking stable doses of antidepressant medications at baseline. These participants were not included in the current analyses.
Randomization Procedure
For details on the randomization scheme and procedures, see the previously published efficacy studies (Rohan et al., 2004; 2007). In brief, participants were randomly assigned to one of three 6-week treatment conditions: group cognitive-behavioral therapy (CBT), light therapy (LT), or the combination of cognitive-behavioral therapy and light therapy (CBT+LT). Treatments were assigned based on a list generated prior to recruitment using random permuted blocks with conditions stratified based on gender and race, reduced to two strata (i.e., White or minority).
Treatments
The treatment protocols and treatment adherence/fidelity data from the studies have been detailed elsewhere (Rohan et al., 2007). In brief, the SAD-tailored CBT condition utilized a group format with 4–8 participants per group and was conducted in accordance with the manual (Rohan, 2008). CBT was administered by the P.I. who wrote the manual and a clinical psychology graduate student co-therapist. To complete treatment before the spontaneous remission of SAD symptoms in the springtime, the 12-session protocol uses more frequent sessions of a longer duration over a shorter time (i.e., 90 minute sessions held twice per week for six weeks) relative to cognitive therapy for depression (Beck et al., 1979). The protocol uses CBT components (i.e., behavioral activation, cognitive restructuring, and relapse-prevention planning) within a seasonality framework to enhance coping with the winter season, limited light availability, and weather changes. LT in both studies utilized 10,000-lux SunRay© light boxes (SunBox Company, Gaithersburg, MD) with participants initiating treatment at home in two daily 45-minute doses, one in the morning between 6:00 and 9:00 am and one in the evening between 6:00 and 9:00 pm. LT administration was continued daily for the six weeks of treatment. A flexible dosing regimen was used in the controlled trial with consultation from an outside LT expert (Teodor T. Postolache, M.D.) who individually tailored the time of day for light administration in order to maximize response, address evident phase shifts, and reduce reported side effects. Following the six weeks of supervised LT, participants could choose, if desired, to continue LT through the end of April, alleviating the ethical concern of treatment discontinuation upon trial completion. The CBT+LT condition in both studies combined all of the procedures of the CBT and LT treatments.
Upon completion of the acute treatment phase, all participants were provided resource information regarding mental health providers and light box companies in the Washington, DC area. Participants were encouraged to continue their study treatment in subsequent fall/winter seasons (i.e., LT participants were encouraged to pursue LT and CBT participants were encouraged to continue using their CBT skills on their own), to seek additional treatment as needed, and to contact the PI if they desired a referral for further treatment.
Measures
Outcome measures
The following outcome measures were collected in the clinical trial designs at pre-treatment, post-treatment, and next winter follow-up. Treatment efficacy results on these outcomes at post-treatment and next winter follow-up have been published elsewhere (Rohan et al., 2004; Rohan et al., 2007; Rohan, Roecklein, Lacy, et al., 2009).
Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version (SIGH-SAD)
The SIGH-SAD (Williams et al., 1992) consists of two parts: the 21-item Structured Interview Guide for the Hamilton Rating Scale for Depression (HAM-D; Williams, 1988) and a supplementary 8-item subscale used to assess atypical symptoms associated with SAD. This measure is the most commonly used measure in SAD research to assess changes in symptoms. We used accepted guidelines (Terman, Terman, & Rafferty, 1990) to define SAD episode onset at study entrance: total SIGH-SAD score ≥ 20 + HAM-D score ≥ 10 + atypical score ≥ 5. Trained raters, blind to treatment condition, completed the SIGH-SAD interviews at pre-treatment, post-treatment, and the next winter follow-up. Independent secondary raters scored an audiotape of the live SIGH-SAD interviews. Training procedures of the raters (Rohan et al., 2007) and inter-rater reliability statistics were reported previously (Rohan et al., 2007; Rohan, Roecklein, Lacy, et al., 2009).
Beck Depression Inventory—Second Edition (BDI-II)
The BDI-II is a 21-item self-report measure of depressive symptom severity with good test-retest reliability and convergent validity (Beck, Steer & Brown, 1996). The BDI-II has shown sensitivity for SAD with significant changes in scores across seasons in SAD patients compared to controls (Rohan, Sigmon, & Dorhofer, 2003). Cronbach’s alphas in this study were 0.86 at pre-treatment, 0.93 at post-treatment, and 0.87 at next winter follow-up.
Moderator measures
The following cognitive measures were administered at pre-treatment and post-treatment.
Automatic Thoughts Questionnaire (ATQ)
The ATQ is a 30-item self-report measure of the frequency of negative automatic thoughts related to depression and has shown good reliability and validity (Hollon & Kendall, 1980). Participants indicate how often they have experienced each thought in the past week on a 5-point Likert scale ranging from 1 (“not at all”) to 5 (“all the time”). Examples of items include “I’m so disappointed in myself” and “My future is bleak.” Cronbach’s alphas in this study were 0.98 at pre-treatment and 0.96 at post-treatment.
Dysfunctional Attitude Scale—Form A (DAS)
The DAS (Weissman & Beck, 1978) is a self-report measure of conviction in 40 beliefs that are commonly endorsed by depressed individuals. This measure has shown high internal consistency and test-retest reliability (Weissman & Beck, 1978). Items include statements such as “If I do not do well all the time, people will not respect me” and “If a person asks for help, it is a sign of weakness.” Participants rate the beliefs on a 7-point Likert scale from 1 (“totally disagree”) to 7 (“totally agree”). Cronbach’s alphas in this study were 0.92 at pre-treatment and 0.91 at post-treatment.
Response Styles Questionnaire (RSQ)
The RSQ (Nolen-Hoeksema, Morrow, & Frederickson, 1993) is a 32-item self-report measure assessing the frequency of using rumination and distraction in response to a depressed mood. Participants indicate how frequently they engage in each type of response when feeling depressed on a 4-point Likert scale ranging from 0 (“almost never”) to 3 (“almost always”). Examples of statements include “Think about how sad you feel” and “Go to a favorite place to get your mind off your feelings.” The Rumination and Distraction subscales have high levels of internal consistency and correlate significantly with respondents’ actual use of rumination and distraction responses (Nolen-Hoeksema & Morrow, 1991). Cronbach’s alphas in this study were 0.95 and 0.88 at pre- and post-treatment, respectively, for the Rumination subscale and 0.77 and 0.79 for the Distraction subscale.
Next Winter Follow-Up Procedures
In both studies, participants who provided post-treatment data were asked to return for a naturalistic follow-up in the next winter during January or February. January and February were chosen as the months of assessment because they are associated with the largest proportions of SAD patients in episode compared to other months (Rosenthal et al., 1984). By design, the participants assigned to the wait-list control group were not assessed at follow-up and were, therefore, not included in the current study. The SIGH-SAD and BDI-II were administered, and participants were compensated $50.
Statistical Analyses
To test our hypothesis that cognitive change over treatment will uniquely relate to next winter outcomes in treatments that include CBT, we conducted an intent-to-treat (ITT) analysis using all 69 participants randomized to CBT, LT, or CBT+LT and multiple imputation of missing data (Little & Yau, 1996; Mazumdar, Lui, Houck, & Reynolds, 1999; Schafer & Graham, 2002). A separate regression was run for each cognitive measure with each dependent variable (follow-up SIGH-SAD or BDI-II score). The degree of change in cognitive constructs across treatment, regardless of pre-treatment levels, was represented as a change score (i.e., pre-treatment minus post-treatment score), computed for each cognitive measure (dysfunctional attitudes, negative automatic thoughts, rumination, and distraction).2 Six variables were included in each regression analysis: pre-treatment depression severity (on the SIGH-SAD or BDI-II), treatment group as two dummy coded variables, cognitive change score, and two interaction terms comparing the effects of cognitive change on next winter depression severity in CBT vs. LT and in CBT+LT vs. LT. As LT is the gold-standard treatment for SAD, this group served as the comparison. Significant interactions were explored graphically post-hoc (Aiken & West, 1991). All analyses were repeated, using available data, without imputation, from the 52 participants who completed the acute treatment phase and the next winter follow-up. These analyses were conducted to examine consistency between completers-only and the ITT analysis, however, the ITT analyses are considered primary. For all tests, p-values of 0.05 or less were considered statistically significant.
Results
Enrollment and Participant Characteristics
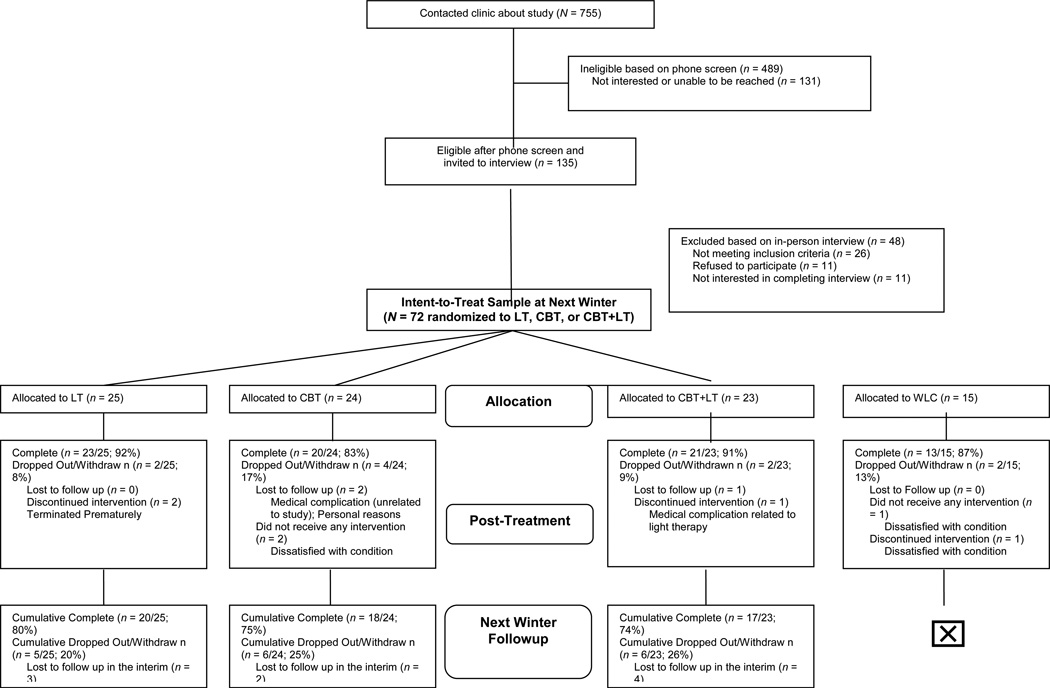
Participant demographic characteristics and flow through the study were presented elsewhere (Rohan et al., 2007; Rohan, Roecklein, Lacy, et al., 2009). Participants were primarily female (92%), Caucasian (80%), and college educated (75%), with a mean age of 46.4 years. The treatment groups did not differ on gender, ethnicity, age, or depression severity at baseline. Over four years of recruitment, 72 participants were randomized to treatment (24 CBT, 25 LT, 23 CBT+LT). Three participants were excluded from these analyses due to antidepressant medication at baseline (1 CBT, 1 LT, 1 CBT+LT). Thus, the final sample sizes were as follows: 69 randomized participants (23 CBT, 24 LT, 22 CBT+LT); 61 provided post-treatment data (19 CBT, 22 LT, 20 CBT+LT); 52 provided next winter follow-up data (17 CBT, 19 LT, 16 CBT+LT), reflecting 12% attrition over acute treatment and an additional 13% over follow-up (total attrition = 25%). See Figure 1 for participant flow.
Figure 1.
Participant flow diagram.
Flow of participants across two pilot studies from randomization through completion of treatment and next winter followup. LT = light therapy, CBT = cognitive-behavioral therapy, CBT+LT = cognitive-behavioral therapy-plus-light therapy, WLC = a concurrent wait-list control (i.e., a minimal contact/delayed light therapy control). This diagram includes the 3 randomized participants (1 LT, 1 CBT, 1 CBT+LT) from our feasibility study that were taking stable doses of antidepressant medications at baseline. All 3 completed acute treatment and provided next winter followup data. Data from these 3 participants were excluded from the current analysis. The design of the randomized controlled trial (Rohan et al., 2007) included a concurrent wait-list control group (WLC), involving weekly SIGH-SAD interviews for 6-weeks, followed by supervised light therapy. Although WLC participants are included in this diagram for completeness, only participants assigned to active treatment (CBT, LT, or CBT+LT) were utilized in the current study as the WLC did not provide follow-up data.
Intent-to-Treat Analyses
Table I displays the pre- and post-treatment scores in the cognitive measures [i.e., Dysfunctional Attitudes Scale (DAS), Automatic Thoughts Questionnaire (RSQ), Response Styles Questionnaire (RSQ)-Rumination and Distraction subscales] and outcome measures [i.e., Beck Depression Inventory – Second Edition (BDI-II), Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version (SIGH-SAD)] across the three treatment conditions. Comparisons at baseline indicated that CBT and CBT+LT groups did not differ from LT (i.e., p > .05) on any of the cognitive measures or outcome measures; LT was used as the comparison group as it is considered the gold standard treatment for SAD. As a preliminary step in examining our hypotheses, we explored the change in dysfunctional attitudes, negative automatic thoughts, rumination, and distraction across the 6-weeks of acute treatment with CBT, LT, and their combination. We fitted mixed effects regression models with treatment group (CBT, LT, CBT+LT), time (pre- and post- treatment) and their interaction as fixed effects and subject as a random effect. Significant time main effects were evident on the DAS, ATQ, and RSQ-Rumination scales. Averaged across treatment groups, there was a significant decrease in DAS, ATQ, and RSQ-Rumination scores from pre-treatment to post-treatment [F(1,56) = 20.82, p < .001, F(1,57) = 59.53, p < .001, F(1,57) = 13.46, p < .001, respectively]. In contrast, averaged across treatment groups, there was not a significant change in RSQ-Distraction scores from pre-treatment to post-treatment [F(1,57) = 2.24, p = .14]. Our results did not reveal a significant Treatment Group × Time interaction for any cognitive construct, suggesting that changes in dysfunctional attitudes, negative automatic thoughts, rumination, and distraction over treatment did not differ according to treatment condition.
Table I.
Cognitive construct and outcome measure scores at pre-treatment, post-treatment, and next winter follow-up by treatment group
| Pre-treatment | Post-treatment | Next Winter Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measur e |
CBT (n=23) |
LT (n=24) |
CBT+L T (n=22) |
CBT | LT | CBT+LT | CBT | LT | CBT+LT |
| DAS | 123.7 (5.7)* |
124.3 (5.6) |
120.2 (5.8)* |
119.8 (6.1) |
105.2 (5.7) |
100.8 (6.2) |
/ | / | / |
| ATQ | 71.3 (4.1)* |
66.5 (4.0) |
60.0 (4.3)* |
45.8 (4.4) | 44.3 (4.1) |
42.4 (4.4) |
/ | / | / |
| RSQ Rum |
27.8 (2.2)* |
27.8 (2.1) |
27.3 (2.2)* |
22.6 (2.4) | 24.0 (2.3) |
20.9 (2.3) |
/ | / | / |
| RSQ Dis | 14.3 (1.2)* |
14.2 (1.2) |
14.1 (1.3)* |
15.4 (1.4) | 14.8 (1.3) |
16.3 (1.3) |
/ | / | / |
| BDI-II | 27.7 (10.3)* |
25.4 (7.1) |
23.6 (6.7)* |
8.6 (6.3) | 9.8 (6.1) | 7.7 (4.7) | 4.8 (3.9) | 11.6 (8.4) |
8.5 (4.7) |
| SIGH SAD |
29.2 (6.5)* |
28.3 (5.5) |
26.6 (5.4)* |
10.9 (8.5) | 11.0 (6.5) |
8.3 (6.3) | 8.9 (7.6) | 15.7 (9.7) |
11.8 (5.4) |
Note. Values are expressed as M (SD). CBT = cognitive-behavioral therapy, LT = light therapy; CBT+LT = CBT-plus-light therapy; DAS = Dysfunctional Attitude Scale; ATQ = Automatic Thoughts Questionnaire; RSQ Rum = Response Styles Questionnaire–Rumination Subscale; RSQ Dis = Response Styles Questionnaire–Distraction Subscale; BDI-II = Beck Depression Inventory, Second Edition; SIGH SAD = Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version.
Not statistically different from LT at pre-treatment (i.e., p > .05) in the Tukey honestly significantly difference comparison.
Subsequently, we conducted the mixed effects regression models using multiple imputation to examine the aim and hypotheses of the current study. Tables II and III display the results of these models examining cognitive change in prediction of next-winter BDI-II and SIGH-SAD scores, respectively. There was not a significant effect of pre-treatment BDI-II or SIGH-SAD score on follow-up BDI-II or SIGH-SAD score, respectively, in any of the analyses. Treatment group, comparing CBT vs. LT, was significant in the prediction of follow-up SIGH-SAD scores in the models analyzing change in RSQ-Rumination and RSQ-Distraction scores. There was not a significant effect of cognitive change over acute treatment in predicting follow-up depression scores in any of the analyses. The interaction term comparing CBT to LT was significant or approached significance in three of the eight models: When predicting next winter follow-up BDI-II scores from DAS change and ATQ change, and when predicting follow-up SIGH-SAD scores from ATQ change. The details of these analyses follow. The interaction term comparing CBT+LT vs. LT was not significant in any of the analyses.
Table II.
Cognitive change predicting next winter follow-up BDI-II scores: Intent-to-treat analyses
| b | S.E. | t | p | |
|---|---|---|---|---|
| Intercept | 8.61 | 3.18 | 2.71 | 0.01 |
| Baseline BDI-II score | 0.05 | 0.12 | 0.41 | 0.69 |
| CBT vs. LT | −4.46 | 2.45 | −1.82 | 0.08 |
| CBT+LT vs. LT | −1.32 | 2.45 | −0.54 | 0.59 |
| DAS change | 0.12 | 0.09 | 1.37 | 0.19 |
| CBT vs. LT * DAS change | −0.19 | 0.09 | −2.03 | 0.05 |
| CBT+LT vs. LT * DAS change | −0.09 | 0.10 | −0.90 | 0.38 |
| Intercept | 7.82 | 3.43 | 2.28 | 0.03 |
| Baseline BDI-II score | 0.06 | 0.14 | 0.46 | 0.65 |
| CBT vs. LT | −2.82 | 2.71 | −1.04 | 0.30 |
| CBT+LT vs. LT | −1.37 | 2.82 | −0.48 | 0.63 |
| ATQ change | 0.12 | 0.11 | 1.17 | 0.28 |
| CBT vs. LT * ATQ change | −0.21 | 0.11 | −1.85 | 0.09 |
| CBT+LT vs. LT * ATQ change | −0.09 | 0.12 | −0.79 | 0.44 |
| Intercept | 9.83 | 3.34 | 2.94 | 0.01 |
| Baseline BDI-II score | 0.08 | 0.11 | 0.73 | 0.47 |
| CBT vs. LT | −6.34 | 2.07 | −3.06 | < 0.01 |
| CBT+LT vs. LT | −3.54 | 2.16 | −1.64 | 0.11 |
| RSQ – Rum change | −0.15 | 0.15 | −1.03 | 0.32 |
| CBT vs. LT * RSQ – Rum change | 0.03 | 0.17 | 0.16 | 0.88 |
| CBT+LT vs. LT * RSQ – Rum change | 0.15 | 0.21 | 0.72 | 0.48 |
| Intercept | 9.92 | 3.06 | 3.24 | < 0.01 |
| Baseline BDI-II score | 0.08 | 0.11 | 0.72 | 0.48 |
| CBT vs. LT | −7.15 | 1.93 | −3.71 | < 0.01 |
| CBT+LT vs. LT | −3.04 | 2.24 | −1.36 | 0.19 |
| RSQ – Dis change | −0.18 | 0.47 | −0.38 | 0.72 |
| CBT vs. LT * RSQ - Dis change | 0.40 | 0.52 | 0.78 | 0.46 |
| CBT+LT vs. LT * RSQ – Dis change | 0.003 | 0.51 | 0.01 | 0.99 |
Note. CBT = cognitive-behavioral therapy, LT = light therapy; CBT+LT = CBT-plus-light therapy; DAS = Dysfunctional Attitude Scale; ATQ = Automatic Thoughts Questionnaire; RSQ – Rum = Response Styles Questionnaire–Rumination Subscale; RSQ – Dis = Response Styles Questionnaire–Distraction Subscale; BDI-II = Beck Depression Inventory, Second Edition.
Table III.
Cognitive change predicting next winter follow-up SIGH-SAD scores: Intent-to-treat analyses
| b | S.E. | t | p | |
|---|---|---|---|---|
| Intercept | 12.15 | 5.33 | 2.28 | 0.03 |
| Baseline SIGH-SAD score | 0.14 | 0.18 | 0.74 | 0.46 |
| CBT vs. LT | −5.92 | 3.03 | −1.96 | 0.06 |
| CBT+LT vs. LT | −2.43 | 3.18 | −0.76 | 0.45 |
| DAS change | 0.04 | 0.11 | 0.34 | 0.74 |
| CBT vs. LT * DAS change | −0.15 | 0.12 | −1.29 | 0.20 |
| CBT+LT vs. LT * DAS change | −0.09 | 0.13 | −0.68 | 0.50 |
| Intercept | 10.69 | 5.53 | 1.93 | 0.06 |
| Baseline SIGH-SAD score | 0.06 | 0.18 | 0.31 | 0.76 |
| CBT vs. LT | −1.04 | 3.34 | −0.31 | 0.76 |
| CBT+LT vs. LT | −1.17 | 3.61 | −0.32 | 0.75 |
| ATQ change | 0.24 | 0.11 | 2.10 | 0.06 |
| CBT vs. LT * ATQ change | −0.32 | 0.12 | −2.72 | 0.01 |
| CBT+LT vs. LT * ATQ change | −0.18 | 0.14 | −1.24 | 0.23 |
| Intercept | 14.13 | 5.08 | 2.78 | 0.01 |
| Baseline SIGH-SAD score | 0.09 | 0.18 | 0.49 | 0.63 |
| CBT vs. LT | −6.13 | 2.56 | −2.39 | 0.02 |
| CBT+LT vs. LT | −4.18 | 2.80 | −1.49 | 0.14 |
| RSQ – Rum change | −0.17 | 0.18 | −0.95 | 0.36 |
| CBT vs. LT * RSQ – Rum change | 0.01 | 0.21 | 0.03 | 0.98 |
| CBT+LT vs. LT * RSQ – Rum change | 0.04 | 0.25 | 0.17 | 0.87 |
| Intercept | 15.27 | 5.06 | 3.02 | < 0.01 |
| Baseline SIGH-SAD score | 0.03 | 0.18 | 0.14 | 0.89 |
| CBT vs. LT | −6.58 | 2.57 | −2.56 | 0.02 |
| CBT+LT vs. LT | −3.86 | 2.51 | −1.54 | 0.13 |
| RSQ – Dis change | −0.23 | 0.43 | −0.52 | 0.61 |
| CBT vs. LT * RSQ – Dis change | 0.41 | 0.48 | 0.86 | 0.40 |
| CBT+LT vs. LT * RSQ - Dis change | 0.12 | 0.50 | 0.24 | 0.81 |
Note. CBT = cognitive-behavioral therapy, LT = light therapy; CBT+LT = CBT-plus-light therapy; DAS = Dysfunctional Attitude Scale; ATQ = Automatic Thoughts Questionnaire; RSQ - Rum = Response Styles Questionnaire–Rumination Subscale; RSQ - Dis = Response Styles Questionnaire–Distraction Subscale; SIGH SAD = Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version.
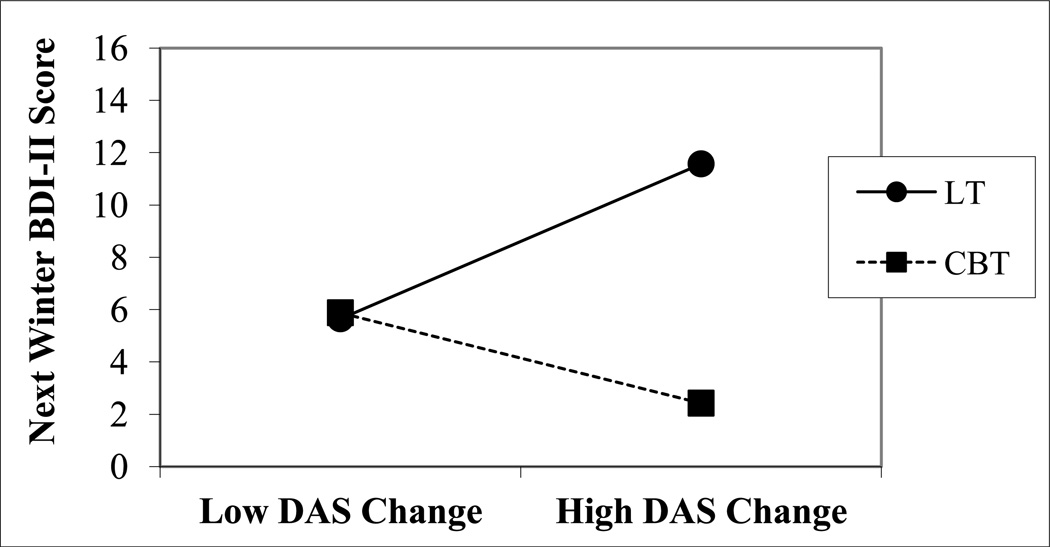
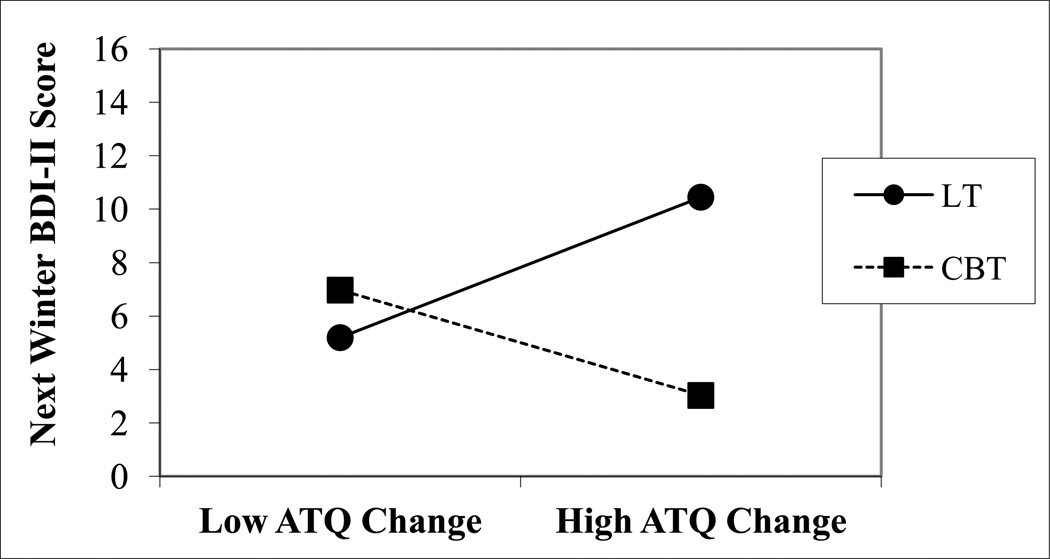
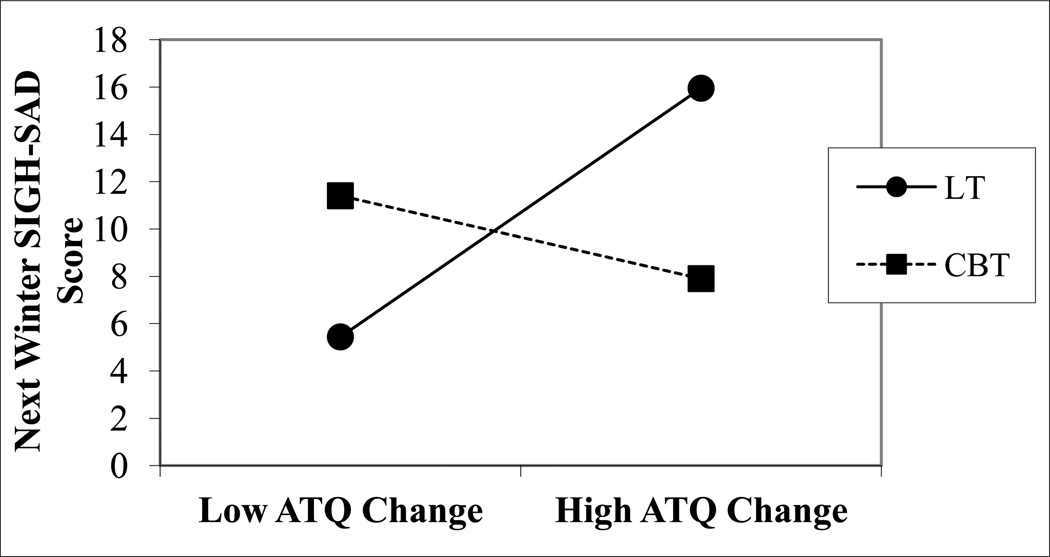
When baseline BDI-II score, treatment type, change in DAS score, and the interactions of treatment group and DAS change were entered into the model in the prediction of next winter follow-up BDI-II scores, the CBT vs. LT × DAS change interaction was statistically significant (b = −.19, SE = 0.09, t[32.7] = −2.03, p = .05). A similar result was found when using change in frequency of automatic thoughts as a predictor of next-winter follow-up BDI-II scores. More specifically, in the model consisting of baseline BDI-II scores, treatment type, change in ATQ score, and the interactions of treatment group and ATQ change, the Treatment Group × ATQ change interaction for CBT vs. LT approached statistical significance (b = −.21, SE = 0.11, t[10.2] = −2.15, p = .09). In the prediction of next winter follow-up SIGH-SAD scores, the Treatment Group × ATQ change interaction for CBT vs. LT was statistically significant when baseline SIGH-SAD scores, treatment type, change in ATQ scores, and the interactions of treatment group and ATQ change were in the model (b = −.32, SE = 0.12, t[19.6] = −2.72, p = .01). These significant interactions were explored graphically post-hoc (see Figures 2, 3, 4).
Figure 2.
Illustration of the interaction effects of dysfunctional attitudes change score and treatment with CBT vs. LT in prediction of next winter BDI-II scores based on predicted values.
BDI-II = Beck Depression Inventory, Second Edition. Low and High cognitive change represents 1 SD above and below the mean.
Figure 3.
Illustration of the interaction effects of negative automatic thoughts change score and treatment with CBT vs. LT in prediction of next winter BDI-II scores based on predicted values.
BDI-II = Beck Depression Inventory, Second Edition. Low and High cognitive change represents 1 SD above and below the mean.
Figure 4.
Illustration of the interaction effects of negative automatic thoughts change score and treatment with CBT vs. LT in prediction of next winter SIGH-SAD scores based on predicted values.
SIGH-SAD = Structured Interview Guide for the Hamilton Rating Scale for Depression-Seasonal Affective Disorder Version. Low and High cognitive change represents 1 SD above and below the mean.
Completer Analyses
Analyses were conducted with the 52 participants who completed acute treatment and attended the next winter follow-up. The overall pattern of results examining cognitive change over treatment in prediction of next winter follow-up depression scores by treatment group was similar to those from the ITT analyses with one exception. In the prediction of next winter follow-up BDI-II scores, the CBT vs. LT × ATQ change interaction was significant (b = −.23, SE = 0.11, t[44] = −2.15, p = .03); this interaction approached significance in the ITT analysis. Similarly, the CBT vs. LT × ATQ change interaction approached significance as a predictor of next winter SIGH-SAD scores (b = −.25, SE = 0.14, t[44] = −1.77, p = .08); this predictor was statistically significant in the ITT analysis. Unlike the ITT analysis, the CBT vs. LT × DAS change interaction was not a significant predictor of next winter BDI-II scores (b = −.16, SE = 0.10, t[43] = −1.50, p = .14).
Discussion
The predictable seasonal pattern of depressive episodes in SAD facilitates the examination of mechanisms underlying long-term outcomes following treatment. Previous studies have demonstrated comparable efficacy of light therapy and a SAD-tailored form of cognitive-behavioral therapy (CBT) in the acute treatment of SAD (Rohan et al., 2004; Rohan et al., 2007) with fewer SAD episode recurrences and less severe patient- and interviewer-rated depressive symptoms associated with CBT the next winter (Rohan, Roecklein, Lacy, et al., 2009). Light therapy and CBT are assumed to target different vulnerabilities (physiological and psychological, respectively) to SAD. This study is a first step in determining whether cognitive mechanisms of action underlie the acute (i.e., post-treatment) and long-term (i.e., next winter) efficacy of CBT for SAD relative to light therapy.
Across the 6-week acute treatment phase in the initial winter, change in dysfunctional attitudes, negative automatic thoughts, and rumination or distraction tendencies did not differ between CBT, light therapy, or combined CBT and light therapy. Collapsing across treatment groups, Dysfunctional Attitudes Scale (DAS), Automatic Thoughts Questionnaire (ATQ), and Response Styles Questionnaire (RSQ)-Rumination subscale scores were significantly lower at post-treatment relative to pre-treatment. In SAD, cognitive change appears to be associated with a reduction in depressive symptoms, not dependent on whether maladaptive cognitions are a focus in treatment, supporting the non-specificity of cognitive change over depression treatment for unipolar nonseasonal depression (DeRubeis et al., 1990; Dozois et al., 2009; Imber et al., 1990; Oei & Yeoh, 1999; Simons, Garfield, & Murphy, 1984; Schmaling et al., 2002; Stravynski et al., 1994).
Examining the relationship between treatment-related cognitive change and mood status the following winter represents an initial step in elucidating potential mechanisms of long-term treatment outcomes. All three active treatment groups showed significant and comparable reductions in depressive symptoms over acute treatment (Rohan et al., 2007). However, in participants randomized to solo CBT (but not to solo LT or to combined CBT+LT), a greater degree of improvement on the DAS and ATQ during the six weeks of treatment was associated with less severe depressive symptoms the next winter in the ITT sample. Similar results were found in a secondary analysis of participants who completed the acute treatment and next winter follow-up, with replication of change in negative automatic thoughts predictive of next winter depression score in solo CBT only. Unlike the ITT analysis, the completer-only analysis did not show change in dysfunctional attitudes as a significant predictor of follow-up depressive symptom severity in the solo CBT group. The regression models were conducted with a sample size of 69 and six predictor variables. This ratio of participants to predictors is sufficient for hypothesis testing based on previous statistical recommendations (Miller & Kunce, 1973).
The observed pattern of results suggests that the effectiveness of solo CBT over light therapy at the next winter follow-up (Rohan, Roecklein, Lacy, et al., 2009) may be due to the change in cognitive constructs over the course of acute CBT treatment. Specifically, a reduction in endorsed dysfunctional attitudes and frequency of automatic negative thoughts over acute treatment with solo CBT may be mechanistic of its long-term effects. This suggests that CBT for SAD may exert lasting benefits via offsetting underlying cognitive vulnerability processes that contribute risk for future onsets of the disorder. In contrast, the degree of change in cognitive constructs over the acute course of LT or combined CBT+LT was not associated with next winter depression outcomes and, therefore, may be incidental to improved depression over treatment. In other words, the change in cognitive constructs observed over treatment with CBT may provide prophylactic benefits and be mechanistic in its long-term effects, whereas cognitive change that occurred during the course of LT and combination treatment may be state-dependent.
These findings are consistent with previous studies on cognitive mechanisms of treatment with cognitive therapy for non-seasonal depression. Research on depression treatment has shown a temporal relationship between cognitive improvement and depressive symptom improvement, whereby early cognitive change proceeds and predicts subsequent decreased symptomatology (Garratt et al., 2007). DeRubeis et al. (1990) compared depressed patients receiving either cognitive therapy or pharmacotherapy (imipramine) on a variety of cognitive constructs over 12 weeks of treatment. Consistent with the results from the current study, significant changes were seen in both groups on the DAS from pre- to mid-treatment with no differences between treatments. However, DAS change within the first 6 weeks of treatment was predictive of subsequent depression improvement in the cognitive therapy group only, implying that cognitive change may be a specific mechanism underlying cognitive therapy’s efficacy. In contrast, cognitive change does not appear to be mechanistic in pharmacotherapy treatments. For example, Fava et al. (1999) found that change in dysfunctional attitudes in patients treated with fluoxetine over 8 weeks was not predictive of symptom improvement, further supporting the specificity of cognitive mechanisms to cognitive therapy outcomes. Additional findings show that dysfunctional attitudes and negative automatic thoughts do not play the same mechanistic role in other psychotherapy interventions distinct from cognitive therapy (i.e., group acceptance and commitment therapy; Zettle et al., 2011). Thus, cognitive change appears to be uniquely instrumental to treatment response to cognitive therapy in non-seasonal depression.
Interestingly, contrary to our hypothesis, cognitive change over treatment did not predict next winter depression outcomes in participants randomized to combined CBT+LT. This finding is consistent with the pattern of results from the primary efficacy analyses (Rohan, Roecklein, Lacy, et al., 2009). Although the CBT (7.0%) and CBT+LT (5.5%) groups both had significantly smaller proportions of winter depression recurrences than the solo LT group (36.7%) the next winter, only solo CBT (not CBT+LT) was associated with significantly lower depression severity on the SIGH-SAD and BDI-II the next winter as compared to solo LT (Rohan, Roecklein, Lacy, et al., 2009). Considering these efficacy results in combination with the results reported here, it is possible that adding LT to CBT waters down the cognitive mechanism of CBT. It is plausible that in the CBT+LT group, there was an over-reliance on the antidepressant effects expected from LT, such that reduced efforts were put into the CBT components of treatment. Furthermore, due to the intensity of the CBT+LT intervention, individuals may have allotted less time or resources to learning or practicing CBT skills. If so, such dilution of the cognitive mechanism would be detrimental in combination CBT+LT considering that CBT may exert its long-term benefits via offsetting cognitive vulnerability processes that contribute risk for future depressive symptoms. A similar finding of apparent “watering down” of CBT’s efficacy in combination treatment was found by Barlow and colleagues (2000) comparing CBT vs. CBT and imipramine in the long-term treatment of panic disorder. Although combination treatment was associated with significantly better results than solo CBT at the conclusion of the 12 weeks of acute treatment and in the short-term (i.e., over the 6 months of maintained treatment), combination treatment was associated with the highest relapse rate at follow-up 9 months later. The authors concluded that the addition of imipramine to CBT treatment reduced the long-term durability of CBT. Furthermore, a meta-analysis comparing CBT plus pharmacotherapy vs. CBT plus placebo across a range of anxiety disorders found that although CBT plus pharmacotherapy was superior at post-treatment, the treatments were comparable at follow-up assessments (Hofmann, Sawyer, Korte, & Smits, 2009). These findings indicate that the addition of adjunct treatments to CBT does not improve, and may be detrimental to, CBT’s long-term efficacy.
It is noteworthy that our results show change over acute treatment in both dysfunctional attitudes and negative automatic thoughts, but not rumination or distraction tendency, as potential mechanisms underlying the antidepressant effects of solo CBT. According to cognitive theories of depression, these cognitive constructs are distinct in content and stability. Beck’s theory of depression (1967; 1979) defines dysfunctional attitudes and automatic thoughts as intermediate and surface-level cognitions, respectively, that are mood-state dependent (i.e., accessible in conscious awareness when in a depressive state) and serve as targets in his cognitive therapy for depression. In contrast, Nolen-Hoeksema’s theory (1991) conceptualizes one’s response style to a depressed mood (i.e., rumination or distraction) as trait-like regardless of current mood state, supported by studies showing stability of response style scores over follow-up periods (Just & Alloy, 1997; Nolen-Hoeksema, Parker, & Larson, 1994). Therefore, rumination reflects a disposition towards a cognitive process whereas automatic thoughts and dysfunctional attitudes reflect cognitive content associated with depressed mood. In line with these theories, cognitive change over CBT treatment as a predictor of follow-up depression status should involve the DAS and ATQ more than rumination.
To our knowledge, this study is the first to examine the effects of cognitive change during acute treatment on long-term outcomes in the treatment of SAD. These findings are an important first step in identifying how CBT for SAD may exert prophylactic effects on SAD. Future studies should employ more frequent assessments to capture the trajectory of change in cognitive processes over the course of treatment and to provide a more detailed picture of when this change occurs. Ecological momentary assessment of cognitive constructs may be one way to examine these processes throughout treatment without the influence of retrospective recall biases (Wenze, Gunthert, & Forand, 2007). Studies examining cognitive variables at follow-up time points would provide a stronger argument for the mechanistic effect of cognitive constructs in the long-term efficacy of CBT for SAD. Specifically, measuring cognitive constructs at the next winter would provide information as to whether cognitive change that occurred over treatment was sustained and whether this differs between treatment groups. As this study focuses on the psychological vulnerability to SAD and a possible mechanism underlying CBT, future studies should also examine theoretically-relevant mechanisms that are better matched to the light therapy modality (e.g., circadian rhythm alignment). A randomized clinical trial comparing the effectiveness of CBT and light therapy that measures both circadian rhythm and cognitive changes at multiple time points over the acute treatment phase and in the next winter would be best suited for this.
There are several limitations to our study. The first, as previously mentioned, is the lack of more frequent cognitive measures over treatment and at the follow-up assessment. Additionally, as this was a naturalistic follow-up, we invited participants to return to our lab the next winter after the initial treatment phase of the study. Depressive episodes and symptom fluctuations may have occurred in the interim between treatment endpoint and next winter follow-up, which would not have been captured. However, as the pattern of depressive episodes in individuals with SAD is highly predictable, there is less concern regarding this than would be the case in non-seasonal depression. Another limitation is the generalizability of our findings due to homogeneous sample demographics. Studies are needed to replicate these results in more diverse samples including greater numbers of males, individuals from under-represented racial and ethnic groups, and less educated individuals. Furthermore, it has yet to be seen if such findings are consistent in different geographical locations, in individuals with comorbid psychopathology, and in community mental health settings. Additionally, this study did not collect data on physiological (e.g., circadian) or other mechanistic measures specific to LT and, therefore, cannot compare CBT vs. LT on potential modality-specific mechanisms underlying treatment efficacy. As another limitation, data on personality disorders and previous treatments utilized as potential moderators of treatment outcomes was not collected. Despite these limitations, our findings are promising and represent a first step in determining mechanisms underlying the enduring effectiveness of CBT following SAD treatment. A reduction in dysfunctional attitudes and negative automatic thoughts may be a unique mechanism underlying solo CBT that explain its enduring effects the next winter.
Footnotes
The decision to call this treatment cognitive-behavioral therapy reflects our view that both cognitive and behavioral (e.g., pleasant event scheduling) treatment components directly target and effect change in depression.
Elsewhere, we have also explored baseline cognitive construct scores as moderators of next winter depression scores (manuscript under review).
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Barber JP, DeRubeis RJ. Change in compensatory skills in cognitive therapy for depression. Journal of Psychotherapy Practice Research. 2001;10:8–13. [PMC free article] [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA. 2000;283(19):2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Hoeber; 1967. [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. New York: International Universities Press; 1976. [Google Scholar]
- Beck AT, Rush JA, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory—2nd edition manual. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Bowers WA. Treatment of depressed in-patients: Cognitive therapy plus medication, relaxation plus medication, and medication alone. British Journal of Psychiatry. 1990;156:73–78. doi: 10.1192/bjp.156.1.73. [DOI] [PubMed] [Google Scholar]
- Coleman D, Cole D, Wuest L. Cognitive and psychodynamic mechanisms of change in treated and untreated depression. Journal of Clinical Psychology. 2009;66(3):215–228. doi: 10.1002/jclp.20645. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Grove WM, Evans MD, Garvey MJ, Tuason VB, et al. How does cognitive therapy work? Cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology. 1990;58:862–869. doi: 10.1037//0022-006x.58.6.862. [DOI] [PubMed] [Google Scholar]
- Dingle GA, Oei TPS, Young RM. Mechanisms of change in negative thinking and urinary monoamines in depressed patients during acute treatment with group cognitive behavioral therapy and antidepressant medication. Psychiatry Research. 2010;175:82–88. doi: 10.1016/j.psychres.2008.12.014. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Bieling PJ, Patelis-Siotis I, Hoar L, Chudzik S, McCabe K, et al. Changes in self-schema structure in cognitive therapy for major depressive disorder: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77(6):1078–1088. doi: 10.1037/a0016886. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-Clinician Version) New York: New York State Psychiatric Institute Biometrics Research Department; 1995. [Google Scholar]
- Garratt G, Ingram RE, Rand KL, Sawalani G. Cognitive processes in cognitive therapy: Evaluation of the mechanisms of change in the treatment of depression. Clinical Psychology: Science and Practice. 2007;14(3):224–239. [Google Scholar]
- Hofmann SG, Sawyer AT, Korte KJ, Smits JAJ. Is it beneficial to add pharmacotherapy to cognitive-behavioral therapy when treating anxiety disorders? A meta-analytic review. International Journal of Cognitive Therapy. 2009;2(2):160. doi: 10.1521/ijct.2009.2.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, Kendall PC. Cognitive self-statements in depression: Development of an Automatic Thoughts Questionnaire. Cognitive Therapy and Research. 1980;3:383–396. [Google Scholar]
- Hollon SD, Stewart MO, Strunk D. Enduring effects for cognitive behavior therapy in the treatment of depression and anxiety. Annual Review of Psychology. 2006;57:285–315. doi: 10.1146/annurev.psych.57.102904.190044. [DOI] [PubMed] [Google Scholar]
- Imber SD, Pilkonis PA, Sotsky SM, Watkins JT, Shea MT, Elkin I, et al. Mode-specific effects among three treatments for depression. Journal of Consulting and Clinical Psychology. 1990;58:352–359. doi: 10.1037//0022-006x.58.3.352. [DOI] [PubMed] [Google Scholar]
- Jones NP, Siegle GJ, Thase ME. Effects of rumination and initial severity on remission to cognitive therapy for depression. Cognitive Therapy and Research. 2008;32:591–604. doi: 10.1007/s10608-008-9191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Just N, Alloy LB. The response styles theory of depression: Tests and an extension of the theory. Journal of Abnormal Psychology. 1997;106(2):221–229. doi: 10.1037//0021-843x.106.2.221. [DOI] [PubMed] [Google Scholar]
- Kwon S, Oei TPS. Cognitive change processes in a group cognitive behavior therapy of depression. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:73–85. doi: 10.1016/s0005-7916(03)00021-1. [DOI] [PubMed] [Google Scholar]
- Lewy AJ, Bauer VK, Cutler NL, Sack RL, Ahmed S, Thomas KH, et al. Morning vs. evening light treatment of patients with winter depression. Archives of General Psychiatry. 1998;55:890–896. doi: 10.1001/archpsyc.55.10.890. [DOI] [PubMed] [Google Scholar]
- Lewy AJ, Sack RL, Miller LS, Hoban TM. Antidepressant and circadian phase-shifting effects of light. Science. 1987;235:252–254. doi: 10.1126/science.3798117. [DOI] [PubMed] [Google Scholar]
- Little R, Yau L. Intent-to-treat analysis with for longitudinal studies with drop-outs. Biometrics. 1996;25:1324–1333. [PubMed] [Google Scholar]
- Mazumdar S, Lui KS, Houck PR, Reynolds CF. Intent-to-treat analysis for longitudinal clinical trials: Coping with the challenge of missing values. Journal of Psychiatric Research. 1999;33:87–95. doi: 10.1016/s0022-3956(98)00058-2. [DOI] [PubMed] [Google Scholar]
- Miller DE, Kunce JT. Prediction and statistical overkill reconsidered. Measurement and Evaluation in Guidance. 1973;6:157–163. [Google Scholar]
- Nolen-Hoeksema S. Sex differences in unipolar depression: Evidence and theory. Psychological Bulletin. 1987;101:259–282. [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61(1):115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J, Frederickson BL. Response styles and the duration of episodes of depressed mood. Journal of Abnormal Psychology. 1993;102:20–28. doi: 10.1037//0021-843x.102.1.20. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Parker L, Larson J. Ruminative coping with depressed mood following loss. Journal of Personality and Social Psychology. 1994;67:92–104. doi: 10.1037//0022-3514.67.1.92. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Bullbeck K, Campbell JM. Cognitive change process during group cognitive behaviour therapy for depression. Jounal of Affective Disorders. 2006;92:231–241. doi: 10.1016/j.jad.2006.02.004. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Sullivan LM. Cognitive changes following recovery from depression in a group cognitive-behaviour therapy program. Australian and New Zealand Journal of Psychiatry. 1999;33:407–415. doi: 10.1046/j.1440-1614.1999.00562.x. [DOI] [PubMed] [Google Scholar]
- Oei TPS, Yeoh AEO. Pre-existing antidepressant medication and the outcome of group cognitive-behavioural therapy. Australian and New Zealand Journal of Psychiatry. 1999;33:70–76. doi: 10.1046/j.1440-1614.1999.00520.x. [DOI] [PubMed] [Google Scholar]
- Rohan KJ. Coping with the seasons: A cognitive-behavioral approach to seasonal affective disorder. Therapist guide. New York, NY: Oxford University Press; 2008. [Google Scholar]
- Rohan KJ, Roecklein KA, Haaga DAF. Biological and psychological mechanisms of seasonal affective disorder: A review and integration. Current Psychiatry Reviews. 2009;5:37–47. [Google Scholar]
- Rohan KJ, Roecklein KA, Lacy TJ, Vacek PM. Winter depression recurrence one year after cognitive-behavioral therapy, light therapy, or combination treatment. Behavior Therapy. 2009;40:225–238. doi: 10.1016/j.beth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Roecklein KA, Tierney Lindsey K, Johnson LG, Lippy RD, Lacy TJ, et al. A randomized controlled trial of cognitive-behavioral therapy, light therapy, and their combination for seasonal affective disorder. Journal of Consulting and Clinical Psychology. 2007;75:489–500. doi: 10.1037/0022-006X.75.3.489. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Sigmon ST, Dorhofer DM. Cognitive-behavioral factors in seasonal affective disorder. Journal of Consulting and Clinical Psychology. 2003;71(1):22–30. doi: 10.1037//0022-006x.71.1.22. [DOI] [PubMed] [Google Scholar]
- Rohan KJ, Tierney Lindsey K, Roecklein KA, Lacy TJ. Cognitive-behavioral therapy, light therapy, and their combination in treating seasonal affective disorder. Journal of Affective Disorders. 2004;80:273–283. doi: 10.1016/S0165-0327(03)00098-3. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Sack DA, Gillin C, Lewy AJ, Goodwin FK, Davenport Y, et al. Seasonal affective disorder: A description of the syndrome and preliminary findings with light therapy. Archives of General Psychiatry. 1984;41:72–80. doi: 10.1001/archpsyc.1984.01790120076010. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Schlager D, Froom J, Jaffe A. Winter depression and functional impairment among ambulatory primary care patients. Comprehensive Psychiatry. 1995;36:18–24. doi: 10.1016/0010-440x(95)90094-c. [DOI] [PubMed] [Google Scholar]
- Schmaling KB, Dimidjian S, Katon W, Sullivan M. Response styles among patients with minor depression and dysthymia in primary care. Journal of Abnormal Psychology. 2002;111(2):350–356. doi: 10.1037//0021-843x.111.2.350. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Gemar M, Williams S. Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. Journal of Abnormal Psychology. 1999;108:3–10. doi: 10.1037//0021-843x.108.1.3. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Kennedy MD, Gemar M, Hood K, Pedersen R, Buis T, et al. Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry. 2006;63:749–755. doi: 10.1001/archpsyc.63.7.749. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention & Treatment. 1999;2(1) [Google Scholar]
- Simons AD, Garfield SL, Murphy GE. The process of change in cognitive therapy and pharmacotherapy for depression. Archives of General Psychiatry. 1984;41:45–51. doi: 10.1001/archpsyc.1984.01790120049007. [DOI] [PubMed] [Google Scholar]
- Sitnikov L, Rohan KJ, Evans M, Mahon JN, Nillni YI. Cognitive moderators of winter depression treatment outcomes in cognitive-behavioral therapy vs. light therapy. doi: 10.1016/j.brat.2013.09.010. submitted. [DOI] [PubMed] [Google Scholar]
- Stravynski A, Verreault R, Gaudette G, Langlois R, Gagnier S, Larose M, et al. The treatment of depression with group behavioural-cognitive therapy and Imipramine. Canadian Journal of Psychiatry. 1994;39:387–390. doi: 10.1177/070674379403900701. [DOI] [PubMed] [Google Scholar]
- Terman JS, Terman M, Lo ES, Cooper TB. Circadian time of morning light administration and therapeutic response in winter depression. Archives of General Psychiatry. 2001;58:69–75. doi: 10.1001/archpsyc.58.1.69. [DOI] [PubMed] [Google Scholar]
- Terman M, Terman JS, Rafferty B. Experimental design and measures of success in the treatment of winter depression by bright light. Psychopharmacology Bulletin. 1990;26:505–510. [PubMed] [Google Scholar]
- Terman M, Terman JS. Light therapy for seasonal and nonseasonal depression: Efficacy, protocol, safety, and side effects. CNS Spectrums. 2005;10(8):647–663. doi: 10.1017/s1092852900019611. [DOI] [PubMed] [Google Scholar]
- Tierney Lindsey K, Rohan KJ, Roecklein KA, Mahon JN. Surface facial electromyography, skin conductance, and self-reported emotional responses to light- and season-relevant stimuli in seasonal affective disorder. Journal of Affective Disorders. 2011;133(1–2):311–319. doi: 10.1016/j.jad.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman A, Beck AT. Development and validation of the Dysfunctional Attitude Scale: A preliminary investigation; Paper presented at the annual meeting of the American Educational Research Association; Toronto, Ontario, Canada. 1978. [Google Scholar]
- Wenze SJ, Gunthert KC, Forand NR. Influence of dysphoria on positive and negative cognitive reactivity to daily mood fluctuations. Behavior Research and Therapy. 2007;45(5):915–927. doi: 10.1016/j.brat.2006.08.010. http://dx.doi.org/10.1016/j.brat.2006.08.010 [DOI] [PubMed] [Google Scholar]
- Westra HA, Dozois DJA, Boardman C. Predictors of treatment change and engagement in cognitive-behavioral group therapy for depression. Journal of Cognitive Psychotherapy. 2002;16(2):227–241. [Google Scholar]
- Whisman MA, Miller IW, Norman WH, Keitner GI. Cognitive therapy with depressed inpatients: Specific effects on dysfunctional cognitions. Journal of Consulting and Clinical Psychology. 1991;59:282–288. doi: 10.1037//0022-006x.59.2.282. [DOI] [PubMed] [Google Scholar]
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Williams JB, Link MJ, Rosenthal NE, Amira L, Terman M. Structured Interview Guide for the Hamilton Depression Rating Scale—Seasonal Affective Disorder Version (SIGH-SAD) New York: New York State Psychiatric Institute; 1992. [Google Scholar]
- Zettle RD, Rains JC. Group cognitive and contextual therapies in the treatment of depression. Journal of Clinical Psychology. 1989;45:436–445. doi: 10.1002/1097-4679(198905)45:3<436::aid-jclp2270450314>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Zettle RD, Rains JC, Hayes SC. Processes of change in acceptance and commitment therapy and cognitive therapy for depression: A mediation reanalysis of Zettle and Rains. Behavior Modification. 2011;35(3):265–283. doi: 10.1177/0145445511398344. [DOI] [PubMed] [Google Scholar]