Abstract
PURPOSE
Substantial heterogeneity in hospital length of stay (LOS) exists among patients admitted with non-ST-segment elevation myocardial infarction (NSTEMI). Furthermore, little is known about the factors that impact LOS and our ability to modify them.
METHODS
We examined 39,107 NSTEMI patients admitted to 351 ACTION Registry®-GWTG™ hospitals from 1/1/07–3/31/09 who underwent cardiac catheterization and survived to discharge. Length of stay was categorized into four groups (≤2, 3–4, 5–7, and ≥8 days), where prolonged LOS was defined as >4 days.
RESULTS
The overall median (25th, 75th) LOS was 3 (2, 5) days. Patients with a LOS of >2 days were older with more comorbidities, but were less likely to receive evidence-based therapies or percutaneous coronary intervention (PCI). Among the factors associated with prolonged LOS >4 days were delay to cardiac catheterization >48 hours, heart failure or shock on admission, female gender, insurance type, and admission to the hospital on a Friday afternoon or evening. Hospital characteristics such as number of beds, academic versus non-academic, or urban versus rural setting, were not associated with prolonged LOS.
CONCLUSION
Patients with longer LOS have more comorbidities and in-hospital complications, yet paradoxically, are less often treated with evidence-based medications and are less likely to receive PCI. Hospital admission on a Friday afternoon or evening and delays to catheterization appear to significantly impact LOS. A better understanding of factors associated with LOS in patients with NSTEMI is needed to promote safe and early discharge in an era of increasingly restrictive healthcare resources.
Keywords: non-ST-segment elevation myocardial infarction, length of stay, hospital discharge
More than a half million patients are hospitalized annually for non-ST-segment elevation myocardial infarction (NSTEMI) in the United States (U.S.).1 Among these patients, there is considerable variability in hospital length of stay (LOS) for reasons that are not well defined. Previous studies have demonstrated that patients with uncomplicated ST-segment elevation myocardial infarction (STEMI) treated with fibrinolysis could be safely discharged as early as three days after presentation.2 Studying the heterogeneity of LOS in STEMI patients has provided important insights into opportunities for safe earlier hospital discharge.3–7 However, to date, no studies have investigated LOS for patients with NSTEMI.
Increasingly, hospitals and healthcare providers are pressured to reduce medical resource expenditures and shorten hospital LOS. The importance of containing healthcare costs underscores the need to better understand the factors associated with longer hospital LOS and to explore opportunities for safe early discharge in patient with NSTEMI. Current treatment guidelines recommend a risk-tailored early invasive approach for the treatment of NSTEMI and advocate for early discharge—especially in those patients who are considered low-risk.8 The effect of patient characteristics and treatment strategies on LOS for NSTEMI patients has not been well studied.
This analysis utilized data from the National Cardiovascular Data Registry® (NCDR) Acute Coronary Treatment Intervention Outcomes Network Registry®-Get With The Guidelines™ (ACTION Registry-GWTG) to explore and identify patient characteristics and clinical factors associated with hospital LOS in patients admitted with NSTEMI who underwent cardiac catheterization. The variables analyzed in this study include patient demographics, treatment strategies, hospital characteristics, medication use, and clinical outcomes as they relate to hospital LOS.
METHODS
The ACTION Registry-GWTG is a result of the merger between the American College of Cardiology Foundation’s (ACCF’s) NCDR ACTION Registry and the American Heart Association’s (AHA) GWTG-Coronary Artery Disease (CAD) Registry. The ACTION Registry-GWTG is a voluntary national quality improvement registry that began collecting data on January 1, 2007 on hospitalized STEMI and NSTEMI patients. This registry is now the largest national quality improvement initiative focusing on patients with myocardial infarction (MI).9
The full details of the registry operations, quality assurance, and data collected have been previously reported.10 Briefly, data were entered at each site by a trained data collector. The NCDR employs a standard data set with uniform data entry and data quality checks.9 The variables recorded included pre-hospital data, acute (within 24 hours) and discharge therapies, medical comorbidities, treatments administered, in-hospital procedures and outcomes, admission time and date, discharge time and date, and contraindications to evidence-based therapy. Institutional review board approval was obtained for data collection according to individual site policies and regulations as related to quality improvement data collection processes.
Patient Population
Between January 1, 2007 and December 31, 2009, 98,545 NSTEMI patients at 384 hospitals were enrolled into the ACTION Registry-GWTG. To focus on a more homogeneous population of patients relative to treatment strategy, patients were excluded if: (1) they did not undergo cardiac catheterization or had missing catheterization status data (n=24,899); (2) underwent coronary artery bypass grafting (CABG) or had missing CABG status data (n=10,581); (3) were transferred out (n=2,336) or transferred in to the reporting hospital (n=20,815); (4) had a LOS equal to zero or missing LOS data (n=59); or (5) died during their hospitalization (n=748). After exclusions, our final study population included 39,107 NSTEMI patients from 351 hospitals.
Definitions
Length of stay was defined as the time interval between date of admission and date of discharge. Exact patient discharge times were not available, so all discharge times were recorded as 12:00pm. For patients with partial days in their LOS, we rounded to the nearest whole number. Patients were categorized into four groups based on hospital LOS: (1) ≤2 days, (2) 3–4 days, (3) 5–7 days, or (4) ≥8 days. Patients were also grouped into the following six categories, based on the day of the week they were admitted: (1) Monday–Wednesday; (2) Thursday; (3) Friday morning (12:00am–<12:00pm); (4) Friday afternoon or evening (12:00pm–<12:00am); (5) Saturday; or (6) Sunday. Major bleeding was defined as an absolute hemoglobin (Hgb) drop of ≥4 g/dL, intracranial hemorrhage (ICH), witnessed retroperitoneal bleeding, red blood cell (RBC) transfusion in a patient with a baseline Hgb ≥9 g/dL, or an RBC transfusion with a witnessed bleeding event in a patient with a baseline Hgb of <9g/dL. In-hospital complications were defined as post-admission reinfarction, cardiogenic shock, heart failure, stroke, major bleeding, or blood transfusion. Early cardiac catheterization and percutaneous coronary intervention (PCI) were defined as occurring within 48 hours. All other variables are defined on the NCDR web site (www.ncdr.com/WebNCDR/ACTION/Elements.aspx).
Statistical Analysis
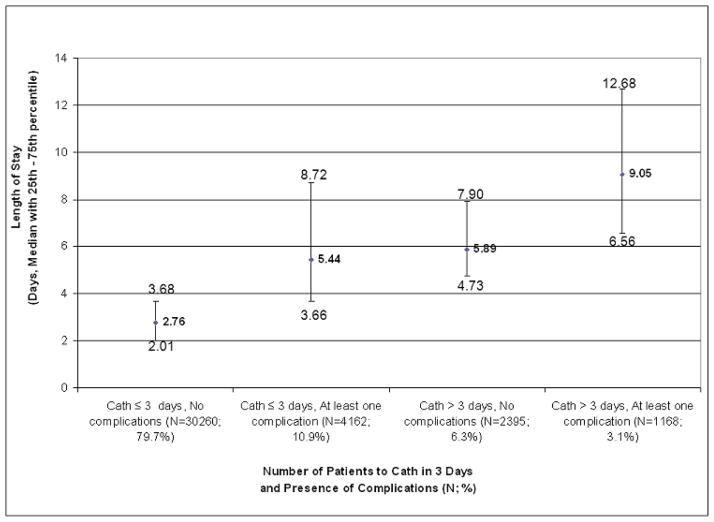
Demographic information, co-existing medical comorbities on admission, presenting signs and symptoms, electrocardiogram (ECG) findings, acute (≤24 hour of hospital arrival) and discharge medications received, time from hospital presentation to ECG, time from hospital presentation to cardiac catheterization and PCI, in-hospital procedures, in-hospital clinical events, and hospital characteristics, were stratified by four LOS categories. Treatments such as acute and discharge medications and procedures were only considered among those without a documented contraindication. Continuous variables were reported as median values (with 25th, 75th percentiles) and categorical values were reported as percentages. Chi-square tests were used to compare categorical variables and the Kruskal-Wallis test was used for continuous variables. Distribution of LOS was displayed in a histogram (Figure 1).
Figure 1. Distribution of LOS.
This figure displays the distribution of LOS in days as a percentage of the entire population studied.
To explore factors associated with prolonged LOS (defined as >4 days vs. ≤4 days), a logistic generalized estimating equations (GEE) method was used with exchangeable working correlation matrix to account for within-hospital clustering. This method produced estimates similar to those from logistic regression, but variances were adjusted for the correlation of outcomes within a hospital.11 Variables in the model were selected based on clinical input.
Statistical significance was defined as p<0.05. All analyses were conducting using SAS software version 9.2 (SAS Institute, Cary, NC).
RESULTS
Baseline Characteristics
For the 39,107 patients with NSTEMI in our analysis cohort, the median age overall was 64 (54, 75) years. Women made up 37.0% of the population and 82.1% of patients were Caucasian. The median LOS (25th, 75th) for the overall cohort in our study population was 3 (2, 5) days and the distribution of LOS is displayed in Figure 1. There were 13,047 (33.4%) patients with LOS ≤2 days; 15,870 (40.6%) with LOS 3–4 days; 6,325 (16.1%) with LOS 5–7 days; and 3,865 (9.9%) with LOS ≥8 days. Twenty-six percent of patients had a LOS >4 days.
The patient baseline and hospital characteristics of our population categorized by LOS are displayed in Table 1. As LOS increased, patients were older, more often female, and less frequently Caucasian. In addition, as LOS increased, patients more frequently presented with heart failure symptoms and ST-segment depression on the initial ECG. They also had an increased number of co-morbidities, including a history of prior MI, heart failure, hypertension, atrial fibrillation, CABG, stroke, or peripheral arterial disease. Patients with longer hospital LOS presented with higher serum creatinine levels, had higher peak serum creatinine levels, and were more likely to be on hemodialysis. These patients were also less likely to be current smokers.
Table 1.
Patient Baseline and Hospital Characteristics by LOS Category
| Overall (N=39,107) | ≤2 days (N=13,047) 33.4% | 3–4 days (N=15,870) 40.6% | 5–7 days (N=6,325) 16.1% | ≥8 days (N=3,865) 9.9% | p-value | |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age (years)* | 64 (54, 75) | 60 (51, 70) | 63 (53, 74) | 70 (60, 79) | 73 (63, 80.5) | <0.0001 |
| BMI (kg/m2)* | 28.7 (25.2, 33.1) | 29.1 (25.7, 33.3) | 28.9 (25.5, 33.2) | 28.3 (24.6, 32.8) | 28.0 (24.1, 32.8) | <0.0001 |
| Female Sex | 37.0 | 31.3 | 36.0 | 45.1 | 47.3 | <0.0001 |
| Hospital characteristics | ||||||
| Non-academic hospital† | 75.1 | 77.0 | 75.0 | 73.9 | 71.2 | <0.0001 |
| Total hospital beds* | 409 (281, 604) | 390 (274, 570) | 410 (281, 612) | 411 (283, 612) | 426 (294, 621) | <0.0001 |
| Urban setting | 92.2 | 92.2 | 91.9 | 92.3 | 93.5 | 0.0103 |
| Region | ||||||
| West | 14.9 | 18.8 | 13.0 | 12.1 | 14.0 | <0.0001 |
| Northeast | 9.5 | 7.0 | 10.0 | 11.5 | 12.5 | |
| Midwest | 36.5 | 39.0 | 34.7 | 35.7 | 36.0 | |
| South | 39.2 | 35.1 | 42.3 | 40.7 | 37.6 | |
| Race | <0.0001 | |||||
| Caucasian | 82.1 | 85.5 | 81.3 | 79.6 | 77.8 | |
| Black | 10.9 | 7.9 | 11.7 | 13.2 | 14.3 | |
| Asian | 1.3 | 1.2 | 1.3 | 1.2 | 1.8 | |
| Hispanic | 4.0 | 3.5 | 4.1 | 4.5 | 4.6 | |
| Medical history | ||||||
| Current smoker | 32.4 | 37.5 | 33.4 | 26.3 | 20.8 | <0.0001 |
| Hypertension | 73.9 | 68.3 | 72.8 | 82.2 | 83.4 | <0.0001 |
| Dyslipidemia | 62.5 | 61.7 | 61.8 | 65.1 | 64.2 | <0.0001 |
| Diabetes | 32.6 | 24.7 | 30.7 | 41.9 | 51.7 | <0.0001 |
| Currently on dialysis | 2.6 | 0.9 | 2.1 | 4.5 | 7.3 | <0.0001 |
| History of | ||||||
| MI | 28.6 | 25.1 | 27.9 | 34.0 | 34.1 | <0.0001 |
| Heart failure | 12.1 | 5.4 | 9.8 | 20.6 | 29.7 | <0.0001 |
| AF | 7.4 | 3.6 | 6.3 | 12.3 | 17.3 | <0.0001 |
| PCI | 28.7 | 28.7 | 28.3 | 29.6 | 29.4 | 0.18 |
| CABG | 20.6 | 16.1 | 20.2 | 26.5 | 27.7 | <0.0001 |
| Stroke | 7.6 | 4.5 | 6.5 | 11.6 | 15.4 | <0.0001 |
| PAD | 10.6 | 7.1 | 9.1 | 15.5 | 20.8 | <0.0001 |
| Signs and symptoms at presentation | ||||||
| Heart failure | 14.4 | 5.1 | 11.1 | 25.7 | 40.4 | <0.0001 |
| Shock | 0.9 | 0.2 | 0.4 | 1.2 | 4.4 | <0.0001 |
| Heart rate (bpm)* | 81 (70, 96) | 78 (68, 91) | 80 (69, 94) | 86 (72, 103) | 91 (76, 109) | <0.0001 |
| Systolic blood pressure (mmHg)* | 148 (129, 168) | 149 (131, 168) | 149 (130, 169) | 145 (125, 167) | 140 (118, 164) | <0.0001 |
| Renal function | ||||||
| Initial creatinine value (mg/dL) [non-dialysis pts]* | 1.00 (0.90, 1.30) | 1.00 (0.80, 1.20) | 1.00 (0.90, 1.20) | 1.10 (0.90, 1.40) | 1.30 (1.00, 1.70) | <0.0001 |
| Peak creatinine value (mg/dL) [non-dialysis pts]* | 1.10 (0.90, 1.40) | 1.00 (0.90, 1.20) | 1.10 (0.90, 1.30) | 1.20 (1.00, 1.60) | 1.60 (1.20, 2.30) | |
| ECG findings (NSTEMI) | <0.0001 | |||||
| ST depression | 10.8 | 9.1 | 10.9 | 12.8 | 13.2 | |
| Transient ST elevation | 1.7 | 2.0 | 1.7 | 1.3 | 1.1 | |
Continuous variables displayed as median values with 25th, 75th percentiles.
Member of the Council of Teaching Hospitals.
AF=atrial fibrillation; BMI=body mass index; bpm=beats per minute; CABG=coronary artery bypass grafting; ECG=electrocardiogram; MI=myocardial infarction; NSTEMI=non-ST-segment elevation myocardial infarction; PAD=peripheral artery disease; PCI=percutaneous coronary intervention; pts=patients
Patients with higher LOS were more likely to be treated at an academic medical center, and at centers with larger bed volumes. Urban versus rural setting of the hospital did not seem to be associated with LOS (Table 1).
Medication Use by LOS
In the absence of documented contraindications, the administration of medications to treat acute coronary syndromes within 24 hours is shown in Table 2 for each category of LOS, as well as the use of anticoagulants at any time during the hospitalization. Table 3 shows discharge medications by LOS category. In general, patients with longer LOS were less likely to be treated with evidence-based medications during the hospitalization and at the time of discharge.
Table 2.
Medications within 24 Hours or Anytime* by LOS Category
| Overall (N=39,107) | ≤2 days (N=13,047) | 3–4 days (N=15,870) | 5–7 days (N=6,325) | ≥8 days (N=3,865) | p-value | |
|---|---|---|---|---|---|---|
| Aspirin | 97.6 | 98.5 | 98.2 | 96.0 | 95.0 | <0.0001 |
| Clopidogrel | 67.2 | 77.1 | 66.6 | 56.7 | 51.8 | <0.0001 |
| Beta-blocker | 91.8 | 92.5 | 92.6 | 90.6 | 87.7 | <0.0001 |
| ACE inhibitor or ARB | 51.5 | 51.7 | 52.4 | 52.7 | 44.7 | <0.0001 |
| Statin | 63.0 | 68.2 | 62.8 | 58.7 | 53.0 | <0.0001 |
| GPIIb/IIIa | 43.8 | 48.8 | 47.0 | 33.8 | 28.4 | <0.0001 |
| Any heparin* | 88.6 | 86.8 | 90.4 | 88.5 | 87.9 | <0.0001 |
| UFH* | 61.9 | 62.1 | 62.0 | 60.1 | 63.5 | <0.0001 |
| LMWH* | 36.9 | 31.9 | 38.7 | 41.1 | 39.3 | <0.0001 |
| Bivalirudin* | 20.9 | 22.4 | 20.2 | 20.4 | 19.6 | <0.0001 |
| Fondaparinux* | 0.2 | 0.2 | 0.2 | 0.2 | 0.5 | 0.01 |
Denotes administered anytime during the hospitalization
ACE=angiotensin-converting enzyme; ARB=angiotensin receptor blocker; GPIIb/IIIa=glycoprotein IIb/IIIa; LMWH=low molecular weight heparin; UFH=unfractionated heparin
Table 3.
Discharge Medications by LOS Category
| Overall (N=39,107) | ≤2 days (N=13,047) | 3–4 days (N=15,870) | 5–7 days (N=6,325) | ≥8 days (N=3,865) | p-value | |
|---|---|---|---|---|---|---|
| Aspirin | 97.6 | 97.9 | 97.9 | 97.0 | 95.8 | <0.0001 |
| Clopidogrel | 84.9 | 86.7 | 87.0 | 80.7 | 76.0 | <0.0001 |
| Coumadin | 7.7 | 3.0 | 6.4 | 13.8 | 18.7 | <0.0001 |
| Beta-blocker | 95.2 | 94.2 | 96.1 | 95.3 | 94.3 | <0.0001 |
| ACE inhibitor or ARB | 73.0 | 70.1 | 74.9 | 75.6 | 70.8 | <0.0001 |
| Statin | 89.6 | 90.9 | 90.8 | 87.3 | 83.0 | <0.0001 |
Clopidogrel use in the first 24 hours after presentation was 77.1% in the ≤2 days group, 66.6% in the 3–4 days group, 56.7% in the 5–7 days group, and 51.8% in the ≥8 days group (p<0.0001 for all comparisons). This pattern was also generally true for aspirin, beta-blockers, angiotensin converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARBs), and statins. The use of anticoagulants such as unfractionated heparin, low molecular weight heparin, bivalirudin, or fondaparinux differed to a lesser degree (Table 2).
Patients who had longer LOS were also less likely to be discharged home on evidence-based medications. Those with the longest LOS (≥8 days) were the least likely to be discharged home on aspirin (95.8%), clopidogrel (76.0%), or a statin (83.0%); p<0.0001 for all comparisons among LOS groups for each medication (Table 3).
In-hospital Procedures, Complications, and Delays to Cardiac Catheterization
Longer LOS was associated with higher rates of clinical complications, less use of PCI, and longer delays to cardiac catheterization and PCI when they were performed (Table 4). Patients with LOS ≥8 days had the highest rates of MI (2.5%), shock (7.6%), heart failure (18.3%), stroke (2.1%), or major bleeding (38.8%) compared with all other groups; p<0.0001. Nevertheless, patients with LOS ≥8 days were the least likely to receive early cardiac catheterization or PCI (53.7%), and were most likely to receive a noninvasive stress test; p<0.0001 for all comparisons. Furthermore, if they did receive cardiac catheterization or PCI, they had the longest delays in time from presentation to cardiac catheterization (49.3 hours, interquartile range [IQR] 19.2, 110.0) or PCI (55.0 hours, IQR 18.4, 131.6) (Table 4).
Table 4.
In-hospital Procedures and Complications by LOS Category
| Overall (N=39,107) | ≤2 days (N=13,047) | 3–4 days (N=15,870) | 5–7 days (N=6,325) | ≥8 days (N=3,865) | p-value | |
|---|---|---|---|---|---|---|
| In-hospital procedures | ||||||
| Noninvasive stress test | 4.2 | 2.7 | 3.9 | 6.6 | 6.8 | <0.0001 |
| Cath within 48 hours of arrival | 79.5 | 99.1 | 80.6 | 54.8 | 48.9 | <0.0001 |
| PCI | 66.0 | 70.3 | 68.2 | 58.9 | 53.7 | <0.0001 |
| PCI within 48 hours of arrival | 53.7 | 70.0 | 56.1 | 31.7 | 25.0 | <0.0001 |
| Time from presentation to: | ||||||
| Cath (hours)* | 21.1 (8.7, 42.0) | 13.9 (4.5, 22.3) | 23.0 (11.7, 43.5) | 42.2 (17.2, 73.5) | 49.3 (19.2, 110.0) | <0.0001 |
| PCI (hours)* | 19.8 (6.7, 38.5) | 12.2 (4.3, 21.5) | 22.2 (10.1, 42.3) | 42.5 (16.0, 78.2) | 55.0 (18.4, 131.6) | <0.0001 |
| Clinical complications | ||||||
| MI | 0.9 | 0.3 | 0.7 | 1.5 | 2.5 | <0.0001 |
| Cardiogenic shock | 1.2 | 0.2 | 0.4 | 1.7 | 7.6 | <0.0001 |
| CHF | 4.5 | 1.0 | 2.8 | 7.9 | 18.3 | <0.0001 |
| Stroke | 0.4 | 0.0 | 0.2 | 0.6 | 2.1 | <0.0001 |
| Overall RBC transfusion | 6.2 | 0.6 | 2.5 | 11.7 | 31.3 | <0.0001 |
| Overall major bleeding | 8.6 | 1.1 | 4.6 | 15.9 | 38.8 | <0.0001 |
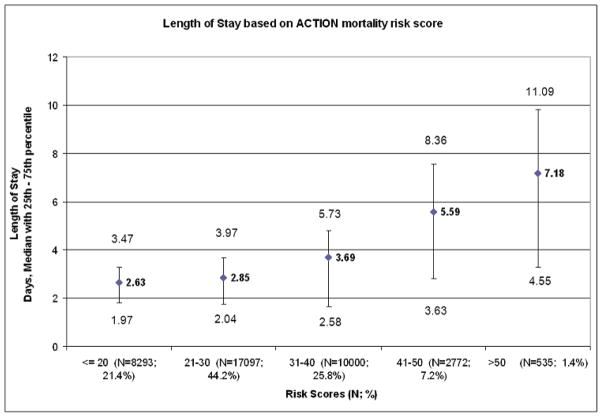
Delays to cardiac catheterization and the presence of complications were both associated with longer LOS (Figure 2). Almost 85% of patients (n=33,010) had no complications. Less than 2% had three or more complications. Moreover, approximately 90% of patients (n=35,037) went to the catheterization lab within three days. The shortest LOS was among those patients with no complications who went to the catheterization lab within three days. The longest LOS was in those patients with at least one complication who went to the catheterization lab after three days. Irrespective of complications, LOS was longer in the cohort who got catheterized after three days, as compared to those who got catheterized within three days (6.66 vs. 2.89, respectively).
Figure 2. Length of Stay based on Time to Catheterization and Occurrence of Complications.
This figure displays the median LOS based on whether or not the patients had cardiac catheterization within three days of admission, or at least one complication. Regardless of the presence of complications, those who received cardiac catheterization after three days from admission had a longer hospital LOS.
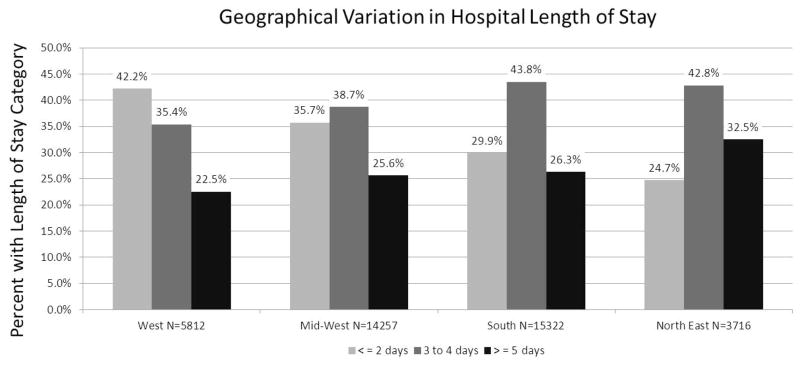
The risk of mortality calculated by the ACTION Registry-GWTG mortality risk score was also positively associated with hospital LOS.12 Figure 3 demonstrates that as the risk increases, there is a consistent increase in LOS.
Figure 3. Length of Stay based on ACTION Registry-GWTG Mortality Risk Score.
There is a consistent trend of increased LOS with increased mortality risk, based on the ACTION Registry-GWTG mortality risk score.
Day of Week Admitted to the Hospital and LOS
Depicted in Table 5 is the time to cardiac catheterization and hospital LOS based on the day of the week admitted to the hospital. Admission to the hospital on a Friday afternoon or evening was studied for its association with prolonged LOS as a way to describe possible delays in care from the upcoming weekend. Those admitted on a Friday afternoon or evening had the longest delays to catheterization (58.5 [13.8–67.1] hours) and longest LOS (3.8 [2.8–4.9] days). While those admitted on Friday morning had a very short time to catheterization (10.6 [4.5–72.0] hours), but this did not translate to earlier discharge (3.5 [2.2–5.1] days).
Table 5.
Arrival to Catheterization Lab and LOS Based on Day and Time of Hospital Admission
| Time of presentation | Number of patients (%) | Median (25th–75th) time to cath lab (hrs) | Median (25th–75th) LOS (days) |
|---|---|---|---|
| Friday afternoon or evening* | 3038 (7.8%) | 58.5 (13.8–67.1) | 3.8 (2.8–4.9) |
| Monday–Wednesday* | 17652 (45.1%) | 19.5 (7.8–31.4) | 2.8 (2.0–4.2) |
| Thursday | 5429 (13.9%) | 17.8 (7.1–26.6) | 3.0 (2.0–4.8) |
| Saturday | 5350 (13.7%) | 41.1 (13.9–52.5) | 3.3 (2.7–4.7) |
| Sunday | 5288 (13.5%) | 23.2 (13.2–36.5) | 3.0 (2.2–4.3) |
| Friday morning | 2350 (6.0%) | 10.6 (4.5–72.0) | 3.5 (2.2–5.1) |
Factors Associated with Prolonged Length of Stay
Baseline demographic, clinical factors, and hospital features associated with prolonged LOS (>4 days vs. ≤4 days) are displayed in Table 6. The factors most strongly associated with LOS >4 days in the adjusted model were undergoing cardiac catheterization >48 hours after presentation (odds ratio [OR] 4.87; 95% confidence interval [CI]: 4.54–5.22), shock at presentation (OR 7.82; 95% CI: 6.01–10.17), or heart failure without shock (OR 2.09; 95% CI: 1.93–2.26). Older age was also strongly associated with LOS >4 days with an OR of 1.14 (95% CI: 1.13–1.16) per every 5-year increase in age.
Table 6.
Factors Associated with Prolonged LOS (>4 days vs. ≤4 days)*
| Variable | OR | 95% CI | Chi-square | P-value |
|---|---|---|---|---|
| Catheterization >48 hrs (vs. ≤48 hrs) | 4.87 | 4.54 – 5.22 | 1953 | <.0001 |
| HF only on admission (vs. none) | 2.09 | 1.93 – 2.26 | 518 | <.0001 |
| Shock only or HF with shock on admission (vs. none) | 7.82 | 6.01 – 10.17 | ||
| Age (per 5 year increase) | 1.14 | 1.13 – 1.16 | 338 | <.0001 |
| Baseline Hgb (per 1 g/dL decrease & Hgb <15 g/dL) | 1.18 | 1.16 – 1.20 | 279 | <.0001 |
| Baseline Hgb (per 1 g/dL increase & Hgb ≥15 g/dL) | 1.04 | 0.99 – 1.09 | ||
| HR (per 10 bpm decrease & HR <70 bpm) | 1.08 | 1.01 – 1.14 | 263 | <.0001 |
| HR (per 10 bpm increase & HR ≥70 bpm) | 1.12 | 1.11 – 1.14 | ||
| Baseline troponin (per 5 xULN increase) | 1.03 | 1.03 – 1.04 | 178 | <.0001 |
| Fri morning (vs. Mon–Wed) | 0.97 | 0.86 – 1.09 | 156 | <.0001 |
| Fri afternoon or evening (vs. Mon–Wed) | 1.13 | 1.02 – 1.25 | ||
| Sat (vs. Mon–Wed) | 0.88 | 0.81 – 0.96 | ||
| Sun (vs. Mon–Wed) | 0.97 | 0.90 – 1.06 | ||
| Thurs (vs. Mon–Wed) | 1.50 | 1.40 – 1.61 | ||
| Baseline serum creatinine (per 1 mg/dL increase) | 1.18 | 1.15 – 1.22 | 120 | <.0001 |
| SBP (per 10 mmHg decrease & SBP <160 mmHg) | 1.07 | 1.05 – 1.09 | 78 | <.0001 |
| SBP (per 10 mmHg increase & SBP ≥160 mmHg) | 1.01 | 0.99 – 1.04 | ||
| Medicaid (vs. HMO/private) | 1.57 | 1.37 – 1.79 | 69 | <.0001 |
| Medicare (vs. HMO/private) | 1.19 | 1.12 – 1.27 | ||
| Other insurance (vs. HMO/private) | 1.07 | 0.86 – 1.33 | ||
| Self/none (vs. HMO/private) | 1.23 | 1.09 – 1.39 | ||
| Diabetes mellitus | 1.29 | 1.21 – 1.37 | 61 | <.0001 |
| Prior HF | 1.33 | 1.24 – 1.43 | 59 | <.0001 |
| Prior stroke | 1.41 | 1.27 – 1.56 | 45 | <.0001 |
| Prior PCI | 0.82 | 0.77 – 0.88 | 29 | <.0001 |
| Prior PAD | 1.24 | 1.14 – 1.34 | 25 | <.0001 |
| Weight (per 5 kg decrease & weight <100 kg) | 1.02 | 1.01 – 1.03 | 16 | 0.0004 |
| Weight (per 5 kg increase & weight ≥100 kg) | 1.02 | 1.00 – 1.03 | ||
| Female (vs. male) | 1.13 | 1.06 – 1.20 | 14 | 0.0001 |
| Prior MI | 1.11 | 1.04 – 1.18 | 12 | 0.0007 |
| Hypertension | 1.11 | 1.04 – 1.19 | 10 | 0.0020 |
| Total # of beds (per 100 beds increase) | 1.03 | 1.00 – 1.05 | 4 | 0.0370 |
Race, history of prior CABG, rural vs. urban location of the hospital, current/recent smoker, and academic vs. non-academic hospital are included in this model but not displayed, as they were not statistically significant in the adjusted model.
CI=confidence interval; Fri=Friday; HF=heart failure; Hgb=hemoglobin; HMO=health maintenance organization; HR=heart rate; Mon–Wed=Monday–Wednesday; OR=odds ratio; PAD=peripheral arterial disease; Sat=Saturday; SBP=systolic blood pressure; Sun=Sunday; Thurs=Thursday; All other abbreviations can be found in Tables 1–5.
As compared to admission to the hospital on a Monday–Wednesday, admission on a Friday afternoon or evening (OR 1.13; 95% CI: 1.02–1.25) or on a Thursday (OR 1.50; 95% CI: 1.40–1.61) was associated with LOS >4 days. Those patients admitted to the hospital on a Saturday were less likely to have a prolonged LOS (OR 0.88; 95% CI: 0.81–0.96) when compared to those admitted to the hospital Monday–Wednesday.
Other comorbidities such as anemia, prior MI, diabetes, heart failure, stroke, peripheral arterial disease, and hypertension all were linked to LOS >4 days. Patients with a history of prior PCI were less likely to have prolonged LOS (OR 0.82; 95% CI: 0.77–0.88). Additionally, patients with private/HMO insurance were also less likely to have a prolonged LOS as compared to patients with all other types of insurance (Medicare, Medicaid), or no insurance at all (none/self-pay). Treatment at an academic medical center versus a non-academic center, a rural hospital versus an urban setting hospital, race of the patient, smoking status, and a history of CABG were variables tested and not associated with a prolonged LOS >4 days (Table 6).
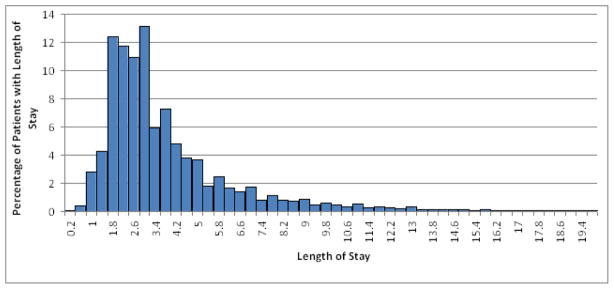
Geographical Variations in Hospital Length of Stay
Shown in Figure 4 are the differences in hospital LOS among four regions in the U.S. The Northeast appears to have the highest percentage of patients with an LOS of at least five days. On the other hand, the West appears to have the lowest percentage of those with LOS ≥5 days and the highest percentage of those with the shortest LOS ≤2 days. The median (25th, 75th) LOS were significantly different among the regions, although only to a mild degree. The shortest LOS was in the West region at 2.77 days (1.98–4.14), while the longest LOS was in the Northeast at 3.34 (2.52–5.14). The South had a median LOS of 3.10 days (2.22–4.63) and the Midwest had a median LOS of 2.97 (2.08–4.56); p<0.0001 for all comparisons.
Figure 4. Geographical Variation in Hospital Length of Stay.
There are important variations in the lengths of stay based on geographical variations in the U.S. The Northeast has highest percentage of patients with LOS ≥5 days, while the West has the highest percentage of patients with LOS ≤2 days and the lowest percentage with LOS ≥5 days.
DISCUSSION
This study examined national patterns of hospital LOS for over 39,000 NSTEMI patients in the ACTION Registry-GWTG. In our analysis, we found that, as expected, patients with longer LOS were older, more likely to have comorbidities and in-hospital complications, and were at a higher calculated baseline risk of death. However, these patients were less often treated with evidence-based medications despite a lack of documented contraindications and were less likely to receive cardiac catheterization or PCI within 48 hours, or PCI in general. We also found that hospital admission on a Friday afternoon or evening and delays to cardiac catheterization were among the factors most highly associated with prolonged LOS. Interestingly, hospital characteristics such as an academic medical center versus non-academic center, and a rural versus urban setting had no association with LOS after adjusting for other variables in the model. However, there does appear to be a geographic variation in LOS for reasons that are not clearly defined.
Despite higher incidences of heart failure, cardiogenic shock, and in-hospital MI, those with the longest LOS were less likely to receive cardiac catheterization or PCI within the first 48 hours of hospital admission and were more likely to undergo noninvasive stress testing. Paradoxically, the Timing of Intervention in Patients with Acute Coronary Syndromes (TIMACS) study, which evaluated an early intervention therapy versus a delayed intervention strategy, demonstrated that those patients with the highest mortality risk derive the most benefit from an early interventional strategy.13 In this study, the one-third of patients with the highest risk (Global Registry of Acute Coronary Events [GRACE] score >140) comprised the only subgroup that showed a significant reduction in the primary composite endpoint of death, MI, or stroke at six months when early intervention was implemented. These studies highlight the risk-treatment mismatch that is common in medicine.
Admission on a Friday and Prolonged LOS
This analysis suggests that those patients admitted on a Friday after 12:00pm have the longest delays to cardiac catheterization and longest LOS. This fact is presumably due to the upcoming weekend and reduced services available in most U.S. hospitals on Saturday and Sunday. Interestingly, those admitted on Friday morning had the shortest delays to cardiac catheterization, but also had the second longest LOS, behind only the Friday afternoon or evening group. This may reflect that there is a push to perform the cardiac catheterization before the upcoming weekend when a patient is admitted on a Friday morning, but that discharges are still delayed because of the weekend. A better understanding of the impact of diminished weekend services on discharge patterns could provide important insights into areas for improved healthcare resource utilization. For example, would routinely performing cardiac catheterizations during the weekend reduce hospital LOS? Would this be cost-effective? Although our study raises this possibility, this important question remains to be answered.
Importance of Understanding Factors Associated with LOS
There is substantial heterogeneity in the patient population admitted for NSTEMI, which was related to wide variations in hospital LOS. Little is known about the factors that influence hospital LOS in NSTEMI. In an era of increasing pressure to save costs and focus on efficient use of resources, there is an important need to better understand factors that contribute to prolonged hospital stays and to appropriately limit their influence. Identifying the characteristics that predict LOS may provide insight into methods to reduce them in a safe manner. Older age was an important predictor of longer LOS in our population, and may in part be explained by the delays to catheterization and less use of PCI. Other studies have demonstrated similar trends with the use of cardiac catheterization among older patients. In an Italian population, the BLITZ-2 study surveyed the epidemiology and management strategies of non-ST-segment elevation acute coronary syndrome (NSTE ACS) in the Italian cardiological network and demonstrated that older patients were significantly less likely to undergo cardiac catheterization.14 Analysis of data from the international trials Sibrafiban versus Aspirin to Yield Maximum Protection from Ischemic Heart Events Post-acute Coronary Syndromes (SYMPHONY) and 2nd SYMPHONY found similar results. Both trials demonstrated that patients over 75 years old were significantly less likely to undergo cardiac catheterization, when compared to younger patients.15
These findings raise the question as to whether a strategy of earlier cardiac catheterization could result in a reduction in LOS for patients admitted with NSTEMI. There are many reasons why older patients with prolonged LOS and increases in in-hospital complications may not receive cardiac catheterization at all. Some of these reasons may include patient or family preference, increased risk of the procedure, or perceived lack of benefit. It is unclear whether or not a more aggressive strategy to perform cardiac catheterization on a higher portion of these patients would translate into a decreased LOS. However, for those in whom cardiac catheterization is felt to be appropriate, decreasing the time from admission to cardiac catheterization may result in shorter hospital stays.
Cardiogenic shock and heart failure on presentation were the factors most strongly associated with prolonged LOS, and keeping this high-risk population in the hospital for longer may be entirely appropriate. In part, prolonged LOS for this subgroup of patients is due to the heterogeneity of heart failure and shock in NSTEMI, which is rarely due to focal coronary lesions and is confounded by age and end organ dysfunction.
Length of Stay and Evidence-based Treatment
A better understanding is needed of our observation that there is a decreased use of evidence-based medications in patients with longer LOS who had more comorbidities and in-hospital complications. This finding is not inconsistent with previously published data. Wang et al. demonstrated that patients who experience bleeding complications after PCI are less likely to be discharged home on appropriated antiplatelet medications, and that this discrepancy continues well after the bleeding event for at least six months.16 Cohen et al. evaluated the racial and ethnic differences in the treatment of MI in 443 hospitals participating in the GWTG-CAD program and found that not only was the use of evidence-based medicines high in this group, but it continued to improve over the 5-year duration of the study.17 Importantly, studies have demonstrated that participation in systematic processes (such as the ACTION Registry-GWTG from which this study is conducted) is associated with improved adherence to evidence-based medicines. Nevertheless, efforts to better characterize medication use in this particularly vulnerable cohort, as well as increase the use of evidence-based medications where appropriate, are needed.
Limitations
The ACTION Registry-GWTG provides retrospective observational data and, therefore, has a number of limitations. First, data are collected during acute hospitalizations only and do not provide longitudinal follow-up. Thus, we cannot examine the association of LOS with post-hospital outcomes. Second, exact discharge times were not available. Since most patients are discharged during daytime business hours, we assumed a discharge time of 12:00pm for all patients. As opposed to using strictly the dates of admission and discharge, it was felt that this would minimize the amount of error in calculating LOS for those admitted late in the day. Third, as in any registry, there is an inherent selection bias. Data comes from a heterogeneous mixture of hospitals that vary in the services and types of procedures they can provide. In an attempt to overcome this limitation, we restricted our analysis to only patients who received cardiac catheterization at the facility to which they initially presented, with the understanding that this would exclude all patients medically managed for NSTEMI and those transferred for cardiac catheterization. We used statistical methods to account for hospital characteristics and within hospital correlation. Restricting our population to patients undergoing cardiac catheterization also served to focus on patients for whom the care team was more convinced that the patient had true acute coronary syndrome, but with enough functionality to justify an invasive approach. Finally, the data collected in this registry captures contraindications to treatment and allows for exclusion of those patients in these analyses; however, relative or undocumented contraindications are not captured and cannot be accounted for.
CONCLUSIONS
This is one of the largest studies ever performed to examine the characteristics of patients admitted with NSTEMI and their association with hospital LOS. Patients with longer LOS were older and had more comorbidities and in-hospital complications, but were less likely to receive evidence-based medications and had delays in cardiac catheterization. Additionally, hospital admission on a Friday afternoon or evening and delays to cardiac catheterization were associated with prolonged LOS. A considerable amount of the heterogeneity was not accounted for by these variables, supporting the concept that there may be the opportunity to reduce LOS by simply applying consistent practice. Applying the results of this study to drive the development of processes to reduce heterogeneity in hospital LOS and associated treatment disparities in NSTEMI patients, as well as to promote safe and early discharge in an era of increasingly restrictive healthcare resources, should lead to more appropriate and efficient care.
Acknowledgments
Funding Sources: The ACTION Registry®-GWTG™ is an initiative of the American College of Cardiology Foundation and the American Heart Association, with partnering support from Society of Chest Pain Centers, The Society of Hospital Medicine, and The American College of Emergency Physicians. The registry is sponsored by Bristol-Myers Squibb/Sanofi Pharmaceuticals.
This project received infrastructure support from grant number U18HS010548 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
The authors would like to thank Erin LoFrese for her editorial contributions to this manuscript. Ms. LoFrese did not receive compensation for her contributions, apart from her employment at the institution where this study was conducted.
Footnotes
Author Verification Statement: All authors had access to the data and a role in writing the manuscript.
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Newby LK, Eisenstein EL, Califf RM, Thompson TD, Nelson CL, Peterson ED, Armstrong PW, Van de Werf F, White HD, et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. N Engl J Med. 2000;342:749–755. doi: 10.1056/NEJM200003163421101. [DOI] [PubMed] [Google Scholar]
- 3.Topol EJ, Burek K, O’Neill WW, et al. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N Engl J Med. 1988;318:1083–1088. doi: 10.1056/NEJM198804283181702. [DOI] [PubMed] [Google Scholar]
- 4.Mark DB, Sigmon K, Topol EJ, et al. Identification of acute myocardial infarction patients suitable for early hospital discharge after aggressive interventional therapy. Results from the Thrombolysis and Angioplasty in Acute Myocardial Infarction Registry. Circulation. 1991;83:1186–1193. doi: 10.1161/01.cir.83.4.1186. [DOI] [PubMed] [Google Scholar]
- 5.Newby LK, Califf RM, Guerci A, et al. Early discharge in the thrombolytic era: an analysis of criteria for uncomplicated infarction from the Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO) trial. J Am Coll Cardiol. 1996;27:625–632. doi: 10.1016/0735-1097(95)00513-7. [DOI] [PubMed] [Google Scholar]
- 6.Every NR, Spertus J, Fihn SD, et al. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J Am Coll Cardiol. 1996;28:287–293. doi: 10.1016/0735-1097(96)00168-4. [DOI] [PubMed] [Google Scholar]
- 7.Grines CL, Marsalese DL, Brodie B, et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. PAMI-II Investigators. Primary Angioplasty in Myocardial Infarction. J Am Coll Cardiol. 1998;31:967–972. doi: 10.1016/s0735-1097(98)00031-x. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non ST-Elevation Myocardial Infarction): developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. Circulation. 2007;116:e148–304. doi: 10.1161/CIRCULATIONAHA.107.181940. [DOI] [PubMed] [Google Scholar]
- 9.Rogers S. ACTION Registry-GWTG Program Overview. [Accessed August 28, 2010];The National Cardiovascular Data Registry web site. http://www.ncdr.com/webncdr/ncdrdocuments/ACTION_v2_0_Program_Summary.pdf. Published December 2009.
- 10.Peterson ED, Roe MT, Chen AY, et al. The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 2010;96:1798–1802. doi: 10.1136/hrt.2010.200261. [DOI] [PubMed] [Google Scholar]
- 11.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 12.Chin CT, Chen AY, Wang TY, et al. Risk adjustment for in-hospital mortality of contemporary patients with acute myocardial infarction: the acute coronary treatment and intervention outcomes network (ACTION) registry-get with the guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. 2011;161:113–122. e2. doi: 10.1016/j.ahj.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Mehta SR, Granger CB, Boden WE, et al. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009;360:2165–2175. doi: 10.1056/NEJMoa0807986. [DOI] [PubMed] [Google Scholar]
- 14.Di Chiara A, Fresco C, Savonitto S, et al. Epidemiology of non-ST elevation acute coronary syndromes in the Italian cardiology network: the BLITZ-2 study. Eur Heart J. 2006;27:393–405. doi: 10.1093/eurheartj/ehi557. [DOI] [PubMed] [Google Scholar]
- 15.Alexander KP, Newby LK, Bhapkar MV, et al. International variation in invasive care of the elderly with acute coronary syndromes. Eur Heart J. 2006;27:1558–1564. doi: 10.1093/eurheartj/ehl067. [DOI] [PubMed] [Google Scholar]
- 16.Wang TY, Xiao L, Alexander KP, et al. Antiplatelet therapy use after discharge among acute myocardial infarction patients with in-hospital bleeding. Circulation. 2008;118:2139–2145. doi: 10.1161/CIRCULATIONAHA.108.787143. [DOI] [PubMed] [Google Scholar]
- 17.Cohen MG, Fonarow GC, Peterson ED, et al. Racial and ethnic differences in the treatment of acute myocardial infarction: findings from the Get With the Guidelines-Coronary Artery Disease program. Circulation. 2010;121:2294–2301. doi: 10.1161/CIRCULATIONAHA.109.922286. [DOI] [PubMed] [Google Scholar]