Abstract
BACKGROUND:
It is recommended that household contacts of children with cystic fibrosis and household contacts of children <2 years of age receive annual influenza vaccinations. There is little information documenting whether this recommendation is being followed.
METHODS:
A 20-question survey was distributed to caregivers of children with cystic fibrosis and to caregivers of healthy children <17 years of age seen in a Saskatoon (Saskatchewan) tertiary care centre. Survey questions addressed the influenza vaccination status of the child and household contacts. Respondents were also asked to rate the influence of various factors on the decision to vaccinate, using a 5-point Likert scale.
RESULTS:
Reported vaccination rates were 21%, 25% and 7% among household contacts of children with cystic fibrosis, children <2 years of age and children ≥2 years of age, respectively. Advice from their physician, belief that they were too healthy, and inconvenient times and locations of vaccination centres were significant influences when compared among the three groups. Other main deterrents to vaccination were belief that the vaccine does not prevent influenza and belief that its side effects are greater than its benefits.
CONCLUSION:
By understanding motivators and barriers to vaccination among household contacts of children with cystic fibrosis, effective strategies may be implemented to improve vaccination coverage against influenza. Strong recommendations by clinicians and improved access to vaccination centres are essential components in improving influenza vaccination coverage.
Keywords: Attitudes, Children, Cystic fibrosis, Household contacts, Influenza, Vaccination
Abstract
HISTORIQUE :
Il est recommandé d’administrer annuellement le vaccin contre l’influenza aux contacts familiaux d’enfants ayant la fibrose kystique et d’enfants de moins de deux ans. Peu d’information étaye le respect de cette recommandation.
MÉTHODOLOGIE :
Un sondage de 20 questions a été distribué aux personnes qui s’occupent d’enfants ayant la fibrose kystique et d’enfants en santé de moins de 17 ans vus dans un centre de soins tertiaires de Saskatoon, en Saskatchewan. Les questions du sondage portaient sur le statut de vaccination contre l’influenza de l’enfant et des contacts familiaux. Les répondants ont également été invités à classer l’influence de divers facteurs sur la décision de vacciner, selon l’échelle de cinq points de Likert.
RÉSULTATS :
Les taux de vaccination déclarés s’élevaient à 21 %, 25 % et 7 % chez les contacts familiaux d’enfants atteints de la fibrose kystique, les enfants de moins de deux ans et les enfants de deux ans et plus, respectivement. Les conseils du médecin, la conviction qu’ils étaient en trop bonne santé, de même que les heures d’ouverture et le lieu peu pratiques des centres de vaccination étaient des influences importantes au sein des trois groupes. Les autres principaux freins à la vaccination étaient la conviction que le vaccin ne prévient pas l’influenza et la conviction que ses effets secondaires sont plus importants que ses avantages.
CONCLUSION :
Si on comprend les sources de motivation et les obstacles à la vaccination des contacts familiaux d’enfants atteints de la fibrose kystique, on pourra peut-être adopter des stratégies efficaces pour améliorer la couverture vaccinale contre l’influenza. Des recom-mandations convaincues de la part des cliniciens et un meilleur accès aux centres de vaccination sont des éléments essentiels à une amélioration de la couverture vaccinale.
Influenza is an acute viral infection that primarily attacks the respiratory tract. It may lead to serious consequences in individuals with underlying chronic disease (eg, respiratory, cardiac or renal disease, diabetes mellitus, cancer) (1,2). Individuals at the extremes of the age range are also more likely to experience increased morbidity and mortality secondary to influenza infection (3,4).
In patients with cystic fibrosis (CF), respiratory viral infections lead to increased bacterial trapping and thickened secretions. This becomes apparent as progressive lung obstruction and worsening pulmonary function (5–8). A CF Foundation patient registry study estimated that a 2.1% increase in pulmonary exacerbations occurs during the influenza season (9). Respiratory viruses have also been suggested to be one of the mediators of the onset of chronic Pseudomonas aeruginosa infection in CF patients (10), perhaps via facilitation of colonization of the lung epithelia (11,12).
Influenza vaccines are safe, elicit adequate antibody responses and have been shown to be an effective means to prevent or attenuate infection in many patient groups (13,14). Several organizations, including the Canadian National Advisory Committee on Immunization, the Canadian Paediatric Society and the American Academy of Pediatrics, recommend annual vaccination for individuals at high risk for influenza-related complications, including patients with CF, as well as those capable of transmitting influenza to high-risk patients such as household contacts (1,15,16).
There is limited evidence demonstrating that the influenza vaccination guidelines, specifically for household contacts, are followed in Canada. We conducted a survey to determine influenza vaccination rates among the household contacts of three separate groups: children with CF, healthy children <2 years of age and healthy children two to 16 years of age. We also sought to better understand perceptions of the influenza vaccine and the barriers to being immunized against influenza.
METHODS
Study setting and population
The present study was conducted between August 1, 2009 and October 31, 2009, at the Royal University Hospital (Saskatoon, Saskatchewan), a tertiary care centre servicing Saskatoon and northern Saskatchewan. The study population included: household contacts of children zero to 16 years of age with CF; household contacts of healthy children >2 years of age; and household contacts of healthy children two to 16 years of age.
The National Advisory Committee on Immunization recommendation for the 2012/2013 influenza season recently expanded the high-risk category to healthy children <5 years of age (1); however, when the present study was conducted, vaccination was recommended for children six to 23 months of age and household contacts of children zero to 23 months of age (17).
Permission for the present study was obtained from the Biomedical Research Ethics Board at the University of Saskatchewan (Saskatoon, Saskatchewan). Participation was voluntary and written informed consent was obtained from all participants.
Data collection
A survey was administered to household contacts of children with CF attending regularly scheduled CF clinics at the Royal University Hospital. The survey was also administered to a convenience sample of household contacts of previously healthy children (<2 years of age and two to 16 years of age) admitted for an acute illness to the inpatient wards at the Royal University Hospital. These children had to have no underlying history of a chronic medical condition or immunodeficiency. All respondents had to be ≥18 years of age. The survey consisted of 20 questions regarding demographic characteristics of the individual completing the survey (age, sex, relationship to the child) and the influenza vaccination status of the child with CF/hospitalized child and of all household contacts for the previous (2008/2009) influenza season. Survey participants were given 14 statements regarding influences for/against influenza vaccination affecting household contacts and were asked to indicate their agreement with the statements using a 5-point Likert scale (0 = not a factor, 1 = strongly negatively influenced, 2 = negatively influenced, 3 = neutral, 4 = influenced, 5 = strongly influenced). Statements for and against vaccination were based on previous studies of barriers to immunization and attitudes toward immunization. All three study groups received the same survey.
Statistical analysis
Descriptive statistics (frequencies, means and SDs) were calculated to characterize the respondents and their survey responses. χ2 tests were used to compare the differences in responses among household contacts of children with CF, healthy children <2 years of age and healthy children two to 16 years of age. Differences among groups were analyzed and the level of statistical significance was set at α=0.05. All statistical analyses were performed using SPSS software (IBM Corporation, USA).
RESULTS
From August 1, 2009 to October 31, 2009, 85 household contacts were approached to complete the survey. Eighty-two surveys were completed and analyzed. Twenty-eight were completed by household contacts of children with CF, 24 by household contacts of healthy children <2 years of age and 30 by household contacts of healthy children two to 16 years of age (Table 1).
TABLE 1.
Demographic characteristics of participants in the influenza vaccination survey
| Characteristic | Household contacts of children with CF (n=28) |
Household contacts of healthy children
|
|
|---|---|---|---|
| <2 years of age (n=24) | Two to 16 years of age (n=30) | ||
| Female sex | 25 (89.3) | 17 (70.8) | 23 (76.7) |
| Relationship | |||
| Mother | 23 (82.1) | 17 (70.8) | 19 (63.3) |
| Father | 3 (10.7) | 7 (29.2) | 7 (23.3) |
| Other | 2 (7.1) | 4 (13.3) | |
| Age, years | |||
| 18–24 | 4 (14.3) | 6 (25.0) | 2 (6.7) |
| 25–34 | 9 (32.1) | 14 (58.3) | 9 (30.0) |
| 35–44 | 11 (39.3) | 4 (16.7) | 11 (36.7) |
| ≥45 | 4 (14.3) | 8 (26.7) | |
Data presented as n (%). CF Cystic fibrosis
Participant demographic data
Demographic data of the participants, including sex, age and relationship to the child, are presented in Table 1.
Influenza vaccination
Influenza vaccination rate of children:
The reported vaccination rate for children with CF was 64%, compared with 46% of healthy children <2 years of age and 17% of healthy children two to 16 years of age.
Influenza vaccination rate of household contacts:
Among survey participants, 60% indicated that none of the household contacts of the child were immunized for influenza for that influenza season, with household contacts of healthy children <2 years of age being more likely to report that at least one additional household member had been immunized. Families of healthy children two to 16 years of age were least likely to have had all household contacts immunized (Figure 1).
Figure 1).
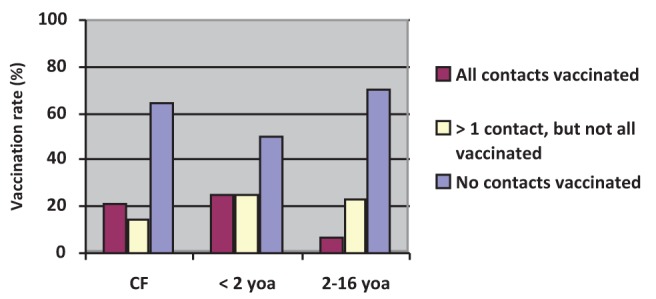
Influenza vaccination rates of household contacts. CF Cystic fibrosis, yoa Years of age
Influences for vaccination or nonvaccination
When all three study groups were combined, the most influential factor for vaccination was advice from a physician. The most influential barrier to vaccination was belief that the “influenza vaccine does not prevent the flu”, followed by “too healthy to receive the flu vaccine” and “side effects are greater than its benefits” (Figure 2).
Figure 2).
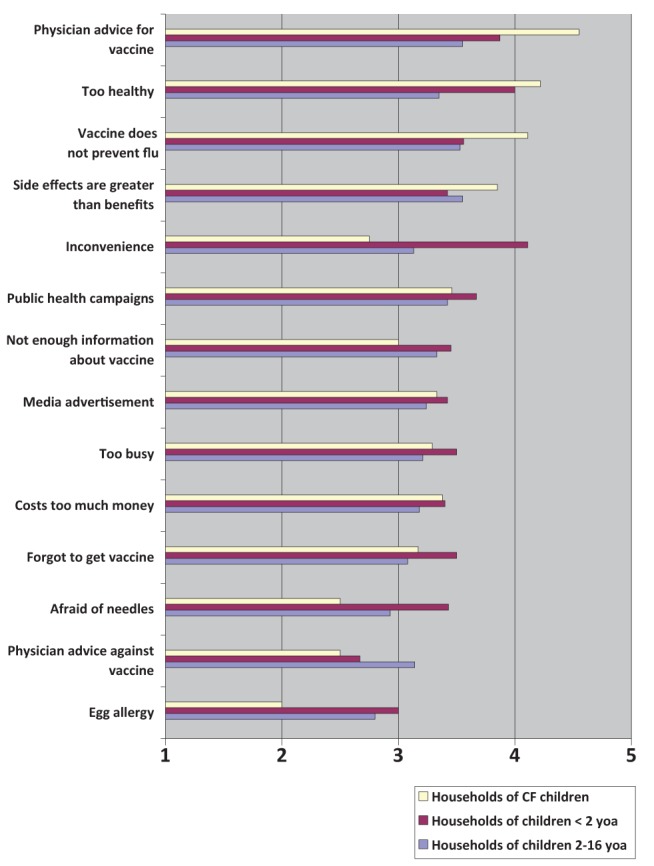
Factors influencing decisions to immunize household contacts against influenza, measured on a Likert scale (1 = strongly negatively influenced; 2 = negatively influenced; 3 = neutral; 4 = influenced; 5 = strongly influenced). CF Cystic fibrosis; yoa Years of age
Comparisons among the three groups revealed that advice from a physician was a significant influence for household contacts of CF children to receive the influenza vaccine compared with household contacts of healthy children <2 years of age and household contacts of healthy children two to 16 years of age (P=0.001). “Inconvenient times and locations of vaccination centers” was not a deterrent for household contacts of CF children compared with household contacts of healthy children of all ages (P=0.001). Household contacts of CF children and household contacts of healthy children <2 years of age were more likely to believe that they were “too healthy to receive the flu vaccine” compared with household contacts of healthy children two to 16 years of age (P=0.01).
DISCUSSION
Previous studies have revealed that certain groups, including those with chronic pulmonary conditions and young children, are at high risk for influenza-related morbidity and mortality (2–4). Influenza vaccination is, therefore, recommended to prevent and attenuate the effects of infection (1,13,14). The present study was the first in Canada to examine influenza vaccination rates and perceptions of the influenza vaccine among household contacts of CF children, and of healthy children zero to 16 years of age.
In our study, less than two-thirds of CF children had been immunized against influenza during the preceding influenza season. This rate is lower than that reported in a study performed in France, in which Murris-Espin et al (18) showed that 86% of CF patients <18 years of age were vaccinated during the 2005/2006 influenza season. The importance of protection against influenza may be underscored in the youngest of this vulnerable population. Emerging evidence shows that asymptomatic infants with CF may already have underlying airway inflammation mediated by neutrophils, with early decline in lung function observed on pulmonary function testing (19). Avoidance of any viral insult is important to prevent further decline in lung function. Data from randomized controlled studies investigating the effectiveness of influenza vaccination in the CF population have not reported clinically relevant outcomes such as lung function, hospitalization rates or mortality (20). Despite this, there remains sufficient evidence in the literature that influenza leads to excess morbidity in this population (eg, an excess of 2.1% of pulmonary exacerbations occuring during the influenza season [9]). Immunization should, therefore, be encouraged.
Only 46% of healthy children <2 years of age were reportedly immunized against influenza in 2008–2009 in our study. Although low, this contrasts sharply with data from Ontario. A telephone survey of Ontario households revealed that only 10.2% of six- to 23-month-olds had been fully immunized against influenza, and 13.8% were partially immunized during the 2006/2007 influenza season (21). Data from other provinces reveal immunization rates of 24.1% to 52.2% (22). A second Ontario study identified all infants born between April 2002 and March 2008 and, using physician fee-for-service claims, determined that 1.1% to 9.7% of children six to 23 months of age had received the influenza vaccine during the 2002–2009 influenza seasons (22). Although receipt of the influenza vaccine could only be determined for invidivuals immunized by their family physician, a previous study revealed that only 23% of Ontario households were immunized by someone other than their family doctor (22). Our data and those reported by other Canadian provinces remain below the target for influenza coverage of 70% (23).
Influenza immunization of at least one household contact was reported by 38% of study participants who had children with CF, compared with 50% of participants who had healthy children <2 years of age. Because the influenza virus is spread via respiratory droplets, and possibly by aerosolization, household contacts can transmit the virus to individuals at high risk for complications from influenza infection. Thus, immunization against influenza is warranted among household contacts of high-risk groups. This is especially true for household contacts of infants <6 months of age, who cannot be immunized themselves because the influenza vaccine has limited immunogenicity at this age (24,25).
Advice from a physician was the most important positive influence for household contacts of CF children, and confirms the important role that physicians play in advocating for immunization (26–29). Interestingly, neither health campaigns or media advertisements appeared to influence any study participant’s decision to immunize their children or household contacts.
Inconvenience was a reported barrier for immunization of household contacts of children <2 years of age, as shown in previous studies investigating barriers to immunization (28,30,31). Although this was reportedly less of a barrier for household contacts of CF patients, our data also shows that, while CF patients were more likely to be immunized, their household contacts were less likely to be immunized compared with household contacts of children <2 years of age. This contradictory response may reflect the fact that influenza vaccination was offered to CF patients attending regularly scheduled CF clinics at the Royal University Hospital, but not to their household contacts.
Household contacts of children with CF and of children <2 years of age both expressed the belief that they were too healthy to require the vaccine, while household contacts of children with CF were more likely than those in the other two groups to perceive that immunization does not prevent influenza infection. Some respondents from all three groups believed that the side effects of being immunized were greater than the benefits. These misperceptions and knowledge gaps have been highlighted in other studies (27,32), and should be addressed if immunization targets for influenza and other vaccine-preventable diseases are to be met.
The challenge is translating this information into effective interventions that increase influenza vaccination uptake. Physicians caring for children at high risk for influenza-related complications need to be cognisant of the guidelines for influenza vaccination, including immunizing household contacts of high-risk patients, and relay this information in an effective manner. Education of families about the risks and benefits of immunization should help to reduce the fear related to obtaining vaccinations. Other helpful strategies include weekend/evening ‘flu shot only’ sessions, open access to flu shots, and reminder telephone calls and postcards to patients (33). These should be tailored not only to the patients themselves, but toward household contacts as well.
Limitations to the present study include potential bias resulting from self-reporting vaccine uptake for both the children and the household contacts one year before. Nevertheless, parent-reported vaccination has been shown to have a sensitivity of 84.9% and a specificity of 68.7% (27). In addition, the small number of participants limits the generalizability of these findings because the study was conducted in one tertiary care centre.
SUMMARY
Influenza vaccination of two high-risk groups of children at our institution (children with CF and healthy children <2 years of age) is low. A more significant concern is the lower rate of influenza vaccination of their household contacts; these are at odds with the guidelines regarding annual influenza vaccination promulgated by national health bodies. The present study reinforces the fact that physicians play an important role in promoting influenza vaccination of groups at risk and their household contacts. Clinicians caring for children need to be cognisant of the guidelines for influenza vaccination in high-risk groups and their household contacts, and relay the cost/benefit information of immunization in an effective manner. Strong messaging needs to come across at every patient encounter, especially as the influenza season approaches.
REFERENCES
- 1.National Advisory Committee on Immunization Statement on seasonal influenza vaccine for 2012–2013. Can Commun Dis Rep. 2012;38:1–36. doi: 10.14745/ccdr.v38i00a02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glezen WP, Decker M, Perrotta DM. Survey of underlying conditions of persons hospitalized with acute respiratory diseases during influenza epidemics in Houston, 1978–1981. Am Rev Respir Dis. 1987;136:550–8. doi: 10.1164/ajrccm/136.3.550. [DOI] [PubMed] [Google Scholar]
- 3.Nair H, Brooks WA, Katz M, et al. Global burden of respiratory infections due to seasonal influenza in young children: A systematic review and meta-analysis. Lancet. 2011;378:1917–30. doi: 10.1016/S0140-6736(11)61051-9. [DOI] [PubMed] [Google Scholar]
- 4.Menec VH, Black C, MacWilliam L, Aoki FY. The impact of influenza-associated respiratory illnesses on hospitalizations, physician visits, emergency room visits and mortality. Can J Public Health. 2003;94:59–63. doi: 10.1007/BF03405054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rowe SM, Miller S, Sorscher EJ. Cystic fibrosis. N Engl J Med. 2005;352:1992–2001. doi: 10.1056/NEJMra043184. [DOI] [PubMed] [Google Scholar]
- 6.Wat D, Gelder C, Hibbits S, Bosler I, Pierrepoint M, Evans R. Is there a role for influenza vaccination in cystic fibrosis? J Cyst Fibros. 2008;7:85–8. doi: 10.1016/j.jcf.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 7.Ong EL, Bilton D, Abbott J, Webb AK, McCartney RA, Caul EO. Influenza vaccination in adults with cystic fibrosis. BMJ. 1991;303:557. doi: 10.1136/bmj.303.6802.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang EEL, Prober CG, Manson B, Corey M, Levison H. Association of respiratory viral infections with pulmonary deterioration in patients with cystic fibrosis. Thorax. 1984;311:1653–8. doi: 10.1056/NEJM198412273112602. [DOI] [PubMed] [Google Scholar]
- 9.Ortiz JR, Neuzil KM, Victor JC, Wald A, Aitken ML, Goss CH. Influenza-associated cystic fibrosis pulmonary exacerbations. Chest. 2010;137:852–860. doi: 10.1378/chest.09-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johansen HK, Høiby N. Seasonal onset of initial colonisation and chronic infection with Pseudomonas aeruginosa in patients with cystic fibrosis in Denmark. Thorax. 1992;47:109–11. doi: 10.1136/thx.47.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Vrankrijker AM, Woljs TF, Clofu O, et al. Respiratory syncytial virus infection facilitates acute colonization of Pseudomonas aeruginosa in mice. J Med Virol. 2009;81:2096–103. doi: 10.1002/jmv.21623. [DOI] [PubMed] [Google Scholar]
- 12.van Ewijk BE, Wolfs TF, Aerts PC, et al. RSV mediates Pseudomonas aeruginosa binding to cystic fibrosis and normal epithelial cells. Pediatr Res. 2007;61:398–403. doi: 10.1203/pdr.0b013e3180332d1c. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP) – United States, 2012–13 influenza season. MMWR Recomm Rep. 2012;61:613–8. [PubMed] [Google Scholar]
- 14.Gross PA, Hermogenes AW, Sacks HS, Lau J, Levandowski RA. The efficacy of influenza vaccine in elderly persons. A meta-analysis and review of the literature. Ann Intern Med. 1995;123:518–27. doi: 10.7326/0003-4819-123-7-199510010-00008. [DOI] [PubMed] [Google Scholar]
- 15.Moore DL, Canadian Paediatric Society, Infectious Diseases and Immunization Committee Statement on seasonal influenza vaccine for 2012–2013. Paediatr Child Health. 2012;17:e90–e93. [Google Scholar]
- 16.American Academy of Paediatrics, Committee on Infectious Diseases Recommendations for prevention and control of influenza in children, 2012–2013. Pediatrics. 2012;130:780. doi: 10.1542/peds.2012-2308. [DOI] [PubMed] [Google Scholar]
- 17.National Advisory Committee on Immunization Statement on influenza vaccination for the 2008–2009 season. Can Commun Dis Rep. 2009;34:1–46. [PubMed] [Google Scholar]
- 18.Murris-Espin M, Aubert M, Bosdure E, Dubus JC. Influenza vaccination coverage in patients with cystic fibrosis followed at 12 care centers in the Greater South Region of France for the season 2005/2006. Vaccine. 2008;26:2615–18. doi: 10.1016/j.vaccine.2008.07.095. [DOI] [PubMed] [Google Scholar]
- 19.Pillarisetti N, Williamson E, Linnane B, et al. Australian Respiratory Early Surveillance Team for Cystic Fibrosis (ARESTCF) Infection, inflammation, and lung function decline in infants with cystic fibrosis. Am J Respir Crit Care Med. 2011;184:75–81. doi: 10.1164/rccm.201011-1892OC. [DOI] [PubMed] [Google Scholar]
- 20.Dharmaraj P, Smyth RL. Vaccines for preventing influenza in people with cystic fibrosis. Cochrane Database Syst Rev. 2009;(4):CD001753. doi: 10.1002/14651858.CD001753.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Moran K, Maaten S, Guttmann A, Northrup D, Kwong JC. Influenza vaccination rates in Ontario children: Implications for universal childhood vaccination policy. Vaccine. 2009;27:2350–5. doi: 10.1016/j.vaccine.2009.02.017. [DOI] [PubMed] [Google Scholar]
- 22.Campitelli MA, Inoue M, Calzavara AJ, Kwong JC, Guttman A. Low rates of influenza immunization in young children under Ontario’s universal influenza immunization program. Pediatrics. 2012;129:e1241–30. doi: 10.1542/peds.2011-2441. [DOI] [PubMed] [Google Scholar]
- 23.Laboratory Centre for Disease Control Canadian Consensus Conference on Influenza. Can Commun Dis Rep. 1993;19:136–42. 145–7. [PubMed] [Google Scholar]
- 24.Groothuis JR, Levin MJ, Rabalais GP, Meiklejohn G, Lauer BA. Immunization of high-risk infants younger than 18 months of age with split-product influenza vaccine. Pediatrics. 1991;87:823–8. [PubMed] [Google Scholar]
- 25.Halasa NB, Gerber MA, Chen Q, Wright PE, Edwards KM. Safety and immunogenicity of trivalent inactivated influenza vaccine in infants. J Infect Dis. 2008;197:1448–54. doi: 10.1086/587643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin CJ, Zimmerman RK, Nowalk MP. Parental perspectives on influenza vaccination of children with chronic medical conditions. J Natl Med Assoc. 2006;98:148–53. [PMC free article] [PubMed] [Google Scholar]
- 27.Bonnani P, Bergamini M. Factors influencing vaccine uptake in Italy. Vaccine. 2001;(20 Suppl 1):S8–12. doi: 10.1016/s0264-410x(01)00284-5. [DOI] [PubMed] [Google Scholar]
- 28.Fredrickson DD, Davis TC, Arnold CL, et al. Childhood immunization refusal: Provider and parent perceptions. Fam Med. 2004;36:431–9. [PubMed] [Google Scholar]
- 29.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Barriers to influenza immunization in a low-income urban population. Am J Prev Med. 2001;20:21–5. doi: 10.1016/s0749-3797(00)00263-4. [DOI] [PubMed] [Google Scholar]
- 30.Deutchman M, Brayden R, Siegel CD, Beaty B, Crane L. Childhood immunization in rural family and general practices: Current practices, perceived barriers and strategies for improvement. Amb Child Health. 2000;6:181–9. [Google Scholar]
- 31.Mack RW, Darden PM. Children’s immunizations: The gap between parents and providers. Health Market Quarterly. 1999;16:7–14. doi: 10.1300/J026v16n04_02. [DOI] [PubMed] [Google Scholar]
- 32.Schmitt H-J. Factors influencing vaccine uptake in Germany. Vaccine. 2001;20(Suppl 1):S2–4. doi: 10.1016/s0264-410x(01)00304-8. [DOI] [PubMed] [Google Scholar]
- 33.Britto MT, Schoettker PJ, Pandzik GM, Weiland J, Mandel KE. Improving influenza immunisation for high-risk children and adolescents. Qual Saf Health Care. 2007;16:363–8. doi: 10.1136/qshc.2006.019380. [DOI] [PMC free article] [PubMed] [Google Scholar]


