Abstract
Objective
To assess the effect that accreditation training in fetal growth surveillance and evidence-based protocols had on stillbirth rates in England and Wales.
Design
Analysis of mortality data from Office of National Statistics.
Setting
England and Wales, including three National Health Service (NHS) regions (West Midlands, North East and Yorkshire and the Humber) which between 2008 and 2011 implemented training programmes in customised fetal growth assessment.
Population
Live births and stillbirths in England and Wales between 2007 and 2012.
Main outcome measure
Stillbirth.
Results
There was a significant downward trend (p=0.03) in stillbirth rates between 2007 and 2012 in England to 4.81/1000, the lowest rate recorded since adoption of the current stillbirth definition in 1992. This drop was due to downward trends in each of the three English regions with high uptake of accreditation training, and led in turn to the lowest stillbirth rates on record in each of these regions. In contrast, there was no significant change in stillbirth rates in the remaining English regions and Wales, where uptake of training had been low. The three regions responsible for the record drop in national stillbirth rates made up less than a quarter (24.7%) of all births in England. The fall in stillbirth rate was most pronounced in the West Midlands, which had the most intensive training programme, from the preceding average baseline of 5.73/1000 in 2000–2007 to 4.47/1000 in 2012, a 22% drop which is equivalent to 92 fewer deaths a year. Extrapolated to the whole of the UK, this would amount to over 1000 fewer stillbirths each year.
Conclusions
A training and accreditation programme in customised fetal growth assessment with evidence-based protocols was associated with a reduction in stillbirths in high-uptake areas and resulted in a national drop in stillbirth rates to their lowest level in 20 years.
Strengths and limitations of this study.
Analysis of national and regional Office of National Statistics data helped to avoid random variation due to small numbers at unit or Trust level and allowed trends to become apparent.
Only total figures were available but previous regional subgroup analysis was able to pinpoint the downward trend in stillbirth rates as due to fewer deaths with intrauterine growth restriction.
The study was observational but there have been no other regional or national initiatives which could have accounted for the reduction in stillbirths over this period, suggesting that the associations observed were causal.
Introduction
Stillbirth rates in England and Wales have seen a little change in the past 20 years and are the highest in Western Europe.1 Reduction of stillbirths is a government target,2 yet a 2012 survey conducted by The Times suggested that most National Health Service (NHS) Trusts which run maternity units in England have no specific plans in place to reduce stillbirth rates.3
Until recently, two-thirds of stillbirths were categorised as unexplained4 and tended, by implication, to be considered unavoidable.5 However, our understanding has improved with the application of better classification systems and customised birth weight percentiles, which identified that most such ‘unexplained’ stillbirths had preceding intrauterine growth restriction associated with placental pathology.6–8 A 2007 confidential enquiry peer review of case notes of normally formed stillbirths with fetal growth restriction found that 84% had substandard care and were potentially avoidable with better recognition and assessment of intrauterine growth.9 This finding is supported by a recent analysis of the West Midlands maternity database which reported that growth restriction was not only the single strongest risk factor for stillbirth, but that antenatal recognition and timely delivery can lead to significant reduction in risk.10
However, antenatal detection of fetal growth problems has been traditionally poor in the NHS, with published reports of detection rates ranging from 15% to 24%,11 12 and 18% in a 2006 baseline audit in Birmingham.13 Therefore, a major focus of the West Midlands Perinatal Institute's stillbirth prevention strategy since 2008/2009, supported by the Strategic Health Authority and the region's Primary Care Trusts, has been to improve the antenatal recognition of growth restriction in low-risk and high-risk pregnancies. The programme was underpinned by customised charts which are adjustable for maternal constitutional characteristics and predict the optimal fetal growth curve for each pregnancy (‘Gestation Related Optimal Weight’, GROW14). The charts are used for serial plotting of fundal height and estimated fetal weight measurements, and have been shown to increase antenatal detection of intrauterine growth problems.15–17 They also lead to fewer false-positive assessments and unnecessary ultrasound referrals,15 18 thus being reassuring for the mother as well as diverting scarce ultrasound resources towards high-risk pregnancies, where serial scans are indicated to monitor fetal growth.19
Training was instituted from 2008 through a series of bespoke accreditation workshops with hands-on teaching and assessment, and the promotion of evidence-based protocols and best practice guidelines.19–21 The rolling workshops were offered as a free programme to Trusts in the West Midlands, and were also held on invitation in interested Trusts in other regions.
We wanted to assess the effect that this training programme had on stillbirth rates, using the latest release of national statistics for English regions and Wales.22
Methods
Training
Accreditation training in customised growth assessment and protocols was conducted in 2.5 h workshops and covered:
Rationale of fetal growth assessment;
National and regional guidelines;
Use of GROW software including data entry and print out of chart;
Training in standardised fundal height measurement and serial plotting;
Definition of normal, slow, static and accelerated growth;
Referral pathways for further investigation by ultrasound and Doppler;
Risk assessment and protocols for serial scans in high-risk pregnancy;
Evaluation through a test with MCQs and short answers including scenarios.
Fortnightly accreditation workshops were commenced in 2008 at the West Midlands Perinatal Institute in Birmingham and were attended by midwives and midwife trainers as well as ultrasonographers and junior and senior obstetricians. The training was also available to staff from Trusts in other regions, through central or locally arranged workshops. Trusts which had accreditation workshops during 2012 were not considered ‘trained’ in this analysis of pregnancies which delivered up to 2012.
Data analysis
Data on live births and stillbirths were derived from the Office of National Statistics (ONS) mortality statistics release for 201222 and previous releases from 2007 onwards.23 All data were fully anonymised and included stillbirths from 24 weeks gestation. Stillbirth rates were presented for single year as well as 3-year moving averages to smooth out short-term fluctuations and highlight longer term trends. Trend analysis was undertaken using standard χ2 trend test with 1 degree of freedom. Least-squares linear regression was used to obtain the slopes for the stillbirth rates of each region.
Results
Uptake of training
Eighteen of the 19 maternity units, representing 14 of the 15 hospital Trusts in the West Midlands, implemented the GROW software and training programme, and the fortnightly workshops resulted in over 2000 staff being trained between 2008 and 2011. In the whole of England and Wales, staff in 46 of the 148 Trusts (31.1%) received accreditation training, resulting in 27.6% of all pregnancies during this period being cared for in units with trained staff (table 1). However, there was wide variation in uptake. In three regions (North East, Yorkshire and the Humber and West Midlands), on average, 78.5% of pregnancies (range 57.6–92.9%) were cared for in units which had GROW training, while this average was 12.0% (range 0–23.8%) for the rest of England and Wales (table 1).
Table 1.
GROW accreditation and protocol training programme—uptake in Trusts in England and Wales, 2008–2011. Percentage of births in high uptake regions (>50%) marked in bold.
| Number (%) of trained Trusts | Total births in trained Trusts (% of all births in region) | ||||||
|---|---|---|---|---|---|---|---|
| Births in 201222 | Number of Trusts |
N |
% | Hospital Trusts in region with accreditation training | N | % | |
| England and Wales | 733 232 | 148 | 46 | 31.1 | 202 637 | 27.6 | |
| Wales | 35 419 | 7 | 0 | 0.0 | 0 | 0.0 | |
| England | 697 598 | 141 | 46 | 32.6 | 202 637 | 29.0 | |
| North East | 30 410 | 8 | 5 | 62.5 | Gateshead; Hartlepool; Newcastle; North Tees; South Tyneside | 17 723 | 57.6 |
| North West | 89 677 | 21 | 6 | 28.6 | Bolton; East Lancashire; Southport & Ormskirk; Tameside; Warrington; Wrighton, Wigan & Leigh | 21 300 | 23.8 |
| Yorkshire and the Humber | 67 747 | 12 | 10 | 83.3 | Airedale; Barnsley; Calderdale & Huddersfield; Doncaster & Bassetlaw; Harrogate; Leeds; Mid Yorkshire; Rotherham; Sheffield; York; | 48 700 | 71.9 |
| East Midlands | 55 923 | 9 | 2 | 22.2 | Kettering; Northampton | 8797 | 15.7 |
| West Midlands | 74 272 | 15 | 14 | 93.3 | Birmingham Women's; Burton; Coventry & Warwickshire; Dudley; George Eliot; Heart of England; Mid Staffordshire; North Staffordshire; Royal Shrewsbury & Telford; Sandwell & West Birmingham; South Warwickshire; Walsall; Worcester; Wye Valley | 68 991 | 92.9 |
| East of England | 74 884 | 17 | 1 | 5.9 | Hinchingbrooke | 2541 | 3.4 |
| London | 134 941 | 22 | 2 | 9.1 | Ealing; Lewisham | 6996 | 5.2 |
| South East | 54 128 | 11 | 1 | 9.1 | East Kent | 7552 | 14.0 |
| South Central | 54 216 | 8 | 2 | 25.0 | Hampshire; Portsmouth | 12 197 | 22.5 |
| South West | 61 400 | 18 | 3 | 16.7 | Northern Devon; Royal Devon & Exeter; South Devon | 7840 | 12.8 |
| High-uptake regions | 172 429 | 35 | 29 | 82.9 | North East, Yorkshire and the Humber, West Midlands | 135 414 | 78.5 |
| Low-uptake regions | 560 588 | 113 | 17 | 15.0 | Rest of English regions and Wales | 67 223 | 12.0 |
Stillbirth rates and trends
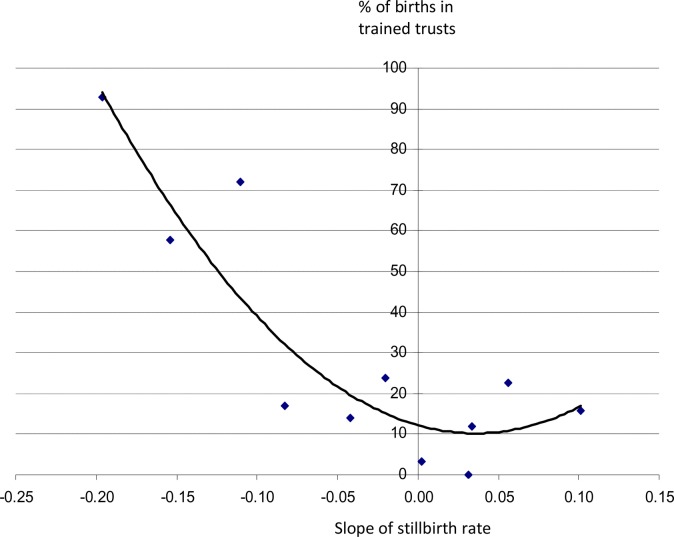
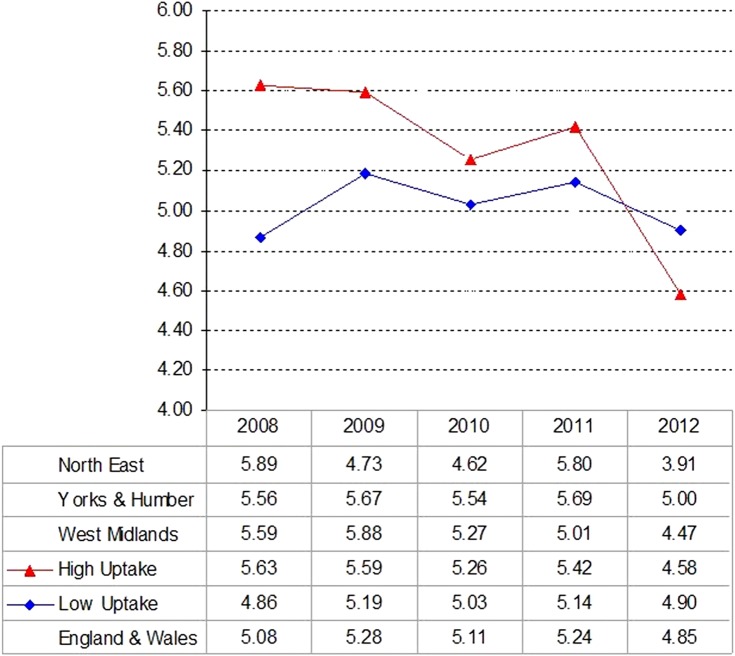
Table 2 lists births, stillbirths and stillbirth rates from 2007 to 2012 for English regions and Wales together with trend analysis. There was a significant fall in stillbirth rates over this period in England (p<0.03) but not in Wales (p=0.7). Among English regions, only the West Midlands had a significant downward trend (p<0.01) and if this region is excluded, the drop in England becomes non-significant. The two other regions which were high GROW accreditation areas, North East and Yorkshire and the Humber, each showed downward trends in stillbirth rates which, when taken together, also reached statistical significance (p<0.03). These three regions were the only ones which achieved a negative (downward) slope of –0.10 or lower (West Midlands: –0.20; North East: –0.15; Yorkshire and the Humber: –0.11; table 2). The training uptake rates in the regions were significantly correlated with negative slopes of stillbirth trends in table 2: R=−0.82, p<0.01 (figure 1). The year-on-year stillbirth rate for the three high-uptake regions is compared graphically with the remaining, low-uptake regions in figure 2.
Table 2.
Total births, stillbirths (SBs) and SB rate (per 1000) in England, English regions and Wales 2007–2012. Values in bold indicate significant trend tests.
| 2007 |
2008 |
2009 |
2010 |
2011 |
2012 |
Trend test |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | Slope* | p Value | |
| England and Wales | 693 611 | 3598 | 5.19 | 712 328 | 3617 | 5.08 | 689 591 | 3644 | 5.28 | 726 879 | 3714 | 5.11 | 727 724 | 3811 | 5.24 | 733 232 | 3558 | 4.85 | −0.04 | 0.05 |
| England | 658 771 | 3414 | 5.18 | 676 236 | 3427 | 5.07 | 656 880 | 3475 | 5.29 | 690 513 | 3506 | 5.08 | 691 739 | 3619 | 5.23 | 697 598 | 3357 | 4.81 | −0.06 | 0.03 |
| North East | 29 728 | 146 | 4.91 | 30 396 | 179 | 5.89 | 29 991 | 142 | 4.73 | 30 969 | 143 | 4.62 | 30 705 | 178 | 5.80 | 30 410 | 119 | 3.91 | −0.15 | 0.1 |
| North West | 86 423 | 476 | 5.51 | 88 617 | 450 | 5.08 | 87 492 | 469 | 5.36 | 89 665 | 466 | 5.20 | 89 235 | 483 | 5.41 | 89 677 | 466 | 5.20 | −0.02 | 0.7 |
| Yorks & Humber | 64 567 | 376 | 5.82 | 66 724 | 371 | 5.56 | 65 559 | 372 | 5.67 | 67 343 | 373 | 5.54 | 66 831 | 380 | 5.69 | 67 747 | 339 | 5.00 | −0.11 | 0.1 |
| East Midlands | 52 716 | 234 | 4.44 | 54 447 | 255 | 4.68 | 47 741 | 270 | 5.66 | 55 525 | 293 | 5.28 | 55 662 | 284 | 5.10 | 55 923 | 278 | 4.97 | 0.10 | 0.2 |
| West Midlands | 70 477 | 379 | 5.38 | 72 129 | 403 | 5.59 | 71 399 | 420 | 5.88 | 72 472 | 382 | 5.27 | 73 391 | 368 | 5.01 | 74 272 | 332 | 4.47 | −0.20 | <0.01 |
| East of England | 69 619 | 308 | 4.42 | 72 042 | 304 | 4.22 | 67 638 | 325 | 4.80 | 73 346 | 345 | 4.70 | 73 565 | 345 | 4.69 | 74 884 | 313 | 4.18 | 0.00 | 1.0 |
| London | 126 286 | 781 | 6.18 | 128 381 | 730 | 5.69 | 129 980 | 719 | 5.53 | 133 853 | 742 | 5.54 | 133 604 | 761 | 5.70 | 134 941 | 755 | 5.60 | −0.08 | 0.1 |
| South East Coast | 50 692 | 239 | 4.71 | 51 800 | 235 | 4.54 | 53 297 | 240 | 4.50 | 53 049 | 256 | 4.83 | 53 418 | 257 | 4.81 | 54 128 | 227 | 4.19 | −0.04 | 0.6 |
| South Central | 51 021 | 236 | 4.63 | 52 694 | 236 | 4.48 | 46 923 | 245 | 5.22 | 53 892 | 251 | 4.66 | 54 246 | 275 | 5.07 | 54 216 | 259 | 4.78 | 0.06 | 0.4 |
| South West | 57 242 | 239 | 4.18 | 59 006 | 264 | 4.47 | 56 860 | 273 | 4.80 | 60 399 | 255 | 4.22 | 61 082 | 288 | 4.71 | 61 400 | 269 | 4.38 | 0.03 | 0.6 |
| Wales | 34 585 | 171 | 4.94 | 35 815 | 165 | 4.61 | 32 711 | 169 | 5.17 | 36 142 | 190 | 5.26 | 35 765 | 167 | 4.67 | 35 419 | 181 | 5.11 | 0.03 | 0.7 |
Source: Office for National Statistics 22, 23 *Slope by linear regression; p values for trend test.
Figure 1.
Correlation between stillbirth trends 2007–2012 in English regions and Wales (table 2) and proportion (%) of pregnancies cared for in units with GROW training (table 1). Regression line: R= −0.82, p<0.01.
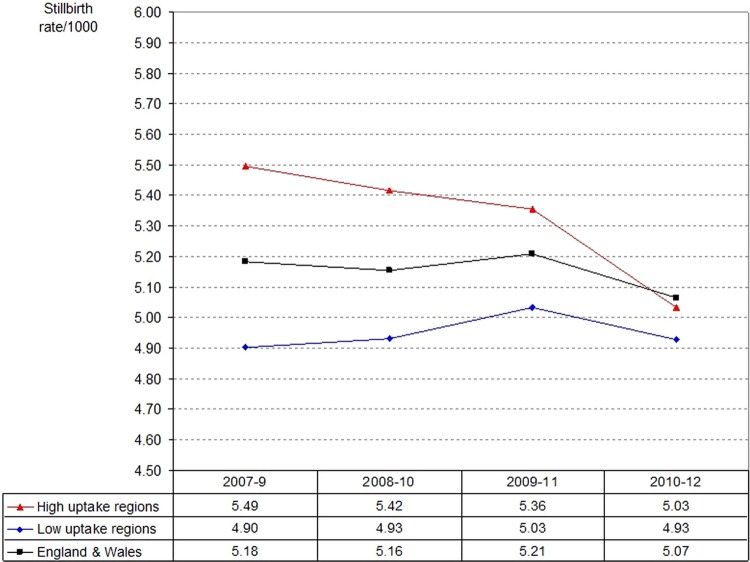
Figure 2.
Yearly stillbirth rates in the three regions with high uptake of GROW training and protocols (‘high uptake’) vs the rest (‘low uptake’), 2008–2012 (see table 1). Analysis of trend: high uptake, p<0.01; low uptake, p=0.9.
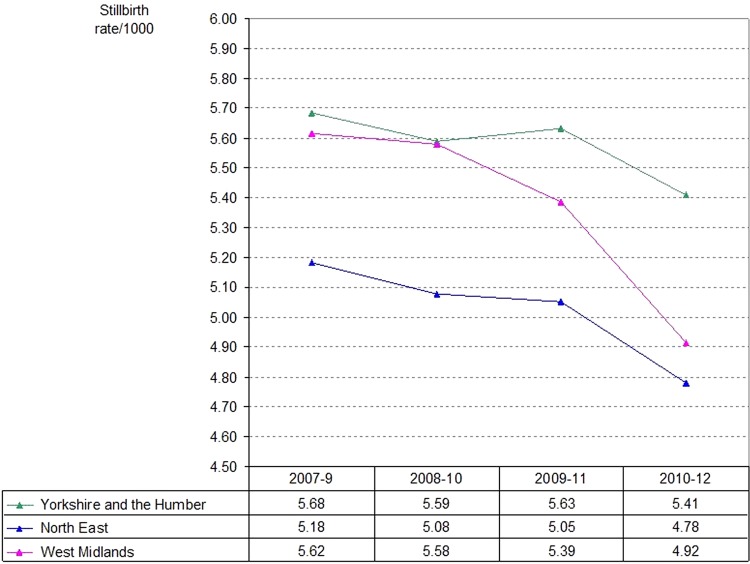
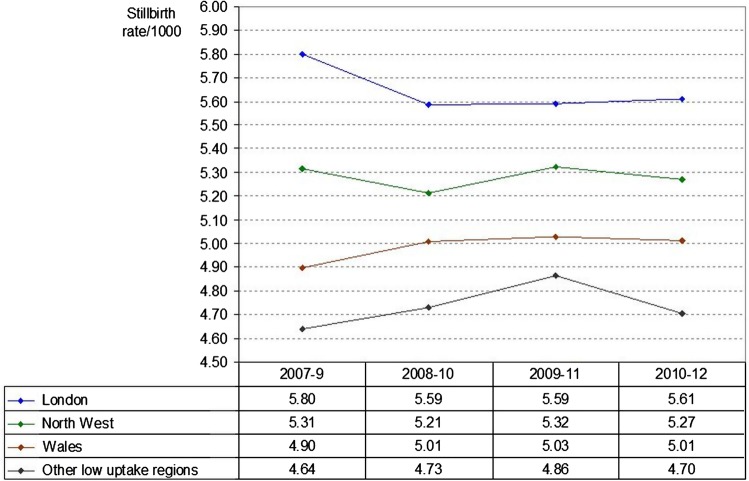
Three-year moving average analysis
In table 3 and figures 3 and 4, 3-year moving average stillbirth rates are listed for high-uptake and low-uptake regions of the accreditation programme. Each of the high-uptake regions displayed a downward trend (figure 3), while stillbirth rates in the other regions and Wales remained stagnant (figure 4). The moving average rates in high-uptake and low-uptake regions are compared in figure 5, demonstrating that the drop in stillbirths in England and Wales was achieved by the three regions with high uptake of GROW training.
Table 3.
Three-year moving average of total births, stillbirths (SBs) and SB rates, England, English regions and Wales, 2007–2012, according to high or low uptake of GROW training
| 2007–2009 |
2008–2010 |
2009–2011 |
2010–2012 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | Total births | SBs | SB rate | |
| England and Wales | 2 095 530 | 10 859 | 5.18 | 2 128 798 | 10 975 | 5.16 | 2 144 194 | 11 169 | 5.21 | 2 187 835 | 11 083 | 5.07 |
| High uptake | 500 970 | 2788 | 5.57 | 506 982 | 2785 | 5.49 | 508 660 | 2758 | 5.42 | 514 140 | 2614 | 5.08 |
| North East | 90 115 | 467 | 5.18 | 91 356 | 464 | 5.08 | 91 665 | 463 | 5.05 | 92 084 | 440 | 4.78 |
| Yorks & Humber | 196 850 | 1119 | 5.68 | 199 626 | 1116 | 5.59 | 199 733 | 1125 | 5.63 | 201 921 | 1092 | 5.41 |
| West Midlands | 214 005 | 1202 | 5.62 | 216 000 | 1205 | 5.58 | 217 262 | 1170 | 5.39 | 220 135 | 1082 | 4.92 |
| Low uptake | 1 594 028 | 8033 | 5.04 | 1 621 315 | 8147 | 5.02 | 1 635 090 | 8368 | 5.12 | 1 673 036 | 8406 | 5.02 |
| North West | 262 532 | 1395 | 5.31 | 265 774 | 1385 | 5.21 | 266 392 | 1418 | 5.32 | 268 577 | 1415 | 5.27 |
| East Midlands | 154 904 | 759 | 4.90 | 157 713 | 818 | 5.19 | 158 928 | 847 | 5.33 | 167 110 | 855 | 5.12 |
| East of England | 209 299 | 937 | 4.48 | 213 026 | 974 | 4.57 | 214 549 | 1015 | 4.73 | 221 795 | 1003 | 4.52 |
| London | 384 647 | 2230 | 5.80 | 392 214 | 2191 | 5.59 | 397 437 | 2222 | 5.59 | 402 398 | 2258 | 5.61 |
| South East Coast | 155 789 | 714 | 4.58 | 158 146 | 731 | 4.62 | 159 764 | 753 | 4.71 | 160 595 | 740 | 4.61 |
| South Central | 150 638 | 717 | 4.76 | 153 509 | 732 | 4.77 | 155 061 | 771 | 4.97 | 162 354 | 785 | 4.84 |
| South West | 173 108 | 776 | 4.48 | 176 265 | 792 | 4.49 | 178 341 | 816 | 4.58 | 182 881 | 812 | 4.44 |
| Wales | 103 111 | 505 | 4.90 | 104 668 | 524 | 5.01 | 104 618 | 526 | 5.03 | 107 326 | 538 | 5.01 |
Figure 3.
Stillbirth rates in regions with high uptake of GROW training and protocols, 2007–2012 (3-year moving average).
Figure 4.
Stillbirth rates in regions with low uptake of GROW training and protocols, 2007–2012 (3-year moving average).
Figure 5.
Stillbirth rates in high and low uptake regions and England and Wales, 2007–2012 (3-year moving average).
Discussion
This is, to our knowledge, the first analysis of national and regional stillbirth trends and their association with a training and accreditation programme. It indicates that stillbirth rates have dropped in regions with high levels of training (West Midlands, North East, Yorkshire and the Humber), while they stagnated in regions with low uptake. The downward trends in these three regions resulted in a drop in the national stillbirth rate to its lowest level since the current ONS stillbirth definitions were introduced in 1992, even though together, these regions account for less than a quarter of births in England (172 429/697 598=24.7%; table 1).
Significance of fetal growth
The focus on intrauterine growth in stillbirth prevention is justified as intrauterine growth restriction, defined as birth weight below the 10th customised centile, constitutes the largest single category of the stillbirth classification by relevant condition at death (ReCoDe), comprising over 50% of normally formed stillbirths.6 In addition, stillbirths are only one of a range of adverse pregnancy outcomes known to follow intrauterine growth restriction, which also includes perinatal morbidity,24 25 mortality26 and cerebral palsy.27 Most pregnancies with fetal growth restriction are due to late onset placental pathology and are born at term.10 28 Case note peer reviews have established that the majority of deaths with fetal growth problems are potentially avoidable, through better assessment of risk factors and surveillance of growth during pregnancy.9 Antenatal recognition of growth restriction leads to appropriate investigations and improved outcome.29–31 It halves the stillbirth risk while resulting in babies being delivered, on average, only 10 days earlier at term, at 270 vs 280 days of gestation.10
Antenatal detection
An ongoing problem in maternity care has been the lack of antenatal recognition of fetal growth problems, which precludes further investigations to determine the optimal time for delivery of the fetus from an unfavourable intrauterine environment. While no national data are available, we know from controlled studies that antenatal detection improves significantly with implementation of customised charts, training and protocols.15 West Midlands audits have shown that improved antenatal recognition is directly linked with uptake of training: in one unit in the region which did not implement the recommended training and protocol, antenatal detection remained at 12.5%, while units which adopted the protocols and ensured staff were trained achieved detection rates up to 50% within 12 months of implementation.32 Once a mother carrying a suspected growth-restricted baby was referred according to protocol for an ultrasound scan on the basis of fundal height measurement plotted on customised charts, antenatal detection rate averaged 62% and could be as high as 85%.33
Fetal growth surveillance in the UK is a multidisciplinary task and requires collaboration between community and hospital midwives, general practitioner, ultrasonographer and obstetrician or maternal-fetal medicine specialist. Care usually starts with the community midwife, who within the NHS is usually the first to see the expectant mother. Her assessment of whether the woman is of low or high risk will initiate the relevant care pathway.
Surveillance in low-risk and high-risk pregnancy
For low-risk mothers, third trimester growth is assessed through serial measurement of fundal height which until recently has had little standardisation in midwifery and medical training. As fundal height varies with maternal size,34 plotting on customised charts is recommended according to RCOG guidelines19 which can predict the expected, optimal fetal growth trajectory after adjustment for each mother's parity, maternal height, maternal weight in early pregnancy and ethnic origin. Where measurements do not follow the expected curve and/or cross percentile lines, protocols should prompt referral for ultrasound scan biometry to determine the estimated fetal weight, which is plotted on the same chart adjusted for maternal and pregnancy characteristics. An estimated fetal weight which is small-for-gestational age on a customised chart, or repeated measurements which show slow growth, are indications for obstetric review and further investigations,19 20 to be managed according to individual circumstances and evidence-based guidelines.19
For mothers at an increased risk of intrauterine growth restriction because of obstetric history or other risk factors, or where fundal height measurement is difficult, for example, due to a maternal body mass index of 35 or more, serial third trimester scans are indicated.19–21 The current weak link in the referral chain is the chronic shortage of sonographers and ultrasound services in the NHS, which can manifest in several ways: referral on the basis of fundal height measurement may be unduly delayed or ignored; or the scan may be refused because of the frequently heard claim that ultrasound biometry at term has less accuracy—a claim which is in fact not supported by evidence.35 Furthermore, case note audits have shown that most of the pregnancies with an indication for serial ultrasound scans receive only one scan in the third trimester,13 resulting in detection rates no better than that obtained in pregnancies which receive no scan at all. Preliminary evidence suggests that antenatal detection in increased risk pregnancies can be improved with a policy of four three-weekly scans in the third trimester, up to and including term.36 Enhanced ultrasound scan policies can be cost-neutral when accompanied by implementation of customised charts, as their use for plotting fundal height measurement15 and estimated fetal weight18 will reduce false-positive diagnoses of ‘small-for-gestational age’ and referrals for unnecessary investigations.
As shown in table 2, crude baseline stillbirth rates vary considerably between regions; they are likely to be related to characteristics of the population including social factors, ethnic mix and differences in congenital anomaly rates. Our analysis does not seek to compare the rates in different regions, but assess year-on-year trends and relative change. Two of the three regions with high uptake in GROW training had above average stillbirth rates at the beginning of the study period. As figures 2 and 3 demonstrate, the drop in stillbirths in these regions has contributed to a reduction in regional inequalities.
Strengths and limitations
The regional analysis helps to reduce random variation due to small numbers at unit or Trust level and allows trends to become apparent. A possible weakness of our study is that only crude ONS figures were available, without subcategories of stillbirths to identify where the improvements occurred. However, previous analysis of the more detailed West Midlands database has shown that the downward trend in regional stillbirth rates, already evident in 2011, could be pinpointed to fewer deaths associated with intrauterine growth restriction, while there was no change in any of the other main stillbirth categories.37
Another potential criticism of our study is that confounders could have been responsible for the findings. However, we are not aware of any other recent or current major initiatives which could have accounted for the reduction in stillbirths over this period, either nationally or in the regions with the observed downward trends.
Our study was observational and looked at the effect of voluntary engagement in a training and protocol programme. While a randomised trial design is usually considered the gold standard, it is not likely to be practical in this field, neither in terms of the power and sample size required when assessing the effects on relatively rare outcomes, nor in the equipoise needed for withholding training and implementation of already established, evidence-based guidelines.
An examination of the nine criteria by Hill38 to establish causality demonstrates that each criterion is fulfilled (table 4), including that of temporality emphasised by Rothman.39 While Hill38 acknowledged that neither of his criteria represent indisputable evidence for or against a cause and effect hypothesis, they do help to determine “…whether there is any other answer equally, or more likely than cause and effect.” The evidence here suggests that the association between the intervention (accreditation training and implementation of evidence-based protocols) and outcome (reduction in stillbirth rates) may indeed be causal.
Table 4.
Examination of association according to Sir Austin Bradford Hill's nine causality criteria38
| Criterion for causality | Findings and associated characteristics of current study |
|---|---|
| Strength of association | Significant downward trend in stillbirth rates which had remained static for the past 20 years. Each of the high-uptake regions dropped to their lowest ever rates (table 2) |
| Temporality | Reduced stillbirth rates followed implementation of accreditation training and protocol. E.g., Yorkshire and the Humber drop in 2012 followed training initiative in 2011 |
| Consistency | Reduction in stillbirths shown in the three regions with high uptake (figure 3), and not in the regions with low uptake (figure 4). See also significant correlation in figure 1 |
| Plausibility | Confidential case reviews have shown that unrecognised fetal growth restriction was the most common cause of stillbirth.9 Population based study has shown that IUGR is the strongest risk factor for stillbirth, and its antenatal recognition reduces risk10 |
| Dose response | The region with the most intensive training programme (West Midlands) had the steepest drop and downward trend in stillbirth rates (figure 3) |
| Experimental evidence | Antenatal recognition of intrauterine growth restriction results in earlier delivery10 and reduces stillbirth risk10 30 31 |
| Coherence | Improved recognition allows the implementation of appropriate investigations15 29 and timely delivery10 |
| Specificity | The regions which demonstrated reduction in stillbirth rates during the period of investigation had high uptake in training and protocols, but no other known interventions which applied selectively to them and no other regions |
| Analogy | Growth restriction associated with placental failure has been shown to lead to fetal death in various animal models |
Regional programmes
The argument that this relationship is likely to be causal is strengthened further when examining the associations between stillbirth trends and time and effort. In the North East, GROW accreditation training was adopted between 2008 and 2011 by the majority of Trusts, and was facilitated by the preceding strong promotion of the 2002 RCOG guidelines19 by the region's lead unit in Newcastle. The 3-year moving average graph (figure 3) shows a gradual drop accentuated in the last triennium, with the 2012 stillbirth rate (3.91/1000) being the lowest ever recorded for the region (table 2).
In Yorkshire and the Humber, all units participated in 2011 in a ‘train the trainer’ programme and developed a regional ‘best practice’ competency document based on the Perinatal Institute's protocols and training tools, which were administered through midwifery supervision. The ensuing year, 2012, saw a drop in stillbirth rates to 5.00/1000 (figure 2), the lowest recorded for the region to date.
In the West Midlands, the introduction of the GROW accreditation programme in 2008 was complemented by regionally agreed protocols for scanning high-risk pregnancies, and were from 2008 to 2011 supported by augmented ultrasound resources in Birmingham, Stoke on Trent and several other areas. In addition, a data collection programme reported quarterly on antenatal detection rates of small for gestational age birth weight as a regionally agreed key performance indicator. The Region's stillbirth rates dropped year on year, with the 2011 rate falling for the first time in 50 years to below the national average.37 This fall continued in 2012 to 4.47/1000 (table 2), which is 1.26/1000 or 22% below the preceding (2000–2007) ONS regional average of 5.73/1000, and was equivalent to 92 deaths in the West Midlands. A similar rate reduction applied to the more than 800 000 annual deliveries in the UK would result in over 1000 fewer stillbirths each year.
International perspectives
While this analysis focuses on English regions and Wales, stillbirths are a global problem, with the overwhelming majority occurring in low-income and middle-income countries.40 Global trends in stillbirth rate reduction lag behind progress in reducing maternal mortality and deaths in children under 5 years.40 Prevention will need to consider fundamental local needs, including provision and access to basic maternal and child health services and intrapartum and emergency care. However while these challenges are of a different order of magnitude, fetal growth restriction is also a universal concern, and the obstacles to improvement are in principle not dissimilar to those encountered here: insufficient awareness of the importance of fetal growth, lack of protocols, staff and equipment and the use of inappropriate growth standards, often imported from high-income countries. Recent work has started to address the need for international standards which are also individually customisable, or at least adjustable to the average characteristics of the local population.41–43 It is hoped that mounting awareness in high-income settings of the avoidability of many stillbirths will also help to enhance global prevention strategies.
Implications for the health service
Each stillbirth is a tragic loss which causes untold grief and distress to the mother, father and extended family. In addition, stillbirths represent a high cost to the health service and society as a whole. Bereaved parents require intensive social and psychological support. Each mature, normally formed stillborn child represents the largest possible loss to society, in terms of lost potential; conversely, prevention of stillbirths, although not yet measured in those terms, would likely to represent the maximum possible gain in quality adjusted life years (QALYs).44
Our findings suggest that many stillbirths are not only avoidable, but have in fact been avoided, in the Trusts which adopted standardised training and evidence-based protocols for identification of fetuses at risk due to fetal growth restriction. We suggest that commissioners and providers should give high priority to ensuring that implementation of such a programme becomes an integral requirement for safe antenatal care, and is monitored by antenatal detection rates of fetal growth restriction as a key indicator of the quality of the service.
Supplementary Material
Footnotes
Contributors: All authors had full access to the data, assisted with its analysis and interpretation of the results, and reviewed and approved the final manuscript. JG wrote the paper, has final responsibility to submit for publication, and is the guarantor.
Funding: All staff were financially supported during the period of the study by NHS West Midlands Strategic Health Authority and Primary Care Trusts.
Competing interests: All authors work for the Perinatal Institute, a not-for-profit organisation which supports the provision of customised growth charts and runs training workshops in fetal growth assessment.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Zeitlin J, Mohangoo A, Delnord M. European Perinatal Health Report: the health and care of pregnant women and their babies in 2010. Paris: INSERM, 2013. http://www.europeristat.com/images/European%20Perinatal%20Health%20Report_2010.pdf (accessed 31 Aug 2013) [Google Scholar]
- 2.The NHS Outcomes Framework 2012/13, Department of Health, London: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_131723.pdf (accessed 31 Aug 2013) [Google Scholar]
- 3.Chaotic NHS fails to prevent hundreds of stillbirths. The Times, 2012. http://www.thetimes.co.uk/tto/health/news/article3612548.ece (accessed 31 Aug 2013)
- 4.Confidential Enquiry into Maternal and Child Health (CEMACH) Perinatal mortality 2006: England, Wales and Northern Ireland. CEMACH, 2008. (Table 4.2) [Google Scholar]
- 5.Gardosi J. Clinical implications of ‘unexplained’ stillbirths. (Commentary) In: Maternal and Child Health Research Consortium, ed: CESDI 8th Annual Report Confidential Enquiry into Stillbirths and Deaths in Infancy, 2001:40–7 http://www.pi.nhs.uk/pnm/CESDI%20SB%20commentary.pdf (accessed 31 Aug 2013) [Google Scholar]
- 6.Gardosi J, Kady S, McGeown P, et al. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ 2005;331:1113–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Froen JF, Gardosi J, Thurmann A, et al. Restricted fetal growth in sudden intrauterine unexplained death. Acta Obstet Gynecol Scand 2004;83:81–7 [DOI] [PubMed] [Google Scholar]
- 8.Serena C, Marchetti G, Rambaldi MP, et al. Stillbirth and fetal growth restriction. J Matern Fetal Neonatal Med 2013;26:16–20 [DOI] [PubMed] [Google Scholar]
- 9.Confidential enquiry into stillbirths with intrauterine growth restriction—West Midlands Perinatal Institute. 2007. http://www.pi.nhs.uk/rpnm/CE_SB_Final.pdf (accessed 31 Aug 2013)
- 10.Gardosi J, Madurasinghe V, Williams M, et al. Maternal and fetal risk factors for stillbirth: population based study. BMJ 2013;346:f108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hepburn M, Rosenberg K. An audit of the detection and management of small-for-gestational age babies. Br J Obstet Gynaecol 1986;93:212–16 [DOI] [PubMed] [Google Scholar]
- 12.Kean LH, Liu DT. Antenatal care as a screening tool for the detection of small for gestational age babies in the low risk population. J Obstet Gynaecol 1996;16:77–82 [Google Scholar]
- 13.Birmingham Fetal Growth Audit West Midlands Perinatal Institute, 2007. http://www.pi.nhs.uk/ultrasound/Birmingham_FGR_Audit_-_Summary.pdf (accessed 31 Aug 2013)
- 14.GROW (Gestation Related Optimal Weight) software version 6.5 (UK). Gestation Network 2012. http://www.gestation.net/GROW_documentation.pdf (accessed 31 Aug 2013)
- 15.Gardosi J, Francis A. Controlled trial of fundal height measurement plotted on customised antenatal growth charts. Br J Obstet Gynaecol 1999;106:309–17 [DOI] [PubMed] [Google Scholar]
- 16.Wright J, Morse K, Kady S, et al. Audit of fundal height measurement plotted on customised growth charts MIDIRS Midwifery Digest 2006;16:341 [Google Scholar]
- 17.Roex A, Nikpoor P, van Eerd E, et al. Serial plotting on customised fundal height charts results in doubling of the antenatal detection of small for gestational age fetuses in nulliparous women. Aust N Z J Obstet Gynaecol 2012;52:78–82 [DOI] [PubMed] [Google Scholar]
- 18.Mongelli M, Gardosi J. Reduction of false-positive diagnosis of fetal growth restriction by application of customized fetal growth standards. Obstet Gynecol 1996;88:844–8 [DOI] [PubMed] [Google Scholar]
- 19.Royal College of Obstetrics and Gynaecology Green-Top Guidelines The investigation and management of the small-for-gestational-age fetus. 2002, 2013. http://www.rcog.org.uk/womens-health/investigation-and-management-small-gestational-age-fetus-green-top-31 (accessed Aug 2013)
- 20.Figueras F, Gardosi J. Intrauterine growth restriction: new concepts in antenatal surveillance, diagnosis, and management. Am J Obstet Gynecol 2011;204:288–300 [DOI] [PubMed] [Google Scholar]
- 21.Morse K, Williams A, Gardosi J. Fetal growth screening by fundal height measurement. Best Pract Res Clin Obstet Gynaecol 2009;23:809–18 [DOI] [PubMed] [Google Scholar]
- 22.Death Registrations Regional Statistics 2012. ONS, 2013. http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-314473 (accessed 31 Aug 2013)
- 23.Perinatal and infant mortality 2007. Health Statistics Quarterly, ONS, 2008. http://www.ons.gov.uk/ons/rel/hsq/health-statistics-quarterly/no--39--autumn-2008/health-statistics-quarterly.pdf (accessed 31 Aug 2013)
- 24.McCowan LM, Harding JE, Stewart AW. Customized birth weight centiles predict SGA pregnancies with perinatal morbidity. BJOG 2005;112:1026–33 [DOI] [PubMed] [Google Scholar]
- 25.Figueras F, Figueras J, Meler E, et al. Customised birth weight standards accurately predict perinatal morbidity. Arch Dis Child Fetal Neonatal Ed 2007;92:F277–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clausson B, Gardosi J, Francis A, et al. Perinatal outcome in SGA births defined by customised versus population-based birth weight standards. BJOG 2001;108:830–4 [DOI] [PubMed] [Google Scholar]
- 27.Jacobsson B, Ahlin K, Francis A, et al. Cerebral palsy and restricted growth status at birth: population-based case-control study. BJOG 2008;115:1250–5 [DOI] [PubMed] [Google Scholar]
- 28.Groom K, North R, Poppe K, et al. The association between customised small for gestational age infants and preeclampsia or gestational hypertension varies with gestation at delivery. BJOG 2007;114:478–84 [DOI] [PubMed] [Google Scholar]
- 29.Alfirevic Z, Neilson JP. Doppler ultrasonography in high-risk pregnancies: systematic review with meta-analysis. Am J Obstet Gynecol 1995;172:1379–87 [DOI] [PubMed] [Google Scholar]
- 30.Lindqvist PG, Molin J. Does antenatal identification of small-for-gestational age fetuses significantly improve their outcome? Ultrasound Obstet Gynecol 2005;25:258–64 [DOI] [PubMed] [Google Scholar]
- 31.Stacey T, Thompson JMD, Mitchell EA, et al. Antenatal care, identification of suboptimal fetal growth and risk of late stillbirth: findings from the Auckland Stillbirth Study. ANZJOG 2012;52:242–7 [DOI] [PubMed] [Google Scholar]
- 32.Key Performance Indicator report—Q2 2010/11; West Midlands Perinatal Institute. 2011. http://www.pi.nhs.uk/pnm/maternitydata/Q2_2010-11_Perinatal_KPI_report.pdf (accessed 31 Aug 2013)
- 33.West Midlands Investing for Health—Perinatal Data Collection Project Q4 Report 2010. West Midlands Perinatal Institute; http://www.pi.nhs.uk/pnm/maternitydata/IfH2c_WM_Q4_Report.pdf (accessed 31 Aug 2013) [Google Scholar]
- 34.Mongelli M, Gardosi J. Symphysis-fundus height and pregnancy characteristics in ultrasound-dated pregnancies. Obstet Gynecol 1999;94:591–4 [DOI] [PubMed] [Google Scholar]
- 35.Francis A, Tonks A, Gardosi J. Accuracy of ultrasound estimation of fetal weight at term. Arch Dis Child Fetal Neonatal Ed 2011;96:Fa61 http://fn.bmj.com/content/96/Suppl_1/Fa61.1.abstract [Google Scholar]
- 36.Tonks AM, Williamson A, Williams A, et al. An enhanced, midwifery-led ultrasound service to monitor fetal growth. Arch Dis Child Fetal Neonatal Ed 2013;98(Suppl 1):A1–11223641499 [Google Scholar]
- 37.Stillbirths in the West Midlands: 2011 Update. West Midlands Perinatal Institute; 2012. http://www.pi.nhs.uk/pnm/clusterreports/2011/WM_2011_Stillbirth_Update_Sept_2012.pdf (accessed 31 Aug 2013) [Google Scholar]
- 38.Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300 [PMC free article] [PubMed] [Google Scholar]
- 39.Rothman KJ. Epidemiology: an introduction. Oxford: Oxford University Press, 2002 [Google Scholar]
- 40.Cousens S, Blencowe H, Stanton C, et al. National, regional and worldwide estimates of stillbirth rates in 2009 with trends since 1995: a systematic analysis. Lancet 2011;377:1319–30 [DOI] [PubMed] [Google Scholar]
- 41.Mikolajczyk RT, Zhang J, Betran AP, et al. A global reference for fetal-weight and birth weight percentiles. Lancet 2011;377:1855–61 [DOI] [PubMed] [Google Scholar]
- 42.Gardosi J. Fetal growth standards: individual and global perspectives. Lancet 2011;377:1812–14 [DOI] [PubMed] [Google Scholar]
- 43.Gestation Network Gestation Related Average Weight (GRAW) v1, 2010. http://www.gestation.net/fetal_growth/graw/ (accessed 31 Aug 2013)
- 44.National Institute for Health and Care Excellence Measuring effectiveness and cost effectiveness: the QALY. National Institute for Health and Care Excellence, 2010. http://www.nice.org.uk/newsroom/features/measuringeffectivenessandcosteffectivenesstheqaly.jsp [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.