Abstract
A 20-year-old male presented with multiple eruptions on his right leg since birth; these bled and were painful on trivial trauma. Examination revealed dark brown, hyperkeratotic, indurated, verrucous linear plaques with irregular borders. Histopathological evidence of hyperkeratosis, acanthosis, and extensive vascular proliferation in papillary dermis confirmed clinical suspicion of angiokeratoma circumscriptum (AKC). Excision and skin grafting yielded a cosmetically favorable outcome. Angiokeratomas, first described by Mibeli in 1889, are a group of vascular ectasias involving the papillary dermis. Angiokeratomas are more common in males; however, AKC–the rarest of its five variants–exhibits a female preponderance (F:M:3:1). AKC is an extremely rare nevoid disorder, only 100 of its cases having been reported in the world literature until 2006. Herein, we have reported a typical case of AKC in a young male that was previously misdiagnosed, and the patient wrongly counseled about the likelihood of its spontaneous regression.
Keywords: Angiokeratoma circumscriptum, vascular malformation, verrucous hemangioma
Introduction
What was known?
Until 2006, only 100 cases had been reported in the world literature of AKC, the nevoid and the rarest of the five varieties of angiokeratomas. It is confirmed histopathologically by hyperkeratosis, papillomatosis, and acanthosis with its vascular proliferation restricted to the papillary dermis, the latter differentiating it from verrucous hemangioma whose vascular proliferation involves dermis and subcutaneous fat.
Angiokeratomas are ectasias of dermal capillaries with an acanthotic and hyperkeratotic overlying epidermis. These dark red to purple papular vascular anomalies can present as a wide range of lesions varying in size, depth, and location.[1] Based on the clinical presentation and evolution, five histopathologically similar variants have been identified. AKC, the rarest of the angiokeratomas, has been reported in about 100 cases in the world literature until 2006.[2,3] It is clinically characterized by hyperkeratotic, blue black, vascular plaque (s) commonly present on the lower limbs since birth in a segmental distribution. The diagnosis, readily suspected clinically by a combination of early onset and clinical appearance of aggregated papules forming a hyperkeratotic plaque, is confirmed by histopathological evidence of papillary vascular malformation with overlying hyperkeratosis and acanthosis. Lack of their spontaneous regression makes destruction of AKC mandatory by appropriate (diathermy, curettage, electrocautery, cryosurgery, deep excision followed by grafting, CO2/argon laser/KTP laser) modality.[4,5]
Case Report
A 20-year-old male presented to our department with the history of presence of multiple eruptions on his right leg since birth. These started as reddish-brown patches and became static after having initially increased in size proportional to the patient's growth. He complained of local pain and bleeding on trivial trauma. There was neither a personal history suggestive of any bleeding disorder nor occurrence of similar lesions in the family.
Skin examination revealed multple, linear,[6] dark red to brown, hyperkeratotic, warty plaques ranging from 2 × 3 cm to 7 × 5 cm with irregular borders on the shin of the right leg. On palpation, these were non-pulsatile, tender, slightly indurated, and non-compressible. Length and circumference of the legs were equal. No bruit was heard on auscultation.
Systemic examination revealed no abnormal findings. Routine lab investigations were normal. No bony defect was detected in X-ray of the legs. Ultrasonography revealed a linear hypodense circumscribed soft tissue mass without any relationship to the underlying bone. Doppler study did not reveal any altered blood flow.
Microscopic evaluation of the deep incisional biopsy specimen showed hyperkeratosis, acanthosis, and extensive papillary dermal vascular proliferation, thereby, confirming our clinical impression of AKC [Figure 1a and b]. He was referred to and managed by reconstructive surgeon via surgical excision, followed by skin grafting [Figures 2 and 3; Video 1].
Figure 1.
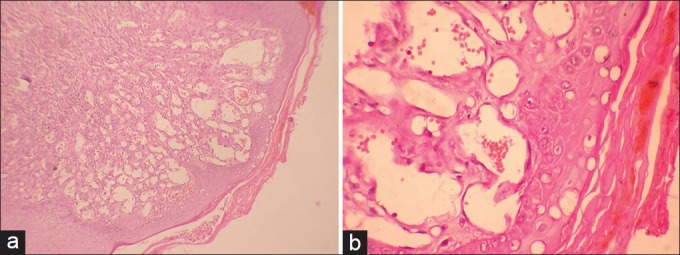
(a) Photomicrograph (H and E stain, ×10) of skin biopsy from the right leg demonstrating hyperkeratosis, acanthosis and congestion in the papillary dermis. (b) Photomicrograph (H and E stain, ×40) of skin biopsy from the right leg demonstrating plump endothelial cells in papillary dermis
Figure 2.

Linear, multiple, dark brown, hyperkeratotic plaques with irregular borders on the right shin which bleed on trivial trauma
Figure 3.

Lesions after excision and skin grafting
Discussion
Angiokeratomas (derived from three Greek words meaning vessels, horn, and tumor, respectively) are vascular lesions that are defined as one or more dilated vessel (s) lying in the papillary dermis accompanied by an epidermal reaction such as acanthosis and/or hyperkeratosis.[5] They are associated with a worldwide prevalence of 0.16% and a slight male preponderance. The precise mechanism for their development is unknown.[4,5] Angiokeratomas can be classified into five types: (1) Angiokeratoma of Mibelli in which acral lesions are associated with cold injury; (2) Angiokeratoma of Fordyce, which are generally genital; (3) Angiokeratoma circumscriptum (AKC), which is nevoid with an onset in early life; and (4) Solitary or multiple angiokeratoma with an onset in adult life;[7,8] (5) Anderson–Fabry disease (angiokeratoma corporis diffusum), a systemic glycolipidosis associated with cutaneous lesions in a diffuse pattern as a result of deficiency of the enzyme ceramide trihexosidase leading to accumulation of glycosphingolipids in vascular endothelium and smooth muscle cells.[6,9]
AKC is the rarest type of angiokeratoma and since its original description by Fabry in 1915, only 100 cases have been reported demonstrating a female preponderance in a ratio of 3:1.[3,10] It most commonly involves the legs in a unilateral or otherwise asymmetrical distribution. In one unique case, only the neck was involved.[11,12] However, truncal as well as several very extensive lesions covering as much as one-quarter of the body have also been reported.[13] It is commonly characterized by reddish papules and nodules, which over time coalesce to form hyperkeratotic verrucous plaques in a zosteriform distribution.[4,5,10] The development of hyperkeratosis may be associated with an expression of matrix metalloproteinase-9 in the lesion.[14] The coexistence of AKC with Klippel–Trenaunay syndrome has been evident in several cases.[13,15] Other associations of AKC include Cobb syndrome, nevus flammeus, cavernous hemagioma, and traumatic AV fistula.[16]
Diagnosis can usually be suspected clinically and confirmed histopathologically by the characteristic features of hyperkeratosis, papillomatosis, and acanthosis with vascular proliferation limited to papillary dermis.[4] Verrucous hemangioma, a congenital, localized, vascular malformation involving the dermis and subcutaneous fat that may clinically mimic AKC is histologically characterized by hyperkeratosis, dilated capillaries, large cavernous, endothelial-lined, and blood-filled spaces extending well into the reticular dermis and subcutaneous fat, unlike AKC in which vascular dilatation is restricted to papillary dermis.[4,17] Hypertrophic angioproducing tumors (telangiectasias) in AKC characteristically evolve from single vascular dilatation without cellular proliferation, while verrucous hemangioma is considered among the angioproducing hyperplastic tumors, characterized by proliferation of mesenchymal cells tending to the formation of capillaries.[4]
As spontaneous regression is not a facet of this disease, definitive treatment is fundamental for its cure. Smaller lesions may be treated by diathermy, curettage, electrocautery, and cryosurgery. Large lesions, as in our case, necessitate deep excision followed by grafting and still larger ones may require laser ablation (carbon dioxide, argon laser, KTP).[10,18]
What is new?
A typical case of AKC is presented to stress on the inevitable requirement of an appropriate method of destruction/removal as this nevoid condition is persistent and liable to the episodes of bleeding and pain on trivial trauma.
Video available on www.e-ijd.org
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Enjolras O. Vascular malformations. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2nd ed. Vol. 2. Spain: Elsevier limited; 2008. pp. 1581–96. [Google Scholar]
- 2.Jansen T, Bechara FG, Altmeyer P. Angiokeratomas: Symptoms, diagnostics and therapy. TKT Europe-5S AB: Danderyd. 2004 [Google Scholar]
- 3.Fabry J. Úber einen Fall von Angiokeratoma circumscriptum am linken Oberschenkel [A case of angiokeratoma circumscriptum] Dermatol Z. 1915;22:1–4. [Google Scholar]
- 4.Mittal R, Aggarwal A, Srivastava G. Angiokeratoma circumscriptum: A case report and review of the literature. Int J Dermatol. 2005;44:1031–4. doi: 10.1111/j.1365-4632.2005.02252.x. [DOI] [PubMed] [Google Scholar]
- 5.Schiller PI, Itin PH. Angiokeratomas: An update. Dermatology. 1996;193:275–82. doi: 10.1159/000246270. [DOI] [PubMed] [Google Scholar]
- 6.Sodaifi M, Aghaei S, Monabati A. Cutaneous variant of angiokeratoma corporis diffusum associated with angiokeratoma circumscriptum. Dermatol Online J. 2004;10:20. [PubMed] [Google Scholar]
- 7.Newton JA, McGibbon DH. The treatment of multiple angiokeratoma with the argon laser. Clin Exp Dermatol. 1987;12:23–5. doi: 10.1111/j.1365-2230.1987.tb01848.x. [DOI] [PubMed] [Google Scholar]
- 8.Imperial R, Helwig EB. Angiokeratoma: A clinicopathological study. Arch Dermatol. 1967;95:166–75. doi: 10.1001/archderm.95.2.166. [DOI] [PubMed] [Google Scholar]
- 9.Desnick RJ, Brady R, Barranger J, Collins AJ, Germain DP, Goldman M, et al. Fabry disease, an under-recognized multisystemic disorder: Expert recommendations for diagnosis, management, and enzyme replacement therapy. Ann Intern Med. 2003;138:338–46. doi: 10.7326/0003-4819-138-4-200302180-00014. [DOI] [PubMed] [Google Scholar]
- 10.Pasyk KA, Argenta LC, Schelbert EB. Angiokeratoma circumscriptum: Successful treatment with argon laser. Ann Plast Surg. 1988;20:183–90. doi: 10.1097/00000637-198802000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Sardana K, Koranne RV, Sharma RC, Mahajan S. Angiokeratoma circumscriptum naeviforme: Rare presentation on the neck. Australas J Dermatol. 2001;42:294–5. doi: 10.1046/j.1440-0960.2001.00540.x. [DOI] [PubMed] [Google Scholar]
- 12.Gupta S, Aggarwal K, Goel S. Angiokeratoma circumscriptum. Ind J Dermatol. 1998;43:16. [Google Scholar]
- 13.Dammert K. Angiokeratosis naeviformis: A form of naevus telangiectaticus lateralis (Naevus flammeus) Dermatologica. 1965;130:17–39. doi: 10.1159/000254513. [DOI] [PubMed] [Google Scholar]
- 14.Kobayashi T, Sakuroka K. A case of angiokeratoma circumscriptum: Immunolocalization of matrix metalloproteinase (MMP)-9. J Dermatol. 1998;25:391–4. doi: 10.1111/j.1346-8138.1998.tb02420.x. [DOI] [PubMed] [Google Scholar]
- 15.Odeh F. Angiokeratoma corporis circumscriptum naeviforme mit angiodysplasie (Klippel-Trenaunay-Weber-syndrome. Z Hautkr. 1979;54:701–6. [PubMed] [Google Scholar]
- 16.del Pozo J, Fonseca E. Angiokeratoma circumscriptum naeviforme: Successful treatment with carbon-dioxide laser vaporization. Dermatol Surg. 2005;31:232–6. doi: 10.1111/j.1524-4725.2005.31048. [DOI] [PubMed] [Google Scholar]
- 17.Pavithra S, Mallya H, Kini H, Pai G. Verrucous hemangioma or angiokeratoma? A missed diagnosis. Ind J Dermatol. 2011;56:599–600. doi: 10.4103/0019-5154.87171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Occella C, Bleidl D, Rampini P, Schiazza L, Rampini E. Argon laser treatment of cutaneous multiple angiokeratomas. Dermatol Surg. 1995;21:170–2. doi: 10.1111/j.1524-4725.1995.tb00135.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


