Abstract
Parental responses to children with chronic pain have been shown to influence the extent of the child’s functional disability, but these associations have not been well-studied in relation to children’s pain-related school functioning. The current study tests the hypothesis that parental pain catastrophizing and parental protective responses to child pain influence the extent of school impairment in children with chronic pain. A mediational model was tested to determine whether parental protective behaviors serve a mediating role between parental pain catastrophizing and child school impairment. Study participants were a clinical sample of 350 children ages 8–17 with chronic pain and their parents. Measures of pain characteristics, demographic characteristics, child depressive symptoms, school attendance rates, overall school functioning, parental pain catastrophizing and parental protective responses to pain were collected. Results show that, controlling for the known influences of pain intensity and child depressive symptoms, parental pain catastrophizing and parental protective responses to child pain each independently predict child school attendance rates and reports of overall school impairment. Parental protectiveness was found to mediate the association between parental cognitions (i.e. parent pain catastrophizing) and child school functioning outcomes. These findings underscore the importance of intervening with parents to foster parental responses to child pain that help children engage and succeed in the school environment despite pain.
Keywords: Chronic pain, Functional disability, Parents, Pediatric Pain, Psychosocial functioning, School functioning
INTRODUCTION
Recent studies robustly demonstrate the impact that parents exert upon children’s chronic pain experience [11,22,37,52]. A burgeoning body of research has explored numerous facets of parental functioning and pain responses [16,18,34,44,49], including but not limited to parents’ beliefs and worries about the child’s pain [11,14], quality of the adolescent-parent relationship [31], and interactional patterns, e.g. the extent to which parents encourage their child’s adaptive or maladaptive pain responses [4,54]. Complex transactional processes appear to link children’s and parents’ emotional, cognitive, and behavioral responses to pain, ultimately influencing the child’s overall functioning [6,39,43,52].
Parental cognitive responses to pain, such as parental pain catastrophizing or exaggerated negative pain appraisals, have received recent attention [12,13,17,48,50]. Goubert and colleagues [11] demonstrated that parent pain catastrophizing influences both parents’ emotional reactions to pain and child functional disability. Recent work further clarifies these associations [3], supporting a mediational pathway from parental pain catastrophizing to parental emotional distress and ultimately to child disability. Parental pain catastrophizing may be an important precursor to more observable parental pain responses and eventually to child outcomes.
Behaviorally, parental protective responses to pain emerge as another key influence on child outcomes. Walker & Zeman [53] introduced the term “illness behavior encouragement” to describe parental protective responses to children’s pain behavior, e.g. increasing attention to pain symptoms or excusing the child from responsibilities. Subsequent studies further illustrated how parental protective responses link to poorer functional outcomes, serving as the proximal link between parents’ internal reactions (e.g. cognitions, emotional distress) and child outcomes [26,38,42,52]. These findings suggest a pathway from parental cognitions to parental behavioral pain responses to child functional outcomes.
To date, studies of parental responses to pain define child functional outcomes broadly, despite evidence that predictors of pain-related functioning vary across functional domains [9]. Although school impairment is a critical outcome in pediatric pain research [10,32,33,41], few studies focus specifically on this domain. This is a crucial outcome in pediatric pain, given evidence that long-term school impairment places individuals at heightened risk for poorer academic and occupational achievement [2], increased educational costs [8], and development of psychiatric disorders [2]. Studies that include school functioning outcomes [7,11,29] rely on school attendance as the sole indicator of this complex construct. Furthermore, studies have examined only isolated parental variables [7,11,29]. Additional studies must include multiple indicators of school functioning, test models incorporating multiple parent factors, and control for other known influences on pain-related school impairment such as child depressive symptoms [23,31,36].
The current study investigates associations between parental cognitive and behavioral responses to pain and school functioning in children with chronic pain, controlling for pain characteristics and child depressive symptoms. We sought to test whether parental behavioral responses to pain (i.e. protective behaviors) mediate associations between parental catastrophizing and school impairmemt). Specifically we hypothesized that a relation between parental pain catastrophizing and school functioning (assessed by multiple indicators) would be mediated by parental protective responses to pain, with greater parental pain catastrophizing associating with higher parental protectiveness, which in turn links to greater school impairment.
METHODS
Participants
All patients, ages 8–17, who underwent a multidisciplinary pain evaluation at a tertiary pain clinic in a large, urban northeast pediatric hospital between September 2008 and August 2010 were invited to participate along with their accompanying parent. Four hundred and one patients were approached and 350 agreed to participate, resulting in an 87% participation rate.
Procedure
Study measures were collected in the context of the child’s multidisciplinary pain evaluation. Most measures (those assessing pain characteristics, school functioning, child depressive symptoms, and parental protective responses to pain) were administered as part of the standard clinical assessment. Measures of parents’ cognitions related to the child’s pain were completed separately as part of a larger IRB-approved research protocol [45]. Measures administered for clinical purposes were mailed to families prior to the child’s evaluation; families were asked to complete those questionnaires independently and return them on the date of their appointment. If parents or children had not completed these questionnaires upon arrival to their appointment, they were asked to do so prior to the start of the evaluation. Pain ratings were obtained during the psychologist interview. At the clinic visit, eligible parents and children were approached by a research assistant prior to their evaluation. Additional measures were completed at this time, and consent/assent obtained for the use of data from the clinical assessment battery in addition to study-specific measures.
Measures
Parental pain catastrophizing
The Pain Catastrophizing Scale for Parents (PCS-P) [11] is a validated 13 item self-report measure of parents’ negative thinking related to their child’s chronic pain (e.g., “When my child is in pain, I can’t keep it out of my mind.”) The parent version of this measure is based on the widely used adult PCS [11] and has been shown to be psychometrically sound. Total scale scores are used in this study, with higher scores indicating greater levels of catastrophizing. The internal consistency for the total scores in this sample was .90.
Parental protective responses to pain
The Adult Responses to Children’s Symptoms [5] scale assesses parents’ responses to their children’s pain in three subscales; parent protectiveness, minimization of pain, and encouraging and monitoring. For the present study, the 13-item protective responses subscale was used because it represents the pattern of parental pain response that is best supported theoretically and empirically [5,43]. The stem for each item is, “When your child has pain, how often do you …?” Responses are rated on a 5-point scale ranging from “never” (0) to “always” (4), and subscale scores are computed by calculating the mean rating for items on each subscale. Higher scores indicate higher levels of parent protective responses. Examples include: “bring your child special treats or little gifts,” and “Spend more time than usual with your child.” The internal consistency for the protectiveness scale in this sample was .74.
School functioning
Attendance rates. Number of school days missed in the past three months due to pain (including for doctors’ appointments) was obtained by parent report, which has been shown to correlate highly with official school attendance records [33]. Reports of days when the participant arrived to school late or left school early due to pain were incorporated into the count of missed days as half days missed. Raw responses were reduced into a six-point scale with categories representing 0 days missed, 1–5 days missed, 6–10 days missed, 11–20 days missed, 21–35 days missed, and greater than 35 days missed.
Global school functioning. The Pediatric Quality of Life Inventory (PedsQL)[47] school functioning subscale is a five-item measure of school functioning. Items all begin with the stem, “In the past one month, how much of a problem has your child had with…” and response options range from 0, “Never” to 4, “Almost Always.” Example items are “Paying attention in class,” and “Keeping up with schoolwork.” Raw scores are then transformed jnto standard scores on a 0–100 scale with higher score indicating better functioning (less impairment). Both parent- and child-report versions of the measure were included in the study, but child report was added after the study began, resulting in missing data. Given the high correlation between parent and child reports (r = 0.71, p<.001), parent report scores were used in data analyses. Cronbach’s alpha for the five-item subscale was .86.
Other variables included in analyses
Pain intensity
Children provided pain intensity ratings for their average or usual pain using a 0–10 numeric rating scale, a reliable and valid method for obtaining children’s self-report of pain in this age group [51].
Time since pain onset
Length of time since the initial onset of the current pain problem was measured in months based on parent report.
Child depressive symptoms
The Children’s Depression Inventory (CDI) [24,25] is a well validated 27 item self-report measure of children’s depressive symptoms that has been widely used in pediatric pain studies. It is a recommended outcome measure for clinical trials in pediatric chronic pain.
Data analysis
Descriptive statistics were used to characterize the sample and to check that all data met assumptions for use of parametric statistical tests. Bivariate Pearson r correlations were computed among all variables, including potentially relevant demographic variables, to inform the development of multivariate models. Hierarchical linear regression models were developed, with separate models tested for each of the two school functioning outcomes (school days missed and PedsQL school function scores). The extent to which parent protective responses mediated the relations between parent catastrophizing and child school functioning was examined with additional hierarchical multiple regression analyses. Bootstrapping as outlined by Preacher and Hayes [40] was done to test the indirect effects for both mediation models.
RESULTS
Participant characteristics
Child participants were primarily White (92.3%) and female (80.6%), consistent with the population of children with chronic pain seen in this tertiary care clinic setting. Mean age of children was 13.7 years (SD = 2.5). Primary pain diagnoses included neuropathic pain syndromes (e.g. Complex Regional Pain Syndrome; 34.3%), musculoskeletal pain (30.8%), back/neck pain (14.1%), chronic abdominal pain (8.9%), gynecological/genitourinary (5.8%), headache (2.0%) and other pain (e.g., chest, ear; 4.0%). Mothers were the participating parent in 90.5% of cases. Family socioeconomic status (SES) based on the four-factor index of social status [20] ranged from 12 to 66, with a mean of 45.5 (SD = 12.1). Regarding educational status, the majority of mothers (60%) and fathers (58%) had a college degree or above. Within the sample, 19.4% of responding parents reported themselves to be at home full time. The majority of responding parents (81%) were married.
Descriptive findings and preliminary analyses
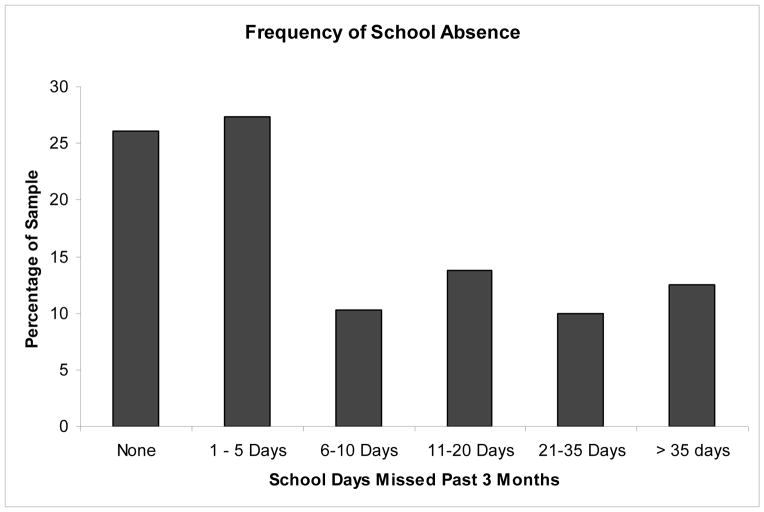
Means and standard deviations for all variables included in analyses are reported in Table 1. Figure 1 depicts frequency of school absences across the sample. Results from bivariate correlational analyses are shown in Table 2. T-tests revealed no differences in school outcomes based on race (White vs. other groups). Boys reported more school days missed than girls (boys’ M=2.4, SD=1.9, girls’ M=1.7, SD = 1.7; F(317) = 2.33, p<.05). Thus, gender was included as a covariate in regression equations testing effects of parental pain responses on school attendance. No gender differences were found on Peds-QL scores. Similarly, there were no gender differences in pain intensity, depression scores, parent pain catastrophizing or parental protective responses to pain. As expected, both pain intensity and depressive symptoms did correlate significantly with school function outcomes (See Table 2). Because time since pain onset did not correlate with any variables of interest, it was not included in subsequent multivariate analyses. A one-way ANOVA revealed no differences on predictor or outcome variable scores across pain diagnoses.
Table 1.
Means and Standard Deviations for Variables
Variable ranges, means and standard deviations
| Variable | Range | Mean (SD) |
|---|---|---|
| Time since pain onset (months) | 1–206 | 24.1 (29.6) |
| Average pain rating | 0–10 | 5.9 (2.1) |
| Child depression (CDI) | 34–81 | 50.1 (10.7) |
| Parental pain catastrophizing (PCS-P) | 5.0 – 52.0 | 26.6 (9.9) |
| Parental protective behavior (ARCS) | 0 – 3.13 | 1.38 (.62) |
| School days missed (previous 3 months) | 0 – 60 | 13.2 (17.7) |
| School functioning (PedsQL-School) | 0–100 | 49.3 (23.9) |
CDI = Childrens Depression Inventory; PCS-P = Pain Catastrophizing Scale; ARCS = Adult Responses to Children’s Symptoms; PedsQL-School = Pediatric Quality of Life Inventory, School Function subscale.
Figure 1.
Reported frequency rates of school absence in the past three months
Table 2.
Bivariate Pearson Correlation Matrix
| Variable | N | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 319 | -- | .12* | .01 | .06 | .06 | .02 | .08 | −.09 |
| 2. Time since pain onset | 318 | -- | −.14** | −.02 | −.05 | −.01 | −.01 | −.02 | |
| 3. Average pain rating | 316 | -- | .22** | .17** | .18** | .17** | −.23** | ||
| 4. Depressive symptoms (CDI) | 310 | -- | .28** | .27** | .27** | −.36** | |||
| 5. Parent pain catastrophizing (PCS-P) | 315 | -- | .41* | .22** | −.30** | ||||
| 6. Parent protective behavior (ARCS) | 302 | -- | .39** | −.54** | |||||
| 7. School days missed | 319 | -- | −.59** | ||||||
| 8. School functioning (PedsQL_School) | 305 | -- |
Correlations are two-tailed.
p<.01;
p<.05
CDI = Childrens Depression Inventory; PCS-P = Pain Catastrophizing Scale; ARCS = Adult Responses to Children’s Symptoms; PedsQL-School = Pediatric Quality of Life Inventory, School Function subscale.
Multivariate regression analyses
Four separate regression equations were tested to examine the effects of parental pain catastrophizing and parental protective responses to pain on school attendance rates and PedsQL school functioning scores. In each analysis, average pain intensity and child depressive symptoms measured on the CDI were entered on the first step of the equation to isolate the effects of the parent factors above and beyond the effects of pain and child depressive symptoms. Results of these four equations are summarized in Table 3. In each of the respective models, parent catastrophizing and protective parent behaviors were significant predictors of school outcomes above and beyond the impact of pain and child depressive symptoms.
Table 3a.
Effects of parental catastrophizing and parent protectiveness on school absence
| Variables | β | Beta | t | R2 Change |
|---|---|---|---|---|
| Model I. (catastrophizing) | ||||
| Step 1 | .12*** | |||
| Child depression | .07 | .28 | 5.00*** | |
| Average pain rating | .10 | .12 | 2.14* | |
| Child gender | .67 | .16 | 2.88** | |
| Step 2 | .02** | |||
| Child depression | .06 | .24 | 4.25*** | |
| Average pain rating | .09 | .10 | 1.85 | |
| Child gender | .65 | .15 | 2.81** | |
| Pain catastrophizing | .02 | .14 | 2.53* | |
| Model II. (protectiveness) | ||||
| Step 1 | .12*** | |||
| Child Depression | .07 | .28 | 4.93*** | |
| Average pain rating | .10 | .12 | 2.11* | |
| Child gender | .67 | .16 | 2.84** | |
| Step 2 | .09*** | |||
| Child depression | .05 | .19 | 3.53*** | |
| Average pain rating | .07 | .08 | 1.53 | |
| Child gender | .58 | .13 | 2.54* | |
| Parental protectiveness | .87 | .31 | 5.74*** | |
P < .05,
P < .01,
P<.001.
To test our second hypothesis regarding a mediating effect of parental protective behaviors on the association between parental pain catastrophizing and school functioning, we conducted two hierarchical linear regression analyses, one for each school functioning outcome. Average pain intensity and child depressive symptoms were entered on the first step to control for these effects. Parental pain catastrophizing was entered on the second step as our independent variable, followed by parental protective behaviors on the final step of the equation as the hypothesized mediator. As described in Baron and Kenny (1986) [1] and Holmbeck (2002) [21], a decrease in the beta weight of the independent variable in the presence of the hypothesized mediator is evidence of a mediated effect. The results are detailed in Table 4. This significance of this effect was further tested using bootstrapping methods. The direct effect of parent catastrophizing on school attendance decreased from β = .14, p < .05 to β = .03, ns after the mediator, parent protectiveness, was entered into the regression equation. The Bootstrap test of the magnitude of this decrease was significant indicating that protectiveness mediated the relation between parent catastrophizing and child school attendance (β = .02, 95% CI .01, .03).
Table 4a.
Hierarchical linear regression model depicting the mediating effect of parent protective responses to pain on the relation between parent pain catastrophizing and child school attendance rates
| Variables | β | Beta | t | R2 Change |
|---|---|---|---|---|
| Step 1 | .12*** | |||
| Child depression | .07 | .28 | 4.93*** | |
| Average pain rating | .10 | .12 | 2.11* | |
| Gender | .67 | .16 | 2.84** | |
| Step 2 | .02* | |||
| Child depression | .06 | .24 | 4.19*** | |
| Average pain rating | .09 | .10 | 1.83 | |
| Gender | .65 | .15 | 2.77** | |
| Parent pain catastrophizing | .02 | .14 | 2.49* | |
| Step 3 | .07*** | |||
| Child depression | .05 | .19 | 3.36*** | |
| Average pain rating | .07 | .08 | 1.47 | |
| Gender | .57 | .13 | 2.53* | |
| Parent pain catastrophizing | .01 | .04 | 0.67 | |
| Parental protective responses | .83 | .30 | 5.16*** |
P < .05,
P < .01,
P<.001.
The direct effect of parent catastrophizing on PedsQL school functioning decreased from β = .20, p < .01 to β = .05, ns after the mediator, parent protectiveness, was entered into the regression equation. The Bootstrap test of the magnitude of this decrease was significant indicating that protectiveness mediated the relation between parent catastrophizing and PedsQl school functioning (β = −.34, 95% CI −.53, −.21). Finally, we explored a possible mediated effect by removing gender as a covariate and instead adding an interaction term (PCS x gender) to the analysis with school attendance as the outcome variable. However, child gender did not emerge as a statistically significant moderator of this mediational model.
DISCUSSION
This study examined effects of parental cognitive and behavioral responses to pain, specifically parental pain catastrophizing and parental protective behaviors, on school functioning in a clinical sample of children experiencing chronic pain. We sought to test a mediational model wherein the effect of parental pain catastrophizing on school impairment was mediated by parental protective responses to the child’s pain. The results support this hypothesis. Examined separately, parental pain catastrophizing and parental protective responses to child pain each predict school functioning outcomes, both in terms of school attendance rates and more global impressions of overall school functioning. Parent cognitive and behavioral responses to the child’s pain account for significant unique variance in child school functioning above and beyond what is explained by the child’s pain intensity and child depressive symptoms. Testing the proposed mediational pathway indicated that parental pain catrastrophizing exerts an indirect effect on the child’s school functioning that is fully mediated by parents’ protective responses to the child’s pain.
The view that parental responses to the child’s pain influence school attendance and overall school impairment is consistent with the social learning theory framework that is often invoked to explain functional outcomes of pediatric chronic pain. This framework suggests that when certain illness behaviors or pain responses receive social rewards (e.g. increased expressions of parental support or concern, more time with parents), these behavior patterns are maintained and strengthened. Parents who have strong negative thoughts about pain and are extremely protective of their child in pain may be quick to sympathize with pain complaints and to acquiesce to requests to remain home from school due to pain. This pattern may be further reinforced if school absence is experienced as an avoidance of a negative or uncomfortable situation (i.e. being in school with pain). Catastrophizing and protective parents may also be more likely to interpret teachers’ or schools’ responses to their child’s condition as unsympathetic, overly demanding, or disbelieving. Social learning influences on child pain behaviors have been shown to continue to predict pain responses into adulthood [28]. These long term effects underscore the importance of intervening early to help parents respond to children’s pain in ways that encourage adaptive functioning, particularly in the school context where impairment exerts high and sometimes irreversible costs in terms of academic and social development.
The findings of the present study are consistent with other recent studies examining the role of parental responses to children in pain. Goubert (2006) [11] and others [3,42] have expanded our understanding of the chain of influence and the links between parent and child responses to pain, emphasizing that parental emotional distress over the child’s pain shapes parents’ pain-related thoughts and behaviors as well as child responses and functional outcomes. Their work points to the need to respond to parent distress as part of efforts to help parents develop more adaptive responses to child pain. Recent work by Vervoort and colleagues [50] supports a transactional pathway leading from child cognitive responses to pain, to parental behavioral responses to the child’s pain, ultimately resulting in increases in child functional disability. These related models are not necessarily mutually exclusive; it is likely that there are multiple pathways that weave together child and parent responses to pain in various combinations, with further influences exerted by the larger family environment [30] as well as by other systems in which the child is embedded, such as school.
Previous studies have demonstrated associations between parental responses to pain and global functional disability [3,42] and one previous study has linked parental protective behaviors to school absence patterns in children with functional abdominal pain [29]. However, this is the first study to test a pathway from parental thoughts to parental behaviors and ultimately link these to school impairment. Furthermore, this study shows that the effects of parental responses to child’s pain not only apply to school attendance but appear to influence school impairment more broadly, thus adding to the small but growing literature aimed at improving our understanding of how childhood chronic pain impacts the school experience.
The findings of the study have clear clinical relevance. They underscore the importance of assessing parental and family factors in attempts to understand how chronic pain affects school functioning. Many parents who feel overwhelmed by their child’s pain condition may be intimidated by the additional challenges of navigating complex school policies and procedures to advocate for their child’s needs. In some cases, healthcare professionals can intervene in fairly simple ways to help deliver appropriate information to schools and ease parents’ concerns about how their child is viewed and treated in the school setting. In line with recent studies suggesting that parental behaviors and distress are important targets to incorporate in interventions to improve pediatric pain-related functional disability [19,27], these results support the inclusion of parent factors as targets of cognitive-behavioral interventions specifically aimed at reducing school impairment among youth with chronic pain. It is important to note that in this study and previous studies by our group [33], children with chronic pain who are missing extensive amounts of school are a minority within the sample of children seeking care in the tertiary pediatric chronic pain clinic; however, they are an important subset of the clinical population because the extent of their school impairment has strong implications for their long-term functioning [2,8].
Several limitations to the study must be considered. First, parental participation was essentially limited to mothers. In light of several recent studies showing differences in both catastrophizing [17] and parental behavioral responses [50] between mothers and fathers and suggesting differential influences on child outcomes, future studies must examine the role of paternal influences on pain-related school impairment. There may also be differential effects by child gender and by specific parent-child dyads (e.g. mother-daughter vs. father-son, etc). However, the over-representation of girls in clinical chronic pain samples is a barrier to fully exploring possible gender effects. There were some limitations to the way in which school attendance data were collected. For example, days missed due to pain were not separated from days missed for doctors’ appointments, and adjustments were not made to attendance rates to account for school vacation times potentially leading to some underestimation of the extent of school absence within the group. Future studies will continue to refine best approaches to collecting school attendance data. The cross-sectional design of the study limits our ability to draw clear conclusions about the causal direction of the relations tested. Although theory supports the assertion that parental cognitions give rise to parental behaviors and that these factors precede and predict child functional outcomes, longitudinal studies are necessary to provide stronger evidence of these claims. This study incorporated several parent factors in an effort to advance our understanding of the interplay among various parent influences on child functioning in the school context, but additional studies encompassing a broader array of parent and family factors and expanding beyond self-report measures of behavior are necessary to develop models comprehensive enough to adequately describe the complexity of family influences on the child pain experience.
This study gives rise to some intriguing directions for future research. The recent development of several validated assessment tools aimed at capturing a range of parental responses to pain, such as parental readiness to adopt a self-management approach to the child’s pain [15], and parental psychological flexibility or pain acceptance [35,46] offer new avenues of inquiry to further clarify the impact of parental responses to child pain upon children’s pain-related school impairment. Although the current study improves upon previous work by expanding the definition of school functioning beyond days absent, school functioning is a complex construct and the effects of chronic pain on school impairment are manifested in numerous, sometimes subtle, ways. Future studies will continue to expand our understanding of this multifaceted outcome domain in the context of pediatric pain. Additionally, the influence of schools’ and teachers’ responses to children with chronic pain are not yet well understood and are an important focus of continued investigation. Merging these lines of inquiry, there may be salient aspects of the parent-school alliance, or lack thereof, that affect a child’s ability to function with pain in school as well. Efforts to ensure that children succeed in the school environment despite pain must involve building strong collaborative relationships among healthcare providers, parents, and schools. Fostering such collaborations may at times be a challenging process but one that goes far toward promoting positive functional outcomes in children facing chronic pain.
Table 3b.
Effects of parental catastrophizing and protectiveness on PedsQL School Function scores
| Variables | β | Beta | t | R2 Change |
|---|---|---|---|---|
| Model I. (Catastrophizing) | ||||
| Step 1 | .16*** | |||
| Child depression | −1.13 | −.34 | −6.45*** | |
| Average pain rating | −1.75 | −.15 | −2.88** | |
| Step 2 | .04*** | |||
| Child depression | −.97 | −.29 | −5.44*** | |
| Average pain rating | −1.48 | −.13 | −2.48 | |
| Pain catastrophizing | −.48 | −.20 | −3.76*** | |
| Model II. (Protectiveness) | ||||
| Step 1 | .16*** | |||
| Child depression | −1.13 | −.34 | −6.43*** | |
| Average pain rating | −1.75 | −.15 | −2.87** | |
| Step 2 | .19*** | |||
| Child depression | −7.37 | −.22 | −4.61*** | |
| Average pain rating | −1.12 | −.10 | −2.08* | |
| Parental protectiveness | −17.86 | −.46 | −9.71*** | |
P < .05,
P < .01,
P<.001.
Table 4b.
Hierarchical linear regression model depicting the mediating effect of parent protective responses to pain on the relation between parent pain catastrophizing and PedsQL school functioning scores.
| Variables | β | Beta | t | R2 Change |
|---|---|---|---|---|
| Step 1 | .16*** | |||
| Child depression | −1.13 | −.34 | −6.43*** | |
| Average pain rating | −1.75 | −.15 | −2.9** | |
| Step 2 | .04*** | |||
| Child depression | −.97 | −.29 | −5.4*** | |
| Average pain rating | −1.5 | −.13 | −2.5* | |
| Parent pain catastrophizing | −4.8 | −.20 | −3.7*** | |
| Step 3 | .16*** | |||
| Child depression | −.71 | −.21 | −4.4*** | |
| Average pain rating | −1.1 | −.09 | −2.0* | |
| Parent pain catastrophizing | −.12 | −.05 | −.88 | |
| Parental protective responses | −17.2 | −.45 | −8.8*** |
P < .05,
P < .01,
P<.001.
Acknowledgments
The study was supported by a Children’s Hospital Boston Career Development Fellowship Award (LS), NIH grant K23HD067202 (LS), The Sara Page Mayo Endowment for Pediatric Pain Research and Treatment, and by the Department of Anesthesiology, Perioperative and Pain Medicine at Children’s Hospital Boston. The authors also wish to thank Lisa Garcia, BA for her valuable research experience.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Personal Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 2.Bernstein GA, Hektner JM, Borchardt CM, McMillan MH. Treatment of school refusal: One-year follow-up. J Am Acad Child Adolesc Psychiatry. 2001;40:206–213. doi: 10.1097/00004583-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Caes L, Vervoort T, Eccleston C, Vandenhende M, Goubert L. Parental catastrophizing about child’s pain and its relationship with activity restriction: The mediating role of parental distress. Pain. 2011;152:212–222. doi: 10.1016/j.pain.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 4.Chambers CTC, Kenneth D, Bennett, Susan MV. The impact of maternal behavior on children’s pain experiences: An experimental analysis. J Pediatr Psychol. 2002;27:293–301. doi: 10.1093/jpepsy/27.3.293. [DOI] [PubMed] [Google Scholar]
- 5.Claar RL, Guite JW, Kaczynski KJ, Logan DE. Factor structure of the Adult Responses to Children’s Symptoms: Validation in children and adolescents with diverse chronic pain conditions. Clin J Pain. 2010;26:410–417. doi: 10.1097/AJP.0b013e3181cf5706. [DOI] [PubMed] [Google Scholar]
- 6.Claar RL, Simons LE, Logan DE. Parental response to children’s pain: The moderating impact of children’s emotional distress on symptoms and disability. Pain. 2008;138:172–179. doi: 10.1016/j.pain.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 7.Dunn-Geier BJ, McGrath PJ, Rourke BP, Latter J, D’Astous J. Adolescent chronic pain: The ability to cope. Pain. 1986;26:23–32. doi: 10.1016/0304-3959(86)90170-3. [DOI] [PubMed] [Google Scholar]
- 8.Evans LD. Functional school refusal subtypes: Anxiety, avoidance, and malingering. Psychol in the Schools. 2000;37:183–191. [Google Scholar]
- 9.Gauntlett-Gilbert J, Eccleston C. Disability in adolescents with chronic pain: Patterns and predictors across different domains of functioning. Pain. 2007;131:132–141. doi: 10.1016/j.pain.2006.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Gorodzinsky AY, Hainsworth KR, Weisman SJ. School functioning and chronic pain: A review of methods and measures. J Pediatr Psychol. 2011;36(9):991–1002. doi: 10.1093/jpepsy/jsr038. [DOI] [PubMed] [Google Scholar]
- 11.Goubert L, Eccleston C, Vervoort T, Jordan A, Crombez G. Parental catastrophizing about their child’s pain. The parent version of the Pain Catastrophizing Scale (PCS-P): A preliminary validation. Pain. 2006;123:254–263. doi: 10.1016/j.pain.2006.02.035. [DOI] [PubMed] [Google Scholar]
- 12.Goubert L, Vervoort T, Cano A, Crombez G. Catastrophizing about their children’s pain is related to higher parent-child congruency in pain ratings: An experimental investigation. Eur J Pain. 2009;13:196–201. doi: 10.1016/j.ejpain.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Goubert L, Vervoort T, Sullivan MJ, Verhoeven K, Crombez G. Parental emotional responses to their child’s pain: The role of dispositional empathy and catastrophizing about their child’s pain. J Pain. 2008;9:272–279. doi: 10.1016/j.jpain.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Guite JW, Logan DE, McCue R, Sherry DD, Rose JB. Parental beliefs and worries regarding adolescent chronic pain. Clin J Pain. 2009;25:223–232. doi: 10.1097/AJP.0b013e31818a7467. [DOI] [PubMed] [Google Scholar]
- 15.Guite JW, Logan DE, Simons LE, Blood EA, Kerns RD. Readiness to change in pediatric chronic pain: Initial validation of adolescent and parent versions of the Pain Stages of Change Questionnaire. Pain. 2011;152(10):2301–11. doi: 10.1016/j.pain.2011.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haraldstad K, Sorum R, Eide H, Natvig GK, Helseth S. Pain in children and adolescents: Prevalence, impact on daily life, and parents’ perception, a school survey. Scand J Caring Sci. 2011;25:27–36. doi: 10.1111/j.1471-6712.2010.00785.x. [DOI] [PubMed] [Google Scholar]
- 17.Hechler T, Vervoort T, Hamann M, Tietze AL, Vocks S, Goubert L, Hermann C, Wager J, Blankenburg M, Schroeder S, Zernikow B. Parental catastrophizing about their child’s chronic pain: Are mothers and fathers different? Eur J Pain. 2011;15:515, e511–519. doi: 10.1016/j.ejpain.2010.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Hermann C, Zohsel K, Hohmeister J, Flor H. Dimensions of pain-related parent behavior: development and psychometric evaluation of a new measure for children and their parents. Pain. 2008;137:689–699. doi: 10.1016/j.pain.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 19.Hicks CL, von Baeyer CL, McGrath PJ. Online psychological treatment for pediatric recurrent pain: A randomized evaluation. J Pediatr Psychol. 2006;31:724–736. doi: 10.1093/jpepsy/jsj065. [DOI] [PubMed] [Google Scholar]
- 20.Hollingshead AB. Four factor index of social status. New Haven, Connecticut: Yale University; 1975. [Google Scholar]
- 21.Holmbeck G. Post-hoc probing of significat moderational and mediational effects in studies of pediatric populations. J Pediatr Psychol. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- 22.Jordan AL, Eccleston C, Osborn M. Being a parent of the adolescent with complex chronic pain: An interpretative phenomenological analysis. Eur J Pain. 2007;11:49–56. doi: 10.1016/j.ejpain.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 23.Kashikar-Zuck S, Goldschneider K, Powers S, Vaught M, Hershey A. Depression and functional disability in chronic pediatric pain. Clin J Pain. 2001;17:341–349. doi: 10.1097/00002508-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Kovacs M. Children’s Depression Inventory. North Tonawanda, NY: Multi-Health Systems; 1992. [Google Scholar]
- 25.Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacol Bull. 1985;21:995–998. [PubMed] [Google Scholar]
- 26.Langer SL, Romano JM, Levy RL, Walker LS, Whitehead WE. Catastrophizing and parental response to child symptom complaints. Child Health Care. 2009;38:169–184. doi: 10.1080/02739610903038750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Feld AD, Ballard SA, Welsh EM, Jeffery RW, Young M, Coffey MJ, Whitehead WE. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol. 2010;105:946–956. doi: 10.1038/ajg.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy RL, Langer SL, Whitehead WE. Social learning contributions to the etiology and treatment of functional abdominal pain and inflammatory bowel disease in children and adults. World J Gastroenterol. 2007;13:2397–2403. doi: 10.3748/wjg.v13.i17.2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Levy RL, Whitehead WE, Walker LS, Von Korff M, Feld AD, Garner M, Christie D. Increased somatic complaints and health-care utilization in children: Effects of parent IBS status and parent response to gastrointestinal symptoms. Am J Gastroenterol. 2004;99:2442–2451. doi: 10.1111/j.1572-0241.2004.40478.x. [DOI] [PubMed] [Google Scholar]
- 30.Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain. 2010;11:1027–1038. doi: 10.1016/j.jpain.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Logan DE, Guite JW, Sherry DD, Rose JB. Adolescent-parent relationships in the context of adolescent chronic pain conditions. Clin J Pain. 2006;22:576–583. doi: 10.1097/01.ajp.0000210900.83096.ca. [DOI] [PubMed] [Google Scholar]
- 32.Logan DE, Simons LE, Kaczynski KJ. School functioning in adolescents with chronic pain: The role of depressive symptoms in school impairment. J Pediatr Psychol. 2009;34(8):882–92. doi: 10.1093/jpepsy/jsn143. [DOI] [PubMed] [Google Scholar]
- 33.Logan DE, Simons LE, Stein MJ, Chastain L. School impairment in adolescents with chronic pain. J Pain. 2008;9:407–416. doi: 10.1016/j.jpain.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 34.Maciver D, Jones D, Nicol M. Parents’ experiences of caring for a child with chronic pain. Qual Health Res. 2010;20:1272–1282. doi: 10.1177/1049732310367499. [DOI] [PubMed] [Google Scholar]
- 35.McCracken LM, Gauntlett-Gilbert J. Role of psychological flexibility in parents of adolescents with chronic pain: Development of a measure and preliminary correlation analyses. Pain. 2011;152:780–785. doi: 10.1016/j.pain.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Palermo TM, Chambers CT. Parent and family factors in pediatric chronic pain and disability: An integrative approach. Pain. 2005;119:1–4. doi: 10.1016/j.pain.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 37.Palermo TM, Eccleston C. Parents of children and adolescents with chronic pain. Pain. 2009;146:15–17. doi: 10.1016/j.pain.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peterson C, Palermo T. Parental reinforcement of recurrent pain: The moderating impact of child depression and anxiety on functional disability. J Pediatr Psychol. 2004;29:331–341. doi: 10.1093/jpepsy/jsh037. [DOI] [PubMed] [Google Scholar]
- 39.Peterson CC, Palermo TM. Parental reinforcement of recurrent pain: the moderating impact of child depression and anxiety on functional disability. J Pediatr Psychol. 2004;29:331–341. doi: 10.1093/jpepsy/jsh037. [DOI] [PubMed] [Google Scholar]
- 40.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 41.Sato AF, Hainsworth KR, Khan KA, Ladwig RJ, Weisman SJ, Davies WH. School absenteeism in pediatric chronic pain: Identifying lessons learned from the general school absenteeism literature. Children’s Health Care. 2007;36:355–372. [Google Scholar]
- 42.Sieberg CB, Williams S, Simons LE. Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatr Psychol. 2011;36:1043–1051. doi: 10.1093/jpepsy/jsr043. [DOI] [PubMed] [Google Scholar]
- 43.Simons LE, Claar RL, Logan DL. Chronic pain in adolescence: Parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol. 2008;33:894–904. doi: 10.1093/jpepsy/jsn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simons LE, Logan DE, Chastain L, Stein M. The relation of social functioning to school impairment among adolescents with chronic pain. Clin J Pain. 2010;26:16–22. doi: 10.1097/AJP.0b013e3181b511c2. [DOI] [PubMed] [Google Scholar]
- 45.Simons LE, Sieberg CB, Carpino E, Logan D, Berde C. The Fear of Pain Questionnaire (FOPQ): assessment of pain-related fear among children and adolescents with chronic pain. J Pain. 2011;12:677–686. doi: 10.1016/j.jpain.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 46.Simons LE, Sieberg CB, Kaczynski KJ. Measuring parent beliefs about child acceptance of pain: a preliminary validation of the Chronic Pain Acceptance Questionnaire, parent report. Pain. 2011;152(10):2294–300. doi: 10.1016/j.pain.2011.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Varni JW, Seid M, Knight TS, Uzark K, Szer IS. The PedsQL 4. 0 Generic Core Scales: Sensitivity, responsiveness, and impact on clinical decision-making. J Behav Med. 2002;25:175–193. doi: 10.1023/a:1014836921812. [DOI] [PubMed] [Google Scholar]
- 48.Vervoort T, Caes L, Crombez G, Koster E, Van Damme S, Dewitte M, Goubert L. Parental catastrophizing about children’s pain and selective attention to varying levels of facial expression of pain in children: A dot-probe study. Pain. 2011;152:1751–1757. doi: 10.1016/j.pain.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 49.Vervoort T, Goubert L, Crombez G. Parental responses to pain in high catastrophizing children: The moderating effect of child attachment. J Pain. 2010;11:755–763. doi: 10.1016/j.jpain.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 50.Vervoort T, Huguet A, Verhoeven K, Goubert L. Mothers’ and fathers’ responses to their child’s pain moderate the relationship between the child’s pain catastrophizing and disability. Pain. 2011;152:786–793. doi: 10.1016/j.pain.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 51.von Baeyer CL. Numerical rating scale for self-report of pain intensity in children and adolescents: recent progress and further questions. Eur J Pain. 2009;13:1005–1007. doi: 10.1016/j.ejpain.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 52.Vowles KE, Cohen LL, McCracken LM, Eccleston C. Disentangling the complex relations among caregiver and adolescent responses to adolescent chronic pain. Pain. 2010;151:680–686. doi: 10.1016/j.pain.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 53.Walker LS, Zeman JL. Parental response to child illness behavior. J Pediatr Psychol. 1992;17:49–71. doi: 10.1093/jpepsy/17.1.49. [DOI] [PubMed] [Google Scholar]
- 54.Williams SE, Blount RL, Walker LS. Children’s pain threat appraisal and catastrophizing moderate the impact of parent verbal behavior on children’s symptom complaints. J Pediatr Psychol. 2011;36:55–63. doi: 10.1093/jpepsy/jsq043. [DOI] [PMC free article] [PubMed] [Google Scholar]