Abstract
Purpose
Femoral tunnel angle (FTA) has been proposed as a metric for evaluating whether ACL reconstruction was performed anatomically. In clinic, radiographic images are typically acquired with an uncertain amount of internal/external knee rotation. The extent to which knee rotation will influence FTA measurement is unclear. Furthermore, differences in FTA measurement between the two common positions (0° and 45° knee flexion) have not been established. The purpose of this study was to investigate the influence of knee rotation on FTA measurement after ACL reconstruction.
Methods
Knee CT data from 16 subjects were segmented to produce 3D bone models. Central axes of tunnels were identified. The 0° and 45° flexion angles were simulated. Knee internal/external rotations were simulated in a range of ±20°. FTA was defined as the angle between the tunnel axis and femoral shaft axis, orthogonally projected into the coronal plane.
Results
Femoral tunnel angle was positively/negatively correlated with knee rotation angle at 0°/45° knee flexion. At 0° knee flexion, FTA for anterio-medial (AM) tunnels was significantly decreased at 20° of external knee rotation. At 45° knee flexion, more than 16° external or 19° internal rotation significantly altered FTA measurements for single-bundle tunnels; smaller rotations (±9° for AM, ±5° for PL) created significant errors in FTA measurements after double-bundle reconstruction.
Conclusion
Femoral tunnel angle measurements were correlated with knee rotation. Relatively small imaging malalignment introduced significant errors with knee flexed 45°. This study supports using the 0° flexion position for knee radiographs to reduce errors in FTA measurement due to knee internal/external rotation.
Level of evidence
Case–control study, Level III.
Keywords: Femoral tunnel angle, Anterior cruciate ligament reconstruction, 3D CT, Tunnel position
Introduction
The concept of anatomic ACL reconstruction has generated significant interest in recent years, with some studies reporting that anatomical ACL reconstruction was superior to non-anatomic ACL reconstruction for restoring normal knee kinematics, improving functional outcomes, and possibly lowering the risk of OA development [11, 18, 23–25]. Recently, a new method for predicting whether the ACL reconstruction was anatomic or non-anatomic was introduced using the femoral tunnel angle (FTA), measured from posterior–anterior (P-A) radiographs [10]. It was considered to be a simple, fast analysis that could be performed using standard clinical images to evaluate tunnel position. However, since the FTA relies upon a two-dimensional measurement, it may be influenced by imperfect limb positioning that commonly occurs when clinical P-A radiographs are obtained [13, 20]. Poor radiographic alignment may result from a variety of factors, including difficulty finding anatomical reference points in excessive surrounding soft tissue and/or knee pain that might limit the patient’s ability to keep the knee in a neutral position. Thus, images are typically acquired with some unknown degree of internal or external knee rotation which will introduce errors in FTA measurement. The flexion angle of the knee can also influence the apparent FTA, particularly when combined with poorly aligned radiographs. Since some clinics use full extension while others prefer 45° flexion positions for post-operative radiographs, it is important to understand the influence of flexion angle on FTA measurements.
The purpose of this study was to determine the effects of knee rotation and flexion angle on the femoral tunnel angle measurement after ACL reconstruction. It was hypothesized that: (1) FTA would be positively correlated with knee rotation angle; (2) within a certain range of knee internal/external rotation, errors in FTA measurement would be acceptable; and (3) FTA measurement would be more reliable with the knee imaged in full extension than when it is imaged in 45° flexion.
Materials and methods
Sixteen ACL-injured subjects were recruited for this study. Subjects underwent either single-bundle (SB) ACL reconstruction (n = 6, 32 ± 9 years old, range 24–46 years; 1 male and 5 female) or double-bundle (DB) ACL reconstruction (n = 10, 39 ± 10 years old, range 23–53 years; 5 male and 5 female). The study was approved by our Institutional Review Board. High-resolution computed tomography (CT) scans with 1-mm-thick slices were obtained and segmented in Mimics software (Materialise, Belgium) to produce 3D models of subjects’ knee joints. Tunnels were manually identified on the bone models by fitting spheres at the opposing ends of the tunnel and forming a representative vector connecting the two points (Fig. 1). The femoral axis was identified by connecting the proximal and distal centres of the femoral shaft. The anatomical axes were derived by placing landmarks on the 3D models following a method similar to Grood and Suntay [6]. The 0° and 45° flexion angles were simulated by rotating the femur about the medial–lateral anatomical axis. Knee internal/external rotation was simulated by rotating the femur about the tibia proximal–distal anatomical axis between ±20° in 1° increments. Femur and tibia models were initially placed in a neutral rotation position with joint translation equivalent to the knee position during the unloaded supine CT scanning. Next, the various permutations of flexion and internal/external rotations were applied about the anatomical axes while the tibia was held in a fixed position. FTA was measured as the angle between the tunnel vector and femoral shaft axis orthogonally projected into the simulated radiographic plane at each internal/external rotational angle and for both 0°–45° of knee flexion (Fig. 2).
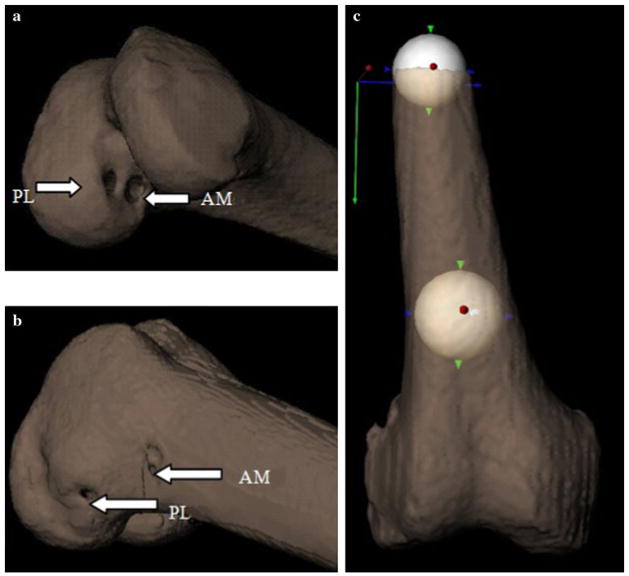
Fig. 1.
Identification of the AM and PL tunnels (a and b) and determination of the femoral shaft axis (c) on the 3D bone models
Fig. 2.
Simulation of the 3D model knee flexion angles of 0° (a) and 45° (b); Knee internal/external rotation at 20° external (c) to 20° internal (d) rotation (0° nee flexion shown). We use the transparent CT bone model technique to estimate the tunnel vector on the bone models. As shown in Fig. 2, FTA (β) of PL tunnel was measured as the angle between the tunnel vector (green line) and femoral shaft axis (grey line) orthogonally projected into the simulated x-ray (a)
Statistical analysis
All statistical analyses were performed in SPSS software, version 16.0 (SPSS, Chicago, IL). The difference of FTA change between the 0° rotation and internal/external rotations was analysed by using an independent sample T test. The Pearson’s correlation coefficient was used to determine the correlation between the FTA and rotational angle of the knee. The level of significance was set a priori at P < 0.05.
Results
Femoral tunnel angle measurements for different positions of the single-bundle (SB) tunnel, antero-medial (AM) tunnel, and posterior–lateral (PL) tunnel are shown in Table 1. At 0° internal/external rotation, the FTA was smaller when measured at 45° flexion than at 0° flexion. FTA was positively correlated with knee rotation angle at 0° flexion (R2 = 0.99 SB, R2 = 0.99 AM, R2 = 0.98 PL) and negatively correlated with knee rotation angle at 45° knee flexion (R2 = −0.99 SB, R2 = −1 AM, R2 = −1 PL) (Table 2). The error of FTA related with malrotation at 45° knee flexion was larger than that of 0° knee flexion. At least 15° error was found between ±20° rotation compared to neutral position. However, smaller error of FTA (<9°) was found at 0° knee flexion (Table 1).
Table 1.
Femoral tunnel angle measurement at different knee rotation angles
| FTA | Rotation at 0° flexion
|
Rotation at 45° flexion
|
||||
|---|---|---|---|---|---|---|
| 20° External | 0° | 20° Internal | 20° External | 0° | 20° Internal | |
| SB tunnel | 29.9 ± 9.1 | 37.9 ± 4.9 | 42.5 ± 3.2 | 49.2 ± 7.4* | 33.1 ± 11.2 | 18.2 ± 10.4* |
| AM tunnel | 27.9 ± 9.5* | 37.4 ± 7.6 | 43.5 ± 5.7 | 4.7 ± 7.1* | 29.1 ± 7.3 | 13.0 ± 7.1* |
| PL tunnel | 48.9 ± 7.1 | 53.4 ± 6.6 | 55.3 ± 6.8 | 64.2 ± 5.4* | 47.1 ± 4.2 | 29.6 ± 3.8* |
The data are presented as average ± SD (degrees)
P value <0.05
Table 2.
Pearson’s Correlations: Femoral tunnel angle and rotation
| FTA | Rotation at 0° flexion
|
Rotation at 45° flexion
|
||||
|---|---|---|---|---|---|---|
| Slope | R2 | P value | Slope | R2 | P value | |
| SB tunnel | 0.32 | 0.99 | < 0.001 | −0.82 | −0.99 | < 0.001 |
| AM tunnel | 0.40 | 0.99 | < 0.001 | −0.81 | −1.00 | < 0.001 |
| PL tunnel | 0.16 | 0.98 | < 0.001 | −0.89 | −1.00 | < 0.001 |
At 0° knee flexion, the FTA increased slightly as knee rotation progressed from external to internal rotation (Table 1). FTA was significantly decreased (P < 0.05) only at 20° or more external rotation for AM tunnels. FTA for the SB and PL tunnels did not change significantly within ±20° of external/internal rotation (Fig. 3).
Fig. 3.

Mean FTA measurement-versus-external/internal knee rotation angle curves of SB tunnel, AM tunnel, PL tunnel at 0° (a) and 45° (b) knee flexion position. FTA was significantly decreased at 20° or more external rotation for AM tunnels (a). Differences from the neutral rotation position reached significance for SB tunnels at more than 16° external or 19° internal rotation; significant differences occurred at smaller rotation angles for the AM (9° external and 9° internal rotation) and PL (5° external and 5° internal rotation) tunnels (b). (* Deviation from zero knee rotation, at which the malrotation became significant. P < 0.05)
At 45° knee flexion, FTA decreased linearly as the knee was positioned from external to internal rotation (Table 1). Differences from the neutral rotation position reached significance for SB tunnels at more than 16° external or 19° internal rotation (P < 0.05). However, significant differences (relative to the neutral position) occurred at smaller rotation angles for the AM (9° external and 9° internal rotation) and PL (5° external and 5° internal rotation) tunnels (all P < 0.05; Fig. 3).
Discussion
The most important finding of this study was that FTA measurement was positively correlated with knee rotation angle and that measurement at the 45° flexion position was less reliable than 0° flexion position. The error in apparent FTA when measured at the 45° flexion position was significant even for small deviations (such as 5°) from the 0° internal/external rotation position.
Many studies have been conducted to determine whether ACL reconstructions were anatomic or non-anatomic [2, 3, 7, 10, 14, 15, 19] when following up with ACL patients. In vivo and in vitro studies showed that anatomical ACL reconstruction was superior to non-anatomical reconstruction [5, 8, 17, 25]. The method of using the FTA with a cut-off angle to determine whether a given reconstruction is anatomic or non-anatomic is an efficient way to make a quick judgement in clinic. With regard to the first hypothesis that FTA correlated with knee rotation angle, the results showed that FTA positively correlated with knee rotation angle at 0° flexion position and negatively correlated with knee rotation angle at 45° knee flexion position. Previous studies have highlighted the effect of knee positioning during radiograph acquisition on measurement accuracy while investigating joint space narrowing [16, 21], lower limb alignment [9], osteoarthritis (OA) grading [4, 12], and while performing ligament reconstructions using surgical guides [1]. In this 3D CT model study, FTA measurement was significantly influenced by malrotation of the knee leading to incorrect results. Using 3D, CT-derived models permit easy identification of tunnels [15]. In a clinical setting using plain radiographs, tunnel identification can be much more difficult. Complicating this issue are tunnel widening, poor bone quality, the confluence of multiple tunnels, and difficulties arising due to femoral condyle or notch geometry [15, 22]. These create challenges in accurately measuring the angle of the femoral tunnel: a 3D construct being reduced to a 2D artefact on a plain radiograph. While assessment of tunnel angle using 3D CT models offers the most reliable identification and measurement of FTA, the lower radiation exposure, cost, and more widespread availability of plain radiograph systems justify this paper’s attempt to find optimal knee positioning using the plain film radiographic methods.
The second goal of this study was to find the range of knee internal/external rotation in which the FTA measurement would be acceptably accurate. The results showed that the FTA-versus-rotation angle curves were positively correlated, and this error will be significant even if the malrotation angle was small (such as 5°). It would be interesting to know whether FTA measured during malrotation will skew the results into a different classification (anatomic/non-anatomic) based on previous studies. Thus, is there a significant chance to misclassify the anatomic into non-anatomic or the non-anatomic into anatomic category only because of this malrotation? To answer this question, we simulated 45° knee flexion to measure FTA. FTA of all the 3 anatomic cases in SB group was above the cut-off angle of 32.7° [10], and FTA of all the 3 non-anatomic cases was below this angle. This indicated the cut-off angle has high sensitivity and specificity when assessed at zero internal/external rotation. With 11° internal rotation, two subjects with anatomic FTA fell below the cut-off angle. It may be misleading to classify those two cases as non-anatomic; therefore, FTA measured under 11° internal rotation will mislead 66 % (2 of 3) of the results. However, with 5° external rotation, FTA of two non-anatomic cases increased above 32.7°. This may lead to misclassification of two out of three non-anatomic cases as anatomic. So, controlling malrotation will be critical when applying this measurement after ACL reconstruction.
Reducing sources of joint positioning error to obtain more reliable FTA measurements is important for the evaluation of the precision and accuracy of ACL reconstruction graft placement. In this study, we compared FTA measurement between the two common positions used for P-A radiograph views (0° knee flexion and 45° knee flexion). We found that the FTA measurement at 45° flexion position was more easily influenced by knee rotation compared with 0° flexion position (Fig. 3). This study therefore supports using the 0° flexion position when measuring the FTA.
There are some limitations of this study. Firstly, the relatively small sample is a limitation; however, in this small group of patients we found significant differences and can provide a very general overview of this problem. Future studies will include a larger sample size to confirm the influence of knee internal/external rotation and flexion angle on FTA measurement. Secondly, the error of FTA found during malrotation will be related to the tunnel placement in those cases. Different tunnel placements may have different ranges of error between ±20° malrotation. A robust rotation error threshold was not defined using these data as the small samples are representative of the surgeries performed at a single institution and a limited number of surgeons.
This paper quantified the susceptibility of FTA measurement to error due to malrotation, an issue not previously described or acknowledged in the literature. While this paper does not offer specific solutions for the internal–external rotation error, we highlight the discrepancies in FTA measurement between 0° and 45° degrees of flexion; two knee positions most commonly used in a clinical setting. The ability of clinicians to easily make judgements from plain radiographs is very useful in clinical practices. These data suggest more careful, or even standardization of, positioning of the knee during plain radiograph acquisition in order to obtain the most accurate FTA measurements. Additionally, direct comparisons of data sets originating at different clinical institutions should be conducted with an understanding of the effect of differing knee positions on angle measurements.
Conclusion
This study has highlighted two significant problems in the evaluation and classification of ACL reconstructions as anatomic or non-anatomic when using plain radiographs: (1) In the clinic, a true P-A radiograph is difficult to obtain reliably. So reducing the amount of internal/external rotation is important. Malrotation will significantly influence the FTA measurement error, even if the malrotation angle was small; (2) using 0° flexion position to measure FTA will be more reliable than 45° flexion position.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Jing Tang, Department of Orthopedic Surgery, University of Pittsburgh, Kaufman Building Suite 1011, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA. Department of Orthopedic Surgery, Beijing Jishuitan Hospital, Fourth Clinical College of Peking University, 31 Xinjiekou Dongjie St., Beijing 100035, China.
Eric Thorhauer, Department of Orthopedic Surgery, University of Pittsburgh, Kaufman Building Suite 1011, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA.
Chelsea Marsh, Department of Orthopedic Surgery, University of Pittsburgh, Kaufman Building Suite 1011, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA.
Freddie H. Fu, Department of Orthopedic Surgery, University of Pittsburgh, Kaufman Building Suite 1011, 3471 Fifth Avenue, Pittsburgh, PA 15213, USA
Scott Tashman, Email: tashman@pitt.edu, Orthopedic Research Laboratories, University of Pittsburgh, 3820 South Water St., Pittsburgh, PA 15203, USA.
References
- 1.Celentano U, Cardoso MP, Martins CA, Ramirez CP, van Eck CF, Smolinski P, Fu FH. Use of transtibial aimer via the accessory anteromedial portal to identify the center of the ACL footprint. Knee Surg Sports Traumatol Arthrosc. 2012;20:69–74. doi: 10.1007/s00167-011-1574-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Forsythe B, Kopf S, Wong AK, Martins CA, Anderst W, Tashman S, Fu FH. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J Bone Joint Surg Am. 2010;92:1418–1426. doi: 10.2106/JBJS.I.00654. [DOI] [PubMed] [Google Scholar]
- 3.Gelber PE, Erquicia J, Abat F, Torres R, Pelfort X, Rodriguez-Baeza A, Alomar X, Monllau JC. Effectiveness of a footprint guide to establish an anatomic femoral tunnel in anterior cruciate ligament reconstruction: computed tomography evaluation in a cadaveric model. Arthroscopy. 2011;27:817–824. doi: 10.1016/j.arthro.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Gensburger D, Roux JP, Arlot M, Sornay-Rendu E, Ravaud P, Chapurlat R. Influence of blinding sequence of radiographs on the reproducibility and sensitivity to change of joint space width measurement in knee osteoarthritis. Arthr Care Res. 2010;62:1699–1705. doi: 10.1002/acr.20311. [DOI] [PubMed] [Google Scholar]
- 5.Giron F, Cuomo P, Edwards A, Bull AM, Amis AA, Aglietti P. Double-bundle “anatomic” anterior cruciate ligament reconstruction: a cadaveric study of tunnel positioning with a transtibial technique. Arthroscopy. 2007;23:7–13. doi: 10.1016/j.arthro.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 7.Hoser C, Tecklenburg K, Kuenzel KH, Fink C. Postoperative evaluation of femoral tunnel position in ACL reconstruction: plain radiography versus computed tomography. Knee Surg Sports Traumatol Arthrosc. 2005;13:256–262. doi: 10.1007/s00167-004-0548-y. [DOI] [PubMed] [Google Scholar]
- 8.Hosseini A, Lodhia P, Van de Velde SK, Asnis PD, Zarins B, Gill TJ, Li G. Tunnel position and graft orientation in failed anterior cruciate ligament reconstruction: a clinical and imaging analysis. Int Orthop. 2012;36:845–852. doi: 10.1007/s00264-011-1333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunt MA, Fowler PJ, Birmingham TB, Jenkyn TR, Giffin JR. Foot rotational effects on radiographic measures of lower limb alignment. Can J Surg. 2006;49:401–406. [PMC free article] [PubMed] [Google Scholar]
- 10.Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am J Sports Med. 2011;39:2611–2618. doi: 10.1177/0363546511420128. [DOI] [PubMed] [Google Scholar]
- 11.Jarvela T. Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc. 2007;15:500–507. doi: 10.1007/s00167-006-0254-z. [DOI] [PubMed] [Google Scholar]
- 12.Kinds MB, Vincken KL, Hoppinga TN, Bleys RL, Viergever MA, Marijnissen AC, Welsing PM, Lafeber FP. Influence of variation in semiflexed knee positioning during image acquisition on separate quantitative radiographic parameters of osteoarthritis, measured by knee images digital analysis. Osteoarthr Cartil. 2012;20:997–1003. doi: 10.1016/j.joca.2012.04.016. [DOI] [PubMed] [Google Scholar]
- 13.Krackow KA, Pepe CL, Galloway EJ. A mathematical analysis of the effect of flexion and rotation on apparent varus/valgus alignment at the knee. Orthopedics. 1990;13:861–868. doi: 10.3928/0147-7447-19900801-09. [DOI] [PubMed] [Google Scholar]
- 14.Lertwanich P, Martins CA, Asai S, Ingham SJ, Smolinski P, Fu FH. Anterior cruciate ligament tunnel position measurement reliability on 3-dimensional reconstructed computed tomography. Arthroscopy. 2011;27:391–398. doi: 10.1016/j.arthro.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 15.Magnussen RA, Debieux P, Benjamin B, Lustig S, Demey G, Servien E, Neyret P. A CT-based classification of prior ACL femoral tunnel location for planning revision ACL surgery. Knee Surg Sports Traumatol Arthrosc. 2012;20:1298–1306. doi: 10.1007/s00167-011-1814-4. [DOI] [PubMed] [Google Scholar]
- 16.Mazzuca SA, Brandt KD, Dieppe PA, Doherty M, Katz BP, Lane KA. Effect of alignment of the medial tibial plateau and x-ray beam on apparent progression of osteoarthritis in the standing anteroposterior knee radiograph. Arthr Rheum. 2001;44:1786–1794. doi: 10.1002/1529-0131(200108)44:8<1786::AID-ART315>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 17.Misonoo G, Kanamori A, Ida H, Miyakawa S, Ochiai N. Evaluation of tibial rotational stability of single-bundle vs. anatomical double-bundle anterior cruciate ligament reconstruction during a high-demand activity—a quasi-randomized trial. Knee. 2012;19:87–93. doi: 10.1016/j.knee.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med. 2010;38:2201–2210. doi: 10.1177/0363546510373876. [DOI] [PubMed] [Google Scholar]
- 19.Siebold R. The concept of complete footprint restoration with guidelines for single- and double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:699–706. doi: 10.1007/s00167-010-1376-x. [DOI] [PubMed] [Google Scholar]
- 20.Swanson KE, Stocks GW, Warren PD, Hazel MR, Janssen HF. Does axial limb rotation affect the alignment measurements in deformed limbs? Clin Orthop Relat Res. 2000;371:246–252. doi: 10.1097/00003086-200002000-00029. [DOI] [PubMed] [Google Scholar]
- 21.Vignon E, Brandt KD, Mercier C, Hochberg M, Hunter D, Mazzuca S, Powell K, Wyman B, Le Graverand MP. Alignment of the medial tibial plateau affects the rate of joint space narrowing in the osteoarthritic knee. Osteoarthr Cartil. 2010;18:1436–1440. doi: 10.1016/j.joca.2010.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang JH, Kim JG, Ahn JH, Lim HC, Hoshino Y, Fu FH. Is femoral tunnel length correlated with the intercondylar notch and femoral condyle geometry after double-bundle anterior cruciate ligament reconstruction using the transportal technique? An in vivo computed tomography analysis. Arthroscopy. 2012;28:1094–1103. doi: 10.1016/j.arthro.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 23.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 24.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 25.Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006;22:240–251. doi: 10.1016/j.arthro.2005.12.017. [DOI] [PubMed] [Google Scholar]