Sir,
Neurothekeomas were described in 1980 as benign cutaneous tumors of nerve sheath differentiation. Subsequent authors suggested neurothekeomas represented variants of dermal nerve sheath myxomas.[1] However, subtle morphologic differences, divergent immunohistochemical staining in human tissue, and ultrastructural studies led many authors to question the relationship between neurothekeomas and nerve sheath myxomas.
A 25-year-old female had 0.7 cm sized single subcutaneous nodule with tenderness on her left thumb [Figure 1]. After excision, specimen showed sharply marginated nodule in the dermis with the multi-lobular structures and amorphous myxoid matrix [Figure 2a]. Within the myxoid matrix, there were scattered collections of epithelioid Schwann cells in corded, nested, ring-like morphology and syncytial-like aggregation [Figure 2b–d]. These cells were immunoreactive for S-100 protein, neuron specific enolase (NSE), vimentin, NKI/C3, and non-reactive for glial fibrillary acidic protein (GFAP), smooth muscle actin (SMA), CD10, CD68 [Figure 3].
Figure 1.
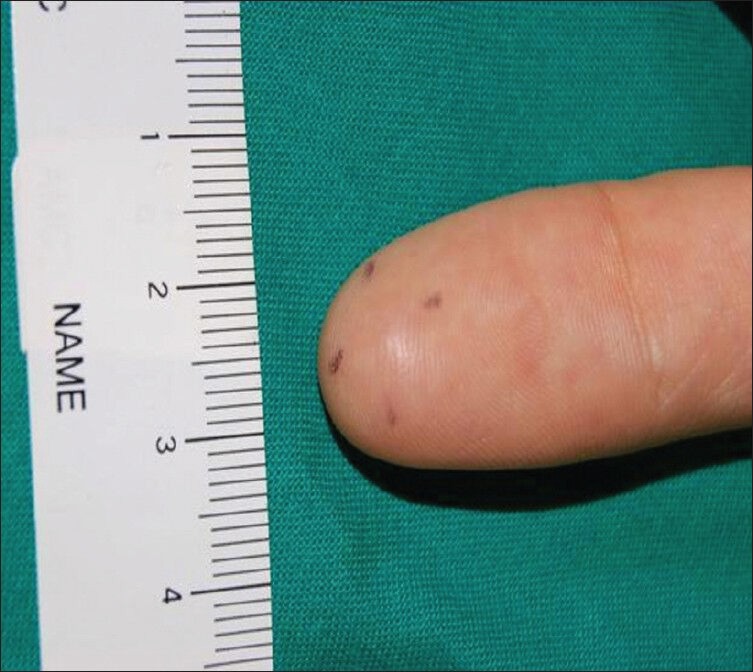
A solitary 7 mm sized, subcutaneous mass on left thumb
Figure 2.
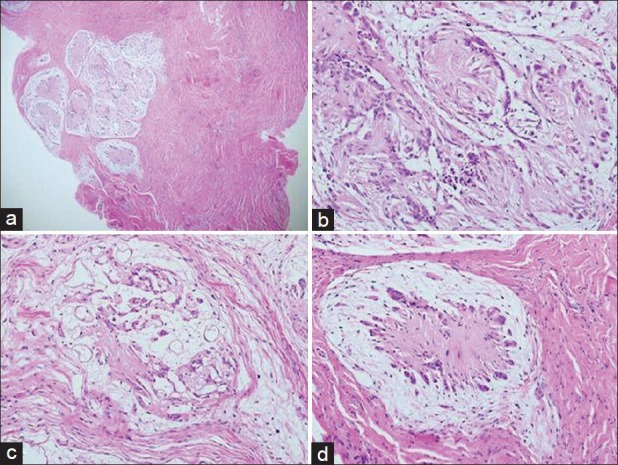
(a) Sharply marginated multiple lobules with abundunt mxyoid matrix in dermis (H and E, ×40). (b) Corded aggregation of epihelioid Schwann cells in tumor (H and E, ×200). (c) A variable number of Schwann cells with a ring-like appearance, (H and E, ×200). (d) Syncytial-like aggregation of Schwann cells (H and E, ×200)
Figure 3.
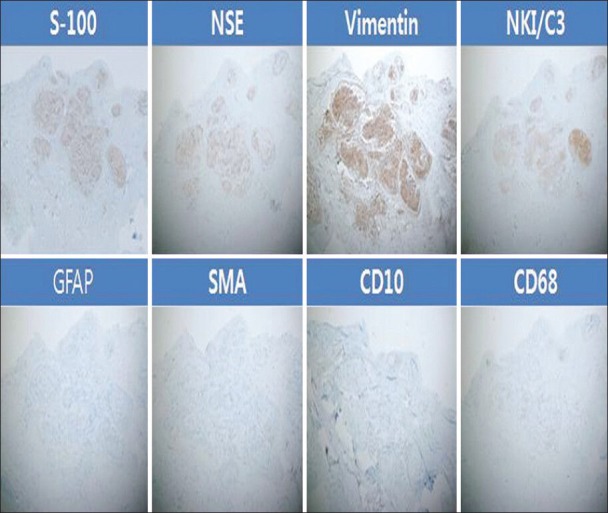
Immunohistochemical staining results
In previous studies, they reported that nerve sheath myxomas involved finger, knee or pretibial region commonly in 3rd and 4th decades of patients. The male-to-female ratio was almost 1:1. On the other hand, neurothekeomas arose most often on the upper limb or head and neck in 2nd and 3rd decades of patents. There was a 1.8:1 female predominance. Tumors of both diseases were similarly described as painless subepidermal nodule.[2,3]
To date, there is ambiguous disease definition between nerve sheath myxomas and neurothekeomas. Recent studies argued that these two diseases are distinct and suggested S-100 protein staining as the crucial reason, not histological findings.[2,4] This was also consistent with our case results. Other immunoreactive staining for nerve sheath myxomas are GFAP, CD57, NSE. Neurothekeomas showed positive staining results for NKI/C3, NSE, and SMA. However, all other staining couldn’t show 100% result consistency, except S-100 protein. Recently, study using the microarray-based gene expression profile showed that S-100B gene was the most significantly differentially expressed gene between the nerve sheath myxomas and the neurothekeomas.[4] This molecular finding correlates with recent immunohistochemical observations and provides the molecular support for recent work reporting negative S100 protein staining by immunohistochemistry in neurothekeomas of all subtypes.[4]
There was one report about soft-tissue tumor of hand in a 5 month old infant.[5] Spindle cells in specimen showed positive staining for S-100, and alcian blue for mucoid stroma. And they diagnosed this as myxoid neurothekeoma. However, according to recent reported studies above mentioned, we suppose attentively that it is better to be diagnosed as nerve sheath myxoma than the neurothekeoma.
Hence, we support that nerve sheath myxoma is a distinct disease of nerve sheath derivation distinguished with the neurothekeoma and S-100 protein staining would be the most powerful criteria to discriminate these diseases.
References
- 1.Pulitzer DR, Reed RJ. Nerve-sheath myxoma (perineurial myxoma) Am J Dermatopathol. 1985;7:409–21. doi: 10.1097/00000372-198510000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Fetsch JF, Laskin WB, Miettinen M. Nerve sheath myxoma: A clinicopathologic and immunohistochemical analysis of 57 morphologically distinctive, S-100 protein- and GFAP-positive, myxoid peripheral nerve sheath tumors with a predilection for the extremities and a high local recurrence rate. Am J Surg Pathol. 2005;29:1615–24. doi: 10.1097/01.pas.0000173025.87476.a4. [DOI] [PubMed] [Google Scholar]
- 3.Fetsch JF, Laskin WB, Hallman JR, Lupton GP, Miettinen M. Neurothekeoma: An analysis of 178 tumors with detailed immunohistochemical data and long-term patient follow-up information. Am J Surg Pathol. 2007;31:1103–14. doi: 10.1097/PAS.0b013e31802d96af. [DOI] [PubMed] [Google Scholar]
- 4.Sheth S, Li X, Binder S, Dry SM. Differential gene expression profiles of neurothekeomas and nerve sheath myxomas by microarray analysis. Mod Pathol. 2011;24:343–54. doi: 10.1038/modpathol.2010.203. [DOI] [PubMed] [Google Scholar]
- 5.Al-Buainain H, Pal K, El Shafie H, Mitra DK, Shawarby MA. Myxoid neurothekeoma: A rare soft tissue tumor of hand in a 5 month old infant. Indian J Dermatol. 2009;54:59–61. doi: 10.4103/0019-5154.48990. [DOI] [PMC free article] [PubMed] [Google Scholar]


