From the punch biopsy instrument to the most advanced laser systems, procedural dermatology has come of age. Many technologies are being developed as others become obsolete. Some perished giving way to more refined and sophisticated systems giving the procedural dermatologist a choice of treatments options whilst making them safer and more effective for the patients. Compared to a decade ago, it would be fair to say that today's procedural dermatologist is much better equipped.
Whilst, the old giving way to the new is the norm, it would also be fair to say that some technologies are here to stay. The good old carbon dioxide laser (CO2) may be one such system which has stood the test of time. Being one of the oldest laser technologies, the odds have always been against the CO2 laser. Notwithstanding, the downtime and post-procedural complications of scarring seen with the older generation continuous wave systems made them near-redundant.
One of the main attributes of this laser beam is that the thermal damage causes hemostasis thus offering the practitioner a bloodless field to operate on. The tissue can be incised by using a high-power, focussed beam which vaporizes the tissue in its immediate path.
The same laser beam can be scanned by rotating mirrors or computer programme generator. In doing so, the laser can deliver higher peak powers in pulsed durations which are shorter than the thermal relaxation time of the skin and this allows safer treatments. The pulsed or scanned CO2 laser beam results in ablation (or vaporization) of the epidermis and sometimes the superficial papillary dermis. This coupled with the thermal damage to a band of underlying dermis, to a depth of 150 μm instead of 400 μm as with the continuous wave beam limits the scarring potential. The resultant collagen denaturation and contraction and eventually upper dermal fibrosis are often referred to as “collagen remodelling”. This rejuvenation effect of the CO2 laser resurfacing approached those obtained by surgical face lift procedures, making it very popular in the 90's.
As the popularity of the laser for this indication has dwindled, search for alternative, less invasive and safer treatments led to development of Erbium: YAG laser. The Erbium: YAG achieves 5-15 μm of ablation per pass and a residual thermal damage of 15 μm which is one tenth of that achieved by the scanned CO2 laser beam. The advantages of the Erbium: YAG laser is faster healing and lesser complication at the expense of less impressive results and poor haemostasis.
Whilst, the safety prolife of these devices is favourable, the results are far from those that can be achieved by the CO2 laser, which set the bench mark against which the results of newer systems are measured. The CO2 laser is an excellent tool not only for rejuvenation but also for a variety of indications as listed in the table below:

Treatment planning and anaesthetic considerations
Informed consent for scarring, post-procedure redness, pallor and hyperpigmentation should be obtained in all cases. Pre-treatment photographs should be mandatory as should adequate sun protection before and after the treatment. CO2 laser treatments are painful, so nearly always require some form of anaesthesia. For small lesions such as milia, topical anaesthesia may be adequate. For other deeper and more ablative procedures, local infiltrative or regional or occasionally general anaesthesia may be preferred. As the treatment will generate laser plume, which may be contaminated causing infection risk, a vacuum suction device should be available. Barrier surgical masks which can filter laser plume should be worn. The post-procedure, topical emollients or barrier creams or antibiotic ointments may be prescribed. Oral antibiotics are rarely required but antiviral prophylaxis should be offered to patients with a history herpes simplex who are undergoing a resurfacing procedure. It would be advisable to avoid ablative resurfacing procedures for patients on isotretinoin, until such time guidance on this issue becomes clearer.
Laser procedure
Benign skin appendageal tumours and hyperplasia
My favoured technique to treat small lesions such as milia [Figures 1a and b], syringomas and sebaceous gland hyperplasia [Figures 2a and b] is to use the CO2 laser in the super pulse mode. This allows generation of high peak power in short durations thus causing disruption of the lesion whilst sparing the deeper dermis and surrounding epidermis. This beam can be used to puncture cysts or steatocystomas to enable evacuation of the contents.[1]
Figure 1.

Milia (a) before and (b) after carbon dioxide laser treatment
Figure 2.

Sebaceous gland hyperplasia (a) treated with superpulse-mode of carbon dioxide laser (b)
Resurfacing and bulk ablation
The fully ablative CO2 laser can improve the acne scarring and the laser heat induced collagen remodelling will improve the appearance of rhytides. Rhinophyma [Figures 3a and b] can be recontoured for cosmetic purposes and in order to relieve nasal obstruction.[2] Other dermatological conditions which can be ablated in this way include warts, granuloma faciale,[3,4] plaques of Hailey-Hailey and Darier's disease. Vulval lymphangiectasia/lymphangioma can be ablated to produce a degree of fibrosis thus preventing the recurrence. Non-infective, pruritic usually red ink tattoo granulomas which have failed to respond to potent topical or intralesional corticosteroids usually respond well when ablated with the CO2 laser.
Figure 3.
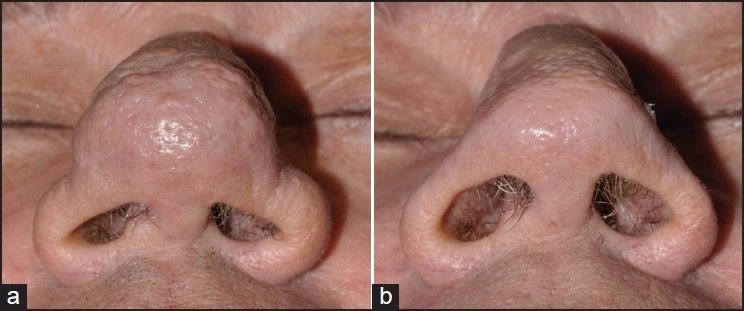
Excellent improvement in rhinophyma (a) following carbon dioxide laser treatment (b)
Cutting mode
The dermatologist will rarely use the CO2 laser in its cutting mode. The continuous beam of the laser can be used to produce a ‘dry’ incision to excise recurrent sinuses and nodules of hidradenitis. The dumb bell tumours of neurofibromas can also be excised similarly albeit at the expense of hypopigmented scars.[5]
Complications of CO2 laser treatment
The main concerns are infection, dyspigmentation, post-treatment erythema and scarring. The difficulty has been predicting the adverse response to the treatment, so laser test patches should be performed to guide the operator and the patient of the likely outcome. Whilst not always predictable when doing full treatments, laser test patches may provide worthwhile medicolegal protection, if needed. Greater the ablation depth, higher is the likelihood of an adverse effect. Permanent post-treatment pallor is one of the reasons for the decline in fully ablative CO2 laser resurfacing procedures in the Western world. The high risk of hyperpigmentation in patients with skin phototype IV onwards may explain the reluctance amongst dermatologists in using the CO2 laser for this patient subgroup.
Fractional CO2 laser
Both CO2 and Er: YAG laser systems have been fractionated and are largely used for cosmetic indications, principally acne scarring and wrinkles. Their use in non-cosmetic dermatology indications has not been fully explored.
In summary, whilst one acknowledges the limitations of the CO2 laser and continues to explore other modalities, for a true surgical dermatologist, there are few better cutting and ablative modalities than the CO2 laser.
REFERENCES
- 1.Madan V, August PJ. Perforation and extirpation of steatocystoma multiplex. Int J Dermatol. 2009;48:329–30. doi: 10.1111/j.1365-4632.2009.03904.x. [DOI] [PubMed] [Google Scholar]
- 2.Madan V, Ferguson JE, August PJ. Carbon dioxide laser treatment of rhinophyma: A review of 124 patients. Br J Dermatol. 2009;161:814–8. doi: 10.1111/j.1365-2133.2009.09317.x. [DOI] [PubMed] [Google Scholar]
- 3.Madan V. Recurrent granuloma faciale successfully treated with the carbon dioxide laser. J Cutan Aesthet Surg. 2011;4:156–7. doi: 10.4103/0974-2077.85050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakkour W, Madan V. Rhinophyma-like granuloma faciale successfully treated with the carbon dioxide laser. Br J Dermatol. 2013 doi: 10.1111/bjd.12649. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Chiang YZ, Al-Niaimi F, Ferguson J, August PJ, Madan V. Carbon Dioxide Laser Treatment of Cutaneous Neurofibromas. Dermatol Ther (Heidelb) 2012;2:7. doi: 10.1007/s13555-012-0007-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


