Abstract
Introduction
Sarcoidosis is an incurable, chronic granulomatous disease primarily involving the lungs and lymph nodes of unknown aetiology, treated with non-specific anti-inflammatory/immunosuppressive drugs. Persistently symptomatic patients worsen with a disabling, potentially fatal clinical course. To determine a possible infectious cause, we correlated in a case-control study the clinical information with the presence of bacterial DNA in sarcoidosis mediastinal lymph nodes compared with control lymph nodes resected during cancer surgery.
Methods
We retrospectively studied formalin-fixed, paraffin-embedded, mediastinal lymph nodes from 30 patients with sarcoidosis and 30 control patients with lung cancer. Nucleic acids were extracted from nodes, evaluated by ribosomal RNA PCR for bacterial 16S ribosomal DNA and the results were sequenced and compared with a bacterial sequence library. Clinical information was correlated.
Results
11/30 (36.7%) of lymph nodes from patients with sarcoidosis had detectable bacterial DNA, significantly more than control patient lymph nodes (2/30, 6.7%), p=0.00516. At presentation, 19/30 (63.3%) patients with sarcoidosis were symptomatic including all patients with detectable bacterial DNA. Radiographically, there were 18 stage I and 12 stage II patients. All stage II patients were symptomatic and 75% had PCR-detectable bacteria. After a mean follow-up of 52.8±32.8 months, all patients with PCR-detectable bacteria in this series were persistently symptomatic requiring treatment.
Discussion
36.6% of patients with sarcoidosis had detectable bacterial DNA on presentation, all of these patients were quite symptomatic and most were radiographically advanced stage II. These findings suggest that bacterial DNA-positive, symptomatic patients have more aggressive sarcoidosis that persists long term and might benefit from antimicrobial treatment directed against this presumed chronic granulomatous infection.
Keywords: BACTERIOLOGY, MICROBIOLOGY
Strengths and limitations of this study.
Although a number of prior studies have demonstrated the consistent presence of bacterial DNA (mostly atypical mycobacteria and Propionibacterium acnes) in sarcoidosis tissue, the current study is the first to correlate clinical outcomes with the presence of detectable bacterial DNA, suggesting the most promising candidates for treatment.
Nevertheless, the molecular approach to bacterial detection has distinct limitations including possible false-positive results secondary to contaminated PCR reagents, the paraffin embedding process or postembedding handling and processing of the paraffin block. Also, the mere physical presence of the bacterial DNA in the lymph nodes does not prove that the disease is caused by the microorganism.
In addition, the number of lymph nodes positive for bacterial DNA may be significantly underestimated because of the tendency of the formalin-fixation and paraffin-embedding process to breakdown prokaryotic DNA.
Introduction
Sarcoidosis is a multisystem, granulomatous disease whose aetiology is obscure and controversial. Nevertheless, the condition is relatively common with a significantly higher age-adjusted annual incidence in African-Americans (35.5 cases/100 000) versus Caucasian-Americans (10.9 cases/100 000). An estimated one million people in the USA have this disease. Based on the current US population of 315 556 000, there will be approximately 38 605 new cases of sarcoidosis this year and just over 1000 (2.6%) will die of the illness.1 2
The fundamental pathological abnormality in the disease is the formation of non-caseating epithelioid granulomas, which usually confine poorly soluble foreign material that simply cannot be removed by a single phagocytic cell. The key feature in sarcoidosis is activated CD4 T cells which differentiate into type 1 helper T cells, secreting interleukin 2 and interferon γ, augmenting macrophage tumour necrosis factor-α and amplifying the local cellular immune response.3 4 This granulomatous inflammation interferes with local tissue homeostasis leading to organ impairment.
Since sarcoidosis primarily involves the lungs, eyes and skin, attention has focused on airborne environmental antigens that might trigger this presumed hypersensitivity response with its T cell-mediated cellular immune response.3 Similar granulomatous responses can be seen from a variety of infectious agents including mycobacteria, parasites (schistosoma) and fungi (coccidiomycosis). Early studies reported associations with non-infective agents including beryllium, zirconium, aluminium, wood-burning stoves, tree pollen, clay soil, talc, insecticides, inorganic particles and moldy environments, but none of these theoretical causes has endured.3 5 6 There is also a several-fold increased incidence of sarcoidosis occurring in siblings and parents, as well as a consistent strong association with specific gene products such as class I and class II human leukocyte antigens, which may add to the familial connection.
Although no infectious agent has been cultured directly from sarcoidosis tissues, clinical and immunological characteristics of the disorder provide the strongest support for a microbial aetiology, at least in some patients.5–7 To explore a possible infectious cause in patients seen at the Moffitt Cancer Center, we correlated the clinical presentation and long-term follow-up of patients with sarcoidosis with the presence of bacterial DNA in archived, surgically resected mediastinal lymph nodes. Results from sarcoidosis nodes were compared with control lymph nodes resected at the time of lung surgery in node-negative, stage I non-small cell lung cancer patients.
Methods
Regulatory oversight
Tissue and clinical data in this case–control study was obtained after approval by the Moffitt Cancer Center Scientific Review Committee Protocol MCC #16131 and the University of South Florida IRB Protocol #108656.
Study design
By searching the Moffitt Cancer Center surgical pathology database between 1 January 2000 and 1 April 2010, we retrospectively identified 30 randomly chosen patients who were diagnosed with sarcoidosis based on the typical radiographic and clinical presentation, and the histological finding of non-caseating epithelioid granulomata in lymph nodes obtained sterilely only by mediastinoscopy, to avoid possible microorganism contamination by endoscopic biopsies. Special stains for microorganisms were negative on the specimens. For inclusion in this group, the following criteria were used to make the diagnosis of sarcoidosis: (1) chest radiograph and chest CT findings of symmetrical mediastinal and hilar adenopathy with or without reticulonodular infiltrates in the lung fields (see figure 1); (2) positron emission tomography (PET) scans demonstrated glucose avidity in the enlarged lymph nodes (see figure 2); (3) asymptomatic presentation or typical symptoms of dyspnoea, cough, chest tightness/pain, night sweats, fevers, fatigue, malaise, skin rash or weight loss; (4) lymph nodes showing histological features of confluent, non-caseating granulomata and (5) any known microorganism causes of granulomata were excluded by history or culture. All histopathological specimens were reviewed by one of the authors (PS) to reconfirm the diagnosis made originally by departmental pathologists at Moffitt.
Figure 1.
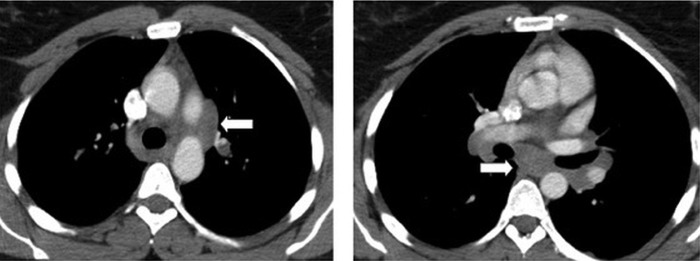
Contrast-enhanced chest CT at two different axial levels showing typical symmetrical hilar and mediastinal adenopathy.
Figure 2.

Positron emission tomography/CT (coronal view) of symmetrical hypermetabolic mediastinal and hilar lymph nodes (arrows).
To insure sterile collection, all control specimens were taken from lymph nodes removed at open thoracotomy by one of the authors (LAR) in 30 (1:1 match with cases) randomly chosen patients with stage IA non-small lung cancer. Lymph nodes were selected only from patients with small peripheral tumours, no obstructive atelectasis and no evidence of active infection. One of the authors (PS) reviewed all control lymph node histology to verify whether there were any metastases, acute inflammation or granulomata.
Clinical data
The clinical data on the patient demographics, initial presenting symptoms and objective findings were extracted from the electronic medical record on all patients with sarcoidosis by one of the authors (LAR). Patients were staged using the modified Scadding radiographic staging system: stage 0 normal chest X-ray; stage 1 hilar and mediastinal adenopathy alone; stage 2 adenopathy and pulmonary infiltrates; stage 3 pulmonary infiltrates alone and stage 4 pulmonary fibrosis.4 Long-term follow-up clinical status and subsequent treatment regimens for all patients with sarcoidosis were obtained from the electronic medical record and telephone calls placed to the patients or their immediate family.
DNA extraction
De-identified, formalin-fixed, paraffin-embedded blocks of lymph nodes from sarcoidosis and control patients were sent to the Departments of Laboratory Medicine and Microbiology at the University of Washington (Seattle, Washington, USA), where investigators were blinded as to the identity of the specimens. The DNA extraction from paraffin-embedded blocks was performed after paraffin was removed by incubation in xylene using the Roche HighPure PCR template purification kit (Roche Diagnostics GmbH, Mannheim, Germany).8 Several negative patient samples (unrelated to the present study) were included in each batch to rule out any contamination. Inhibition was ruled out by checking the ability of exogenously added target DNA to be amplified in the same PCR mix that contained DNA extracted from clinical specimen. Mycobacterium tuberculosis and Bartonella henselae have been detected multiple times in the past using these PCR assays. 16S primers used were of broad range for all bacteria. hsp65 and rpoB were of broad range for Mycobacteria spp only. 16S PCR detected non-Mycobacterium spp DNA such as Propionibacterium acnes. Mycobacterium spp DNA were detected by hsp65 and/or rpoB primers. Primers used for amplification were also used for amplicon sequencing. The PCR amplicon was directly sequenced; no cloning was performed. Mixed infection was not detected in this set of specimens. For alignment, BLASTN was used. Identification was based on exact match on all cases. No sequence that could not be linked to a microbe was detected.
P acnes was detected by 16S primers and Mycobacterium avium was detected by hsp65 primers. M avium was detected and identified by sequence analysis.
PCR analysis for 16S ribosomal DNA, heat shock protein 65 (hsp65), RNA polymerase subunit (rpoB)
The 16S gene fragment was amplified as previously described.8 The hsp65 gene was amplified using TB11 and TB12 primers, and the RNA polymerase subunit gene (rpoB) was amplified using MF and MR primers.9 The amplified products were then sequenced using the Big Dye Sequencing kit (Applied Biosystems, Foster City, California, USA) as per the vendor's recommended protocol. The sequences of two strands were assembled into double-stranded contig using Sequencher software (Gene Codes, Ann Arbor, Michigan, USA). The final sequences were used to search the National Center for Biotechnology Information (National Institutes of Health) database using the Basic Local Alignment Search Tool (BLAST) to identify the amplified DNA.
Quantitative variables
The primary variable to be compared between the sarcoidosis and controls patients is the number of patients in each group with bacterial DNA found in lymph nodes. The N-1 Two Proportion test for comparing independent proportions for small sample size is used to compare the results between the two groups.10 In addition, ORs with 95% CIs were calculated.11 All numerical data are expressed as the mean±SD.
Results
The demographic and clinical characteristics of the 30 sarcoidosis study patients are found in table 1.
Table 1.
Sarcoidosis patient results
| No. | Age/sex | Race | X-ray stage | Pack-year smoking | Prior ca | Chemo | PCR result on lymph nodes | Initial symptoms (year) | Follow-up (months) | Current status (long term) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41/F | AA | I | 7 | Uterine | No | Mycobacterium chelonae | Yes (2009) | 36 | Sympt, alive |
| 2 | 63/F | C | II | 20 | Breast | Yes | M chelonae | Yes (2008) | 12 | Sympt, deceased from COPD 2009 |
| 3 | 64/F | C | II | None | None | No | Mycobacterium mucogenicum | Yes (2008) | 41 | Sympt, alive |
| 4 | 43/M | C | I | None | Melanoma | No | Negative | No (2009) | 31 | Asympt, alive |
| 5 | 61/F | C | I | None | Synovial cell sarcoma | Yes | Negative | No (2009) | 23 | Asympt; new endometrial. ca, alive |
| 6 | 39/M | C | II | 5 | None | No | Proprionibacterium acnes | Yes (2008) | 35 | Sympt, alive |
| 7 | 58/M | C | I | 3 | Tonsil cancer | Yes | Corynebacterium propinquum | Yes (2006) | 65 | Sympt; tonsil ca. relapse, alive |
| 8 | 54/M | C | II | None | None | No | P acnes | Yes (2006) | 60 | Sympt, alive |
| 9 | 52/F | AA | I | 6 | None | No | Negative | Yes (2007) | 58 | Sympt, alive |
| 10 | 53/F | C | I | 5 | Melanoma | Yes | Negative | No (2007) | 53 | Asympt, alive |
| 11 | 34/M | AA | II | None | None | No | P acnes | Yes (2007) | 53 | Sympt, alive |
| 12 | 40/M | C | I | Cigars | None | No | Negative | Yes (2007) | 36 | Sympt, alive |
| 13 | 49/M | AA | II | None | None | No | Duganella zoogloeoides | Yes (2010) | Lost | Unknown, alive |
| 14 | 57/F | AA | II | 5 | Breast | Yes | P acnes | Yes (2000) | 136 | Sympt; breast ca relapse; polymyalgia rheumatica; Hashimoto's thyroiditis, alive |
| 15 | 67/M | C | I | None | None | No | Negative | No (2001) | Lost | Unknown, alive |
| 16 | 30/M | H | I | None | None | No | Negative | No (2001) | Lost | Unknown, alive |
| 17 | 75/F | C | I | None | Ovarian | Yes | Negative | No (2002) | 36 | Asympt, deceased from ca, 2005 |
| 18 | 67/F | C | I | 50 | Liposarcoma | No | Negative | No (2003) | 106 | Sympt, alive |
| 19 | 60/F | C | I | None | Nerve sheath tumour | No | Negative | No (2003) | 60 | Asympt, deceased unknown cause 2008 |
| 20 | 41/F | C | I | None | None | No | Negative | No (2005) | 78 | Asympt, alive |
| 21 | 50/F | C | I | None | None | No | Negative | Yes (2005) | 73 | Asympt, alive |
| 22 | 48/F | C | I | None | Breast | Yes | P acnes | Yes (2003) | 24 | Sympt; deceased from ca 2005 |
| 23 | 41/F | C | II | None | Adrenal ca; melanoma | Yes | Negative | Yes (2006) | 4 | Deceased from ca 2007 |
| 24 | 35/M | H | I | 2.5 | None | No | Negative | Yes (2006) | 24 | Asympt, alive |
| 25 | 32/M | C | I | 1.0 | None | No | Negative | No (2006) | Lost | Unknown, alive |
| 26 | 37/M | C | II | 15 | Hodgkin's disease | Yes | P acnes | Yes (2007) | 66 | Sympt, alive |
| 27 | 51/F | AA | II | None | None | No | Negative | No (2007) | 64 | Sympt; (mildly), alive |
| 28 | 56/F | C | II | None | Colon ca | Yes | Negative | No (2008) | Lost | Unknown, alive |
| 29 | 33/M | C | I | 5 | Melanoma | No | Negative | No (2009) | 38 | Asympt, alive |
| 30 | 52/F | H | II | 1 | Uterine | No | Negative | Yes (2002) | 48 | Asympt, alive |
All patients positive on PCR for microorganism DNA in lymph nodes are shown in italic type.
AA, African-American; asympt., asymptomatic; C, Caucasian; Ca, cancer; Chemo, chemotherapy; COPD, chronic obstructive pulmonary disease; F, female; H, Hispanic; M, male; Sympt, symptomatic.
Demographics
Patient ages are mean 52.5±12.3 years (median 53 years, range 30–75 years). The male:female ratio is 14:16. The ethnicity includes Caucasian 73.3% (22), African-American 16.7% (5) and Hispanic 10% (3). Most of the patients were overweight: mean body mass index is 31.4±6.9, median 28.5 and range 18.8–47.3.
Clinical presentation
At the time of initial presentation, 19 of 30 patients (63.3%) were symptomatic, usually with multiple symptoms. Of these 19 patients, the duration of symptoms before diagnosis was a mean of 22.1±30.0 months (median 12 months, range 1–120 months). The most common symptoms were night sweats 9 (30.0%), dyspnoea 8 (26.7%), chest pain 7 (23.3%), chest tightness 5 (16.7), fevers 3 (10.0%), fatigue 3 (10%), skin rash 2 (6.7%) and stomach ulcer 2 (6.7%). Other symptoms present in at least one patient include dyspepsia, dysphagia, diarrhoea, constipation, kidney stones, joint and muscle pains, orthopnoea, nose and mouth skin lesions, intermittent bronchospasm, malaise and weight loss.
Comorbidities include asthma 2 (6.7%), coronary artery disease 2 (6.7%), diabetes mellitus 4 (13.3%) and hypertension 5 (16.6), and one each of gout, hypothyroidism, eczema, fibromyalgia and Crohn's disease. Malignancies were extremely common with over half (53.3%) having a current or prior tumour, a finding noted previously by others.12 The malignancies prior to or at the time of presentation are breast 3, melanoma 3, uterine 2, sarcomas 3, tonsil 1, ovary 1, adrenal 1, colon 1 and Hodgkin's lymphoma 1.
Radiographic studies
Chest CT was performed on all 30 patients and all had symmetrical mediastinal and hilar adenopathy. Four of 30 patients (13.3%) had obvious abdominal adenopathy. Lung nodules were present in 12 patients (40%) and were radiographic stage II sarcoidosis. The other 18 patients (60%) had stage I disease. All 12 stage II patients were symptomatic. PET/CT scans were performed in 25 of 30 patients with sarcoidosis. All patients demonstrated glucose avidity in the enlarged mediastinal and hilar nodes (see figure 2 for typical example), and glucose avidity was seen in the abnormal abdominal nodes in the four patients with radiographic adenopathy below the diaphragm.
Laboratory results
Twelve of 30 patients had lymph node tissue sent at the time of mediastinoscopy for aerobic, fungal and mycobacterial cultures. All cultures showed no growth after 6 weeks of incubation.
Bacterial DNA detected by PCR
Eleven of 30 lymph nodes (36.7%) in patients with sarcoidosis had bacterial DNA present by PCR. Only 2 of 30 (6.7%) control patients were found to have bacterial DNA in their lymph nodes. The microorganisms present in each group are shown in table 2. There are significantly more patient with sarcoidosis lymph nodes positive for microorganism DNA than control lymph nodes: 11/30 versus 2/30, p=0.00516 (2-tailed p value); OR is 8.1053 with 95% CIs 1.6115 to 40.7675, p=0.0111.
Table 2.
Bacterial DNA detected by PCR
| Sarcoidosis (11/30) | Control (2/30) |
|---|---|
| Propionibacterium acnes: 7 | Mycobacterium avium: 1 |
| Mycobacterium | Propionibacterium acnes: 1 |
| Chelonae: 2 | |
| Mucogenicum: 1 | |
| Duganella zoogloeoides: 1 | |
| Corynebacterium propinquum: 1 |
All patients with sarcoidosis with detectable bacterial DNA in lymph nodes (36.7%) were symptomatic at presentation. In addition, 73% (8/11) of bacterial DNA-positive patients with sarcoidosis were symptomatic at presentation and had radiographic stage II disease.
Long-term follow-up
Long-term follow-up was complete in 25 of 30 (83.3%) patients with sarcoidosis, for a mean follow-up of 50.4±28.2 months (median 48 months, range 4–132 months). Five of these patients are deceased: three from cancers, one from chronic obstructive pulmonary disease and one from unknown causes. The other five patients lost to direct follow-up are still living based on information obtained from the Social Security Death Index.13
Of the 10 patients with sarcoidosis with bacterial DNA found in their lymph nodes in this series in whom long-term follow-up was available, all were symptomatic at a mean follow-up of 52.8±32.4 months (median 47 months, range 12–136 months). The one additional bacterial DNA-positive patient was lost to follow-up.
Discussion
The objectives of this case–control study were twofold: (1) to evaluate sterilely resected lymph nodes in documented patients with sarcoidosis for the presence of bacterial DNA by molecular methods and (2) to correlate the results with clinical characteristics of the patients.
Bacterial DNA
As expected, our molecular testing using PCR demonstrated that over one-third of patients with sarcoidosis (36.7%) had evidence of bacterial DNA in the nodes, indicating either the past or the current involvement with these microorganisms. This percentage of bacterial DNA-positive specimens falls in the range found in numerous prior published studies from the past two decades (using various methodologies), which range from 26% to 80% positive (table 35 7 14–17). Furthermore, atypical mycobacteria and P acnes represented almost all DNA identified, also consistent with the findings of the multiple prior studies (table 3). Additionally identified were one skin and mucous membrane organism (Corynebacterium propinquum), and one aerobic Gram-negative bacillus (Duganella zoogloeoides) that is usually found in aqueous environments. Interestingly, the latter patient (no. 13) with D zoogloeoides was an asbestos technician originally from tropical Haiti. As a disclaimer, just the finding of DNA from a microorganism in lymph nodes does not tell us whether the viable organism is present or whether it caused the granulomatous reaction.
Table 3.
Selected studies of DNA of infectious agents found in sarcoidosis tissues
| Author (year) | Sarcoid tissue (number of patients) | Technique | Organisms (%) | Number of controls (% organisms) |
|---|---|---|---|---|
| Li (1999)14 | Skin (20) | PCR (restriction enzyme pattern) | Mycobacteria (2 tuberculosis, 14 other Mycobacteria) (80 total positive) | 20 normals (0 organisms) |
| Du Bois (2003)7 (Review of pre-1999 studies) | Lymph nodes (12 studies with 295 patients) | PCR (various methods) | Mycobacterium spp (34) | Various |
| Eishi (2002)15 (5 centre study) | Lymph nodes (108) | Quantitative real-time PCR |
Propionibacterium acnes (72) Propionibacterium granulosum (55) Mycobacterium tuberculosis (4) Escherichia coli (2) |
86 normals (29 P acnes, 12 P granulosum, 2 M tuberculosis) |
| Drake (2002)16 | Lymph nodes (25) | Nested PCR | Mycobacterium spp (60) | 25 normals (0) |
| Gupta (2007)5 (meta-analysis) | Various (31 studies with 874 patients | PCR (various methods) | Mycobacterium spp (26) | 745 controls (3) |
| Ichikawa (2008)17 | Bronchoalveolar lavage (42) | Quantitative PCR | Propionibacterium spp (3X higher genome levels vs controls) | 30 controls (low levels same genome) |
Similar to prior published studies summarised in table 3, significantly less (only 2 of 30 or 6.7%, p=0.00516) of control lymph nodes resected at the time of lung cancer surgery showed evidence of bacterial DNA (M avium and P acnes). This difference strongly suggests that the demonstration of bacterial DNA in sarcoidosis lymph nodes is a real finding in our study (and in over 35 prior published studies) and they are not just processing contaminants, therefore pointing to microorganisms as potential contributors to the genesis of this disease. In addition, P acnes DNA was found in only 1 of 30 (3.3%) control lymph nodes in our study, in stark contrast to Ishige et al18 in Japan who reported this microorganism as an ubiquitous pulmonary lymph node commensal found in 8 of 11 (72.7%) non-sarcoid patients in their study. Such a very high positive result in their study is likely due to either geographical/ethnic/racial differences or potential contamination in processing.
Clinical characteristics
Perhaps the most intriguing findings came from correlation of the PCR findings with the clinical information. All patients with lymph nodes containing bacterial DNA on presentation were also highly symptomatic and 75% of them had the poorer-prognosis radiographic stage II findings. Moreover, after a median 4 years follow-up, all bacterial DNA-positive patients were still highly symptomatic. This striking correlation strongly suggests that demonstration of bacterial DNA by PCR in lymph nodes on initial presentation is an adverse prognostic factor and makes it unlikely that these patients will have a spontaneous remission.
Indeed, if infection with one of these microorganisms triggers an exuberant granulomatous immune response, the 50–80% of patients who usually have a spontaneous remission1 likely clear the offending organism and the immune reaction subsides. We postulate that those patients who have persisting symptomatic disease likely continue to harbour the microorganism, which perpetuates the vigorous, destructive immune response as well as permit the microorganism to travel elsewhere to other organs to create distant granulomatous inflammation.
Limitations of this study
Many pathogenic microorganisms such as Mycobacterium leprae (leprosy) or coronaviruses (severe acute respiratory syndrome) cannot be grown directly in culture or they are very slow growing or difficult to culture such as Tropheryma whippelii (Whipple's disease).5 19 In these instances, detection and identification rely on molecular mechanisms such as PCR used in this study. Nevertheless, the molecular approach has distinct limitations including possible false-positive results secondary to contaminated PCR reagents, the paraffin embedding process or postembedding handling and processing of the paraffin block. However, in our study, 30 control lymph nodes were processed in an identical manner and bacterial DNA was detected in only 2/30 (6.6%), significantly less than the sarcoidosis nodes (36.7%, p=0.00516), suggesting that contamination is unlikely to account for the findings.
Another obvious limitation in interpreting the results of this and other prior molecular studies relates to colonisation versus causation. Just the finding of microbial DNA in the nodes does not prove that the organism is actively involved in the pathogenesis of the disease. The microorganism may just be a commensal or theoretically it might even be attracted to the area of granulomatous inflammation. Nevertheless, the marked difference in the percentage of microbial DNA-positive nodes in sarcoidosis versus control patients is certainly suggestive of disease causation by the microorganisms.
In addition, the number of lymph nodes positive for bacterial DNA may be significantly underestimated because of the tendency of the formalin-fixation and paraffin embedding process to breakdown prokaryotic DNA. Over time other investigators have found degradation of the prokaryotic bacterial DNA (especially mycobacteria) with ageing of the paraffin-embedded specimens.16 Of note, the only three sarcoidosis lymph nodes positive for mycobacteria in our study were less than 3 years old when evaluated by PCR. Had we used fresh lymph node tissue like Drake et al16 who found 60% PCR positive for mycobacteria spp, there may have been a much higher rate of positive bacterial DNA results (particularly mycobacteria) in our study.
Implications of the study
Sarcoidosis is a granulomatous disease primarily involving the lungs, lymph nodes and other organs that appears to be the result of an exuberant T cell and macrophage immunological response to the continued presentation of a poorly degradable antigen. Numerous non-infective agents have been implicated based on epidemiological studies but none have stood up to scrutiny.1 3 5 The focus over the past two decades has been on infective agents that might trigger sarcoidosis, with the strongest suspects found in the mycobacteria family and the common commensal P acnes. And like classical tuberculosis where up to 90% of people infected with M tuberculosis remain in remission without treatment,20 sarcoidosis also has a 65–80% spontaneous remission rate without treatment.1 One may speculate that similar to tuberculosis, the immune system, after its initial response to a triggering microorganism, is successful in eradicating the agent and the immune response subsides. Then in the 20% or so with persistent and progressive sarcoidosis, the organism remains viable and perpetuates the destructive immune response.
Symptomatic sarcoidosis is usually treated with various anti-inflammatory and immunosuppressive agents such as corticosteroids, methotrexate and TNF-inhibitors (biologics).21 The similarities in immunological abnormalities and treatment to another debilitating granulomatous disease, Crohn's disease, are striking.22 Granulomatous ileitis (Crohn's) has been suspected by many investigators to be the result of a chronic infection with the obligate intracellular microorganism M avium subspecies paratuberculosis (MAP) that is known to cause a granulomatous ileitis in cattle and other ruminants called Johne's disease.23 Although the classical treatment of Crohn's disease has been with immunosuppressive agents just like with sarcoidosis, many recent studies suggest a much more effective treatment with less side effects may be a triple antibiotic regimen geared towards the putative triggering agent MAP.24–26 In fact, many in the field suspect that this intracellular organism (MAP) that resides in the macrophage impairs the normal autophagy that would usually eradicate the organism.24 Agents that enhance autophagy such as 16α-bromoepiandersterone,27 28 currently in human trials, may prove effective along with antibiotics in Crohn's disease.24
Can some antibacterial/antimycobacterial regimen such as that used in Crohn's disease alter the natural history of sarcoidosis in chronically symptomatic patients? Sixty years ago a number of small trials using classical antituberculous drugs (isoniazid, streptomycin or cortisone) were published with discouraging results.29 However, atypical mycobacteria (rather than M tuberculosis) that are more likely to be one of the aetiological agents in sarcoidosis are almost all resistant to the standard antituberculosis agents such as isoniazid.30–35 And if other organisms such as P acnes or perhaps cell-wall deficient (L-forms) bacteria trigger and perpetuate sarcoidosis in some individuals, then the standard antituberculous drugs would also be ineffective.
The tetracycline derivatives (minocycline and doxycycline) as well as the antimalarial drug chloroquine have been shown to be quite effective in treating cutaneous sarcoidosis.36 Minocycline can produce complete responses in two-thirds of cases, although it is debated whether this is an antimicrobial effect or an immunomodulating effect.37
Attention has recently turned to randomised sarcoidosis treatment trials with various antimicrobial agents. Drake et al38 just published positive results of the first randomised trial (NCT01074554) of an antimicrobial regimen (directed at atypical mycobacteria) in the USA using oral concomitant levofloxacin, ethambutol, azithromycin and rifampin (CLEAR) regimen to treat 30 patients with cutaneous sarcoidosis, with quite significant reductions in cutaneous lesion size. Gupta et al39 in their comprehensive review of sarcoidosis and its similarities to tuberculosis present a convincing case for antituberculous treatment of sarcoidosis. Gupta is also the principal investigator in an ongoing clinical trial in India using more standard antituberculous therapy “Rifampicin and Isoniazid Along With Prednisolone Compared to Prednisolone Alone in Treatment of Sarcoidosis: a Pilot Randomized Controlled Trial” (ClinicalTrials.gov Identifier: NCT01245036).40 The results of this trial in India with its high burden of tuberculosis will be available next year, though the drug regimen used may not be as effective in countries with a low tuberculosis burden. If indeed sarcoidosis arises from an abnormal immunological response to a microorganism(s), the patient's geographical location may dictate which microorganism is involved and what antimicrobial regimen will be most effective.
Conclusions
Over the past three decades or more, numerous studies have examined every aspect of sarcoidosis including its dysfunctional immune response. The primary therapy is immune suppression in various forms but this treats only symptoms and does not seem to alter the natural history of the disease.4 21 Dozens of studies (table 3) have repeatedly demonstrated evidence of microorganisms in 30–80% of sarcoidosis tissues, mostly various mycobacteria and P acnes and more of these molecular studies are not likely warranted.
Perhaps we should follow the lead of the Crohn's disease gastroenterologists24 25 and proceed with a therapeutic clinical trial using a regimen of multiple antibiotics in patients with persistently symptomatic, advanced-stage sarcoidosis. Indeed, if there is a persistent, viable microorganism infection causing the continuing or progressive debilitating symptoms and organ failure, antibiotics might favourably impact the course of this disease.
Supplementary Material
Footnotes
Contributors: LAR had full access to all of the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis; he also contributed to the conception, hypotheses delineation and design of the study; data acquisition, analysis and interpretation, and writing and revision of the article prior to submission. PS contributed to the conception, hypothesis delineation, and design of the study; data acquisition, analysis and interpretation; and revision of the article prior to publication. DJS contributed to the data acquisition, analysis and interpretation; and revision of the article prior to publication. JLP contributed to the data acquisition, analysis and interpretation. RLS contributed to the conception, hypothesis delineation, and design of the study; and revision of the article prior to publication.
Funding: This project was supported by a grant from the W. Paul Hoenle Foundation, Sarasota, Florida 34242, USA.
Competing interests: The material is the result of work supported with resources and use of facilities at the Moffitt Cancer Center (LAR, PS and RLS) and the University of Washington (DJS and JLP). Bacteria were identified by the Molecular Microbiology Laboratory at the University of Washington Medical Center http://depts.washington.edu/molmicdx
Ethics approval: Institutional Review Board, University of South Florida College of Medicine, Tampa, Florida.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Extra data can be accessed via the Dryad data repository at http://datadryad.org/ with the doi:10.5061/dryad.23k48.
References
- 1.American Thoracic Society Statement on sarcoidosis. Am J Respir Crit Care Med 1999;160:736–55 [DOI] [PubMed] [Google Scholar]
- 2.Rybicki BA, Maliarik MJ, Major M, et al. Epidemiology, demographics, and genetics of sarcoidosis. Semin Respir Infect 1998;13:166–73 [PubMed] [Google Scholar]
- 3.Iannuzzi MC, Brybicki BA, Teirstein AS. Sarcoidosis. N Engl J Med 2007;357:2153–65 [DOI] [PubMed] [Google Scholar]
- 4.Baughman RP, Culver DA, Judson MA. A concise review of pulmonary sarcoidosis. Am J Respir Crit Care Med 2011;183:573–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta D, Agarwal R, Aggarwal AN, et al. Molecular evidence for the role of mycobacteria in sarcoidosis: a meta-analysis. Eur Respir J 2007;30:508–16 [DOI] [PubMed] [Google Scholar]
- 6.Newman LS, Rose CS, Bresnitz EA, et al. A case control etiologic study of sarcoidosis. Am J Respir Crit Care Med 2004;170:1324–30 [DOI] [PubMed] [Google Scholar]
- 7.Du Bois RM, Goh N, McGrath D, et al. Is there a role for microorganisms in the pathogenesis of sarcoidosis? J Intern Med 2003;2003:4–17 [DOI] [PubMed] [Google Scholar]
- 8.de Sanctis JT, Carpenter CF, Sims MD, et al. Culture-negative endocarditis and the use of molecular diagnostics. Infect Dis Clin Pract 2010;18:120–3 [Google Scholar]
- 9.Itoh S, Kazumi Y, Abe C, et al. Heterogeneity of RNA polymerase gene (rpoB) sequences of Mycobacterium gordonae clinical isolates identified with a DNA probe kit and by conventional methods. J Clin Microbiol 2003;41:1656–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Measuring Usability: A/B Test Calculator. 2012. http://www.measuringusability.com/ab-calc.php#comments (accessed 7 Apr 2013).
- 11.MedCalc Software http://www.medcalc.org/calc/odds_ratio.php (accessed 29 Oct 2013).
- 12.Asking J GJ, Eklund A, Hillerdal G, et al. Increased risk for cancer following sarcoidosis. Am J Respir Crit Care Med 1999;160:1668.–(5 Pt 1) [DOI] [PubMed] [Google Scholar]
- 13.Social Security Death Index. 2013. http://www.genealogybank.com/gbnk/ssdi/?kbid=9064&m=9 (accessed 7 Apr 2013).
- 14.Li N, Bajoghi A, Kubba A, et al. Identification of mycobacterial DNA in cutaneous lesions of sarcoidosis. J Cutan Pathol 1999;26:271–8 [DOI] [PubMed] [Google Scholar]
- 15.Eishi Y, Suga M, Ishige I, et al. Quantitative analysis of mycobacterial and propionibacterial DNA in lymph nodes of Japanese and European patients with sarcoidosis. J Clin Microbiol 2002;40:198–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Drake WP, Pei Z, Pride DT, et al. Molecular analysis of sarcoidosis tissues for Mycobacterium species DNA. Emerg Infect Dis 2002;8:1334–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ichikawa H, Kataoka M, Hiramatsu J, et al. Quantitative analysis of propionibacterial DNA in bronchoalveolar lavage cells from patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 2008;25:15–20 [PubMed] [Google Scholar]
- 18.Ishige I, Takemura T, Kobayashi L, et al. Propionibacterium acnes is the most common bacterium commensal in peripheral lung tissue and mediastinal lymph nodes from subjects without sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 2005;22:33–42 [PubMed] [Google Scholar]
- 19.Fenollar FBM, Didier R. Culture of Tropheryma whipplei from human samples: a 3-year experience (1999–2002). J Clin Microbiol 2003;41:3816–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rubin EJ. The granuloma in tuberculosis—friend or foe? N Engl J Med 2009;360:2471–3 [DOI] [PubMed] [Google Scholar]
- 21.Iannuzzi MC J.R. F. Sarcoidosis, clinical presentation, immunopathogenesis and therapeutics. J Am Med Assoc 2011;305:391–9 [DOI] [PubMed] [Google Scholar]
- 22.McFadden JJ, Fidler HM. Mycobacteria as possible causes of sarcoidosis and Crohn's disease. J Appl Bacteriol 1996;81:47S–52S [PubMed] [Google Scholar]
- 23.Motiwala AS, Li L, Kapur V, et al. Current understanding of the genetic diversity of Mycobacterium avium subspecies paratuberculosis. Microbes Infect 2006;8:1406–18 [DOI] [PubMed] [Google Scholar]
- 24.Chamberlain W, Borody TJ, Campbell J. Primary treatment of Crohn's disease: combined antibiotics taking center stage. Expert Rev Clin Immunol 2011;7:751–60 [DOI] [PubMed] [Google Scholar]
- 25.Khan KJ, Ullman TA, Ford AC, et al. Antibiotic therapy in inflammatory bowel disease: a systematic review and meta-analysis. Am J Gastroenterol 2011;106:661–73 [DOI] [PubMed] [Google Scholar]
- 26.Das K, Seril DN. Mycobacterium avium subspecies paratuberculosis in Crohn's disease: the puzzle continues. J Clin Immunol 2012;46:627–8 [DOI] [PubMed] [Google Scholar]
- 27.Nicoletti F, Conrad D, Wang A, et al. 16alpha-bromoepiandrosterone (HE2000) limits non-productive inflammation and stimulates immunity in lungs. Clin Exp Immunol 2009;158:308–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stickney DR, Novelijic Z, Garsd A, et al. Safety and efficacy of immune modulator HE2000 on the incidence of tuberculosis and other opportunistic infections in AIDS patients. Antimicrob Agents Chemother 2007;51:2639–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edelson E. Isoniazid in the treatment of sarcoidosis; a preliminary report. J Invest Dermatol 1953;21:71–4 [DOI] [PubMed] [Google Scholar]
- 30.Sahasranaman V, Tucci VT, Vincent AL, et al. The clinical manifestations, diagnosis and treatment of non-tuberculous mycobacteria infections. J Gen Med 2008;20:31–45 [Google Scholar]
- 31.Israel HL, Sones M, Harrell D. Ineffectiveness of isoniazid and iproniazid in therapy of sarcoidosis. Am Rev Tuberc 1953;67:671–3 [DOI] [PubMed] [Google Scholar]
- 32.Holsinger RE, Dalton JE. Isoniazid therapy in cutaneous tuberculosis and sarcoidosis. J Am Med Assoc 1954;154:475–81 [DOI] [PubMed] [Google Scholar]
- 33.Hoyle C, Dawson J, Mather G. Treatment of pulmonary sarcoidosis with streptomycin and cortisone. Lancet 1955;268:638–43 [DOI] [PubMed] [Google Scholar]
- 34.Chatterjee SC, Ghosh JC. Sarcoidosis treated with anti-tuberculous drugs. J Indian Med Assoc 1957;29:61–3 [PubMed] [Google Scholar]
- 35.James DG, Thomson AD. The course of sarcoidosis and its modification with treatment. Lancet 1959;1:1057–61 [DOI] [PubMed] [Google Scholar]
- 36.Lodha S, Sanchez M, Prystowsky S. Sarcoidosis of the skin: a review for the pulmonologist. Chest 2009;136:583–96 [DOI] [PubMed] [Google Scholar]
- 37.Steen TEJ. Oral minocycline in treatment of cutaneous sarcoidosis. JAMA Dermatol 2013;149:758–60 [DOI] [PubMed] [Google Scholar]
- 38.Drake WP, Oswald-Richter K, Richmond BW, et al. Oral antimycobacterial therapy in chronic cutaneous sarcoidosis: a randomized, single-masked, placebo-controlled study. JAMA Dermatol 2013;149:140–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta D, Agarwal R, Aggarwal AN, et al. Sarcoidosis and tuberculosis: the same disease with different manifestations or similar manifestations of different disorders. Curr Opin Pulm Med 2012;18:506–16 [DOI] [PubMed] [Google Scholar]
- 40.Rifampicin and isoniazid along with prednisolone compared to prednisolone alone in treatment of sarcoidosis: a pilot randomized controlled trial. http://clinicaltrials.gov/show/NCT01245036 (accessed 29 Oct 2013).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


