Abstract
Female sex workers (FSWs) in China are exposed to multiple work-related harms that increase HIV vulnerability. Using mixed-methods, we explored the social-ecological aspects of sexual risk among 348 FSWs in Beijing. Sex-work harms were assessed by property stolen, being underpaid or not paid at all, verbal and sexual abuse, forced drinking; and forced sex more than once. The majority (90%) reported at least one type of harm, 38% received harm protection from ‘mommies’ (i.e., managers) and 32% reported unprotected sex with clients. In multivariate models, unprotected sex was significantly associated with longer involvement in sex work, greater exposure to harms, and no protection from mommies. Mommies’ protection moderated the effect of sex-work harms on unprotected sex with clients. Our ethnography indicated that mommies played a core role in sex-work networks. Such networks provide a basis for social capital; they are not only profitable economically, but also protect FSWs from sex-work harms. Effective HIV prevention interventions for FSWs in China must address the occupational safety and health of FSWs by facilitating social capital and protection agency (e.g., mommies) in the sex-work industry.
Keywords: female sex workers, sex-work harms, social ecology, China, social capital
Introduction
Female sex workers (FSWs) are enmeshed in a web of complex interactions among owners of sex-work establishments, managers, clients, non-paid steady partners, brokers in the sex-work industry, local law-enforcement authorities and public health agencies (Harcourt and Donovan 2005). The work conditions and daily lives of FSWs are affected by the ways in which these interactions influence each other. Within sex-work environments, FSWs are exposed to multiple work-related harms (sex-work harms hereafter), such as violence, alcohol and drug dependency, stigmatisation and discrimination, debt, criminalisation and exploitation (Rekart 2005), which potentially can increase transmission of HIV and sexually transmitted infections (STIs).
These sex-work harms are context-specific, with risk and vulnerability shaped by variations in sex-work structures, especially in the thriving sex industry in China. The country’s urbanisation has led to massive rural-to-urban migration, gender inequality in economic sectors and the proliferation of sex work, resulting in the resurgence of STIs, which has a potential to escalate rapid diffusion of HIV (Gil et al. 1996, Chen et al. 2000). Empirical data on the effects of these harms on HIV risk among FSWs are, however, limited (Pirkle et al. 2007). Most studies focus on disease surveillance and individual exposure to HIV risk, and prevention interventions largely use cognitive-behavioural strategies (Hong and Li 2009). Such emphasis on behavioural change at the individual-level fails to consider how the sex-work structure facilitates a risk environment where a formal protection system is almost non-existent.
Social ecology of sex-work environment
As a social-ecological approach focuses on the environment in terms of its physical and social components, qualities and networks among the factors and resources (Poundstone et al. 2004), it directs attention to the occupational hazards of sex work, which often are regarded as unalterable ‘risks of trade’ or a ‘trade-off of work’ (Alexander 1998, Wolffers and van Beelen 2003, Shannon and Csete 2010). Globally, research about FSWs has addressed the importance of the sex-work environment as an enabler of health promotion and occupational health by increasing proximity to health resources, enhancing the quality of work-related conditions, reducing the occurrence of violence and encouraging safer sex norms (Kerrigan et al. 2006).
There has also been growing recognition of the importance of environmental context in terms of its effect on HIV risk among FSWs in China. Several studies developed typologies of sex-work environments based on the degree of exposure to risk factors and the social climate, such as economic gain, organisational dynamics with managers and power relationships with clients (Huang et al. 2004, Choi and Holroyd 2007, Fang et al. 2007). This kind of venue-level analysis across settings provides insight into the socio-economic hierarchy of the sex-work industry and its relationship to HIV risk. Yet, relatively little empirical data focus on a within-structure analysis of the impact of sex-work harms on HIV risk, and relational attributes of HIV risk and protection in the network (Yi et al. 2010). In China, societal stigmatisation of sex work precludes public-health systems from acknowledging these risks as occupational hazards. However, viewing sex work through the lens of occupational safety can contribute new theoretical insights about the contextual determinants and potential pathways by which the characteristics of the workplace, including organisational culture, working conditions and managers’ attitudes, enhance HIV risk and protection behaviour among FSWs.
Violence is one of the most frequent occupational sex-work harms faced by FSWs. It occurs in various forms, including physical, verbal and sexual abuse; rape; robbery; kidnapping; and murder. Lack of any system to protect FSWs in China against workplace violence increases their risk of being easy targets for harassment and violence. Violence against FSWs is often tolerated and justified as ‘normative’ or ‘part of the job’; therefore, they are reluctant to report incidents to the authorities, or to even seek help from their managers. Some FSWs resort to habitual alcohol or drug use as a survival adaptation to a traumatic environment, in some cases diminishing their appreciation of the importance of health (Rekart 2005). When health needs and the reduction of work-related stress are viewed as lower priorities than economic gain, the institutional culture of sex work may undermine HIV-prevention efforts.
Within the sex-work industry in China, ‘mommies’, like agents in any other business, play an important role as the intermediaries for sexual business. With their experience in sex work, they ensure the financial revenue of the establishment, which is often proven by their ‘assets’ (e.g., the number/list of clients and FSWs whom they manage). In the HIV-prevention literature, mommies are usually regarded as ‘gatekeepers’ to the FSW community (Yang et al. 2005, Cheng and Mak 2010), yet their role in the management of occupational health and safety is poorly understood. Thus, it is critical to determine whether and how the roles of mommies can be utilised for HIV-prevention agency. In this study, we first explored to what extent sex-work harms and mommies’ protection of FSWs from the harms influence sexual risk among FSWs (quantitative analysis). We also explore how the structure of sex work would provide a foundation for informal and formal cooperation among FSWs and mommies to prevent harms and promote safer sex (qualitative analysis).
Study setting and design: mixed methods
The current study was based on a community HIV-prevention project among FSWs in a low-middle income neighbourhood (‘Fourth Ring’) in Beijing’s north-western district. As part of the project, the project-leading NGO established a drop-in centre for FSWs, funded by a UN developmental agency in China. The NGO rented a hotel room in the neighbourhood (where sex-work services were offered) for the drop-in centre so that FSWs would not feel ‘checked or seen’ by others. The drop-in centre provides not only free condoms but also a place for social gatherings (e.g., Chinese chess, Internet and yoga are offered). The centre also provides meetings with social workers and a retired Obstetrics and Gynecology female doctor for a free STI checkup once per week.
In order to enrich our social-ecological investigations, we conducted a mixed-methods analysis, based on a sequential explanatory design in which the collection and analysis of quantitative data was followed by the collection and analysis of qualitative data (Tashakkori and Teddlie 2003). Our first source of quantitative data was a needs assessment. We first conducted participatory mapping in the community, establishing a partnership with various sex-work venues via FSW volunteers and mommies, who were knowledgeable about the community. They received training on participatory research ethics by the project director. A cross-sectional survey was conducted between November 2008 and January 2009 since many migrant women come to Beijing in the winter to earn money during the non-agricultural season in their rural hometowns.
Based on the findings from the survey about the relationship between sex-work harm, protection and sexual risk, the first author conducted ethnographic interviews with mommies in the community to explore and corroborate the quantitative findings of the role of mommies, focusing on social capital for HIV prevention in sex-work settings. The informants of mommies were recruited from a self-support group named ‘broken-wing angels’ (zheyitianshi), which they formed for themselves through our HIV-prevention project. The group consists of approximately 10 mommies. Most of them were former FSWs, each managed 15–20 FSWs and none is an owner of a sex-work establishment. The interviews were conducted with verbal consent either in the drop-in centre or their workplaces during daytime. The second social-political source of data was drawn from the second author’s ethnography of 2 years of participant observation in sex-work establishments while she lived and worked as a hostess without providing sexual services to clients (Zheng 2009). During her field study, she interacted with 200 FSWs from 10 karaoke bars and witnessed the operation of the sex-work industry, including police crackdowns on sex-work establishments. The ethnographic data elaborated how mommies protected FSWs and secured their business. We triangulated the findings from the three sources to provide a contextual explanation of how mommies play a role as a protection agency in the dynamics of sex-work harms and HIV risk in the sexual organisation of the study community.
Quantitative needs assessment
Sample and procedures
Using a venue-based target sampling method, a diverse sample of 348 FSWs was recruited from karaoke bars (‘KTV’) (36%), nightclubs (11%), hotels (7%), saunas and bathhouses (19%), footbath and hair salons (10%) and roadside brothels and streets (17%). Eligibility for study participation was being a female over 18 years of age who was involved in sex work at the time of the survey. To ensure participants’ safety and privacy, after informed consent, the survey was conducted in a private space at the work site or the drop-in centre. Although the survey was self-administered, a trained interviewer was available to address any questions that participants had. Participants received a quilt after completing the survey as compensation. The survey was developed in Chinese with the guidance of the funding institution and reviewed by the FSW volunteers for cultural sensitivity and language appropriateness. The questionnaire was then translated into English and the first author checked the content validity of the English translation. The ethics approvals were obtained from the authors’ affiliated universities.
Measures
The domains of analysis included: (1) demographic characteristics including migration; (2) sex-work background (e.g., duration and type of sex work) and working conditions (e.g., police arrest); (3) HIV knowledge and history of STI symptoms (e.g., discomfort in genital area, vaginal discharge, dryness, and smell, lower abdominal pain and painful urination) in the past year; and (4) illicit drug use in the past year. HIV knowledge measured by 14 true/false items demonstrated good internal-consistency reliability (Kuder-Richardson 20 Coefficient=0.78). Sex-work settings were categorised as: (1) entertainment establishments, (2) personal hygienic services and (3) street-based brothels (see Yi et al. 2010). Sex-work harms were assessed in seven domains: (1) property stolen during sex work, (2) being underpaid or not paid at all, (3) physical abuse, (4) verbal abuse, (5) sexual abuse, (6) forced alcoholic drinking and (7) forced sex more than once. As an indicator of mommies’ protection against harms, we used the following two statements (1) whether FSWs received help from their mommies when any of the harmful incidents above occurred and (2) whether their mommies’ protection was helpful. Those who responded ‘yes’ to both were considered as receiving protection from mommies. Our primary outcome was unprotected sex with clients (USC) in the past 3 months.
Statistical analysis
We described the study variables and conducted logistic regressions for the outcome. Variables with a Wald statistic significant at the p <0.10 were retained for multivariate analysis. Multiple regressions were performed to determine independent predictors using the covariates retained from bivariate regressions. Covariates at the p>0.05 were subsequently removed, and likelihood ratio tests compared between the reduced and full models to ascertain the improvement of the model. This process continued until all covariates were significant (p<0.05). We computed 95% of confidence intervals for crude and adjusted odds ratios (AOR) in testing the measure of association. Lastly, based on our research interest in the role of mommies, we explored possible interactions among the main effects by testing the following hypotheses: (1) there would be a positive association between sex-work harms and USC and (2) mommies’ protection of FSWs would moderate the effect of sex-work harms on USC.
Results
Characteristics of participants
Table 1 presents demographic and sex-work background characteristics of the sample. Participants ranged in age from 19 to 45 years old (M=29.0, SD=6.1). About one-quarter (24%) had either not gone to school or only completed elementary school. With respect to origin of migration, slightly more than two-thirds (68%) of FSWs came from a rural area, 24% migrated from county-level cities and 8% from provincial capitals. Approximately one-third (32%) stayed in Beijing for less than 1 year. The majority of FSWs were either married or divorced, or lived with their partners, while 30% were single. Slightly more than half (55%) worked in entertainment establishments, 28% worked in personal hygienic services and 17% worked on the ‘street’ or in roadside brothels. Forty-two percent of the FSWs reported a monthly income of less than US$450 (approximately 3000 Yuan; 3726 Yuan is the average monthly income among Beijing residents).
Table 1.
Demographic and sex-work background characteristics by unprotected sex with clients.
| Total (N=348)
|
Unprotected sex with clients (N=111, 31.9%)
|
||
|---|---|---|---|
| N (%) | N (%) | Crude OR (95% CI) | |
| Demographic characteristics | |||
| Age (M, SD) | 29.0 (6.1) | 29.5 (6.5) | 1.02 (0.98–1.06) |
| Always use condom with clients | 28.8 (5.9) | – | |
| 18–20 years | 27 (7.8) | 11 (40.7) | – |
| 21–30 years | 191 (54.9) | 53 (27.7) | 0.56 (0.24–1.28) |
| 31–40 years | 117 (33.6) | 44 (37.6) | 0.88 (0.37–2.06) |
| 41–50 years | 13 (3.7) | 3 (23.1) | 0.44 (0.01–1.96) |
| Education | |||
| Primary school | 83 (23.8) | 29 (34.9) | – |
| Middle school | 169 (48.6) | 50 (29.6) | 0.81 (0.52–1.28) |
| Completed high school | 96 (27.6) | 28 (29.2) | 0.84 (0.50–1.40) |
| Origin of migration | |||
| Rural town | 236 (67.8) | 72 (30.5) | – |
| County-level city | 84 (24.1) | 30 (35.7) | 1.26 (0.75–2.11) |
| Provincial capital | 28 (8.0) | 9 (32.1) | 1.01 (0.44–2.32) |
| Length of stay in Beijing | |||
| <1 year | 112 (32.2) | 26 (23.2) | – |
| >1 year | 236 (67.8) | 85 (36.0) | 1.86 (1.12–3.11)* |
| Relationship status | |||
| Single | 105 (30.2) | 25 (23.8) | – |
| Divorced | 83 (23.9) | 22 (26.5) | 0.71 (0.41–1.24) |
| Cohabitation | 70 (20.1) | 36 (51.4) | 2.87 (1.67–4.91)*** |
| Married | 90 (25.9) | 28 (31.1) | 0.95 (0.57–1.60) |
| Sex-work background | |||
| Type of sex work | |||
| Entertainment | 191 (54.9) | 61 (31.9) | – |
| Personal-service | 99 (28.4) | 31 (31.3) | 0.96 (0.58–1.59) |
| Street/brothel-based | 58 (16.7) | 19 (32.8) | 1.05 (0.58–1.91) |
| Monthly incomea | |||
| <450 USD | 145 (41.7) | 40 (27.6) | – |
| 450–750 USD | 98 (28.2) | 35 (35.7) | 1.27 (0.78–2.08) |
| >750 USD | 105 (30.2) | 36 (34.3) | 1.17 (0.72–1.90) |
| Length of sex work** | |||
| <1 year | 175 (50.3) | 41 (23.4) | – |
| >1 year | 173 (49.7) | 70 (40.5) | 2.22 (1.40–3.53)*** |
| Considered sex work as ‘job’ | 200 (57.5) | 65 (32.5) | 1.07 (0.68–1.69) |
| No | 148 (42.5) | 46 (31.1) | |
| STI symptoms | 275 (79.0) | 94 (34.2) | 1.71 (0.94–3.11) |
| No | 73 (21.0) | 17 (23.3) | |
| Drug use | 28 (8.0) | 11 (39.3) | 1.42 (0.64–3.15) |
| No | 320 (92.0) | 100 (31.3) | |
| Arrested by police | 109 (31.3) | 34 (31.2) | 0.95 (0.59–1.55) |
| No | 239 (68.7) | 77 (32.2) | |
| HIV Knowledge* M (SD) | 10.2 (2.9) | 9.6 (2.6) | 0.90 (0.83–0.98)* |
| Always use condom with clients | 10.3 (2.8) | – | |
p <0.05;
p <0.01;
p <0.001.
1000 Chinese Yuan Renminbi (RMB) = 150 US Dollars (USD).
Demographic characteristics of age, education and hometown of migration of the FSWs were not significantly associated with USC. Notably, although there was no difference in USC by age, those who were younger than 20 years old reported a higher rate of USC (41%) compared to other age groups. FSWs living with partners in non-marital relationships reported higher rates of USC than those who were married or single (OR=2.87). Living in Beijing and being involved in sex work for more than 1 year were significantly associated with USC (OR=1.86 and 2.22, respectively). History of having a STI symptom was not associated with USC. The following symptoms were associated with USC: discomfort in genital area (28.2% vs. 39.1%, p=0.048), vaginal dryness and smell (28.1% vs. 47.1%, p=0.002) and urination pain (6.4% vs. 17.0%, p=0.009). Past drug use and arrest by police was not associated with USC. Those reporting higher scores on HIV knowledge were less likely to engage in USC (OR=0.90).
Sex-work harms and HIV risk
Sex-work harms were significantly associated with USC (Table 2). Those FSWs who experienced harms were significantly more likely than those who did not to report USC. Among the sex-work harms variables, physical abuse, rape, forced drinking and forced multiple sex were highly associated with USC (OR=3.56, 11.26, 4.90, and 9.55, respectively; p<0.001 for all). Since most of the sex-work harms variables were related to USC, we constructed a sex-work harm composite index. As shown in Table 2, sex-work harms had a relatively linear relationship with the likelihood of engaging in USC (OR=1.63, 95% CI: 1.40–1.90). For example, among those who never experienced harms only 9.8% reported USC, whereas 100% of those who experienced all types of harms reported USC. In cases of harms, 38% received useful protective help from mommies, 8% from coworkers, 40% dealt with it by themselves, 5% did not know how to deal with it and 9% felt abandoned. Those who did not receive help from mommies were more likely than their counterparts to engage in USC (OR=1.51, 95% CI: 1.18–1.94).
Table 2.
Sex-work harms index by unprotected sex with clients and drug use.
| Total (N= 348)
|
Unprotected sex with clients (N=111, 31.9%)
|
||
|---|---|---|---|
| N (%) | N (%) | Crude OR (95% CI) | |
| Property stolen | 90 (25.9) | 35 (38.9) | 1.52 (0.92–2.52) |
| No | 258 (74.1) | 76 (29.5) | |
| Paid less or no payment | 199 (57.2) | 76 (38.2) | 2.01 (1.25–3.23)* |
| No | 149 (42.8) | 35 (23.5) | |
| Verbally abused | 248 (71.3) | 85 (34.3) | 1.48 (0.88–2.49) |
| No | 100 (28.7) | 26 (26.0) | |
| Physically abused | 156 (44.8) | 73 (46.8) | 3.56 (2.22–5.73)*** |
| No | 192 (55.2) | 38 (19.8) | |
| Raped | 17 (4.9) | 14 (82.4) | 11.26 (3.16–40.06)*** |
| No | 331 (95.1) | 97 (29.3) | |
| Forced drinking | 176 (50.6) | 84 (47.7) | 4.90 (2.96–8.13)*** |
| No | 172 (49.4) | 27 (15.7) | |
| Forced multiple sex | 32 (9.2) | 25 (78.1) | 9.55 (3.99–22.89)*** |
| No | 316 (90.8) | 86 (27.2) | |
| Sex-work harm index (0–7) | 1.63 (1.40–1.90)*** | ||
| 0 | 51 (14.7) | 5 (9.8) | |
| 1 | 47 (13.5) | 11 (23.4) | |
| 2 | 64 (18.4) | 14 (21.9) | |
| 3 | 70 (20.1) | 21 (30.0 | |
| 4 | 67 (19.3) | 21 (43.3) | |
| 5 | 33 (9.5) | 16 (48.5) | |
| 6 | 12 (3.4) | 11 (91.7) | |
| 7 | 4 (1.1) | 4 (100.0) | |
| No protection form mommy | 135 (38.8) | 29 (21.5) | 1.51 (1.18–1.94)** |
| Yes, help for protection | 213 (61.2) | 82 (38.5) | |
p <0.05;
p <0.01;
p <0.001.
Figure 1 shows the rates of USC between those who received help from mommies and those who did not by the number of sex-work harms reported. In the group with mommies’ help, USC increased with an increased number of harms – from 6.3% (no harm reported) to 66.7% (six harms) and no FSWs in the group reported all seven harms. In the group without mommies’ help, the rates of USC increased from 11.4% (no harm) to 100% (seven harms); all of the FSWs who experienced the seven types of harms reported USC (χ2 = 52.5, df=7, p<0.0001). Notably, there was a sharp increase in USC between five and six harms, suggesting harms and USC is highly associated, independent of the mommies’ intervention.
Figure 1.
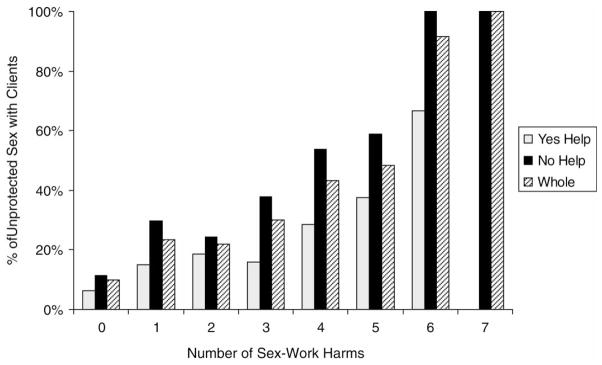
Percentage of unprotected sex with clients by the number of sex-work harms between FSWs who received help from mommies and those who did not.
Multivariate analysis
All the variables found to be significant in bivariate regressions remained for further testing (Table 3). The multiple logistic regressions controlled for potential confounders – age, education, origin of migration, length of stay in Beijing and relationship status – as previous studies of FSWs in China reported that demographic characteristics were related to HIV risk. However, in this study, none of these variables were found to be significant in the models. USC was independently associated with low HIV knowledge (AOR=1.19), longer sex-work involvement (AOR=1.82), higher exposure to sex-work harms (AOR=1.58) and not getting help from mommies (AOR=1.62). Since one of our interests in this study was to explore the role of mommies in the association between sex-work harms and HIV risk, we examined the moderation effects among the predictors. Significant interaction effects were found between sex-work harms and no protection from mommies (AOR=1.11, 95% CI: 1.03–1.21) and sex-work harms, mommies’ protection and length of sex work (AOR=1.02, 95% CI: 1.01–1.04).
Table 3.
Multivariate models for unprotected sex with clients and interaction effects.
| Full model
|
Interaction 1: Sex-work harms×no protection
|
Interaction 2: interaction 1×Sex-work>1 year
|
|
|---|---|---|---|
| Adjusted OR (95% CI) | Adjusted OR (95% CI) | Adjusted OR (95% CI) | |
| 1. HIV knowledge | 1.19 (1.08–1.31)*** | 1.19 (1.08–1.31)*** | 1.20 (1.09–1.32)*** |
| 2. Sex work >1 year | 1.82 (1.37–2.40)*** | 1.83 (1.38–2.42)*** | 1.70 (1.28–2.25)*** |
| 3. Sex-work harms | 1.58 (1.34–1.87)*** | 1.53 (1.27–1.83)*** | 1.59 (1.34–1.89)*** |
| 4. No mommies’ protection | 1.62 (1.23–2.15)** | 1.23 (1.10–2.28)* | 1.45 (1.09–1.94)* |
| 3×4 | 1.11 (1.03–1.21)* | – | |
| 2×3×4 | 1.02 (1.01–1.04)* |
Note: Regression models were controlled for age, education, origin of migration, length of stay in Beijing and relationship status.
p <0.05;
p <0.01;
p<0.001.
Ethnography of the role of mommies
Network position of mommies
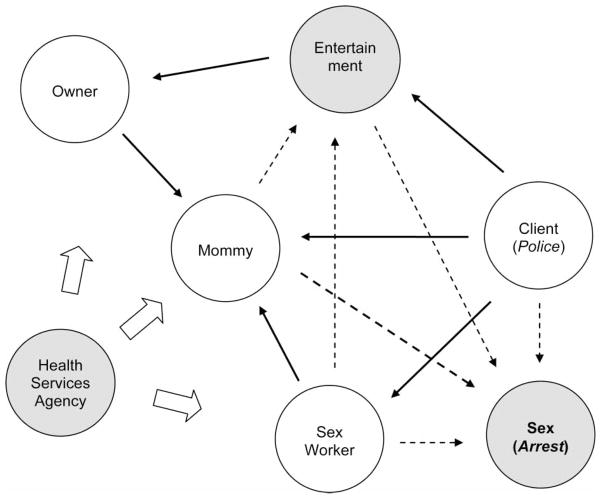
An ethnographic inquiry about the business-agency role of mommies led us to draw a network diagram of the flow of money and services in sex-work environments. As shown in Figure 2, mommies are positioned as a core in the network. During ‘onstage’ entertainment, FSWs accompany clients in singing, dancing, drinking and playing games. When a client wants to have sex with a FSW, he must approach her mommy. Likewise, FSWs have to report to mommies if they go ‘offstage’ with clients (i.e., leave the bar to offer sexual services). Mommies handle the sexual business as they collect a set amount of the fee, ranging from 10% to one-third of the total negotiated fee received from each client. If FSWs conduct secret deals with clients to go ‘offstage’, the establishment will fail to earn any profit. Mommies’ supervision is critical because entertainment establishments only earn a very small profit from sex workers serving clients ‘onstage’. Some portion of the profits from ‘onstage’ services is also shared with mommies. Some regular clients set a time with their favourites or ‘new faces’ through mommies by paying them extra money. Therefore, almost every service between FSWs and clients is mediated through mommies. To ensure that FSWs follow the rules and do not make clandestine deals with clients, mommies enforce stringent work policies, including mandatory presence during work hours, except when ‘offstage’ and collecting fines otherwise.
Figure 2.
Exploratory network of sex-work environment. Italics in parentheses indicate a potential harmful source and effect by undercover police. Bold arrows indicate the flow of money during sexual service; dashed arrows indicate attributes of HIV risk; bold dashed arrows indicate an enabling factor of mommies for protection; and boxed arrows indicate a potential multilevel intervention in the sex-work environment.
Protective roles of mommies
Mommies’ network position in promoting economic gain appears to work well in protecting FSWs from sex-work harms. Mommies understand that they need to protect FSWs from undercover police, potentially harmful clients and STIs to keep their business profitable. The first role of mommies’ protection is to handle the policing of sex work. Indeed, as owners contend, it is a crucial skill needed from mommies. Since 1989, with the emergence of entertainment establishments, China has maintained a nationwide anti-pornography campaign (saohuangdafei) to ensure state security and control, with the motto of cultural purification and the creation of a spiritual civilisation (jingshenwenming). Under the campaign, sex for money is considered to be an ‘ugly social phenomenon’ of capitalism, which must be wiped out to maintain a healthy socialist system. The sex-work business is declared ‘cultural trash’ that destabilises state rule. Therefore, erotic services (seqingpeishi) in entertainment establishments is against ‘socialist spiritual civilisation’. The Public Security Bureau, known as ‘Iron Great Wall’, performs crackdowns (yanda, literally, ‘to strike severely’) against social deviances. These crackdowns usually last for 3 months at a time or are repeated three times a year, strategically around holidays (e.g., National Day and Army Day) and during international events (e.g., the Olympic Games). Of all crackdown targets, sex-work venues are attacked with the most organisational force. The Bureau employs a complex system of raids. Their techniques were self-described as ‘guerrilla warfare’, in reference to the heroic efforts of Communist revolutionaries against Japanese invaders and nationalists. Raids have several types, including ‘regular raids and shock raids, timed raids and random raids, systematic raids and block raids, daytime raids and night raids’, and undercover inspections. The work performance of the Bureau units is assessed by the number of arrested FSWs and the amount of fines levied; officers who perform well receive high honours and cash bonuses from the municipal government.
Thus, Mommies have to be acutely aware of any sources of information on crackdowns and undercover policing. If mommies serve a client whom they have never seen, they would be very cautious and forbid FSWs from providing them with sexual services in order to protect both their establishment and FSWs. Mommies make it clear that if FSWs dismiss mommies’ warning and insist on going ‘offstage’ with an unfamiliar client, they would have to take full responsibility for potential consequences (e.g., arrest, fines or incarceration). As a result of this warning system, few sex workers are willing to take the risks.
Mommies also make efforts to protect FSWs from potentially violent clients. Using their insights, they screen ‘bad dates’ before allowing FSWs to have sex with them. Potentially violent clients can be found among new clients, those acting impolitely or violently during ‘onstage’ entertainment, or those who are identified by other sex workers as violent. As in the case of checking undercover police, if FSWs insist on having sex with clients who appear to be ‘suspicious’ to mommies, the FSWs have to take responsibility for any harm that arises. Some mommies provide ‘workshops’ to FSWs about how to deal with clients’ violence and harms. As noted earlier, the mommies’ self-support group actively sought resources regarding sexual health. They provided FSWs with informal education about negative consequences from HIV/STIs and reproductive health (e.g., adverse effects of unwanted pregnancy and abortion) and guidance on how to approach health clinics. FSWs were more receptive to the information given by mommies who understood their lifestyle and used their everyday languages.
Our ethnography focused on the protective roles of mommies. Since the roles of mommies are dependent on power dynamics among those involved, whether or not the relationships facilitate risk or protection are far more complex. If FSWs, mommies, or owners pursue their own interests (e.g., higher economic gain), their networks may lead to adverse outcomes in terms of HIV risk. During the ethnography, some FSWs decided not to use a condom in exchange for a higher fee, which often was initiated by clients. Likewise, mommies and clients negotiated sexual services without a condom. Some mommies refused to accept the introduction of health services to their FSWs and our outreach team experienced ‘being blocked’. Further analyses are needed to understand how these constraints transform such risk-enhancing networks.
Discussion
The purposes of this study were (1) to situate the various forms of occupational sex-work harms in regard to HIV vulnerability among FSWs in China by demonstrating how the harms were associated with sexual risk; and (2) to determine the extent to which mommies play a role in protecting FSWs from harms in the risk environments where traumatic events occur repeatedly and cumulatively. The FSWs experienced multiple harms that increased the likelihood of USC, while mommies’ protection moderated the relationship between the two variables. The positive association between longer sex-work involvement and USC suggests that FSWs who work longer may develop maladaptive coping mechanisms for sex work-related stressors as they are exposed to HIV risk behaviours (Although the data are not presented, 79% of drug-using FSWs were involved in sex work for more than 1 year).
The role of mommies was further illustrated by our ethnography showing that mommies are situated as a core linked to all other actors to protect their economic interests as well as their FSWs from harms. In this system, mommies establish norms that endorse particular forms of behaviour, while imposing sanctions on those who did not follow the rules. These interdependent relationships of profit and workers’ safety indicate that these sex-work structures, which have a vested profit interest, can also be used as social capital for HIV-prevention intervention.
We believe that our study may be the first in China to provide empirical evidence about the relationship between sex-work harms, manager’s protection and sexual risk, with a focus on violence against FSWs. Our data suggest that intervention to promote safer sex among FSWs should incorporate violence-reduction strategies and occupational-health promotion, as well as their labour rights more broadly. Creating a violence-free sex-work environment will change the structural foundation of HIV vulnerability beyond the individual level. Such an approach is particularly important in China because many FSWs are migrants or otherwise mobile and face structural obstacles to accessing prevention resources. Strengthening protective mechanisms in the workplace will safeguard these itinerant FSWs against sex-work harms.
Importantly, this study focuses on within-structure aspects of the sex-work environment in China by highlighting occupational harms. The study findings provide evidence that the social capital of mommies’ protective network affects the outcomes of HIV prevention. Whilst the mobilisation of FSWs could be an effective way to reduce HIV risk factors, this seems to be unlikely in China due to the criminalisation of sex work. A viable alternative would be to target mommies in sex-work establishments and find ways to ensure that those who see the value of humane HIV prevention among FSWs can act on that value and those who do not see the value become better informed about occupational rights and safety in public health.
Limitations
This quantitative study was conducted in a low- to middle-income neighbourhood in Beijing, and participants were recruited through venue-based ‘snowball’ sampling. Therefore, the study findings are not representative of all FSWs in China, limiting the generalisability of study findings to other FSW populations. Since the survey was designed as a needs assessment to identify risk factors of HIV/STIs, assessment of sexual behaviours, including characteristics of clients and non-paid steady partners, was limited. The study is also limited in understanding the impact of mobility on occupational protection, especially the aspect of temporal (‘floating’) rural-to-urban migration for sex work during the non-agricultural winter season. Although this study used an occupational model of sex work, the identity aspect of FSWs, such as resiliency from hardships, was not assessed. Whereas our ethnography findings illustrate the enabling protective roles of mommies, the understanding in the structure of mommy’s constraint networks is limited. Social capital can be harmful for certain network members, as a source of conflict, resulting in negative effects on health (Due et al. 1999). Further ethnographic comparative network analyses are needed in terms of contested controllability (e.g., perceived trust), the agency of FSWs, the owners’ involvement in the policy of occupational safety, and tacit approval by the police across different contexts.
Implications
The mommy-centred sex-work structure in our study sheds light on the potential of translating social capital into HIV-prevention interventions for the FSW community in China. Social capital builds on social cohesion and facilitates the development of networks among the members of a community in their pursuit of a common goal. In seeking the mutual advantage, social networks use bonding and bridging to convey influence, and linking to convey new information (Kawachi 2006). In China, peer outreach using social networks has been a key component in HIV prevention among FSWs. However, the scope of peer-led prevention is limited and few empirical data provide evidence of the effectiveness of this approach, especially in terms of its multifaceted structural interventions (Hong and Li 2009).
This may be due to the negligible attention paid to the structural foundation of prevention capacity in the community, which consists of the dynamics of ties (Tucker et al. 2011). Notably, strong bonding networks in disadvantaged communities are likely to promote risk norms if these marginalised communities have limited access to external influences and information (Cattell 2001). As such, FSWs in China might be prone to experiencing adverse outcomes of HIV/STIs and other occupational harms from their bonding ties that often lacks internal and external protection agency. Institutional and sociocultural stigmatisation against sex work prevents FSWs from viewing formal health service systems as representing their interests or needs. This kind of absence of social capital (e.g., social exclusion in healthcare settings) may explain low levels of scaling up access to HIV prevention services for FSWs in China. The success of linking sex-work settings to external health services might be determined by whether a particular network is oriented toward providing institutional support for the safety of sex work; the degree to which the support is tailored to the needs of FSWs; and the extent to which mommies or owners want and allow the services to be accessible. FSWs will adopt healthy practices if they learn new norms and behaviours from people they trust, and, importantly, if they believe that the changes may actually make a difference. If prevention programmes are not seen as ‘trustworthy’ or fail to address FSWs’ unmet needs, they are less likely to be successful in China. Thus, social reinforcement (e.g., policy) should reflect the occupational needs of FSWs.
Peer-led prevention in China also neglects its potential impact on reducing structural barriers at the macro level as interpersonal interventions could increase collective consciousness and activities targeting environmental changes beyond the individual level (Hirsch et al. 2007). Such a lack of attention limits the application of network-based structural interventions. In order to strengthen social cohesion for HIV prevention, aiming for structural intervention in occupational safety and sex workers’ rights for health equality, multiple sources of protection and resilience within sex-work networks should be taken into consideration (Berkman et al. 2000), including recognition of the agency of FSWs as individual social capital (Loff et al. 2003).Not all sex workers see themselves as victims, oppressed or exploited. Instead, many are taking control of their own lives, finding solutions to their problems, acting in their individual and collective interest and contributing to the fight against the HIV epidemic. Indeed, some of the most successful interventions have been led by FSWs, where they organised themselves in partnership with managers to protect their own safety, raising collective awareness of HIV/STI prevention as a primary concern within trusted networks (UNAIDS 2009). Such an approach also frames HIV risk reduction and violence prevention within a broader context of occupational health improvement. Successful interventions among FSWs require the integration of health-care systems of HIV/STI prevention and treatment/care, occupational health and safety and environmental protection networks. The development of theoretical and empirical indicators of various forms of social capital for occupational safety will make significant contributions to current HIV-prevention efforts to reduce structural health risk factors among FSWs in China.
Acknowledgments
The authors thank the participants in this research for their time, staff members and peer outreach volunteers, Fang Xuefei, Wang Hui, Chen Ying and Zhang Zhiqiang, at the Aizhixing Institute of Health who worked to enhance the well-being of underserved populations and the managers of sex-work venues who helped us to conduct the interviews. This research was funded by the United Nations Population Fund (UNFPA). The contents of this study do not necessarily represent the official opinions and views of UNFPA. We especially thank Ms. Kumiko Yoshida and Mr. Jianzhong Chen, AIDS Project Coordinators, UNFPA China office, for providing valuable suggestions as well as monitoring and evaluating this project. The authors also thank Prof. Roger Vaughan at the Mailman School of Public Health, Columbia University, for his advice on data analysis. This research was also supported by a training grant from the National Institute of Mental Health (T32 MH19139, Behavioral Sciences Research in HIV Infection; Principal Investigator: Anke A. Ehrhardt, Ph.D.).
References
- Alexander P. Sex work and health: a question of safety in the workplace. Journal of American Medical Women’s Association. 1998;53:77–82. [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science and Medicine. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Cattell V. Poor people, poor places, and poor health: the mediating role of social networks and social capital. Social Science and Medicine. 2001;52:1501–1516. doi: 10.1016/s0277-9536(00)00259-8. [DOI] [PubMed] [Google Scholar]
- Chen XS, Gong XD, Liang GJ, Zhang GC. Epidemiologic trends of sexually transmitted diseases in China. Sexually Transmitted Diseases. 2000;27:138–142. doi: 10.1097/00007435-200003000-00003. [DOI] [PubMed] [Google Scholar]
- Cheng SSY, Mak WWS. Contextual influences on safer sex negotiation among female sex workers (FSWs) in Hong Kong: the role of non-governmental organizations (NGOs), FSWs’ managers, and clients. AIDS Care. 2010;22:606–613. doi: 10.1080/09540120903311441. [DOI] [PubMed] [Google Scholar]
- Choi SY, Holroyd E. The influence of power, poverty and agency in the negotiation of condom use for female sex workers in mainland China. Culture, Health, and Sexuality. 2007;9:489–503. doi: 10.1080/13691050701220446. [DOI] [PubMed] [Google Scholar]
- Due P, Holstein B, Lund R, Modvig J, Avlund K. Social relations: network, support and relational strain. Social Science and Medicine. 1999;48:661–673. doi: 10.1016/s0277-9536(98)00381-5. [DOI] [PubMed] [Google Scholar]
- Fang X, Li X, Yang H, Hong Y, Zhao R, Dong B, Liu W, Zhou Y, Liang S, Shenton B. Profile of female sex workers in a Chinese county: does it differ by where they came from and where they work? World Health and Population. 2007;9:46–64. doi: 10.12927/whp.2007.18695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gil VE, Wang MS, Anderson AF, Lin GM, Wu ZO. Prostitutes, prostitution and STD/HIV transmission in mainland China. Social Science and Medicine. 1996;42:141–152. doi: 10.1016/0277-9536(95)00064-x. [DOI] [PubMed] [Google Scholar]
- Harcourt C, Donovan B. The many faces of sex work. Sexually Transmitted Infections. 2005;81:201–206. doi: 10.1136/sti.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch GB, Levine R, Miller RL. Using systems dynamics modeling to understand the impact of social change initiatives. American Journal of Community Psychology. 2007;39:239–254. doi: 10.1007/s10464-007-9114-3. [DOI] [PubMed] [Google Scholar]
- Hong Y, Li X. HIV/AIDS behavioral interventions in China: a literature review and recommendation for future research. AIDS and Behavior. 2009;13:603–613. doi: 10.1007/s10461-008-9483-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y, Henderson GE, Pan S, Cohen MS. HIV/AIDS risk among brothel-based female sex workers in China: assessing the terms, content, and knowledge of sex work. Sexually Transmitted Diseases. 2004;31:695–700. doi: 10.1097/01.olq.0000143107.06988.ea. [DOI] [PubMed] [Google Scholar]
- Kawachi I. Social capital and health: making the connections one step at a time. International Journal of Epidemiology. 2006;35:989–993. doi: 10.1093/ije/dyl117. [DOI] [PubMed] [Google Scholar]
- Kerrigan D, Moreno L, Rosario S, Gomez B, Jerez H, Barrington C, Weiss E, Sweat M. Environmental-structural interventions to reduce HIV/STI risk among female sex workers in the Dominican Republic. American Journal of Public Health. 2006;96:120–125. doi: 10.2105/AJPH.2004.042200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loffa B, Overs C, Longoc P. Can health programmes lead to mistreatment of sex workers? Lancet. 2003;361:1982–1983. doi: 10.1016/S0140-6736(03)13595-7. [DOI] [PubMed] [Google Scholar]
- Pirkle C, Soundardjee R, Stella A. Female sex workers in China: vectors of disease? Sexually Transmitted Diseases. 2007;34:695–703. doi: 10.1097/01.olq.0000260989.70866.94. [DOI] [PubMed] [Google Scholar]
- Poundstone KE, Strathdee SA, Celentano DD. The social epidemiology of human immunodeficiency virus/acquired immunodeficiency syndrome. Epidemiologic Review. 2004;26:22–35. doi: 10.1093/epirev/mxh005. [DOI] [PubMed] [Google Scholar]
- Rekart ML. Sex-work harm reduction. Lancet. 2005;366:2123–2134. doi: 10.1016/S0140-6736(05)67732-X. [DOI] [PubMed] [Google Scholar]
- Shannon K, Csete J. Violence, condom negotiation, and HIV/STI risk among sex workers. Journal of the American Medical Association. 2010;304:573–574. doi: 10.1001/jama.2010.1090. [DOI] [PubMed] [Google Scholar]
- Tashakkori A, Teddlie C. Handbook of mixed methods in social & behavioral research. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- Tucker JD, Peng H, Wang K, Chang H, Zhang SM, Yang LG, Yang B. Female sex worker social networks and STI/HIV prevention in south China. PLoS One. 2011;6 (9):e24816. doi: 10.1371/journal.pone.0024816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. UNAIDS guidance note on HIV and sex work. Geneva, Switzerland: UNAIDS; 2009. [Google Scholar]
- Wolffers I, van Beelen N. Public health and the human rights of sex workers. Lancet. 2003;361:1981. doi: 10.1016/S0140-6736(03)13594-5. [DOI] [PubMed] [Google Scholar]
- Yang H, Li X, Stanton B, Fang X, Zhao R, Dong B, Liu W, Liang S, Zhou Y, Hong Y. Condom use among female sex workers in China: role of gatekeepers. Sexually Transmitted Diseases. 2005;32:572–580. doi: 10.1097/01.olq.0000175418.48665.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yi H, Mantell JE, Wu R, Lu Z, Zeng J, Wan Y. A profile of HIV risk factors in the context of sex work environments among migrant female sex workers in Beijing, China. Psychology, Health and Medicine. 2010;15:172–187. doi: 10.1080/13548501003623914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng T. Red lights: the lives of sex workers in post-socialist China. Minneapolis, MN: University of Minnesota Press; 2009. [Google Scholar]