Abstract
Background
The purpose of this study was to compare changes in corneal staining in patients with dry eye after 6 weeks of treatment with Systane® Gel Drops or Refresh Liquigel® lubricant eye drops.
Methods
Patients aged ≥18 years with a sodium fluorescein corneal staining sum score of ≥3 in either eye and best-corrected visual acuity of 0.6 logarithm of the minimum angle of resolution or better in each eye who were using a lubricant eye gel or ointment for dry eye were included in this randomized, parallel-group, multicenter, double-blind trial. Patients were randomized to four times daily Systane® Gel Drops (polyethylene glycol 400 0.4% and propylene glycol 0.3%) or Refresh LiquiGel® Drops (carboxymethylcellulose sodium 1%) for 6 weeks. The primary efficacy outcome was mean change from baseline to week 6 in sodium fluorescein corneal staining. Supportive efficacy outcomes included conjunctival staining, tear film break-up time, Patient Global Assessment of Improvement, Impact of Dry Eye on Everyday Life (IDEEL) Treatment Satisfaction/Treatment Bother Questionnaire, Single Symptom Comfort Scale, and Ocular Symptoms Questionnaire. The safety analysis comprised recording of adverse events.
Results
In total, 147 patients (Systane group, n=73; Refresh group, n=74; mean ± standard deviation age, 57±16 years) were enrolled and included in the safety and efficacy analyses. Corneal staining was significantly reduced from baseline to week 6 for Systane and Refresh (−3.4±2.5 and −2.5±2.6 units, respectively; P<0.0001, t-test), with a significantly greater improvement with Systane versus Refresh (P=0.0294). Results for conjunctival staining, tear film break-up time, and patient-reported outcome questionnaires were not statistically different between groups. No safety issues were identified; adverse events were reported by 19% of patients with Systane and 30% of patients with Refresh eye drops.
Conclusion
Systane Gel Drops were associated with significantly better corneal staining scores versus Refresh Liquigel eye drops in patients with dry eye. Supportive efficacy outcomes were not significantly different between groups. Both treatments were well tolerated.
Keywords: artificial tears, corneal staining, Systane Gel Drops, Refresh Liquigel, patient-reported outcomes
Introduction
Dry eye is a chronic multifactorial condition resulting from increased tear film evaporation or decreased tear production.1 Dry eye can cause visual disturbances, eye discomfort, and tear film instability that can lead to eye surface damage.2,3 Estimates of the prevalence of dry eye range from 7% to approximately 34% and vary by geographic area and demographic characteristics of the population studied; in the US, epidemiologic studies show an overall prevalence of 7% and 4% in women and men, respectively.2
Dry eye is caused by a cycle of tear film instability, hyperosmolarity, and inflammation3,4 that can ultimately result in increased friction and damage to the surface of the eye.5,6 Clinical assessment of dry eye is not standardized, and there appears to be little correlation between signs and symptoms of dry eye.7–9 However, information derived from clinical signs can be indicative of the state of the ocular surface.9 There are limitations of signs and symptoms of dry eye; for example, corneal and conjunctival staining are not sensitive in the early stages, and tear film break-up time shows a sharp transition between the normal state and the disease state, whereas tear osmolarity shows an approximately linear relationship with disease severity.10,11
The causes of dry eye are usually impaired tear production (ie, aqueous/mucin-deficient dry eye), excessive evaporation (ie, lipid-deficient dry eye), or both.1,4 Products have been developed to treat both types of pathophysiology.12 Topical therapies for dry eye available over the counter include the carboxymethylcellulose-containing artificial tears Refresh Liquigel® lubricant eye drops (Allergan Inc, Irvine, CA, USA), as well as the polyethylene glycol/propylene glycol-containing Systane® family of artificial tear lubricant eye drops, that includes Systane Balance (which contains propylene glycol as its only active ingredient), Systane Ultra, and Systane Gel Drops lubricant eye gel (Alcon Laboratories Inc, Fort Worth, TX, USA). Systane Gel Drops is intended for use by patients in need of extra protection against symptoms of severe dry eye. Systane Gel Drops and the original Systane Lubricant Eye Drops have similar concentrations of the demulcents polyethylene glycol (PEG) 400 (0.4%) and propylene glycol (0.3%), but Systane Gel Drops has a higher concentration of one of its excipients (hydroxypropyl guar). Systane Gel Drops is formulated with a pH of 7.0 and a relatively low viscosity; once exposed to the higher ocular pH, cross-linking of hydroxypropyl guar with borate results in the formation of a gel that helps to adhere the demulcents to the ocular surface.
This randomized study investigated the change in sodium fluorescein (NaFl) corneal staining of patients with dry eye after 6 weeks of treatment with PEG-containing lubricant eye drops (PEG 400 0.4%, propylene glycol 0.3%; Systane Gel Drops) or carboxymethylcellulose sodium (CMC)-containing lubricant eye drops (CMC 1%; Refresh Liquigel).
Materials and methods
Patients
Investigators from 10 study sites in the US recruited patients aged ≥18 years with a NaFl corneal staining sum score ≥3 in either eye and best-corrected visual acuity of 0.6 logarithm of the minimum angle of resolution (logMAR) or better in each eye who were already using a lubricant eye gel or ointment at least once weekly over the previous month. Key exclusion criteria included any ocular or systemic medical condition that may, in the opinion of the investigator, preclude safe administration of treatment or affect the results of the study, including inability to discontinue use of concomitant topical ocular drops during the study period (no washout period was required before the screening/baseline visit), previous ocular or intraocular surgery, intolerance or hypersensitivity to any component in the study medications, ocular infections within the last 30 days, temporary punctal plugs, permanent punctal plugs inserted ≤30 days before screening, punctal occlusion performed ≤30 days before screening, use of systemic medications that may contribute to dry eye (unless on a stable dosing regimen for ≤30 days before screening), active iritis or uveitis, or unwillingness to discontinue contact lens wear starting one week or more before screening.
Study design
This was a randomized, parallel-group, multicenter, double-blind, 6-week clinical trial of patients with dry eye using PEG-containing lubricant eye drops (PEG 400 0.4%, propylene glycol 0.3%; Systane Gel Drops) or CMC-containing lubricant eye drops (CMC 1%; Refresh Liquigel). The protocol was approved by all relevant institutional review boards, and the study was performed in compliance with the Declaration of Helsinki and Good Clinical Practice. All patients provided written informed consent.
At the screening/baseline visit, patients were assessed for eligibility, and an ophthalmic examination was conducted using best-corrected visual acuity, evaluation of ocular signs (eyelids, conjunctiva, iris, anterior chamber, and lens), NaFl tear film break-up time, lissamine green conjunctival staining, and NaFl corneal staining. NaFl corneal staining was evaluated using the National Eye Institute scale (five areas: 3 maximum points per area; 15 total points). Patients also completed the Single Symptom Comfort Scale and the Ocular Symptoms Questionnaire at the screening/baseline visit.
Eligible patients were enrolled and randomly assigned in a 1:1 ratio to one of the two eye drops and instructed to instill one drop four times daily in both eyes for 6 weeks. At the week 1 visit (7±2 days), week 2 visit (14±2 days), and week 4 visit (28±3 days), patients were assessed by NaFl tear film break-up time, NaFl corneal staining, and lissamine green conjunctival staining, and completed the Single Symptom Comfort Scale and the Ocular Symptoms Questionnaire. At the week 6 visit (42±3 days), patients were assessed by best-corrected visual acuity, evaluation of ocular signs, NaFl tear film break-up time, NaFl corneal staining, and lissamine green conjunctival staining; patients also completed the Patient Global Assessment of Improvement, Single Symptom Comfort Scale, Ocular Symptoms Questionnaire, and Impact of Dry Eye on Everyday Life (IDEEL) Treatment Satisfaction/Treatment Bother Questionnaire. Patient compliance was assessed at all on-therapy study visits by asking study participants about the frequency of use of their assigned study treatment since their last visit.
Assessments
Efficacy parameters included ocular staining, tear film breakup time, and patient-reported outcomes. The primary efficacy outcome was mean change from baseline to week 6 in NaFl corneal staining. Supportive efficacy outcomes were NaFl corneal staining at weeks 1, 2, and 4; lissamine green conjunctival staining and NaFl tear film break-up time at weeks 1, 2, 4, and 6; Patient Global Assessment of Improvement and IDEEL Treatment Satisfaction/Treatment Bother Questionnaire at week 6; and Single Symptom Comfort Scale and Ocular Symptoms Questionnaire at weeks 1, 2, 4, and 6.
For the corneal staining, 5 μL of NaFl nonpreserved dye were instilled into each eye. Investigators were instructed to wait at least 3 minutes before evaluating the staining using a slit lamp through a cobalt blue filter. Similarly, for the conjunctival lissamine green staining, 5 μL of nonpreserved lissamine green dye were instilled. Investigators were instructed to wait 2–3 minutes before examining the staining using a slit lamp with low intensity white light.
Safety outcomes comprised solicited and unsolicited adverse events. Adverse events (coded using the Medical Dictionary for Regulatory Activities, version 13.0) were recorded throughout the study and at each visit.
Statistical methods
This was a descriptive study; therefore, there were no testable hypotheses. Descriptive statistics were calculated for demographic and baseline characteristics and all efficacy and safety outcomes. With a sample size of approximately 75 patients in each treatment group and a standard deviation (SD) of ±2.4, this study was powered to detect a difference of approximately 0.77 from the observed difference in means. All patients who received study medication were included in the safety population. All data analyses were performed in the intent-to-treat population (defined as all randomized patients with post-baseline data). Missing data were not imputed. If both eyes were eligible for the study both were treated with study medication but only the eye with the worse total corneal staining score at baseline was selected for analysis (if equal, the right eye was used).
Estimates of the differences in treatment means and the two-sided 95% confidence intervals (CIs) of differences from two-sample t-tests were provided for observed change from baseline data for NaFl corneal staining, lissamine green conjunctival staining, NaFl tear film break-up time, Symptom Comfort Scale, and Ocular Symptoms Questionnaire. Additionally, P-values from one-sample t-tests for within-treatment change from baseline to week 6 were provided for NaFl corneal staining. All CIs and P-values were provided for descriptive purposes only. Patient Global Assessment of Improvement responses were dichotomized and frequencies describing improvement (score 1–3) and no change/worsening (score 0 to −3) were calculated. IDEEL Treatment Satisfaction/Treatment Bother responses were dichotomized and frequencies describing positive (most/all of the time [score 3–4] versus none/little/some of the time [score 0–2]) and negative (none/little of the time [score 0–1] versus some/most/all of the time [score 2–4]) responses were calculated. Exact CIs for difference between study medications were provided. For the week 6 visit, P-values using Fisher’s Exact test were provided for descriptive purposes only. A significance level of 0.05 was used for all analyses. Statistical analyses were performed using SAS (SAS Institute, Cary, NC, USA).
Results
Patients
A total of 147 patients were enrolled in the study (PEG group, n=73; CMC group, n=74), which was conducted from January 21, 2011, to April 1, 2011. All 147 patients were included in the intent-to-treat/safety population. Ten patients discontinued during the study; six patients from the PEG eye drops group discontinued because of patient decision (n=3) and other reasons (n=3), and four patients from the CMC eye drops group discontinued because of adverse events (n=3) and patient decision (n=1).
Patient demographics and baseline characteristics were similar between groups (Table 1). More than three quarters of the patients were women, and the mean ± SD age in the overall population was 57±16 years. Compliance with the dosing regimen was high in both treatment groups across all visits (97.3%–100.0% of patients in the PEG group and 95.9%–100.0% of patients in the CMC group).
Table 1.
Patient demographics
| Demographics | PEG eye drops (n=73) | CMC eye drops (n=74) |
|---|---|---|
| Age | ||
| Mean ± SD, years | 56.5±15.0 | 57.5±16.6 |
| <65 years, n (%) | 50 (69) | 45 (61) |
| ≥65 years, n (%) | 23 (32) | 29 (39) |
| Race, n (%) | ||
| White | 65 (89) | 68 (92) |
| Black | 6 (8) | 4 (5) |
| Asian | 1 (1) | 2 (3) |
| Other | 1 (1) | 0 |
| Gender, n (%) | ||
| Male | 15 (21) | 17 (23) |
| Female | 58 (79) | 57 (77) |
Abbreviations: CMC eye drops, carboxymethylcellulose sodium 1% eye drops; Peg eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops.
Corneal staining
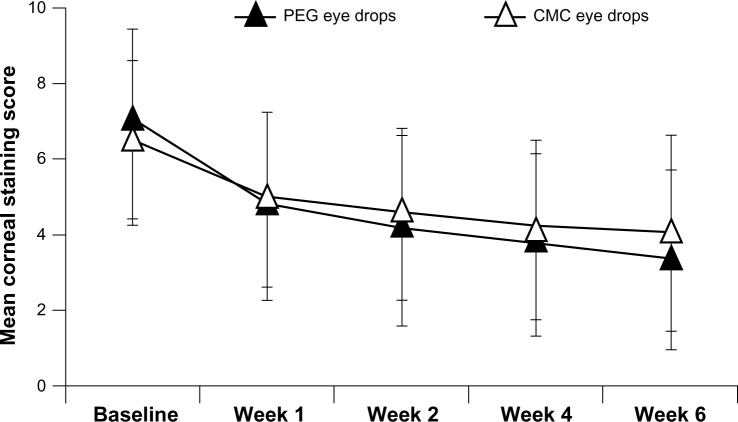
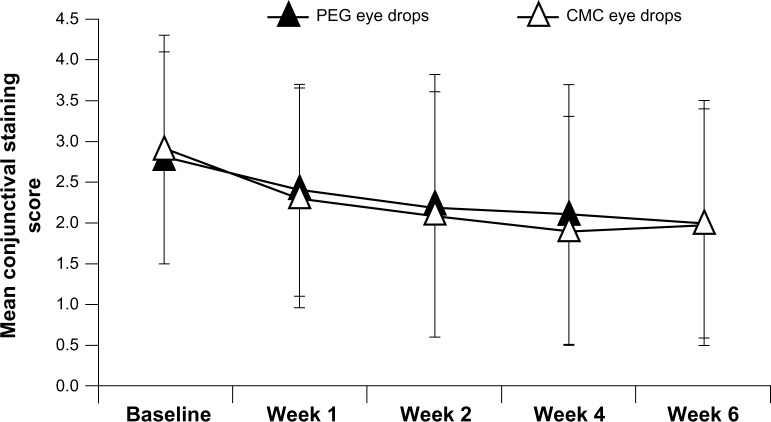
At baseline, mean ± SD corneal staining scores were 6.9±2.5 units with PEG eye drops (n=73) and 6.4±2.2 units with CMC eye drops (n=74), as shown in Figure 1. At every post-baseline visit, mean corneal staining scores were slightly lower in the PEG group than in the CMC group. At week 6, mean corneal staining scores were 3.3±2.4 units with PEG eye drops (n=67) and 4.0±2.6 units with CMC eye drops (n=70). Corneal staining was significantly reduced from baseline to week 6 for both the PEG (−3.4±2.5 units, P<0.0001, 49% reduction) and CMC (−2.5±2.6 units, P<0.0001, 39% reduction) groups (Figure 2). PEG-containing drops showed a significantly greater decrease (ie, improvement) in mean sum of corneal staining from baseline than CMC-containing drops (P=0.0294).
Figure 1.
Mean ± standard deviation NaFl corneal staining scores across visits.
Abbreviations: CMC eye drops, carboxymethylcellulose sodium 1% eye drops; NaFl, sodium fluorescein; PEG eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops.
Figure 2.
Mean ± standard deviation change in NaFl corneal staining scores from baseline to the week 6 visit.
Abbreviations: CMC eye drops, carboxymethylcellulose sodium 1% eye drops; NaFl, sodium fluorescein; PEG eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops.
Conjunctival staining
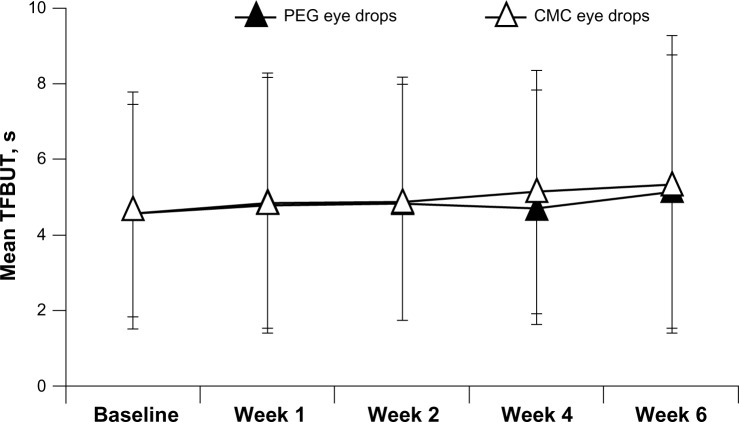
At baseline, mean lissamine green conjunctival staining scores were 2.8±1.3 units in the PEG group and 2.9±1.4 units in the CMC group (Figure 3). At each visit, differences in mean conjunctival staining scores were ≤0.2 units between groups. No significant differences between groups were observed in mean scores or in change from baseline scores at any visit.
Figure 3.
Mean ± standard deviation conjunctival staining scores across visits.
Abbreviations: CMC eye drops, carboxymethylcellulose sodium 1% eye drops; PEG eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops.
Tear film break-up time
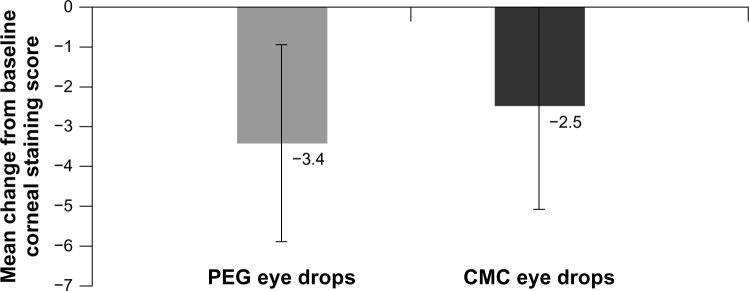
At baseline, the mean tear film break-up time was 4.6±2.8 seconds with PEG eye drops and 4.6±3.1 seconds with CMC eye drops (Figure 4). At each visit, differences in mean tear film break-up time were ≤0.4 seconds between groups. No significant differences were observed between treatment groups in mean scores or in change from baseline scores.
Figure 4.
Mean ± standard deviation NaFl tear film break-up time across visits.
Abbreviations: CMC eye drops, carboxymethylcellulose sodium 1% eye drops; NaFl, sodium fluorescein; PEG eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops; s, seconds; TFBUT, tear film break-up time.
Patient-reported outcomes
At week 6, the percentages of patients reporting improvement on the Patient Global Assessment of Improvement was 85% in the PEG group and 74% in the CMC group (P=0.1383). Mean change from baseline to week 6 on the Single Symptom Comfort Scale was −2.1±2.0 for the PEG group and −1.6±1.9 for the CMC group; there were no statistically significant between-group differences at any visit for mean score or change from baseline scores.
With the Ocular Symptoms Questionnaire, no significant differences were observed between groups in mean changes from baseline to week 6 for any of the following questions: “Do your eyes feel dry?” (−1.2±1.1 and −1.3±1.1 for PEG versus CMC eye drops, respectively), “Do you feel a gritty or sandy sensation in your eyes?” (−0.9±1.1 versus −1.0±1.1), “Do your eyes have a burning sensation?” (−0.9±1.0 versus −1.0±1.0), “Are your eyes red?” (−0.6±1.0 versus −0.8±1.1), and “Do you notice crusting on your lashes?” (−0.1±1.3 versus 0.1±1.3). Furthermore, there were no significant changes between groups for mean scores or mean change from baseline scores at any visit.
With the IDEEL Treatment Satisfaction/Treatment Bother Questionnaire at week 6, responses were similar between treatment groups for all but one statement (“I was bothered by blurriness shortly after using my eye drops”), for which responses were significantly better with CMC eye drops (patients answering “none of the time” or “a little of the time”: 24% in the PEG group versus 41% in the CMC group; P=0.0310). Responses were not significantly different with PEG-containing versus CMC-containing eye drops at week 6 for the following statements: “I was happy with how quickly my treatment worked” (patients answering “most of the time” or “all the time”: 70% in the PEG group versus 54% in the CMC group); “I was happy with how long the effects of my treatment lasted” (“most of the time” or “all the time”: 60% versus 56%); “The treatment I used completely eliminated my dry eye symptoms” (“most of the time” or “all the time”: 49% versus 39%); “The treatment I used relieved most of my dry eye symptoms” (“most of the time” or “all the time”: 60% versus 51%); “I was bothered by how often I had to use dry eye treatments” (“none of the time” or “a little of the time”: 66% versus 67%); “I was embarrassed when I had to use my eye drops” (“none of the time” or “a little of the time”: 97% versus 97%); and “I felt like I could not go anywhere without my eye drops” (“none of the time” or “a little of the time”: 57% versus 60%).
Safety
No safety issues were identified in a population of patients with dry eye using PEG eye drops for up to 42 days, based on a review of adverse events (Table 2). The following treatment related adverse events were observed in the PEG and CMC groups: eye pruritus (n=2 [3%] and n=0 [0%] events, respectively), eyelid margin crusting (n=1 [1%] and n=4 [5%]), foreign body sensation in eyes (n=1 [1%] and n=2 [3%]), abnormal sensation in eye (n=0 [0%] and n=1 [1%]), and eye irritation (n=0 [0%] and n=1 [1%]). Adverse events related to eye disorders (ie, eyelid margin crusting, foreign body sensation, eye pain, dry eye, eye pruritus, decrease in visual acuity, abnormal sensation, eye allergy, and eye irritation) were observed in nine cases (12%) in six patients using PEG eye drops, and in 15 cases (20%) in ten patients using CMC eye drops (Table 2). Other treatment-emergent adverse events (occurring in ≥2% of patients) were nasopharyngitis, upper respiratory tract infection, and seasonal allergy (Table 2).
Table 2.
Adverse events in safety population
| n (%) | PEG eye drops (n=73) | CMC eye drops (n=74) |
|---|---|---|
| Patients experiencing one or more AE | 14 (19) | 22 (30) |
| Treatment-emergent AEs related to eye disorders | ||
| Foreign body sensation in eyes | 3 (4) | 2 (3) |
| Eyelid margin crusting | 2 (3) | 4 (5) |
| Eye pruritus | 2 (3) | 0 |
| Eye allergy | 1 (1) | 0 |
| Eye pain | 1 (1) | 3 (4) |
| Dry eye | 0 | 2 (3) |
| Reduced visual acuity | 0 | 2 (3) |
| Abnormal sensation in eye | 0 | 1 (1) |
| Eye irritation | 0 | 1 (1) |
| Other treatment-emergent AEsa | ||
| Nasopharyngitis | 2 (3) | 3 (4) |
| Upper respiratory tract infection | 2 (3) | 1 (1) |
| Seasonal allergy | 0 | 2 (3) |
| Any serious AE | 1 (1)b | 0 |
| AEs leading to discontinuation | 0 | 3 (4)c |
Notes:
Occurring in ≥2% of either group
nephrolithiasis, not treatment related
two reports of moderate dry eye and one report of moderate eye pain; none were treatment related.
Abbreviations: AE, adverse event; CMC eye drops, carboxymethylcellulose sodium 1% eye drops; PEG eye drops, polyethylene glycol 0.4%, propylene glycol 0.3% eye drops.
One patient using PEG-containing drops experienced a serious adverse event (nephrolithiasis) not related to treatment during the study. Three patients in the CMC group discontinued the study because of adverse events not related to treatment (dry eye [n=2], eye pain [n=1]), whereas no patient in the PEG group discontinued the study because of an adverse event.
Discussion
Dry eye is characterized by tear film instability and ocular surface damage. Methods for diagnosis and evaluation of dry eye have not been standardized; however, certain tests produce information that is indicative of the condition of the ocular surface. Corneal and conjunctival staining, for example, are recommended as the best means of assessing ocular surface damage and dysfunction.13,14 Staining is particularly useful in the diagnosis and monitoring of more severe dry eye.3 The primary objective of this randomized, double-blind clinical study was to evaluate mean change from baseline to week 6 in NaFl corneal staining scores, as a sign of dry eye, in patients receiving PEG-containing or CMC-containing eye drops. Patients taking either type of eye drop showed significant reductions in corneal staining scores at week 6 compared with baseline, but improvements with PEG eye drops were significantly better than with CMC eye drops. These results indicate that ocular surface damage may be ameliorated to a greater degree with this PEG restorative eye drops formula than with CMC eye drops after 6 weeks of treatment. However, changes in conjunctival staining scores, tear film break-up time, and patient-reported outcomes were not significantly different between groups. Because dry eye is a multifactorial disease, a treatment difference observed in a single study parameter may not translate to a clinically meaningful difference in the management of dry eye symptoms. Both treatments were well tolerated.
Generic patient-reported outcomes and dry eye-specific patient-reported outcomes can be used to better differentiate efficacy data between dry eye treatments. Patient questionnaires are recommended for screening and diagnosis of dry eye, and these questionnaires can be used to guide treatment because results of subjective assessments of patient symptoms are repeatable over time.15–17 In the current study, a majority of patients using PEG-containing eye drops reported improvement in dry eye at week 6, with a slightly higher percentage of patients indicating symptom improvement with PEG versus CMC eye drops in the Patient Global Assessment of Improvement. Changes in the Single Symptom Comfort Scale and Ocular Symptoms Questionnaire were similar between groups. A majority of patients indicated satisfaction with PEG eye drops in the IDEEL Treatment Satisfaction questionnaire, with the exception of the question relating to complete elimination of dry eye symptoms; scores on this scale were similar between groups, except that a lower percentage of patients in the CMC group indicated blurriness after drop installation compared with those in the PEG group.
There are a few limitations to the current study design. A comparator was used rather than a placebo control. Although this study design is a commonly used approach for evaluating drops for dry eye,5,18 it does not allow direct comparison with untreated individuals. Also, use of separate patient populations for each treatment group (ie, a non-crossover design) raises the possibility that the results may be attributable to intrinsic differences in the two populations (eg, concomitant disorders); however, general baseline characteristics (eg, age, race) were similar between treatment groups. Further, corneal surface defects were evaluated solely with NaFl staining, which may not be a specific or sensitive measure of dry eye symptoms.19 In addition, because patients enrolled in clinical trials may be more compliant with treatment,16 the improvements in dry eye symptoms observed in this trial may not be directly generalizable to all patients treated for dry eye. Long-term studies may be needed to assess the safety and efficacy of PEG-containing drops for extended use.
In summary, patients with dry eye receiving four times daily PEG-containing eye drops showed better NaFl corneal staining that was statistically significant and a somewhat improved adverse event profile compared with those receiving CMC-containing drops after 6 weeks of treatment. These data are consistent with the mechanism of action of PEG-containing drops, which is to provide ocular surface protection. Results of conjunctival staining, tear film break-up time analysis, and patient-reported outcomes were not significantly different between treatments. Both treatments were well tolerated, and no safety issues were identified.
Footnotes
Disclosure
This study was funded by Alcon Laboratories Inc (Fort Worth, TX, USA). Medical writing support was provided by Peter A Rittenhouse of Complete Healthcare Communications Inc (Chadds Ford, PA, USA), and was funded by Alcon. SC and KS report no conflicts of interest in this work. AM is an employee of Alcon Laboratories Inc.
References
- 1.Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472–478. doi: 10.1097/ICO.0b013e318225415a. [DOI] [PubMed] [Google Scholar]
- 2.Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405–412. doi: 10.2147/opth.s5555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.International Dry Eye Workshop The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5(2):75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 4.McGinnigle S, Naroo SA, Eperjesi F. Evaluation of dry eye. Surv Ophthalmol. 2012;57(4):293–316. doi: 10.1016/j.survophthal.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Jacobi C, Kruse FE, Cursiefen C. Prospective, randomized, controlled comparison of Systane UD eye drops versus Visine Intensiv 1% EDO eye drops for the treatment of moderate dry eye. J Ocul Pharmacol Ther. 2012;28(6):598–603. doi: 10.1089/jop.2012.0066. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan DA, Hammitt KM, Schaumberg DA, et al. Report of the TFOS/ARVO Symposium on global treatments for dry eye disease: an unmet need. Ocul Surf. 2012;10(2):108–116. doi: 10.1016/j.jtos.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Cuevas M, Gonzalez-Garcia MJ, Castellanos E, et al. Correlations among symptoms, signs, and clinical tests in evaporative-type dry eye disease caused by Meibomian gland dysfunction (MGD) Curr Eye Res. 2012;37(10):855–863. doi: 10.3109/02713683.2012.683508. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan BD, Crews LA, Sonmez B, et al. Clinical utility of objective tests for dry eye disease: variability over time and implications for clinical trials and disease management. Cornea. 2012;31(9):1000–1008. doi: 10.1097/ICO.0b013e318242fd60. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2012 Dec 28; doi: 10.1111/aos.12012. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 10.Lemp MA, Bron AJ, Baudouin C, et al. Tear osmolarity in the diagnosis and management of dry eye disease. Am J Ophthalmol. 2011;151(5):792–798. e791. doi: 10.1016/j.ajo.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 11.Sullivan BD, Whitmer D, Nichols KK, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010;51(12):6125–6130. doi: 10.1167/iovs.10-5390. [DOI] [PubMed] [Google Scholar]
- 12.Benelli U. Systane lubricant eye drops in the management of ocular dryness. Clin Ophthalmol. 2011;5:783–790. doi: 10.2147/OPTH.S13773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Dry Eye Workshop Design and conduct of clinical trials: report of the Clinical Trials Subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5(2):153–162. doi: 10.1016/s1542-0124(12)70084-8. [DOI] [PubMed] [Google Scholar]
- 14.Stevenson W, Chauhan SK, Dana R. Dry eye disease: an immune-mediated ocular surface disorder. Arch Ophthalmol. 2012;130(1):90–100. doi: 10.1001/archophthalmol.2011.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nichols KK. Patient-reported symptoms in dry dye disease. Ocul Surf. 2006;4(3):137–145. doi: 10.1016/s1542-0124(12)70040-x. [DOI] [PubMed] [Google Scholar]
- 16.International Dry Eye Workshop Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye Workshop. Ocul Surf. 2007;5(2):108–152. doi: 10.1016/s1542-0124(12)70083-6. [DOI] [PubMed] [Google Scholar]
- 17.Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea. 2004;23(3):272–285. doi: 10.1097/00003226-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Wang TJ, Wang IJ, Ho JD, et al. Comparison of the clinical effects of carbomer-based lipid-containing gel and hydroxypropyl-guar gel artificial tear formulations in patients with dry eye syndrome: a 4-week, prospective, open-label, randomized, parallel-group, noninferiority study. Clin Ther. 2010;32(1):44–52. doi: 10.1016/j.clinthera.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 19.Savini G, Prabhawasat P, Kojima T, et al. The challenge of dry eye diagnosis. Clin Ophthalmol. 2008;2(1):31–55. doi: 10.2147/opth.s1496. [DOI] [PMC free article] [PubMed] [Google Scholar]