Abstract
Purpose
This study examined the acceptability and initial efficacy of a multimedia decision support (MDS) intervention to improve intention to complete an advanced directive (AD) among hospitalized adults following an episode of critical illness.
Data sources
This study used comparative quasi-experimental post-test only design. Forty-nine hospitalized adults, recovering from a critical illness, received either MDS or AD educational brochure. Demographic characteristics and self-report measures of AD knowledge were captured at baseline and used as covariates. Helpfulness of the intervention (acceptability) and the outcome variable, intention to complete an AD decision, were assessed after exposure to the MDS intervention or educational brochure (information-only control condition).
Conclusions
The MDS was a more acceptable form of education compared to a brochure. After adjusting for covariates, participants exposed to the MDS intervention were 24.7 times more likely to intend to complete an AD compared to those who were assigned to the information-only control condition.
Implications for practice
This pilot study establishes the acceptability and initial efficacy of the MDS intervention among individuals with critical illness, who are at high risk for hospital readmission life-sustaining treatment. This study illuminates a teachable moment in which patients are more receptive to interventions to complete an AD.
Keywords: advance direct, hospitalized adults, educational interventions, decision support, critical illness
The Patient Protection and Affordable Healthcare and Federal Patient Self-Determination Acts underscore the importance of decision support and advance care planning. However, Kass-Bartelmes, Hughes, & Rutherford (2003) and Camhi et al., (2009) report that less than 50% of hospitalized adults who were severely or terminally ill had advance directives (ADs) documented in their medical records. Hospitalized adults who are critically ill and require temporary life-sustaining treatments, such mechanical ventilation, hemodialysis, or artificial nutrition, represent a high risk cohort likely to experience frequent hospital readmissions, impaired functional status, and a recurring need for life-sustaining treatments (Cox & Carson, 2007; Cox, Carson, & Lindquist, 2007; Cox et al., 2009; Daly & Douglas, 2005; Douglas & Daly, 2001; Douglas, Daly, Gordon, & Brennan, 2002; Douglas, Daly, Kelley, O'Toole, & Montenegro, 2007). Among chronically critically ill adults, AD completion rates are low. These individuals are at high risk for readmission. In a recent study by Camhi and colleagues (2009), only 16% of chronically ill adults with prolonged mechanical ventilation had ADs established before or after their episode of critical illness. This research illuminates the need for establishing ADs prior the patient’s discharge and before subsequent hospital admissions to promote patient-centered decision making. Yet, few studies have explored educational interventions to promote intention to complete an AD among hospitalized adults recovering from a critical illness.
A patient’s perception of illness and their preferences for life-sustaining treatments may change as a result of their hospital experience. Exposure to life-sustaining treatments and convalescence in a hospital may serve as opportune time to provide AD education to hospitalized adults. Teachable moments, naturally occurring cueing events, can alter an individual’s state of receptiveness to receive health education and stimulate their contemplation leading to a desired health behavior change (Cohen, Clark, Lawson, Casucci, & Flocke, 2011; Flocke et al., 2012). Previous work among patients admitted to an emergency department or an intensive care unit for an acute health problems (Boudreaux, Bock, & O'Hea, 2012; Boudreaux et al., 2010; Clark & Moss, 2011), and several studies conducted in primary care and outpatient settings indicate that the risk of acute health problem can signify a teachable moment that permits healthcare providers an opportunity to introduce health education resources and effectively facilitate a desired health behavior change (Cohen, et al., 2011; Floyd, Steffens, Pavlik, & Andrykowski, 2011; Sommers, Lyons, Bohn, Ribak, & Fargo, 2013). Building on this previous research and the premise of a teachable moment, we postulated that the experience of surviving an episode of critical illness requiring an acute episode of mechanical ventilation may alter a hospitalized adult’s perspective on advance care planning by increasing their receptiveness to educational interventions focused on AD completion.
This pilot study aimed to capitalize on the routinely missed teachable moment by examining the effects of two educational interventions to overcome established factors that influence AD decision making (age, race, and knowledge of ADs) and enhance the intention to complete AD among hospitalized adults (Alano et al., 2010; Salmond & Estrellam, 2005; Tamura, Goldstien, & Perez-Stable, 2010). Therefore, the purpose of this study is to present evidence on the acceptability and initial efficacy of a multimedia decision support (MDS) intervention when compared to the American Hospital Association’s commonly used educational brochure, Putting It In Writing, among hospitalized adults recovering from a critical illness.
Methods
Design
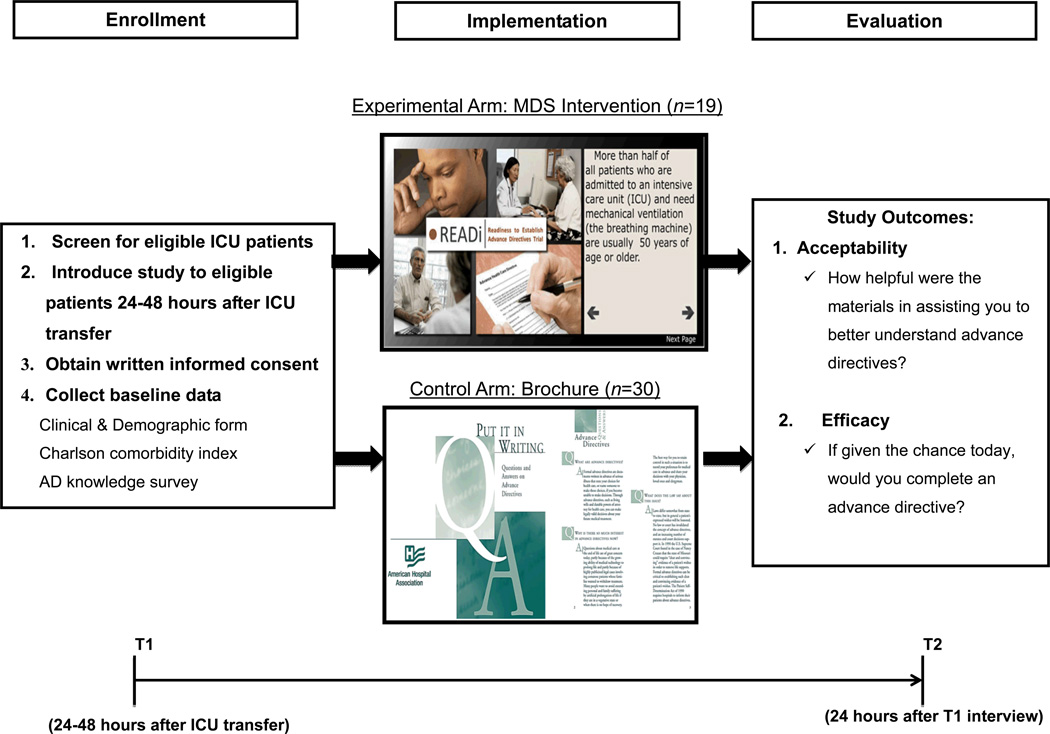
As shown in Figure 1, this is a comparative quasi-experimental study with a posttest-only design. The first 30 subjects enrolled into this study were assigned to the control condition and received the American Hospital Association’s Putting It In Writing brochure (retrieved from http://www.aha.org/content/13/putitinwriting.pdf). Subsequently enrolled subjects (n=19) were assigned to the experimental condition, the MDS intervention. Subjects exposed to, the MDS intervention received a single dose of the interactive computer program administered on a laptop computer. The components of the intervention were: (1) a 10 minute video vignette of a patient and his spouse who have not considered an AD and conveys the psychological impact of not having an AD had on the spouse while providing education about ADs; and (2) interactive education consisting of state specific AD education and additional internet resources on advance care planning. Subjects assigned to the either study condition were exposed a single of dose of the respective educational intervention immediately after the collection of their demographic data.
Figure 1.
Overview of subject flow through the study protocol
Sample
A convenience sample of hospitalized adults (N=49) who required an episode of acute mechanical ventilation were recruited from the medical and surgical intensive care unit (ICUs) of an academic medical center in Northeast Ohio. Subject screening and recruitment were conducted from January 2011 to February 2012. Subjects were at least 50 years of age, required acute mechanical ventilation for less than 72 hours, convalesced on an inpatient unit, made his/her own healthcare decisions, and did not have AD documentation in their medical records at ICU discharge. Hospitalized adults were excluded if they were unable to read and speak English, had severe vision or hearing impairment, or received inpatient palliative and/or hospice care.
Instrumentation
Acceptability
Acceptability of the educational interventions was measured by the single item question, “How helpful were the materials in assisting you to better understand advance directives?” This item was constructed as Likert scale from zero (not at all helpful) to 10 (extremely helpful). A mean score and standard deviation for the item was calculated to quantify acceptability.
Efficacy
Efficacy was assessed by a single item, “If given the chance today, would you complete a written advance directive?” with “do not intend to complete an AD” or “intend to complete an AD” as the responses. Immediately upon enrollment, participants received the intervention. Thus, this question was administered post-test only to reduce a potential threat to internal validity, testing effect, from repeated exposures to this single-item (Shadish, Cook, & Campbell, 2002).
Covariates
Based on prior research examining the effects of interventions to enhance AD completion rates (Alano, et al., 2010; Salmond & Estrellam, 2005; Tamura, et al., 2010), age, race, and level of pre-existing knowledge of ADs have been shown to influence AD completion and were selected a priori as covariates. To capture age and race, each subject self-reported his or her age and racial identity. The Advance Directive Survey (ADS) was used to assess knowledge of ADs. For this survey, subjects endorse a response for each of the five items, provided in a multiple-choice format. Correct answers are scored as one, and incorrect answers are scored as zero. A total score, ranging from 0 to 5, was calculated by adding the number of correct responses. A higher ADS scores indicate that the subject has greater knowledge on ADs. This questionnaire has established construct validity in a sample of hospitalized male veterans (Johnson-Greene et al., 1996). In this sample of hospitalized adults, the Kuder Richardson (KR)-21 formula coefficient was .42, which indicates an adequate internal reliability consistency for a dichotomously scored scale consisting of less than 10 items.
Procedures
Subject recruitment and screening
Institutional review board approval from the academic medical center was obtained prior to the conduct of this clinical research. Each week day, the research assistant screened critically ill patients for study eligibility, by review of the mechanical ventilation records and progress notes. All eligible critically ill patients transferred from the ICU to an inpatient unit were approached for study participation within 24–48 hours after their admission to an inpatient unit.
Data Collection
Data were collected by structured interviews at two time points, at baseline (24–48 hours after transfer from an ICU) and 24 hours following baseline (T2). Each interview was 30–40 minutes in duration. Clinical and demographic data were obtained from the patient’s electronic and physical medical records and assessment of AD knowledge were collected at baseline. Data on intention to complete an AD and the acceptability of the intervention were collected at T2.
Data Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS, version 20; Somers, NY). Descriptive statistics, chi square analyses, independent samples t-tests, and a logistic regression for multiple predictor variables were employed to evaluate acceptability, and efficacy of the MDS intervention compared to the AHA’s brochure, Putting It In Writing. The criterion for statistical significance for all statistical tests included in this report was p≤.05.
Acceptability
To determine the acceptability of the two educational interventions, descriptive statistics (means and standard deviations) of the single item measure, “How helpful were the materials in assisting you to better understand advance directives?” were generated, and an independent samples t-test was performed to determine if acceptability differed by group assignment.
Efficacy
A hierarchical logistic regression with multiple predictors was performed to assess the effects of group assignment on the outcome variable, intention to complete an AD, while adjusting for the potential influences of covariates (age, race, and AD knowledge). To determine the unique contribution of the covariates and the independent variable (group assignment), the covariates were simultaneously entered into model and the independent variable was subsequently entered.
Results
Sample characteristics
Table 1 shows the clinical and demographic characteristics of subjects by group assignment (n=49). This convenience sample of hospitalized adults had a mean age of 63 (SD=9.5) years. Most subjects were white (63%), male (59%), transferred from the surgical ICU (84%), and experienced a mean ICU and hospital lengths of stay of 3.2 (SD=4.1) days and 11.4 (SD=8.0) days respectively. There was a significant difference in age by group assignment. On average, the subjects exposed to the experimental condition were younger (M= 60.0, SD=6.0) compared to subjects in the control group (M=65.4, SD=10.8, t=2.2 p<.05). At baseline, AD knowledge scores did not differ by group assignment (t=.85, p=.40).
Table 1.
Clinical and demographic characteristics of subjects by group assignment
| Variable | Control (n=30) | Experimental (n=19) | |||
|---|---|---|---|---|---|
| M | SD | M | SD | t | |
| Age (years) | 65.4 | 10.8 | 60.0 | 6.0 | 2.2* |
| ICU LOS (days) | 2.7 | 2.4 | 4.0 | 5.9 | −.97 |
| Hospital LOS (days) | 10.2 | 6.9 | 13.3 | 9.3 | −1.3 |
| Charlson comorbidity index | 2.7 | 6.8 | 3.1 | 4.2 | −.25 |
| n | % | n | % | χ2 | |
| Gender: Male | 19 | 63 | 10 | 53 | .55 |
| Race: White | 18 | 60.0 | 13 | 68.4 | .35 |
| Marital status: Married | 17 | 56.7 | 7 | 36.8 | 1.8 |
| Annual income | |||||
| $20,000 or less | 7 | 25.9 | 4 | 21.1 | .18 |
| $20,001–49,999 | 10 | 37.0 | 7 | 36.8 | |
| $50,000 or more | 10 | 37.0 | 8 | 42.1 | |
Note. ICU LOS: intensive care unit length of stay. Hospital LOS: hospital length of stay.
p <.05.
Acceptability
At T2, subjects (n=44) completed a single item measure to assess the helpfulness of the educational resources delivered by each intervention. On average, subjects who were assigned to the MDS intervention (M=8.11, SD=3.84) found the educational content more helpful in improving their understanding of ADs compared to subjects exposed to the information-only control group (M=5.80, SD=3.84, t=−2.67, p=.03). The post hoc effect size was large (d=.68) and the observed power (1-β) was .71 (one-tailed).
Efficacy
In order to examine the influence of MDS intervention on the outcome variable, intention to complete an AD, we conducted a hierarchical logistic regression analysis. In the initial step of the regression model, intention to complete an AD decision was regressed on covariates known to affect AD decision making (age, race, and AD knowledge), which did not achieve statistical significance. In the final step, the independent variable, group assignment, was added to evaluate its contribution to the model. As seen in Table 2, with study group assignment included in the model, the explained variance, Nagelkerke R2, was .501 and the overall correct classification of 79%. Based on this final model, subjects exposed to the MDS intervention were 24.7 times more likely to intend to complete an AD compared to those who were assigned to the control condition. In addition to exposure to the MDS intervention, having an effect on the intention to complete an AD, subjects who were white (OR=7.275, p=.049) and having lower AD knowledge scores (OR=.399, p=.040) were found to be more likely to intend to complete an AD after controlling for age and group assignment.
Table 2.
Hierarchical logistic regression of intention to complete an AD decision on age, race, AD knowledge, and group assignment (n=41)
| Predictor | β | SE β | Exp β | p | |
|---|---|---|---|---|---|
| Step 1 | Age (0=50–64 yrs., 1=≥65 yrs.) | −.306 | .749 | .736 | .736 |
| Race (0=white, 1=nonwhite) | 1.091 | .755 | 2.98 | .678 | |
| AD knowledge | −.658 | .315 | .518 | .279 | |
| Step 2 | Age | .775 | .930 | 2.171 | .405 |
| Race | 1.984 | 1.006 | 7.275 | .049* | |
| AD knowledge | −.918 | .448 | .399 | .040* | |
| Group assignment (0=control, 1=experimental) | 3.206 | 1.608 | 24.690 | .004** |
Note. AD: advance directive. Yrs.: years. Dependent variable: intention to complete an AD.
Model statistics for step 1: R2= .151 (Cox & Snell), .203 (Nagelkerke). Model χ2=6.697, df=3, p=.082. Hosmer & Lemeshow test (χ2=12.408, df=8, p=.137).
Model statistics for step 2: ΔR2= .221 (Cox & Snell), .298 (Nagelkerke). R2= .372 (Cox & Snell), .501 (Nagelkerke). Model χ2=19.074, df=4, p<.0. Hosmer & Lemshow test (χ2=2.748, df=7, p=.907). Overall correct classification was 79% for this model.
p<.05,
p<.01.
Discussion
The results of this comparative quasi-experimental study establish the preliminary evidence for the acceptability and efficacy of the MDS intervention among hospitalized adults recovering from a critical illness. In the present study, our two educational interventions helped to increase subjects understanding of ADs. In particular, subjects assigned to the experimental condition found the interactive MDS intervention significantly more helpful compared to the educational brochure. Notably, this study confirms a statistically and clinically significant difference by group assignment in the proportion of subjects who intended to complete an AD. There was a significant difference in the proportion of subjects exposed to experimental condition were more inclined to complete an AD compared who received the information only. Thus, these preliminary results are quite promising regarding the acceptability and efficacy of the MDS intervention. Our results using a single dose electronic intervention demonstrate similar efficacy as studies that have used combine approaches, counseling with education, to improve rates of AD completion (Heffner, Fahy, Hilling, & Barbieri, 1997; Payne, Prentice-Dunn, & Allen, 2009; Song et al., 2010). In addition to establishing the influence of the MDS intervention on intention to complete an AD decision, we found two significant predictors. Lower AD knowledge scores and individuals who identified their race as white were more likely have the intention to complete an AD. Our findings regarding the influence of race and AD knowledge are consistent with the work of Sulmasky, Song, Marx, & Mitchell (1996) and Alano et al., (2010).
Limitations
There are several limitations that affect the internal and external validity of this research. First, the research design was quasi-experimental and subjects were not randomly assigned to the study conditions, but rather enrolled into the study sequentially. Second, the primary outcome, intention to complete an AD, was only captured after the subject was exposed to a study condition. This posttest only design precluded statistically controlling for within-subject variation across time, but does reduce the threat of testing. Third, the research design did not account for a novelty effect of our MDS intervention, and future research is recommended to prospectively compare the efficacy of two electronic educational interventions. Lastly, the sample is small and consists of clinical and demographic characteristics that limit the external generalizability of the results to hospitalized adults who are white males with moderate levels of education and socioeconomic status.
Implications for Practice
This pilot study established the acceptability and efficacy among hospitalized patients recovering from a critical illness. Educational interventions have been tested and efficacious, but have not considered the timing of intervention exposure which could impact receptiveness to establishing an AD and subsequently, the efficacy of intervention. In clinical practice, advance practice nurses seize naturally occurring opportunities, teachable moments, to provide education and foster health promotion behaviors. Yet, discussions about advance directives are routinely omitted from the clinical management of acutely ill patients in hospital settings before discharge. This study provides evidence for a promising computer mediated intervention to promote completion of an AD, while capitalizing on the use of technology to minimize workload burden of registered nurses and advanced practice nurses. This technology allows patients to access educational materials and provides patients with a unique self-customized experience that promotes reflection, leveraging the teachable moment that may be embedded in the experience of critical illness. Future research should evaluate the essential components of the intervention, determine the mechanism by which the intervention works to increase intention to complete an AD, and examine the influence of the technology on the behavior of AD completion.
Acknowledgments
Personal acknowledgements:
This publication was made possible by funding from Case Western Reserve University, Center on Aging and Health and the following grant awards: 2KLTR000440-06, L30RR033212, and L30MH091738 from the National Center for Advancing Translation Science (NCATS), the former National Center for Research Resources (NCRR), and the National Institute of Mental Health (NIMH), components of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCATS, NCRR, NIMH, or the NIH.
Contributor Information
Ronald L. Hickman, Jr, Assistant Professor, Case Western Reserve University, School of Nursing, Cleveland, OH, Acute Care Nurse Practitioner, University Hospitals Case Medical Center, Cleveland, OH.
Amy R. Lipson, Email: arl11@case.edu, Research Associate, Case Western Reserve University, Cleveland, OH.
Melissa D. Pinto, Email: mdp55@case.edu, KL2 Clinical Research Scholar and Instructor, Case Western Reserve University, Cleveland, OH.
Grant Pignatiello, Email: gap54@case.edu, BSN Student, Case Western Reserve University, Cleveland, OH.
References
- Alano G, Pekmezaris R, Tai J, Hussain M, Jeune J, Louis B, Wolf-Klein G. Factors influencing older adults to complete advance directives. Palliative and Supportive Care. 2010;8(3):267–275. doi: 10.1017/S1478951510000064. [DOI] [PubMed] [Google Scholar]
- Boudreaux E, Bock B, O'Hea E. When an event sparks behavior change: An introduction to the sentinel event method of dynamic model building and its application to emergency medicine. Academic Emergency Medicince. 2012;19:329–335. doi: 10.1111/j.1553-2712.2012.01291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreaux E, Moon S, Baumann B, Camargo C, O'Hea E, Ziedonis D. Intentions to quit smoking: Causal attribution, perceived illness severity, and event-related fear during an acute health event. Annals of Behavioral Medicine. 2010;40:350–355. doi: 10.1007/s12160-010-9227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camhi S, Mercado A, Morrison S, Du Q, Platt D, August G, Nelson J. Deciding in the dark: Advance directives and continuation of treatment in chronic critical illness. Critical Care Medicine. 2009;37(3):919–925. doi: 10.1097/CCM.0b013e31819613ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark B, Moss M. Secondary prevention in the intensive care unit: Does ICU admission represent a "teachable moment". Critical Care Medicine. 2011;39(6):1500–1506. doi: 10.1097/CCM.0b013e31821858bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen D, Clark E, Lawson P, Casucci B, Flocke S. Identifying teachable moments for health behavior counseling in primary care. Patient Education and Counseling. 2011;85(2):e8–e15. doi: 10.1016/j.pec.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox C, Carson S. An economic evaluation of prolonged mechanical ventilation. Critical Care Medicine. 2007;35(8):1918–1927. doi: 10.1097/01.CCM.0000275391.35834.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox C, Carson S, Lindquist J. Differences in one year health outcomes and resource utilization by definition of prolonged mechanical ventilation: a prospective cohort study. Critical Care Medicine. 2007;11(1):120–131. doi: 10.1186/cc5667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox C, Martinu T, Sathy S, Clay A, Chia J, Gray A, Tulsky J. Expectations and outcomes of prolonged mechanical ventilation. Critical Care Medicine. 2009;37(11):2888–2894. doi: 10.1097/CCM.0b013e3181ab86ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly B, Douglas S. Trial of a Disease Management Program to reduce Hospital Readmissions of the Chronically Critically Ill. CHEST. 2005;128(2):507–517. doi: 10.1378/chest.128.2.507. [DOI] [PubMed] [Google Scholar]
- Douglas S, Daly B. Hospital Readmission Among Long-term Ventilator Patients. CHEST. 2001;120(4):1278–1286. doi: 10.1378/chest.120.4.1278. [DOI] [PubMed] [Google Scholar]
- Douglas S, Daly B, Gordon N, Brennan P. Survival and quality of life: Short-term versus long-term ventilator patients. Critical Care Medicine. 2002;30(12):2655–2662. doi: 10.1097/00003246-200212000-00008. [DOI] [PubMed] [Google Scholar]
- Douglas S, Daly B, Kelley C, O'Toole E, Montenegro H. Chronically Critically Ill Patients: Health-Related quality of Life and Resource Use after a Disease Management Intervention. Journal of Critical Care. 2007;16(5):447–457. [PMC free article] [PubMed] [Google Scholar]
- Flocke S, Antognoli E, Step M, Marsh S, Parran T, Mason J. A teachable moment communication process for smoking cessation talk: Description of a group randomized clinician-focused intervention. BMC Health Services Research. 2012;12(109) doi: 10.1186/1472-6963-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd A, Steffens R, Pavlik E, Andrykowski M. Receipt of a false positive test result during routine screening for ovarian cancer: A teachable moment? Journal of Clinical Psychology in Medical Settings. 2011;18(1):70–77. doi: 10.1007/s10880-011-9226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heffner JE, Fahy B, Hilling L, Barbieri C. Outcomes of advance directive education of pulmonary rehabilitation patients. American journal of respiratory and Critical Care Medicine. 1997;155(3):1055–1059. doi: 10.1164/ajrccm.155.3.9116986. [DOI] [PubMed] [Google Scholar]
- Johnson-Greene D, Anderson C, Adams K, Buchtel H, Miller T, Dehring M. The psychologist's role in assessing and facilitating patients' knowledge of advance directives in medical settings: A preliminary investigation. Journal of Clinical Psychology in Medical Settings. 1996;3(2):103–113. doi: 10.1007/BF01996131. [DOI] [PubMed] [Google Scholar]
- Kass-Bartelmes B, Hughes R, Rutherford M. Advance care planning: preferences for care at end of life. Research in Action. 2003;12 Retrieved from http://www.scribd.com/doc/47966710/AHRQ-Research-In-Action-Advance-Care-Planning. [PubMed] [Google Scholar]
- Payne KL, Prentice-Dunn S, Allen RS. A comparison of two interventions to increase completion of advance directives. Clinical Gerontologist. 2009;33(1):49–61. [Google Scholar]
- Salmond S, Estrellam D. Attitudes toward advance directives and advance directive completion rates. Orthopaedic Nursing. 2005;24(2):117–127. doi: 10.1097/00006416-200503000-00007. [DOI] [PubMed] [Google Scholar]
- Shadish W, Cook T, Campbell D. Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin; 2002. p. 55. [Google Scholar]
- Sommers M, Lyons M, Bohn M, Ribak C, Fargo J. Health-compromising behaviours among young adults in the urban emergency department: Opportunity for a teachable moment. Clinical Nursing Research. 2013 doi: 10.1177/1054773812471971. [DOI] [PubMed] [Google Scholar]
- Song J, Ratner E, Bartels D, Ulvestad N, Petroskas D, West M, Gelberg L. Effect of an end-of-life planning interventio on the completion of advance directives in homeless persons: a randomized trial. Annals of Internal Medicine. 2010;153(2):76–84. doi: 10.7326/0003-4819-153-2-201007200-00003. [DOI] [PubMed] [Google Scholar]
- Sulmasy D, Song K, Marx E, Mitchell J. Strategies to promote the use of advance directives in a residency outpatient practice. Journal of General Internal Medicine. 1996;11(11):657–663. doi: 10.1007/BF02600156. [DOI] [PubMed] [Google Scholar]
- Tamura M, Goldstien M, Perez-Stable E. Preferences for dialysis withdrawal and engagement in advance care planning within a diverse sample of dialysis patients. Nephrology Dialysis Transplantation. 2010;25(1):237–242. doi: 10.1093/ndt/gfp430. [DOI] [PMC free article] [PubMed] [Google Scholar]