Abstract
Background:
Previous work reports an association between familial risk factors stemming from parental characteristics and offspring disruptive behavior disorders (DBDs). This association may reflect a) the direct effects of familial environment, and b) a passive gene-environment correlation, wherein the parents provide both the genes and the environment. The current study examined the contributions of direct environmental influences and passive gene-environment correlations by comparing the effects of familial risk factors on child DBDs in genetically related (biological) and non-related (adoptive) families.
Method:
Participants were 402 adoptive and 204 biological families. Familial environment was defined as maternal and paternal maladaptive parenting and antisociality, marital conflict, and divorce; offspring DBDs included attention deficit/hyperactivity disorder, conduct disorder, and oppositional defiant disorder. Mixed-level regressions estimated the main effects of familial environment, adoption status, and the familial environment by adoption status interaction term, which tested for a presence of passive gene-environment correlations.
Results:
There was a main effect of maternal and paternal maladaptive parenting and marital discord on child DBDs, indicating a direct environmental effect. There was no direct environmental effect of maternal or paternal antisociality, but maternal and paternal antisociality had stronger associations with child DBDs in biological families than adoptive families, indicating the presence of a passive gene-environment correlation.
Conclusions:
Many familial risk factors affected children equally across genetically-related and non-related families, providing evidence for direct environmental effects. The relationship of parental antisociality and offspring DBDs was best explained by a passive gene-environment correlation, where a general vulnerability toward externalizing psychopathology is passed down by the parents to the children.
Current research has established a number of robust predictors of child disruptive behavior disorder (DBD) symptoms. These include maladaptive, inconsistent, harsh, punitive, or abusive parenting; marital conflict among parents; divorce; and parental antisocial behavior. Across both clinical and community samples, maladaptive parental disciplinary practices are linked with offspring attention-deficit hyperactivity disorder (ADHD), oppositional-defiant disorder (ODD) , and conduct disorder (CD) symptoms (Loeber & Stouthamer-Loeber, 1986; Burt et al. 2003; Caspi et al. 2004; Stormshak et al. 2000; Stanger et al. 2004). Similarly, divorce and marital discord are significantly related to DBD symptoms (Gartstein & Fagot, 2003; Burt et al. 2008). Finally, one of the strongest predictors of child conduct problems is parental antisocial behavior (Herndon & Iacono, 2005), as it is consistently associated with offspring DBD symptoms, delinquency, and criminal acts.
Arguably, these studies put forth familial factors as environmental risk factors contributing directly to child DBD symptoms. Indeed, a recent meta-analysis of twin studies reported that shared environmental factors (i.e., factors common to both members of a sibling pair that make them similar) accounted for 10%–15% of the variance in child DBD symptoms and diagnoses (Burt, 2009). Other studies indicate familial risk factors are associated with child DBD symptoms in large part through shared environmental mechanisms (McGue et al. 1996; Pike et al. 1996; Burt et al. 2003; Burt et al. 2007;). However, additional research on the link between familial risk factors and child DBD symptoms suggests alternative explanations which implicate genetic influences. One key finding largely supporting this is that parental antisociality is highly heritable. In a review of studies on the etiology of child antisociality, Rhee and Waldman (2002) found genes influenced 32% of the variance in child antisociality, and shared environmental factors influenced 16%. Previous studies (Bornovalova. 2010) indicate parental externalizing psychopathology (including adult antisociality) influences child DBD symptoms through transmitting a common genetic vulnerability. Likewise, multiple studies report genetic influences on marital relationships (Reiss et al. 2000; Spotts et al. 2004; Spotts et al. 2006), divorce (McGue & Lykken, 1992), and maladaptive parenting (Jaffee & Price, 2008; see Kendler & Baker, 2007 for a review). Collectively, this research suggests patterns of influence generally attributed to the familial environment are in part genetically mediated. Putative environmental factors may be indirectly related to offspring DBD symptoms through the mechanism of passive gene-environment correlation (rGE).
Passive rGE occurs when parents provide both the genes and environment that lead to a certain child outcome. As applied to the current topic, a heritable propensity toward impulsive and disinhibitory behavior may increase likelihood of exhibiting high antisocial traits, especially while being reared in an environment characterized by marital conflict, divorce, and maladaptive parenting. The combination of genetic and environmental risk in turn increases likely manifestation of child DBD symptoms in the offspring (Bornovalova, 2010; Silberg et al. 2012). Unfortunately, neither studies of biological families nor typical twin designs are able to disentangle environmental sources of influence from passive rGE because parents provide both genes and environment for their biological children. And, in classic twin designs, passive rGE can mimic shared environmental influences when the origins are, in fact, a function of common parent– child genes.
An elegant method of disentangling environmental influences from passive rGE involves comparing the effects of putative environmental variables in genetically unrelated families (adoptive families) and genetically related families (biological families). The logic of this design is as follows: In families where the biological parents are rearing their own offspring, parents provide both the child’s environment and his/her genes. Thus, any association between parenting and child DBD symptoms could be due to genetically mediated influences, purely environmental influences, or any combination of the two. In contrast, in an adoptive family, the child’s adoptive parents provide the environment, but the child’s birth parents provide his/her genetic makeup and typically do not provide environmental influences after the child was adopted. As such, the possibility of passive rGE is eliminated (provided children are not selectively placed into adoptive homes). If the magnitude of association between familial factors and child DBD symptoms is significantly greater in biological families than in adoptive families, then some degree of passive rGE is indicated because the association between family environment and biological offspring outcomes depends on both genetic and shared environmental factors. Conversely, if the magnitude of the familial factors-child DBD symptoms association is comparable in biological and adoptive families, then passive rGE effects are ruled out and environmental risk processes are implicated (Plomin, 1994).
Six previous studies (Dunn et al. 1985; Dunn & Plomin, 1986; Dunn et al. 1986; Rende et al. 1992; Braungartrieker et al. 1995; O'Connor et al. 2000) used this design to examine contribution of passive rGE in the association between familial risk factors and DBD symptoms. Findings generally indicated, with the exception of divorce (which consistently shows solely a direct environmental effect), a mix of direct environmental effects and passive rGE effects. Using a very different method (the Extended Children of Twins Design, a design incorporating children of twins and their cousins capitalizing on a large range of genetic relatedness in immediate and extended family), at least four other studies (Neiderhiser et al. 2004; Harden et al. 2007; Neiderhiser et al. 2007; Narusyte et al. 2011; Silberg et al. 2012) found similar effects. Collectively, these studies suggest both passive rGE and direct environmental effects account for the relationship between family conflict, parenting behavior, and parental antisociality and child DBD symptoms. Although these studies contribute importantly to understanding the relative influence of environmental effects and rGE, each examined one or two selected contextual risk factors making it difficult to evaluate the relative contribution of each. Moreover, previous work suggests the importance of examining maternal and paternal parenting factors separately (Rothbaum & Weisz, 1994; Denham et al. 2000; Johnson et al. 2001) but only a few studies (Neiderhiser et al. 2004; Neiderhiser et al. 2007) have investigated possible differences between fathering and mothering in the interplay between genetic and environmental factors. This last point is quite important, as the effects of maternal versus paternal parenting effects may differ in (a) strength of effect, and (b) underlying mechanism of transmission (Rothbaum & Weisz, 1994; Denham et al. 2000; Johnson et al. 2001; Neiderhiser et al. 2004; Neiderhiser et al. 2007). Additionally, among these studies there is large variability in offspring age (ranging from toddlers to adolescents). It is important to extend these studies by examining the effects of multiple familial risk factors on child DBD symptoms late enough in development to allow manifestation of such symptoms. Finally, it is especially worthwhile to attempt to replicate and extend findings from multiple studies using widely different methods (e.g., adoptive designs; Extended Children of Twins Designs), since confidence in the veracity of an effect increases if the same results are found using multiple methodological approaches.
Current Study
We aimed to examine relative contribution of passive rGE and direct environmental effects in the relationship between multiple familial risk factors and child DBD symptoms using a large sample of families with biological or adoptive offspring recruited from the community. We selected maladaptive parenting behavior; familial discord; divorce; and parental antisociality as our key familial predictors as all are related to offspring DBD symptoms and all have substantial heritability (Kendler & Baker, 2007); thus, the effect of each selected familial risk factor on offspring DBD symptoms had the potential to be genetically mediated. In extending previous findings, we used several methodological advancements: (a) including both parents in our analyses and examining relative contributions to DBD symptoms; (b) using multi-reporter indices of child DBDs (ruling out the potential confounding of reporter type); and (c) including multiple indices of maladaptive environment and parenting. Our hypotheses were as follows:
If purely environmental effects are influencing child DBD symptoms, then effects of maladaptive parenting, parental discord, and parental antisociality should occur equally in both adoptive and biological adolescents.
If passive rGE played a role in the relationship between familial risk factors and adolescent DBD symptoms, then effects of familial factors would be stronger in biological children than adoptive children, and the effect would fail to reach significance in the adoptive offspring.
If a combination of direct environmental and passive rGE effects occurred, then effects of familial factors would be stronger in biological children than adoptive children; however, the effect of familial factors in adoptees would still reach significance.
Previous work indicates DBD symptoms load on a common “externalizing” factor that subsumes all shared environmental effects (with no disorder-specific shared environmental effects) (Burt et al. 2003). As the current study focused on variables which broadly fall under the rubric of “shared environment”, we tentatively expected the same pattern of results across all categories of DBD symptoms.
Method
Participants
The current study sample included 402 adoptive and 204 biological families participating in the Sibling Interaction Study (SIBS) at the University of Minnesota. Each family included two children between the ages of 11 and 21 years that were no more than five years apart in age. In the adoptive families, siblings were biologically unrelated, although one sibling could be biological offspring of the adoptive parents. Previous work found “mixed” adoptive families do not differ in SES, adult antisocial behavior, externalizing psychopathology, and depression (McGue et al. 2007). All adoptees were placed permanently in their adoptive home prior to age two; no information is available on their birth parents. In the biological families, the siblings were fully biological and selected to have a distribution of sex and age, but not other characteristics (e.g., income or ethnicity) comparable to those in adoptive families. Participation rates did not differ significantly between adoptive (63.2%) and biological families (57.3%) invited to participate. See McGue, Keyes et al. (2007) for a complete description of the SIBS sample. Mean age was 14.9 (SD=1.9); approximately half (45%) were male; 55.9% of the adolescents were Caucasian, 39% Asian, and 5.1% “other.”
Measures
Parenting Behaviors/Attitudes
Problematic parenting was assessed via questions regarding the parent’s opinions toward physical punishment. The Parental Environment Questionnaire (PEQ) (Elkins et al. 1997) is a 50-item self-report instrument measuring negative interactions between parent and child, and the parent’s belief that he/she has knowledge to benefit the child. Parents respond to each item using a four-point scale yielding the subscales of Conflict, (lack of) Involvement, and (lack of) Parent Regard (αs ranged from .78-.87). Finally, parent’s opinions on favoring punishment were assessed from nine items on a child rearing questionnaire (α=.75) tapping favoring of and willingness to use physical punishment. Higher scores indicated higher levels of maladaptive parenting behavior.
Marital Discord
Marital discord was assessed via questions regarding marital status quality. First, parental separation/divorce status was reported by mothers. In our sample, 90.4% of the mothers were currently married and 7.9% were divorced/separated from the biological father; the remaining 1.7% either never married or widowed and were excluded from the “marital status” analyses. Next, we measured marital quality in couples where spouses were both the child’s biological parents via the Marital Relationship Scale (MRS). The MRS is a slightly modified version of the Dyadic Adjustment Scale (Spanier, 1976) with two items added regarding degree of agreement on child rearing issues. The questionnaire included 34 items querying the respondent on topics such as marital consensus, marital satisfaction, affective expression, and marital cohesion (α=.93). Each parent rated the relationship separately and their scores were averaged together to form a single estimate for each couple. The MRS score correlated (r=.66, p < .001) between parent reports. Higher MRS scores equaled higher marital discord.
Parental Antisocial Behavior (AAB)
Each parent underwent a structured in-person diagnostic interview and was assessed for DSM-IV Adult Antisocial Behavior (AAB; i.e., “adult” symptoms of Antisocial Personality Disorder that occur after age 15). The interview included a modified version of the Structured Clinical Interview for DSM-III-R (Spitzer et al. 1987) that was updated to include DSM-IV diagnostic criteria. Two levels of diagnostic certainty were used: definite (all adult diagnostic criteria satisfied) and probable (one symptom short of a definite diagnosis). To allow for inclusion of affected individuals who may underreport symptoms due to reliance on fallible memory, participants were classified as having AAB if they met probable or definite diagnosis. Additional precedent for our approach derives from reports that individuals with mild forms of psychopathology who fail to meet DSM criteria for a definite diagnosis are nonetheless significantly impaired (Pickles et al. 2001; Kessler et al. 2003). The definite cutoff only provides an extreme estimate that tends to underestimate and is often lower than expected (Elkins et al. 2006; King et al. 2009). Using this classification, 8.6% of mothers were classified as having AAB, as were 32.8% of fathers.
Child Measures
A revised version of the Diagnostic Interview for Children and Adolescents DICA-R (Welner et al. 1987) with additional probes and questions added to assess DSM-IV disorders was used. Mother and offspring reports were combined using a best-estimate procedure such that if either the mother or the adolescent endorsed a symptom, it was considered present. Symptom count variables were used to index ADHD, ODD, and CD. In our sample, there was a mean of .66 (SD=1.25) CD symptoms, 1.40 (SD=1.85) ODD symptoms, and 3.04 (SD=3.84) ADHD symptoms. Because these three disorders are reported to reflect an underlying externalizing (EXT) dimension (Bornovalova, 2010), and all DBD symptom categories in the current sample yielded one principal component (all loadings > .78), an EXT variable was created by taking the first principal component derived from CD, ODD, and ADHD symptoms. EXT was scaled as a standardized variable [Mean (SD)=0.00 (1.00), with a range of −1 to 5, with higher values indicating higher levels of EXT]. Rates of offspring who met DSM-IV DBD diagnoses at the probable or definite level are reported in Table 1.
Table 1.
Demographic characteristics and child psychopathology levels in adoptive and biological families
|
Adoptive
M (SD)/% |
Biological
M (SD)/% |
ANOVA/ X2 value | |
|---|---|---|---|
| Mothers | |||
| Age | 47.92(3.59) | 44.07(4.03) | 284.87*** |
| % Caucasian | 98.8% | 97.1% | 4.35* |
| % College graduate | 63.8% | 54.4% | 10.07** |
| Fathers | |||
| Age | 49.38(3.65) | 46.0(4.9) | 163.31*** |
| % Caucasian | 97.7% | 96.1% | .50 |
| % College graduate | 70.0% | 59.8% | 12.65*** |
| Adolescents | |||
| Age | 14.86(2.01) | 15.06(1.76) | 2.71 |
| % male | 43.4% | 48.3% | 2.62 |
| % Caucasian | 34% | 99% | 447.28*** |
| Symptom Count | |||
| CD symptom count | 0.67(1.24) | .65(1.26) | .05 |
| ODD symptom count | 1.55(1.93) | 1.12(1.64) | 14.73*** |
| ADHD symptom count | 3.35(4.04) | 2.43(3.325) | 15.64*** |
| EXT composite | .07(1.03) | −.13(.916) | 11.07*** |
| Diagnostic Rates [N(%)] | |||
| CD | 81 (11.8%) | 51 (9.7%) | 1.36 |
| ODD | 190 (27.7%) | 81 (15.4%) | 25.91*** |
| ADHD | 126 (18.4%) | 62 (11.8%) | 9.82** |
Note. AAB = adult antisocial behavior; CD = conduct disorder; ODD = oppositional defiant disorder; ADHD = attention deficit hyperactivity disorder; EXT = externalizing composite score (first principal component of CD, ODD, and ADHD symptoms);
p<.05,
p<.01,
p< .001
Results
Differences between Biological and Adoptive Families
Table 1 presents demographic characteristics and child psychopathology levels across adoptive and biological families. In the adoptive families (compared to biological families), mothers and fathers on average were older and had completed more education, mothers were slightly more likely to be Caucasian, and children were less likely to be Caucasian as well as evidenced more symptoms of ODD, ADHD (but not CD), and general EXT. The rates of DBD diagnoses are also presented in Table 1 and are consistent with previously reported rates in biological and adoptive offspring (Keyes et al. 2008).
Table 2 presents the T-scored values of parenting variables, marital discord, percentages of divorce, and parental antisociality in adoptive and biological families. Adoptive mothers reported slightly (but significantly) less involvement and parental regard than biological mothers. However, both mothers and fathers in biological families reported favoring physical punishment more than did parents in the adoptive families. Likewise, parents from biological families were more likely to divorce than parents in adoptive families, and fathers in biological families had higher rates of AAB than fathers in adoptive families. Correlations across maternal and paternal parenting behaviors, among measures of marital discord, and between maternal and paternal AAB are reported in Table 3.
Table 2.
Parenting variables, dyadic adjustment, divorce, and parental antisociality in adoptive and biological families
| Parenting Variables | Adoptive M (SD)/% |
Biological M (SD) /% |
ANOVA/ X2 value |
|---|---|---|---|
| Parenting | |||
| Mother | |||
| Conflict | 50.11(8.41) | 49.78(12.50) | .29 |
| Lack of Involvement | 50.69(7.98) | 48.68(12.94) | 10.49*** |
| Lack of Parent Regard | 50.80(6.71) | 48.47(14.22) | 14.24*** |
| Favors Punishment | 48.54(9.24) | 52.87(10.80) | 51.72*** |
| Father | |||
| Conflict | 50.40(9.79) | 49.159(1.39) | 3.56 |
| Lack of Involvement | 50.05(9.33) | 49.89(11.30) | .06 |
| Lack of Parent Regard | 50.23(9.96) | 49.52(10.08) | 1.14 |
| Favors Punishment | 48.39(9.53) | 53.49(1.106) | 62.94*** |
| Marital Variables | |||
| Marital Discord 1 | 50.39(9.61) | 49.41(10.09) | 2.11 |
| Divorce | 6.6% | 10.9% | 6.58** |
| Parental Antisociality | |||
| Mom AAB | 7.9% | 9.9% | 1.29 |
| Dad AAB | 29.7% | 39.5% | 10.27** |
Note. Scores on each measure (except for divorce) were transformed into T scores with a mean of 50 and standard deviation of 10.
Marital discord examined in married couples only.
* p<.05,
p<.01,
p< .001
Table 3.
Correlations of parenting variables, parental antisociality and divorce.
| MC | MI | MR | MP | FC | FI | FR | FP | MAAB | FAAB | DIV | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mother | |||||||||||
| Conflict | -- | −.30* | −.43* | .15* | .20* | .08 | .05 | .09* | .09 | .02 | .01 |
| Lack of Involvement | -- | .79* | .07 | .16* | .13* | .05 | .05 | −.04 | −.05 | −.06 | |
| Lack of Regard | -- | −.02 | .09* | .06 | .03 | .01 | −.07 | −.00 | −.04 | ||
| Favors Punishment | -- | .04 | .01 | −.01 | .49* | .01 | .01 | −.02 | |||
|
| |||||||||||
| Father | |||||||||||
| Conflict | -- | −.33* | −.51* | .12* | −.00 | −.01 | −.03 | ||||
| Lack of Involvement | -- | .76* | .10* | −.05 | .03 | .09* | |||||
| Lack of Regard | -- | .01 | −.03 | .04 | .05 | ||||||
| Favors Punishment | -- | −.07 | .06 | −.02 | |||||||
|
| |||||||||||
| Parental Antisociality | |||||||||||
| Mother AAB | -- | .19* | .01 | ||||||||
| Father AAB | -- | .14* | |||||||||
| Marital Variables | |||||||||||
| Divorce | . | -- | |||||||||
Note. MC = mother parent-child conflict; MI = mother lack of involvement; MR = mother lack of regard; MP = mother preference for physical punishment; FC = father parent-child conflict; FI = father lack of involvement; FR = father lack of regard; FP = father preference for physical punishment; MAAB = mother adult antisocial behavior; FAAB = father adult antisocial behavior; DIV = divorce,
p<.01.
Parenting Behaviors, Adoptive Status, and Child DBDs
Main Effects of Parenting Behaviors and Adoptive Status
A series of log-linear Poisson mixed-level regression models estimated via generalized estimating equations (a) assessed the relationship between child DBD symptoms and parental measures and (b) tested if adoption status moderated strength of the association. Poisson regressions were used because of the non-normal (Poisson) distribution of the child symptom counts. For each family risk factor, we fit two regression models. These models also accounted for multiple observations (e.g., two children) clustered within a higher-order family unit (Hanley et al. 2003). This technique controls for the correlation between two children within a family as members of a family are likely to be correlated at higher than chance rates. In all analyses, we adjusted for maternal and paternal age, education, child ethnicity, and child adoptive status. Additionally, as symptoms of CD, ODD, and ADHD differed by sex [Fs(1)=66.08, 7.29, 75.69, 63.90 for CD, ODD, ADHD, and EXT, respectively; all ps< .001] and (except for ADHD) showed a significant association with age (rs=.13, .19, .15 for CD, ODD, and EXT, respectively; all ps< .01), sex and age were used as covariates1. Given previous studies indicating maternal and paternal parenting styles exert independent effects on child psychopathology (Bornovalova et al. 2012), we controlled for co-parent parenting style as well. Due to multiple tests, significance cut-off was set at .01 for all regression analyses.
In the first model (termed Main Effects), we examined effects of the mother’s (or father’s) parenting, discord/divorce, or parental AAB on child DBD symptoms while adjusting for all covariates. A significant main effect of family risk factors on child DBD symptoms is evidence for a direct environmental effect. The effect of adoptive (v. biological) status of the child was also included in this model, which controlled for differences between biological and adoptive offspring DBD symptom levels. In the second model (termed Interaction model) we added an interaction term to the main effects regression model to test the interaction between adoptive status and each familial risk factor after controlling for the main effects identified above. A significant interaction term was taken as evidence for a stronger relationship between the familial risk factor and child DBD symptoms in one type of offspring (biological) than the other (adoptive). As such, the interaction term was our test of passive rGE.
As seen in Table 4, there were robust main effects of maternal and paternal parent-child conflict and maternal (but not paternal) willingness to use punishment on child CD, ODD, ADHD, and EXT symptoms. Thus, as maternal and paternal conflict and maternal willingness to use punishment increased, so did child DBD symptoms in adoptive and biological children. Because it was possible that effects in the biological families drove the main effects of familial risk factors (incorrectly interpreted as an environmental effect) we repeated all the analyses separately for adoptive families. Results indicated that, out of the 12 original main effects, 11 were significant in adoptive families. The only effect that failed to reach significance was paternal conflict on offspring ADHD symptoms, but the effect was roughly equal in biological and adoptive offspring [B(SE) = .37 (.21), ns; .26 (.15), ns for adoptive and biological offspring, respectively]. Thus, we concluded the main effects were not being driven by a single family group.
Table 4.
Relationship between parenting variables and child DBDs in adoptive and non-adoptive families.
| Risk Factors: | CD | ODD | ADHD | EXT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Main effects | Interaction | Main effects | Interaction | Main effects | Interaction | Main effects | Interaction | |||||
|
| ||||||||||||
| Risk | A/B | Risk X | Risk | A/B | Risk X | Risk | A/B | Risk X | Risk | A/B | Risk X | |
| Factor | A/B | Factor | A/B | Factor | A/B | Factor | A/B | |||||
| Mother | ||||||||||||
|
| ||||||||||||
| Conflict | .25 | −3.68 | .05 | .27 | −4.77 | −.03 | .21 | −5.26 | −.03 | .40 | −3.39 | −.04 |
| (.04)* | (1.60) | (.07) | (.04)* | (1.25)* | (.08) | (.04)* | (1.05)* | (.07) | (.07)* | (1.04)* | (.13) | |
| Lack of | .28 | −3.32 | −.67 | .31 | −4.71 | −.12 | .14 | −5.33 | .04 | .16 | −4.28 | −.19 |
| Involvement | (.26) | (1.64) | (.18)* | (.16) | (1.28)* | (.32) | (.09) | (1.09)* | (.02) | (.09) | (1.12)* | (.15) |
| Lack of Parent | .07 | −3.34 | −.82 | .15 | −4.55 | −.21 | .02 | −5.38 | .00 | .05 | −4.27 | −.13 |
| Regard | (.24) | (1.66) | (.20)* | (.25) | (1.31)* | (.41) | (.06) | (1.11)* | (.11) | (.07) | (1.13)* | (.13) |
| Favors | .21 | −4.15 | −.06 | .17 | −5.17 | .12 | .14 | −5.31 | .01 | .15 | −4.64 | −.02 |
| Punishment | (.07)* | (1.63) | (.11) | (.05)* | (1.24)* | (.08) | (.05)* | (1.08)* | (.08) | (.04)* | (1.05)* | (.07) |
|
| ||||||||||||
| Father | ||||||||||||
|
| ||||||||||||
| Conflict | .16 | −3.68 | −.14 | .15 | −4.77 | −.06 | .12 | −5.26 | −.05 | .13 | −3.39 | −.15 |
| (.04)* | (1.59) | (.06) | (.03)* | (1.25)* | (.07) | (.03)* | (1.05)* | (.06) | (.04)* | (1.04)* | (.08) | |
| Lack of | .09 | −3.32 | .00 | .16 | −4.71 | .05 | .06 | −5.33 | −.09 | .08 | −4.28 | −.05 |
| Involvement | (.11) | (1.63) | (.19) | (.07) | (1.27)* | (.12) | (.04) | (1.09)* | (.09) | (.03) | (1.11)* | (.07) |
| Lack of Parent | .10 | −3.34 | .07 | .13 | −4.55 | .23 | .06 | −5.38 | −.08 | .060 | −4.27 | −.03 |
| Regard | (.12) | (1.66) | (.21) | (.10) | (1.31)* | (.18) | (.04) | (1.11)* | (.09) | (.03) | (1.13)* | (.06) |
| Favors | .07 | −4.15 | .07 | −.02 | −5.17 | .21 | .01 | −5.31 | .11 | .01 | −4.64 | .09 |
| Punishment | (.07) | (1.63) | (.11) | (.06) | (1.24)* | (.09) | (.05) | (1.08)* | (.09) | (.04) | (1.05)* | (.06) |
Note. Unstandardized regression coefficients and standard errors are presented. The first model is the main effects model and includes all identified covariates, co-parent effects (except in the case of the marital variables), adoption status (“Adopt/Bio” = adoptive vs. biological), and the risk factor. The second model is the interaction model, including an interaction term between adoption status and the risk factor. Variables are coded so that higher levels of a risk factor indicate more problematic parenting; a positive sign for the regression weight for the “Risk Factor” indicates that as the value of the scale increases, so do child DBDs. Negative regression weights for “A/B” indicate lower rates of DBDs in biological children. ADHD, attention-deficit hyperactivity disorder; ODD, oppositional-defiant disorder; CD, conduct disorder; EXT, Externalizing factor.
p<.01.
Interactions between Parenting Behaviors and Adoptive Status
The interaction models in Table 4 show the effects for adoptive status by parenting variable interaction. There were two significant interactions: in the case of lack of maternal involvement and in lack of maternal parental regard on child CD symptoms. As maternal involvement decreased, CD symptoms in adoptive offspring increased [B(SE)=.67(.11), p< .01]; however, lack of maternal involvement had no effects on CD symptoms in biological offspring (B(SE)= −.07(.12), ns]. Likewise, as maternal parental regard decreased, CD symptoms increased in adoptive [B(SE)=.78(.18), p < .01], but not biological offspring (B(SE)= −.07(.08), ns].
Marital Quality/Divorce, Parental Antisociality, Adoptive Status, and Child DBDs
Main Effects of Marital Quality/Divorce, Parental Antisociality and Adoptive Status
The effects of marital discord and divorce showed minimal association with child DBD symptoms (Table 5). Two main effects, for ODD and EXT, indicated that as marital discord increased, ODD and general EXT symptoms increased as well. Out of the two significant original main effects, the effect of marital discord on offspring ODD symptoms was significant in the adoptive offspring. The effect of marital discord on offspring EXT was not significant in the adoptive offspring, but the effect was roughly equal in biological and adoptive offspring [B(SE) = .13 (.06), ns; .13 (.05), ns for adoptive and biological offspring, respectively]. There were no main effects of divorce, maternal or paternal antisociality on child DBD symptoms.
Table 5.
Relationship between marital conflict, divorce, and parental antisociality with child DBDs in adoptive and non-adoptive families.
| Risk Factors: |
CD | ODD | ADHD | EXT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Main effect model |
Interact
model |
Main effect model |
Interact
model |
Main effect model |
Interact
model |
Main effect model |
Interact
model |
|||||
|
| ||||||||||||
| Risk | A/B | Risk X | Risk | A/B | Risk X | Risk | A/B | Risk X | Risk | A/B | Risk X | |
| Factor | A/B | Factor | A/B | Factor | A/B | Factor | A/B | |||||
| Marital Variables | ||||||||||||
|
| ||||||||||||
| Marital | .14 | −3.04 | −.04 | .18 | −5.68 | .10 | .10 | −5.19 | .01 | .13 | −04.68 | −.01 |
| Discord | (.06) | (1.97) | (.13) | (.04)* | (1.39)* | (.09) | (.04) | (1.28)* | (.09) | (.04)* | (1.26)* | (.08) |
| Divorce | 1.47 | −3.85 | 2.05 | .59 | −5.06 | 3.29 | .29 | .29 | 6.08 | .53 | −4.59 | 2.95 |
| (2.67) | (1.68) | (5.64) | (1.94) | (1.25)* | (4.46) | (1.90) | (1.90)* | (3.94) | (1.50) | (1.10)* | (3.29) | |
|
| ||||||||||||
| Parental Antisociality | ||||||||||||
| Mom AAB | 2.42 | −4.44 | 1.97 | 2.05 | −5.32 | 7.09 | 1.42 | −5.41 | 11.03 | 1.77 | −4.81 | 8.29 |
| (2.01) | (1.68)* | (3.60)* | (1.42) | (1.27)* | (2.88) | (1.51) | (1.08)* | (2.75)* | (1.20) | (1.10)* | (2.36)* | |
| Dad AAB | 1.89 | −4.44 | 5.35 | .23 | −5.32 | 3.59 | .13 | −5.41 | 4.92 | .43 | −4.81 | 3.57 |
| (1.31) | (1.68)* | (2.53) | (.97) | (1.27)* | (1.98) | (.92) | (1.08)* | (1.84)* | (.71) | (1.10)* | (1.38)* | |
Note. Unstandardized regression coefficients and standard errors are presented. The first model is the main effects model and includes all identified covariates, co-parent effects (except in the case of the marital variables), adoption status (“Adopt/Bio” = adoptive vs. biological), and the risk factor. The second model is the interaction model, including an interaction term between adoption status and the risk factor. Variables are coded so that higher levels of a risk factor indicate more problematic parenting; a positive sign for the regression weight for the “Risk Factor” indicates that as the value of the scale increases, so do child DBDs. Negative regression weights for “A/B” indicate lower rates of DBDs in biological children. ADHD, attention-deficit hyperactivity disorder; ODD, oppositional-defiant disorder; CD, conduct disorder; EXT, Externalizing factor.
p<.01.
Interaction Effects of Marital Quality/Divorce and Parental Antisociality with Adoptive Status
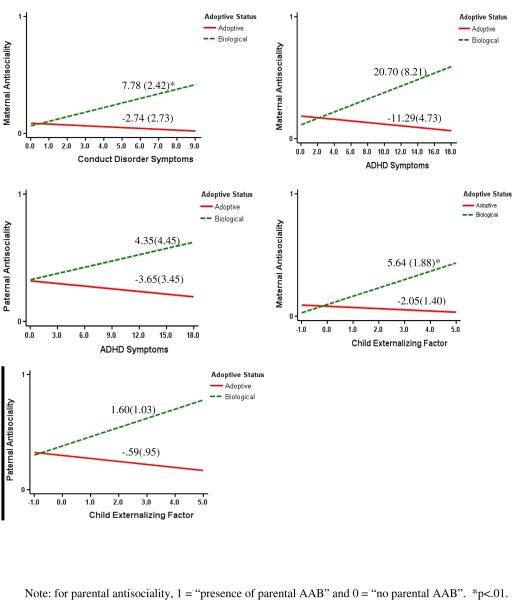
The interaction models of adoptive status by parental antisociality (Table 5) revealed several significant interactions for maternal and paternal antisociality. There were interaction effects of maternal antisociality and adoptive status on offspring CD, ADHD, and EXT symptoms. Maternal antisociality had a significant positive effect on CD symptoms and EXT in the biological adolescents, but no effect in adoptive adolescents (effects by group are reported in Figure 1). In other words, as maternal antisociality increased, so did CD and EXT symptoms in biological offspring. The effect of maternal antisociality on offspring ADHD symptoms was weaker, but with identical overall direction and pattern of results. As maternal antisociality increased so did ADHD symptoms in biological offspring (albeit nonsignificantly), but maternal AAB had little effect on adoptive offspring. Paternal antisociality was more strongly associated with children’s symptoms of ADHD and EXT in biological than adoptive families; yet, effects of paternal antisociality on these problems failed to reach significance in either the biological or adoptive adolescents. Overall, paternal AAB was significantly more associated with offspring DBD symptoms in biological compared to adoptive families, indicating a passive rGE transmission mechanism2.
Figure 1.
Interactions between parental antisociality and adoptive status on child DBDs
Discussion
The current study examined relative contributions of passive rGE and direct environmental influences on child psychopathology. In particular, we compared effects of maladaptive parenting, divorce, marital discord, and parental antisociality on child DBD symptoms in biological and adoptive families. Our study comprehensively replicates and extends prior literature in five ways. First, we used an entirely different methodological approach than most previous studies (Children of Twins and Extended Children of Twins designs), with consistent results across methodological approaches adding confidence to the larger body of literature. Second, whereas most studies on the topic concentrate on one type of familial risk factor (e.g., maladaptive parenting) we examined multiple risk factors simultaneously. Third, we examined relative contributions of both parents. Fourth, we examined all offspring in adolescence, after risk for many DBD symptoms has been expressed. Finally, we utilized a large sample, allowing us to detect even small rGE effects.
Our results indicated maternal and paternal parent-child conflict, maternal use of physical punishment, and (albeit in fewer cases) marital discord had a relatively equal effect on biological and adoptive children. These results are consistent with conceptual work and empirical studies of biological families on how parental behavior often shapes child behavioral outcomes (Loeber & Stouthamer-Loeber, 1986; Stormshak et al. 2000; Caspi et al. 2004; Stanger et al. 2004; Herndon & Iacono, 2005) and with findings from other genetically-informed designs indicating familial factors account for a moderate proportion of the shared environmental effect on child DBD symptoms (Rende et al. 1992; O'Connor et al. 2000; Burt et al. 2003; Neiderhiser et al. 2004; Burt et al. 2007; Harden et al. 2007; Neiderhiser et al. 2007; Burt et al. 2008; Narusyte et al. 2011). Cumulatively, our data and previous work suggest a large part of the socialization of child behavior is a function of interactions in close relationships constructed and sustained over time. And, the current findings add to the literature beginning to specify the nature of shared environmental influences in childhood and adolescence.
Nonetheless, it is important to note two cases where effects of familial factors differed between adoptive and biological adolescents (albeit in an unexpected direction). Effects of maternal involvement and parental regard for punishment were inversely associated with child CD symptoms more strongly in adoptive than biological children. In absence of replication, it remains uncertain how much credence to assign these findings, but there are possible interpretations. Adoptive adolescents may be more responsive to positive parenting behaviors because of their adoptive status. Or, adoptive parents might make more effort to use appropriate and healthy parenting techniques due to difficulty bonding with an adoptive child. Our study design is unable to disentangle parent-driven from child-driven effects, and understanding this finding should be a focus of future research. Our study is not unique in this unusual finding, as O’Connor et al. (2000) reported divorce had higher impact on adopted adolescents’ internalizing psychopathology and substance use.
Another important finding was that (a) there was no direct environmental effect of maternal or paternal antisociality, but (b) both maternal and paternal antisociality had stronger associations with child DBD symptoms in biological families than adoptive families. This finding is consistent with a passive rGE effect, where a general vulnerability toward DBD symptoms is passed down by the parents to the children. Previous research shows this general vulnerability manifests as antisocial behavior, alcohol use disorders, and drug use disorders in the mother/father but as attention problems, oppositionality, and conduct problems in pre-adolescent/adolescent offspring (Bornovalova, 2010; Silberg et al. 2012). The replication of part of that effect in the current study is important in its own right, given the methodological differences, and provides direction for future work. Particularly, future studies will benefit from examining the generality versus specificity of the passive rGE transmission mechanism in the relationship between adult EXT psychopathology and child DBD symptoms.
Several limitations of the present study should be noted. Foremost, it is important to understand adoptive and biological families differ from each other in more ways than merely the biological relationship between parent and child. Although families were selected to be similar on age and gender, they were not selected to be similar on other characteristics (e.g., income and ethnicity), and thus differ in this respect. Here, the adoptive parents were older, more educated, and reported fewer symptoms of paternal antisociality. While we statistically controlled for these effects, differences between parent-child associations in biologically related and adoptive families cannot automatically be assumed to be due to differences in genetic relatedness. It is necessary to replicate the current study using a sample of families with both a biological and adoptive child to ensure the consistency of the effects.
Further, the current sample had low rates of divorce and the adoptive families showed higher socioeconomic indices than the biological families, opening up possibility of range restriction. A lack of a main effect of divorce may have stemmed from this fact. Indeed, previous studies reporting a direct environmental effect of divorce on offspring DBD symptoms (e.g., D’Onofrio et al, 2005, 2007; O’Connor et al, 2000) have substantially higher rates of divorce (range 19%-23%). The low rate of divorce in the current sample along with differences in methodology could have contributed to the lack of consistency. Notably, however, McGue et al. (2007) showed range-restricted SES did not substantially affect estimates of shared environmental variance. Additionally, we could not rule out possibility of selective placement, as information about the mental health of birth parents was not available. However, most of the adoptions were international, with no opportunity for selective placement. Additionally, selective placement usually pertains to physical attributes and if an at-risk child were to be placed in a particularly nurturing environment, environmental effects would have diminished. Since the current study still detected multiple direct effects, selective placement is unlikely in this case. Finally, although less of a limitation than a future direction, it is important to extend the current design to the relationship between putative environmental risk factors and internalizing psychopathology.
To conclude, results from the current study indicate many parental risk factors affect children equally across genetically-related and non- related families. Other familial risk factors, however, (namely, parental antisociality) are associated with child DBD symptoms via the mechanism of passive rGE. Future directions might include using the current design to track how these effects change as a function of developmental context (late adolescence and adulthood). Indeed, shared environmental factors are major contributors to the variation in child DBD symptoms (Burt, 2009), whereas in late adolescence and adulthood this is not necessarily true. Passive rGE effects and direct environmental effects may, in later developmental stages, give way to influences of genetic effects. Understanding this type of developmental gene-environment interplay on child DBD symptoms is likely to contribute substantially to knowledge of the etiology of child DBD symptoms and inform intervention strategies to help prevent and minimize child psychopathology.
Acknowledgments
Data for this project were collected at the University of Minnesota. This work was supported by National Institute on Drug Abuse Grant DA05147, National Institute on Alcohol Abuse and Alcoholism Grants AA09367 and AA015621, and National Institute of Mental Health Grant T32 MH017069.
Footnotes
A previous study (Blazei et al. 2008) showed that boys and girls are similarly influenced by the parenting and familial variables used in the current study; thus, effects for males and females were not evaluated separately.
The current study used “probable” diagnostic cutoff for parental AAB. Thus, we were interested in investigating whether the effects remain even after using a “definite” diagnostic cutoff. The pattern of results was identical, and in 75% of the cases, the interaction effects found when including a probable diagnosis category held for only the definite diagnosis category.
References
- Bornovalova MA. Familial transmission and heritability of childhood disruptive disorders. American Journal of Psychiatry. 2010;167:1414–1414. doi: 10.1176/appi.ajp.2010.09091272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Blazei R, Malone SH, McGue M, Iacono WG. Disentangling the relative contribution of parental antisociality and family discord to child disruptive disorders. Personality Disorders: Theory, Research, and Treatment. 2012 doi: 10.1037/a0028607. epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braungartrieker J, Rende RD, Plomin R, Defries JC, Fulker DW. Genetic mediation of longitudinal associations between family environment and childhood behavior problems. Development and Psychopathology. 1995;7:233–245. [Google Scholar]
- Burt SA. Rethinking environmental contributions to child and adolescent psychopathology: A meta-analysis of shared environmental influences. Psychological Bulletin. 2009;135:608–637. doi: 10.1037/a0015702. [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, McGue M, Iacono WG. Parent-child conflict and the comorbidity among childhood externalizing disorders. Archives of General Psychiatry. 2003;60:505–513. doi: 10.1001/archpsyc.60.5.505. [DOI] [PubMed] [Google Scholar]
- Burt SA, McGue M, Krueger RF, Iacono WG. Environmental contributions to adolescent delinquency: A fresh look at the shared environment. Journal of Abnormal Child Psychology. 2007;35:787–800. doi: 10.1007/s10802-007-9135-2. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Morgan J, Rutter M, Taylor A, Arseneault L, Tully L, Jacobs C, Kim-Cohen J, Polo-Tomas M. Maternal expressed emotion predicts children's antisocial behavior problems: Using monozygotic-twin differences to identify environmental effects on behavioral development. Developmental Psychology. 2004;40:149–161. doi: 10.1037/0012-1649.40.2.149. [DOI] [PubMed] [Google Scholar]
- Denham SA, Workman E, Cole PM, Weissbrod C, Kendziora KT, Zahn-Waxler C. Prediction of externalizing behavior problems from early to middle childhood: The role of parental socialization and emotion expression. Development and Psychopathology. 2000;12:23–45. doi: 10.1017/s0954579400001024. [DOI] [PubMed] [Google Scholar]
- D’Onofrio BM, Turkheimer E, Emery RE, Slutske WS, Heath AC, Madden PAF. A genetically informed study of marital instability and its association with offspring psychopathology. Journal of Abnormal Psychology. 2005;114:570–586. doi: 10.1037/0021-843X.114.4.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio BM, Turkheimer E, Emery RE, Maes HH, Silberg JL, Eaves LJ. A children of twins study of parental divorce and offspring psychopathology. Journal of Child Psychology and Psychiatry. 2007;48:667–675. doi: 10.1111/j.1469-7610.2007.01741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn J, Plomin R. Determinants of maternal-behavior towards 3-year-old siblings. British Journal of Developmental Psychology. 1986;4:127–137. [Google Scholar]
- Dunn JF, Plomin R, Daniels D. Consistency and change in mothers behavior toward young siblings. Child Development. 1986;57:348–356. doi: 10.1111/j.1467-8624.1986.tb00034.x. [DOI] [PubMed] [Google Scholar]
- Dunn JF, Plomin R, Nettles M. Consistency of mothers behavior toward infant siblings. Developmental Psychology. 1985;21:1188–1195. [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Genetic and environmental influences on parental son relationships: Evidence for increasing genetic influence during adolescence. Developmental Psychology. 1997;33:351–363. doi: 10.1037//0012-1649.33.2.351. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: prospective links from adolescence to young adulthood. Journal of Abnormal Psychology. 2006;115:26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- Gartstein MA, Fagot B. Parental dysphoria, related family/parenting variables, and child externalizing behaviors: Effortful control as a potential mediator. Journal of Applied Developmental Psychology. 2003;24:143–177. [Google Scholar]
- Hanley JA, Negassa A, Edwardes MDD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: An orientation. American Journal of Epidemiology. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- Harden KP, Turkheimer E, Emery RE, D’Onofrio BM, Slutske WS, Heath AC, Martin NG. Marital conflict and conduct problems in children of twins. Child Development. 2007;78:1–18. doi: 10.1111/j.1467-8624.2007.00982.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herndon RW, Iacono WG. Psychiatric disorder in the children of antisocial parents. Psychological Medicine. 2005;35:1815–1824. doi: 10.1017/S0033291705005635. doi: doi:10.1017/S0033291705005635. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Price TS. Genotype-environment correlations: implications for determining the relationship between environmental exposures and psychiatric illness. Psychiatry. 2008;7:496–499. doi: 10.1016/j.mppsy.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Archives of General Psychiatry. 2001;58:453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Baker JH. Genetic influences on measures of the environment: A systematic review. sychological Medicine. 2007;37:615–626. doi: 10.1017/S0033291706009524. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Merikangas KR, Berglund P, Eaton WW, Koretz DS, Walters EE. Mild disorders should not be eliminated from the DSM-V. Archives of General Psychiatry. 2003;60:1117–1122. doi: 10.1001/archpsyc.60.11.1117. [DOI] [PubMed] [Google Scholar]
- King SM, Keyes M, Malone SM, Elkins I, Legrand LN, Iacono WG, McGue M. Parental alcohol dependence and the transmission of adolescent behavioral disinhibition: a study of adoptive and non-adoptive families. Addiction. 2009;104:578–86. doi: 10.1111/j.1360-0443.2008.02469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M. Family factors as correlates and predictors of juvenile conduct problems and delinquency. In: Tonry M, Morris N, editors. Crime and Justice. Vol. 7. University of Chicago Press; Chicago: 1986. pp. 219–339. [Google Scholar]
- McGue M, Keyes M, Sharma A, Elkins I, Legrand L, Johnson W, Iacono WG. The environments of adopted and non-adopted youth: Evidence on range restriction from the Sibling Interaction and Behavior Study (SIBS) Behavior Genetic. 2007;37:449–462. doi: 10.1007/s10519-007-9142-7. [DOI] [PubMed] [Google Scholar]
- McGue M, Lykken DT. Genetic influence on risk of divorce. Psychological Science. 1992;3:368–373. [Google Scholar]
- McGue M, Sharma A, Benson P. The effect of common rearing on adolescent adjustment: Evidence from a US adoption cohort. Developmental Psychology. 1996;32:604–613. [Google Scholar]
- Narusyte J, Neiderhiser JM, Andershed AK, D’Onofrio BM, Reiss D, Spotts E, Ganiban J, Lichtenstein P. Parental criticism and externalizing behavior problems in adolescents: The role of environment and genotype-environment correlation. Journal of Abnormal Psychology. 2011;120:365–376. doi: 10.1037/a0021815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neiderhiser JA, Reiss D, Lichtenstein P, Spotts EL, Ganiban J. Father-adolescent relationships and the role of genotype-environment correlation. Journal of Family Psychology. 2007;21:560–571. doi: 10.1037/0893-3200.21.4.560. [DOI] [PubMed] [Google Scholar]
- Neiderhiser JM, Reiss D, Pedersen NL, Lichtenstein P, Spotts EL, Hansson K. Genetic and environmental influences on mothering of adolescents: A comparison of two samples. Developmental Psychology. 2004;40:335–351. doi: 10.1037/0012-1649.40.3.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor TG, Caspi A, DeFries JC, Plomin R. Are associations between parental divorce and children’s adjustment genetically mediated? An adoption study. Developmental Psychology. 2000;36:429–437. [PubMed] [Google Scholar]
- Pickles A, Rowe R, Simonoff E, Foley D, Rutter M, Silberg J. Child psychiatric symptoms and psychosocial impairment: relationship and prognostic significance. British Journal of Psychiatry. 2001;179:230–235. doi: 10.1192/bjp.179.3.230. [DOI] [PubMed] [Google Scholar]
- Pike A, McGuire S, Hetherington EM, Reiss D, Plomin R. Family environment and adolescent depressive symptoms and antisocial behavior: A multivariate genetic analysis. Developmental Psychology. 1996;32:590–603. [Google Scholar]
- Plomin R. Genetics and Experience: The Developmental Interplay between Nature and Nurture. Sage; Newbury Park: 1994. [Google Scholar]
- Reiss D, Neiderhiser JM, Hetherington EM, Plomin R. The relationship code: Deciphering genetic and social influences on adolescent development. Harvard University Press; Cambridge: 2000. [Google Scholar]
- Rende RD, Slomkowski CL, Stocker C, Fulker DW, Plomin R. Genetic and environmental-influences on maternal and sibling interaction in middle childhood: A sibling adoption study. Developmental Psychology. 1992;28:484–490. [Google Scholar]
- Rhee SH, Waldman ID. Genetic and environmental influences on antisocial behavior: A meta-analysis of twin and adoption studies. Psychological Bulletin. 2002;128:490–529. [PubMed] [Google Scholar]
- Rothbaum F, Weisz J. Parental converging and child externalizing behavior in nonclinical samples: A meta-analysis. Psychological Bulletin. 1994;116:55–74. doi: 10.1037/0033-2909.116.1.55. [DOI] [PubMed] [Google Scholar]
- Silberg JL, Maes H, Eaves LJ. Unraveling the effect of genes and environment in the transmission of parental antisocial behavior to children’s conduct disturbance, depression and hyperactivity. Journal of Child Psychology and Psychiatry. 2012;53:668–677. doi: 10.1111/j.1469-7610.2011.02494.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbons M, First MB. Structured clinical interview for DSM-III-R personality disorders (SCID II) Biometrics Research Division, New York State Psychiatric Institute; NY: 1987. [Google Scholar]
- Spotts EL, Neiderhiser JM, Towers H, Hansson K, Lichtenstein P, Cederblad M, Pederson NL, Reiss D. Genetic and environmental influences on marital relationships. Journal of Family Psychology. 2004;18:107–119. doi: 10.1037/0893-3200.18.1.107. [DOI] [PubMed] [Google Scholar]
- Spotts EL, Prescott C, Kendler K. Examining the origins of gender differences in marital quality: A behavior genetic analysis. Journal of Family Psychology. 2006;20:605–613. doi: 10.1037/0893-3200.20.4.605. [DOI] [PubMed] [Google Scholar]
- Stanger C, Dumenci L, Kamon J, Burstein M. Parenting and children's externalizing problems in substance-abusing families. Journal of Clinical Child & Adolescent Psychology. 2004;33:590–600. doi: 10.1207/s15374424jccp3303_16. [DOI] [PubMed] [Google Scholar]
- Stormshak EA, Bierman KL, McMahon RJ, Lengua LJ. Parenting practices and child disruptive behavior problems in early elementary school. Journal of Clinical Child Psychology. 2000;29:17–29. doi: 10.1207/S15374424jccp2901_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welner Z, Reich W, Herjanic B, Jung K, Amado H. Reliability, validity, and parent-child agreement studies of the Diagnostic Interview for Children and Adolescents (DICA) Journal of the American Academy of Child and Adolescent Psychiatry. 1987;26:649–653. doi: 10.1097/00004583-198709000-00007. [DOI] [PubMed] [Google Scholar]