Abstract
A postpartum four-vessel cervical artery dissection with no stroke is reported. This transient vasculopathy took place in the autoimmune context of the HELLP syndrome combined with the reversible posterior leucoencephalopathy syndrome. Correlations between the clinical, radiological and biological entities are discussed.
Key Words : Postpartum cervical artery dissection, HELLP syndrome, Immunity
Introduction
Pires et al. [1] have recently published a case report of a 31-year-old woman who developed four-vessel cervical artery dissection (CAD) without stroke 18 days after an uncomplicated caesarean delivery. As no mechanical trigger event or prolonged vaginal labour was observed, this case emphasizes the possible vasculotropic origin of this disorder, as suggested by some authors [2].
We report a new case of a woman presenting with postpartum four-vessel CAD with no stroke at all in the context of the HELLP syndrome (haemolysis with elevated liver enzymes and low platelet count).
Case Report
A 39-year-old woman had been followed by her obstetrician during her first pregnancy without any complication until the 34th week of gestation when she complained of unusual headaches and epigastric pain. Her blood pressure was found to be 190/110 mm Hg with positive proteinuria findings consistent with a preeclampsia syndrome. Blood samples showed thrombopenia (80,000/mm3) and mild elevation of liver function tests (serum glutamic oxaloacetic transaminase and serum glutamic pyruvic transaminase were 100 IU/mm3). These abnormalities were suggestive of the HELLP syndrome. An emergency caesarean section was performed. The infant's initial Apgar score was 2 and the newborn baby was immediately transferred to the Paediatric Reanimation Department with good achievement a few days later.
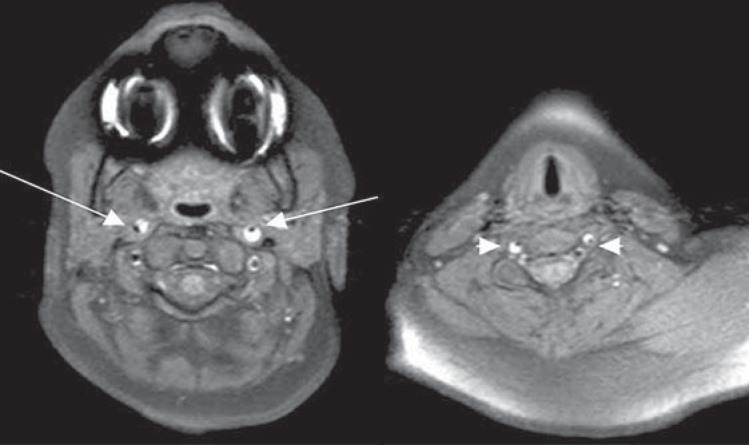
The mother's blood pressure was controlled with intravenous polytherapy (nicardipine and labetalol). She was transferred to the Reanimation Department due to thrombopenia; at the same time, acute renal failure was observed. On day 10, she presented with spontaneous abnormal movements of her right body side. No focal signs were detected. Brain imaging using fluid-attenuated inversion recovery magnetic resonance (FLAIR-MR) sequences revealed multiple bilateral high signal intensity in the frontoparietal lobes. T1-weighted, fat-suppressed axial cranial MR images (fig. 1) showed the presence of a four-vessel CAD with no stroke seen on the diffusion-weighted images. Anticoagulation therapy was started and after a few days, while biological abnormalities improved progressively, the patient was transferred from the Reanimation to the Neurology Department.
Fig. 1.
T1-weighted, fat-suppressed axial cranial MRI showing intramural haematomas on the two extracranial internal carotid arteries (arrows) and on the two vertebral arteries (arrowheads).
Several controls of the cervical arteries using the cervical echo Doppler and transcranial ultrasound system did not show artery modifications, but a second brain MRI revealed the complete withdrawal of the initial FLAIR lesions compatible with the reversible posterior leucoencephalopathy syndrome. The patient was discharged from the hospital at postpartum day 26. An MRA was performed at month 3 coupled with a cervical Doppler examination. Dissection signs had completely resolved at that time. The patient was asymptomatic and the baby was developing normally. After 1 year of follow-up, the patient did not complain of any neurologic symptom.
Discussion
Four-vessel CAD is an extremely rare condition which is found in 1.3 cases among 1,000 dissections [3]. Nothing is known about the prognosis and the risk of associated stroke; however, we suppose that the early activation of intracranial collateral vessels might influence the outcome [4].
Postpartum CAD is also an uncommon cause of stroke and represents only 6% of all cervical dissections in women [2]. According to Arnold et al. [2], CAD in the context of the postpartum period is more frequently coupled with reversible cerebral vasoconstriction syndrome, subarachnoid haemorrhage or reversible posterior leucoencephalopathy syndrome. In such cases, reversible posterior leucoencephalopathy syndrome is related to high blood pressure, but no direct link with CAD has ever been reported to date [5].
The HELLP syndrome is biologically defined as the association of haemolysis (H), elevated liver enzymes (EL) and a low platelet count (LP), and it occurs in about 0.2-0.8% of pregnancies. It is usually associated with preeclampsia, which is defined as de novo hypertension in pregnancy (>140/90 mm Hg after 20 weeks of gestation) returning to normal after having given birth, and the presence of proteinuria [6]. Experts in the field consider the central role to be autoimmune thrombotic microangiopathy leading to the development of the HELLP syndrome [6]. However, cases of CAD are very rare in this context, and to our knowledge only 2 have been published to date: the first case involves a bithalamic infarct as a result of a left vertebral artery dissection [7] and the second case a bilateral internal carotid artery dissection without stroke in a severe preeclamptic setting [8]. However, in view of the current knowledge, no correlation between the HELLP syndrome and CAD can be established.
In conclusion and in agreement with Pires et al. [1], we hypothesize that a transient cervical artery vasculopathy may have led to the patient's four-vessel CAD. In our case, this impression is supported by the inadequate immune response resulting in the development of the HELLP syndrome.
Disclosure Statement
The authors have no conflict of interest to disclose.
References
- 1.Pires C, Geraldes R, Neto L, Melo TP. Spontaneous multiple cervical artery dissection in the puerperium. Cerebrovasc Dis. 2011;32:511–512. doi: 10.1159/000332089. [DOI] [PubMed] [Google Scholar]
- 2.Arnold M, Camus-Jacqmin M, Stapf C, Ducros A, Viswanathan A, Berthet K, et al. Postpartum cervicocephalic artery dissection. Stroke. 2008;39:2377–2379. doi: 10.1161/STROKEAHA.107.510107. [DOI] [PubMed] [Google Scholar]
- 3.Arnold M, De Marchis GM, Stapf C, Baumgartner RW, Nedeltchev K, Buffon F, Galimanis A, Sarikaya H, Mattle HP, Bousser MG. Triple and quadruple spontaneous cervical artery dissection: presenting characteristics and long-term outcome. J Neurol Neurosurg Psychiatry. 2009;80:171–174. doi: 10.1136/jnnp.2008.155226. [DOI] [PubMed] [Google Scholar]
- 4.Silvestrini M, Altamura C, Cerqua R, Pedone C, Balucani C, Luzzi S, Bartolini M, Provenciali L, Vernieri F. Early activation of intracranial collateral vessels influences the outcome of spontaneous internal carotid artery dissection. Stroke. 2011;42:139–143. doi: 10.1161/STROKEAHA.110.595843. [DOI] [PubMed] [Google Scholar]
- 5.Lee VH, Wijdicks EFM, Manno EM, Rabinstein AA. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol. 2008;65:205–210. doi: 10.1001/archneurol.2007.46. [DOI] [PubMed] [Google Scholar]
- 6.Abildgaard U, Heimdal K. Pathogenesis of the syndrome of hemolysis, elevated liver enzymes, and low platelet count (HELLP): a review. Eur J Obstet Gynecol Reprod Biol. 2013;166:117–123. doi: 10.1016/j.ejogrb.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 7.Borelli P, Baldacci F, Vergallo A, Del Dotto P, Lucetti C, Nuti A, Bonuccelli U. Bilateral thalamic infarct caused by spontaneous vertebral artery dissection in pre-eclampsia with HELLP syndrome: a previously unreported association. J Stroke Cerebrovasc Dis. 2012;21:914.e9–e10. doi: 10.1016/j.jstrokecerebrovasdis.2012.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Hoffmann C, Augé M, Falzone E, Martel-Jacob S, Mercier FJ. Bilateral carotid artery dissection in a severe preeclamptic setting: an unusual cause of postpartum headache. Ann Fr Anesth Reanim. 2013;32:267–270. doi: 10.1016/j.annfar.2013.02.008. [DOI] [PubMed] [Google Scholar]