Abstract
OBJECTIVES
We used validated sensitive and specific questions associated with clinically-confirmed diagnoses of unexplained vulvar pain (Vulvodynia) to compare the cumulative incidence of vulvar pain and prevalence of care seeking behavior in Boston, Massachusetts metropolitan area (BMA) and in Minneapolis/St. Paul (MSP), Minnesota, between 2001–2005 using census-based data, and 2010–2012, using outpatient community-clinic data, respectively.
STUDY DESIGN
We received self-administered questionnaires from 5,440 women in BMA and 13,681 in MSP, 18–40 years of age, describing their history of vulvar burning or pain on contact that persisted >3 months that limited/prevented intercourse.
RESULTS
By age 40, 7–8% in BMA and MSP reported vulvar pain consistent with Vulvodynia. Women of Hispanic/Latina origin compared to Caucasians were 1.4 times more likely to develop vulvar pain symptoms (95%CI: 1.1–1.8). Many women in MSP (48%) and BMA (30%) never sought treatment, and >50% who sought care with known health care access received no diagnosis.
CONCLUSIONS
Using identical screening methods, we report high prevalence of vulvar pain in two geographical regions, and that access to health care does not increase the likelihood of seeking care for chronic vulvar pain.
Keywords: Ethnic groups, Health services accessibility, Prevalence, Vulvodynia
INTRODUCTION
We1 and others2–4 have shown that vulvodynia (chronic vulvar pain in the absence of objective abnormalities such as infection or dermatoses), is highly prevalent with lifetime estimates ranging from 10–28% among reproductive-aged women in the general population. Our previous assessment of vulvodynia cumulative incidence in the Boston metropolitan area (BMA) was conducted in women systematically sampled from census-based directories. All ethnicities we sampled were affected, with a somewhat greater occurrence among Hispanic/Latina women. Furthermore, the cumulative incidence decreased with increasing age, with nearly half of all women affected choosing not to seek treatment.1
We have also recently shown that questions asked of women in the general population pertaining to undiagnosed pain on contact that limited or prevented intercourse, have good sensitivity and specificity compared to a clinically confirmed diagnosis of vulvodynia.5 Thus, in the absence of a clinical examination, investigators now have the capability to use a few questions to reasonably screen for the proportion of women in the general population who may possibly be suffering from vulvodynia. This is particularly important given that so many women choose not to seek treatment1,6 and therefore can only be identified through population screening methods.
Using data from a new sample of women in the Minneapolis/Saint Paul metropolitan area (MSP), in conjunction with our previously reported sample from the Boston Metropolitan Area (BMA), we have the opportunity to extend our previous estimates of vulvodynia occurrence. Our data allows for a comparison of vulvodynia cumulative incidence from a census-based population sample (BMA), and a sample derived from the administrative database of women who were seen for any reason at one of several outpatient community clinics within a defined geographic region (MSP). In addition to cumulative incidence comparisons, we also assess care-seeking behavior between those with and without known access to health care resources. We believe these findings provide the best estimates of the magnitude of this debilitating condition in the general population given that similar diagnostic screening occurred across two geographical regions. Our findings also shed light on the associated stigma that prevents women from seeking care even when access to health care resources is available.
MATERIALS AND METHODS
This study has been approved by the Human Subjects Research Committees at the Brigham and Women’s Hospital, the University of Minnesota and Fairview Health Services.
Population-sampling frame, Boston Metropolitan Area (BMA)
Details pertaining to the source of subjects within this sampling frame have previously been described.1 At the time of this earlier publication, we were still screening and recruiting women through this sampling frame. We now have completed this screening study and present a larger sample than previously reported. Although the BMA sample included women 18–64 years of age, we restricted the sample in this analysis to women 18–40 years of age for comparability between BMA and MSP. Thus, the BMA sample included 9,878 women between 18 and 40 years of age from three ethnically diverse Boston-area neighborhoods and two west-suburban communities surveyed between January, 2001 and September, 2005. Massachusetts Town Books (annual publications that list residents by name, age and address according to voter precincts) served as the source population for our sample which was restricted to households in which we could confirm an address and telephone number. The sample was weighted according to the 2000 Census age distribution within each of the five geographical areas.
A self-administered questionnaire to assess a history of vulvar pain (see vulvar pain classification below) was mailed to each woman, and after two mailings and one telephone follow-up assessment, 67.2% completed the questionnaire. Response varied by less than 10% across communities and age categories. After further restricting the respondents to those with complete screening data, 5,440 (55.1% of the target sampled population) were included in these analyses.
Population-sampling frame, Minneapolis/St, Paul Metropolitan Area (MSP)
Our sampling frame in MSP included women between 18–40 years of age who were seen for any reason in any outpatient clinic that was part of a large health care network that caters to approximately 27% of the MSP population. We randomly sampled 25,754 women seen in any of these clinics within the past two years that were within a 70-mile radius of the University of Minnesota between March, 2010 and December, 2011.
Women sampled were mailed a letter describing the study and a self-administered questionnaire to assess the same history of vulvar pain as that queried among women in the BMA. After three mailings, 13,681 women (53.1%) returned a completed questionnaire that included all key questions needed for this analysis. Participants represented all geographical areas of the MSP region.
Classifying vulvar pain and assessing care-seeking behavior
The initial development of the self-administered screening questionnaire, which was given to both samples of women, has been previously described.1 In brief, we assessed a vulvar pain history for each woman on criterion used to classify a history consistent with vulvodynia. These criterion are consistent with the International Society for the Study of Vulvovaginal Disorders (ISSVD) initiative to develop consistent diagnostic criteria for vulvodynia.7 Women surveyed in both BMA and MSP were asked about their history of vulvar burning or pain on contact that persisted for a period of three months or longer. Self-reported age at first onset of vulvar pain was obtained and used to estimate age-specific cumulative incidence (see Statistical approach below). We further queried whether the discomfort was continuous, intermittent, provoked or spontaneous. In addition, we determined whether the pain and discomfort occurred only during intercourse or at other times as well, and whether it limited or prevented women from having intercourse. Although all of these questions were asked of women sampled from both BMA and MSP, we previously reported that women reporting pain on contact for a period of three months or longer that limited or prevented intercourse was associated with an 83% sensitivity and 94% specificity for meeting a true diagnosis of vulvodynia based on the gold standard of a clinical examination to rule out other known causes of vulvar pain.5
Statistical methods
We created a retrospective cohort of all women sampled who completed the self-administered screening questionnaire and then assessed the age at first onset of vulvar pain categorized as younger than 20, 20–24, 25–29, 30–34, and 35–40. We also stratified the cumulative incidence by the following self-reported race/ethnicity categories: Caucasian or White, Black or African-American, Hispanic or Latina, or of other racial backgrounds. Calculating age specific cumulative incidence of vulvar pain required us to account for censoring since a woman’s history stopped at the time they completed the survey. Cumulative incidence was estimated using life table methods8 and confidence intervals (CIs) were obtained by bootstrapping. Kaplan-Meier product-limit survival analyses were used to illustrate differences in cumulative incidence by age across ethnic groups and the two geographic regions.
We then restricted the analyses to women who met our classification for symptoms consistent with vulvodynia to assess geographical differences in care seeking behavior and by primary (always having had pain on contact) versus secondary (having had a pain-free period of intercourse prior to the onset of vulvar pain symptoms) onset of vulvodynia. We estimated what proportion of women sought treatment, how many different clinicians were seen to address their vulvar pain, and whether they were able to receive a diagnosis (either correct or incorrect based on the respondent’s self-report). Separate logistic models were used to determine the adjusted proportion of women who sought treatment, and whether or not a diagnosis was obtained, adjusted for the women’s age at the time of the survey, race, and the length of time they had suffered from vulvodynia-like symptoms. Multinomial models were used to estimate the proportion of women with Vulvodynia who saw 1–2, 2–3, or 4 or more clinicians to address their vulvar pain. We examined differences in these proportions between women from BMA and MSP, and between women with primary versus secondary vulvar pain onset. All analyses were performed using STATA v12 (College Station, TX).
RESULTS
In both the BMA and the MSP sample, respondents and non-respondents were comparable by age (BMA: 41% of respondents and 41% of non-respondents were <30 years; MSP: 49% of respondents and 55% of non-respondents were <30 years).
Table 1 shows the demographic characteristics of the BMA census-based and MSP community-clinic-based samples. Women in the BMA sample were somewhat older, more highly educated, less likely to be married and have a body mass index (BMI) greater than 25. A higher proportion of the MSP sample self-reported being white of non-Hispanic origin compared to the BMA sample. However, in the MSP sample, 15% of the participants were non-White allowing for reasonable analytical comparisons to the BMA sample. There were no clinically meaningful differences in the proportion of women reporting difficulty and/or pain with first tampon use between the two samples suggesting comparability in early life exposures that may contribute to vulvar pain onset later in life.1
Table 1.
Characteristics of women screened for vulvar pain in Boston, MA, 2001–2005 and the Twin Cities metropolitan are in MN, 2010–2011*
| Twin Cities, 2010 – 2011 (N=13,681) n (%) |
Boston, 2001 – 2005 (N=5,440) n (%) |
|
|---|---|---|
| Age at Survey, y | ||
|
| ||
| <20 | 409 (3.0) | 63 (1.2) |
| 20–24 | 1,896(13.9) | 798 (14.7) |
| 25–29 | 3,588 (26.2) | 1,052 (19.3) |
| 30–34 | 3,983 (29.1) | 1,453 (26.7) |
| 35–40 | 3,805 (27.8) | 2,074 (38.1) |
|
| ||
| Education | ||
|
| ||
| < High school | 1,376 (10.1) | 632 (11.6) |
| High school grad | 4,315 (31.5) | 1,181 (21.7) |
| Some college | 5,327 (38.9) | 2,304 (42.4) |
| College degree | 2,643 (19.3) | 1,236 (22.7) |
| Missing | 20 (0.2) | 87 (1.6) |
|
| ||
| Race | ||
|
| ||
| White | 11,589 (84.8) | 3,678 (67.7) |
| African American | 508 (3.7) | 490 (9.0) |
| Hispanic/Latina | 441 (3.2) | 360 (6.6) |
| Asian | 722 (5.3) | 160 (2.9) |
| Other | 402 (2.9) | 246 (4.5) |
| Missing | 19 (0.1) | 506 (9.3) |
|
| ||
| Marital Status | ||
|
| ||
| Single | 5,158 (37.7) | 2,370 (43.6) |
| Married/partnered | 7,729 (56.5) | 2,741 (50.3) |
| Separated/divorced | 738 (5.4) | 299 (5.5) |
| Widowed | 17 (0.1) | 10 (0.2) |
| Missing | 39 (0.3) | 20 (0.4) |
|
| ||
| BMI | ||
|
| ||
| <20 | 1,436 (10.5) | 685 (12.6) |
| 21–24.9 | 4,906 (35.9) | 2,021 (37.1) |
| 25–29.9 | 3,123 (22.8) | 1,149 (21.1) |
| 30+ | 2,559 (18.7) | 852 (15.7) |
| Missing | 1,657 (12.1) | 733 (13.5) |
|
| ||
| Pain with first tampon use | ||
|
| ||
| No difficulty | 3,885 (28.5) | 1,529 (28.1) |
| Difficulty/no pain | 3,727 (27.2) | 1,599 (29.4) |
| Difficulty/some pain | 4,504 (32.9) | 1,541 (28.3) |
| Difficulty/great pain | 893 (6.5) | 249 (4.6) |
| Never used tampon | 617 (4.5) | 489 (9.0) |
| Missing | 55 (0.4) | 33 (0.6) |
Due to such large sample sizes, all characteristics differed by geographical region at p< 0.0
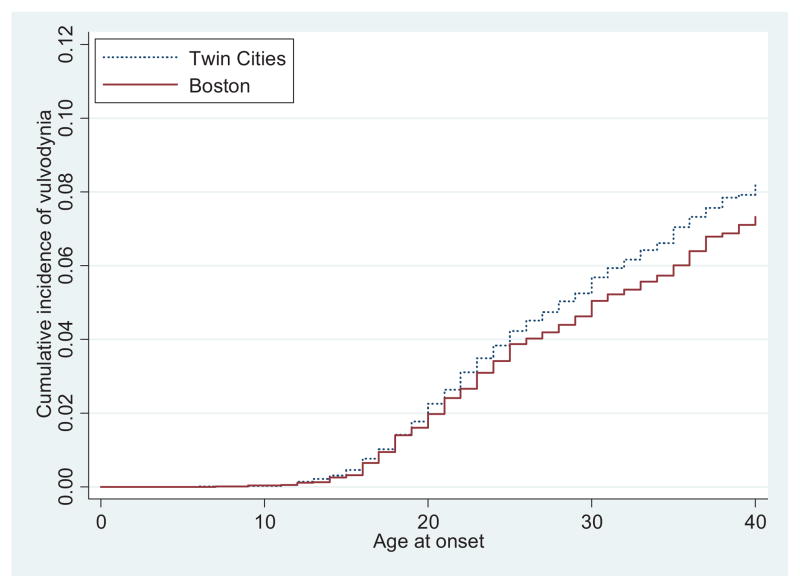
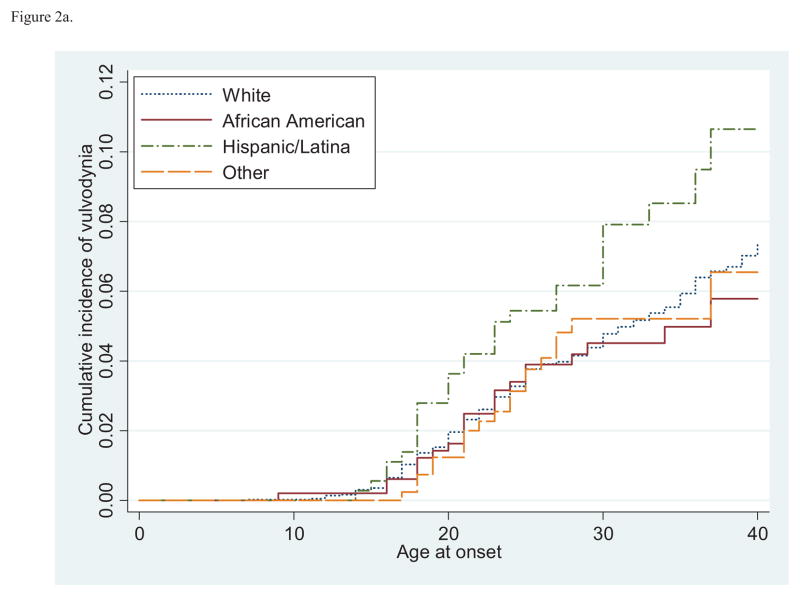
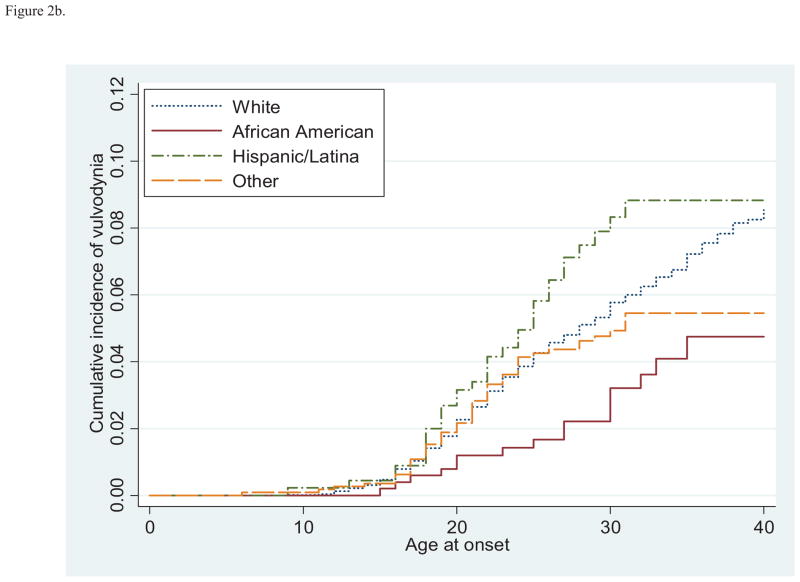
As shown in Table 2, the age-specific risk of vulvodynia in the BMA sample was similar to that in the MSP sample across each of the age categories. Also, within both samples, the rate of first onset of vulvar pain was greatest before the age of 25, decreased during the late 20s and early 30s, and then rose again as women approached their later reproductive years. We further estimated the cumulative incidence of vulvodynia among women in both samples (Figure 1) and observed that women in the MSP and BMA samples were within approximately one percentage point of each other, suggesting no appreciable difference in vulvodynia incidence between the two populations. These results suggest that by age 40, 7–8% of women will have experienced symptoms consistent with vulvodynia. We further stratified this figure by race (Figures 2a and 2b). In both samples, women of Hispanic/Latina origin were at a greater risk of developing vulvar pain symptoms. We used a Cox Proportional Hazards model to test this difference and found that, combined across both geographic regions, by age 40 Hispanic/Latina women were 1.4 times more likely to develop vulvar pain compared to Caucasian women (95% CI 1.1–1.8).
Table 2.
Age-specific cumulative incidence of vulvodynia* in women age 18 to 40 years from two geographical locations
| Total | Twin Cities | Boston | ||||
|---|---|---|---|---|---|---|
| Population at risk, n | % (95% CI) | Population at risk, n | % (95% CI) | Population at risk, n | % (95% CI) | |
| Age at onset, y | ||||||
| <20 | 19,100 | 1.8 (1.6, 2.0) | 13,662 | 1.8 (1.6, 2.0) | 5,438 | 1.7 (1.3, 2.0) |
| 20–24 | 18,325 | 2.0 (1.9, 2.2) | 13,035 | 2.1 (1.9, 2.4) | 5,290 | 1.9 (1.5, 2.2) |
| 25–29 | 15,478 | 1.4 (1.2, 1.6) | 1,023 | 1.5 (1.3, 1.7) | 4,455 | 1.3 (0.9, 1.6) |
| 30–34 | 10,982 | 1.4 (1.2, 1.7) | 7,549 | 1.5 (1.2, 1.8) | 3,433 | 1.2 (0.8, 1.6) |
| 35–40 | 5,694 | 2.0 (1.5, 2.6) | 3,684 | 1.9 (1.3, 2.6) | 2,010 | 2.1 (1.4, 2.9) |
Defined as pain on contact in the last 6 months that limited or prevented intercourse
Figure 1.
Age-specific cumulative incidence of vulvodynia among women age 18 to 40 from two geographical locations.
Figure 2.
Figure 2a. Age-specific cumulative incidence of vulvodynia by self- reported race/ethnicity among women age 18 to 40 in the Boston metropolitan area, Massachusetts, 2001 – 2005.
Figure 2b. Age-specific cumulative incidence of vulvodynia by self-reported race/ethnicity among women age 18 to 40 in the Twin Cities metropolitan area, Minnesota, 2010 –2011.
Table 3 restricts the samples to those reporting symptoms consistent with vulvodynia to assess healthcare seeking behavior after adjustment for age, race, and length of time suffering from vulvar pain. A higher proportion of women suffering from vulvodynia in the BMA sample sought treatment compared to women suffering from vulvodynia in the MSP sample. This can be empirically quantified as a Risk Difference of 18% (95% CI= 11.3–24.6). Yet, there were still a substantial proportion of both samples of women who never sought treatment (48% in MSP, 30% in BMA). Of those who sought treatment, those in the BMA sample were more likely to seek care from more than two clinicians compared to women in the MSP sample, and thus were more often able to receive a diagnosis. However, even within the BMA sample, more than 30% were unable to receive a diagnosis, and within the MSP sample, more than 50% received no diagnosis for their condition.
Table 3.
Healthcare seeking among women with vulvodynia* age 18 to 40 years from two geographical locations: Number and adjusted† proportions
| All Cases n (%) [95%CI] |
Twin Cities (MSP) n (%) [95% CI] |
Boston (BMA) n (%) [95%CI] |
|
|---|---|---|---|
| Sought treatment⋄ | 586 (56.5) [53.5, 59.4] | 405 (52.0) [48.5, 55.5] | 181 (70.0) [64.3, 75.6] |
|
| |||
| Clinicians seen**‡ | |||
| 1 or 2 | 329 (59.0) [55.0, 63.0] | 241 (62.7) [58.0, 67.50] | 88 (50.8) [43.5, 58.1] |
| 3 or 4 | 129 (23.1) [19.7, 26.6] | 70 (18.6) [14.6, 22.5] | 59 (32.8) [25.8, 39.8] |
| 5 or more | 101 (17.9) [14.8, 21.0] | 70 (18.7) [14.8. 22.6] | 31 (16.4) [11.0, 21.8] |
| Diagnosis** | 264 (48.0) [44.0, 52.0] | 148 (39.0) [34.1, 43.9] | 116 (67.4) [60.5, 74.4] |
Defined as pain on contact in the last 6 months that limited or prevented intercourse
Adjusted for age at time of survey, race, and length of time suffering from vulvodynia
Risk Difference for sought treatment (Boston versus Twin Cities) was 18 (95%CI=11.3, 24.6)
Only among women who sought treatment
24 women from the Twin Cities and 3 women from Boston who failed to provide number of clinicians seen or were missing key covariate information are not included in the analysis
Within the MSP sample only, we had the opportunity to distinguish women reporting vulvodynia symptoms by those reporting primary (always had pain on contact) versus secondary (initiation of pain after a period of pain-free intercourse) onset of pain (Table 4). After adjustment for age, race, and length of time suffering with vulvar pain, women who always had pain on contact (primary Vulvodynia) were somewhat more likely to have sought treatment compared to women whose pain began after a period of pain-free intercourse (Risk Difference = 8.1%, 95%CI −0.6–16.8). However, of those who sought treatment, there was little difference in the number of clinicians seen by primary versus secondary onset of pain, and more than 50% reported being unable to receive a diagnosis, irrespective of timing of pain onset.
Table 4.
Healthcare seeking among women with vulvodynia*, age 18 to 40 years, from the Twin Cities metro area by primary case status (who always had pain on contact) or secondary case status (had pain on contact that started later): Number and adjusted† proportions
| Always had pain on contact n (%) [95% CI] |
Pain on contact started later n (%) [95% CI] |
|
|---|---|---|
| Sought treatment⋄ | 105 (57.6) [50.1, 65.0] | 262 (49.5) [45.3, 53.7] |
|
| ||
| Clinicians seen**‡ | ||
| 1 or 2 | 59 (63.7) [54.4, 73.0] | 157 (62.2) [56.3, 68.2] |
| 3 or 4 | 15 (14.5) [7.5, 21.5] | 48 (19.9) [14.8, 24.9] |
| 5 or more | 24 (21.8) [13.9, 29.7] | 42 (17.9) [13.1, 22.7] |
| Diagnosis** | 31 (35.0) [25.2, 44.8] | 103 (40.8) [34.7, 46.9] |
Defined as pain on contact in the last 6 months that limited or prevented intercourse
Adjusted for age at time of survey, race, and length of time suffering from vulvodynia
38 women missing who sought treatment but in whom we could not classify their onset of pain as primary versus secondary; Risk Difference (Always versus Started later) was 8.1 (−0.6–16.8)
Only among women who sought treatment
An additional 22 women missing who failed to provide number of clinicians seen or were missing key covariate information
COMMENT
These findings add to our previous publication that brought to the attention of the scientific community the much greater prevalence of this condition in the general population than had previously been reported.1 However, we now have shown in two distinct geographical regions, with the use of a much better indicator of symptoms that are strongly associated with the likelihood of a diagnosis of vulvodynia,5 that approximately 8% of women may experience these symptoms by the age of 40.
There have been two reports of Latina women being at increased risk of vulvodynia.1,6 We were the first to show this association1 and have now replicated this previous finding in a second geographical location. A subsequent report by Reed et al6 found that Latina women in Michigan were at a higher risk of developing vulvodynia as well, compared to White women. It is interesting to note that the Hispanic women in the BMA are more likely to be of Caribbean descent while those in the MSP are more likely to have Central and South American origins. In addition, we can also not rule out selection bias as a potential explanation for these differences (consistent in both geographical regions) if, in truth, there are differences by race among those with vulvar pain who do and do not agree to participate in the survey.
Of great importance is the fact that we observed a similar cumulative incidence for symptoms consistent with vulvodynia across two geographical regions in which the source population differed. In BMA, women were sampled from community census directories while those in the MSP region were identified from the administrative records of women seen for any medical reason over the past two years at selected community healthcare clinics that cater to both insured and uninsured populations. Given that the MSP women currently have access to healthcare resources, it was surprising to find that despite accounting for the length of time with vulvar pain, MSP women were even less likely to seek treatment for their vulvar pain symptoms compared to their BMA counterparts. This may emphasize the substantial stigma associated with vulvar pain given that these women choose to seek care for other medical problems,9 but apparently do not convey to their healthcare providers the presence of vulvar pain. However, reasons not to seek care may be multifactorial and further research should delineate these factors.
In comparing our findings to that of other studies, we run into complications due to differences in study populations, sampling methods, and diagnostic criteria. Populations are either clinic-based or population-based, and sampling methods are either random or convenience samples. A primary difference in diagnostic criteria used is whether self-reported vulvar pain was present for a minimum of three or a minimum of six months to qualify as vulvodynia. One of the first clinic-based studies to examine the prevalence of vulvodynia reported that 15% of women met clinical criteria consistent with a vulvodynia diagnosis.10 Two subsequent clinic-based studies reported lifetime prevalence estimates of vulvar pain as 13.3%11 and 11%.12 In Denbow’s study,11 the authors clinically confirmed a subset of women with vulvar vestibulitis (now classified as localized provoked vulvodynia) and estimated its prevalence as approximately 3%. However, we now know that clinic-based assessments do not accurately estimate prevalence because it includes only those women who choose to seek treatment and ultimately receive a diagnosis, which represents approximately half of those who truly have this condition in the general population as shown in these and our earlier findings.1
We previously contributed one of the first community-based studies,13 and sought to determine the prevalence of lower genital tract discomfort in women from the general population, finding that 12% were experiencing “knife-like” pain, or pain on contact, suggestive of vulvodynia.13 However, we recognized the need to be much more specific in our screening assessment which led to our publication suggesting a 16% lifetime prevalence of vulvar pain in women 18–64 years of age with a point prevalence of 7% at the time of the survey.1 More recently, other community-based studies have replicated our findings. A study conducted by Arnold et al.4 used a telephone survey and reported a 9.9% prevalence of vulvodynia using the ISSVD’s description of vulvodynia with symptoms lasting at least six months. This estimate is quite similar to another telephone survey6 that used a random digit dialing sample frame and found that 8.3% of women reported “having pain at the vulva or opening to the vagina” that was present for a minimum of three months. Both Reed and Arnold’s estimates are similar to our current estimate suggesting that differences in time to define chronicity in diagnostic criteria may not have a large impact on prevalence estimates.4,6 Finally, two other studies conducted by Reed found prevalence estimates of 7.6%14 and 9.4%2 among women in a health registry. An internet-based survey conducted by the same research group in 2004 reported that 27.9% of women had a history of vulvar pain and that 7.8% of women had experienced this pain in the past six months.3
There are certain limitations that may impact the validity of our findings and those of others. Without an actual clinical examination, we cannot be sure that those classified as having symptoms consistent with vulvodynia would in fact meet the existing or future clinically-confirmed diagnostic criteria for this condition. Thus, our estimates of age-specific risk and cumulative incidence across two geographical regions will likely include some degree of misclassification. However, we used a set of questions that were validated against the gold standard of a clinical examination consistent with an 83% sensitivity and 95% specificity.5 We suspect any misclassification would be non-differential across region, biasing our estimates of the difference between region toward the null, on average.
We can also not rule out that our prevalence estimates could be influenced by selective recall of vulvar pain symptoms and care seeking behavior. For example, younger women affected with this condition may have been more willing to report its presence, while older women may be less inclined to be forthcoming due to a secular trend of greater perceived stigma with increasing age. In a large study of women from the National Vulvodynia Association, we found that the longer a woman had vulvodynia, the less likely she is to feel comfortable discussing it in social relationships.15 However, it is unclear what factors may contribute to this discomfort in discussing vulvar pain, or how length of pain may be associated with discussing pain with a healthcare provider. Further, we can also not rule out that our prevalence estimates may be potentially over-inflated, since women with a history of vulvar pain may have been more likely to agree to complete our screener interview. Although we recognize these weaknesses, they are offset by the fact that we were able to assess the magnitude of this problem in women from community-based samples rather than clinical specialty practices.15
In summary, we have shown that approximately 8% of women may develop vulvar pain symptoms by the age of 40, and that the risk of developing this condition by the age of 40 is higher among Hispanic/Latina women than White women. We have used similar screening methods to estimate the cumulative incidence of this condition in two distinct geographical locations. We have also shown that a large proportion of women sampled from the administrative records of outpatient community health care clinics suffer from vulvar pain and choose not to seek care, just as that observed in those sampled from census-based data. Vulvar pain is a prevalent and debilitating disorder that women need to recognize as a condition that can be diagnosed and managed with appropriate care and guidance. More importantly, we hope these findings lead to a greater awareness on the part of clinicians caring for reproductive-aged women so that they may initiate discussion around this problem that may lead to disclosure, and ultimately effective ways to manage this condition.
Approximately 8% of women may experience symptoms consistent with a diagnosis of vulvodnia by the age of 40.
These estimates are remarkably similar across two distinct geographical regions.
Women of Hispanic/Latina origin are more likely to report a history of these symptoms and again this observation was present in both geographical regions.
A large proportion of women choose not to seek care for these symptoms despite having access to health care services.
Acknowledgments
This study was supported by NIH grants R01-HD384285 and R01-HD058608
Footnotes
The authors report no conflict of interest.
Reprints will not be available.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Bernard L. HARLOW, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
Ms. Christine G. KUNITZ, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
Ruby H.N. NGUYEN, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
Ms. Sarah A. RYDELL, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
Ms. Rachel M. TURNER, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
Richard F. MACLEHOSE, Division of Epidemiology & Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota.
References
- 1.Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc. 2003;58(2):82–8. [PubMed] [Google Scholar]
- 2.Reed BD, Haefner HK, Sen A, Gorenflo DW. Vulvodynia incidence and remission rates among adult women: A 2-year follow-up study. Obstet Gynecol. 2008;112:231–7. doi: 10.1097/AOG.0b013e318180965b. [DOI] [PubMed] [Google Scholar]
- 3.Reed BD, Crawford S, Couper M, Cave C, Haefner HK. Pain at the vulvar vestibule: A web-based survey. J Low Genit Tract Dis. 2004;8:48–57. doi: 10.1097/00128360-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Arnold LD, Bachmann GA, Rosen R, Rhoads GG. Assessment of vulvodynia symptoms in a sample of US women: A prevalence survey with a nested case control study. Am J Obstet Gynecol. 2007;196(2):128.e1–128.e6. doi: 10.1016/j.ajog.2006.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harlow BL, Vazquez G, MacLehose RF, Erickson DJ, Oakes JM, Duval SJ. Self-reported vulvar pain characteristics and their association with clinically confirmed vestibulodynia. J Womens Health. 2009;18(9):1333–9. doi: 10.1089/jwh.2008.1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed BD, Harlow SD, Sen A, et al. Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am J Obstet Gynecol. 2012;206:170–9. doi: 10.1016/j.ajog.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bachmann GA, Rosen R, Pinn VW, et al. Vulvodynia: a state-of-the-art consensus on definitions, diagnosis and management. Consensus Development Conference. J Reprod Med. 2006;51(6):447–56. [PubMed] [Google Scholar]
- 8.Hosmer DW, Lemeshow S. Wiley Series in Probability and Statistics. New York, NY: 1999. Applied Survival Analysis; p. 79.p. 79. [Google Scholar]
- 9.Nguyen R, Turner R, Rydell S, MacLehose R, Harlow BL. Perceived stereotyping and seeking care for chronic vulvar pain. Pain Med. 2013 Jun 6; doi: 10.1111/pme.12151. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goetsch MF. Vulvar vestibulitis: Prevalence and historic features in a general gynecologic practice population. Am J Obstet Gynecol. 1991;164:1609–14. doi: 10.1016/0002-9378(91)91444-2. [DOI] [PubMed] [Google Scholar]
- 11.Denbow ML, Byrne MA. Prevalence, causes and outcome of vulval pain in a genitourinary medicine clinic population. Int J STD AIDS. 1998;9:88–91. doi: 10.1258/0956462981921738. [DOI] [PubMed] [Google Scholar]
- 12.Lavy RJ, Hynan LS, Haley RW. Prevalence of vulvar pain in an urban, minority population. J Reprod Med. 2007;52:59–62. [PubMed] [Google Scholar]
- 13.Harlow BL, Wise LA, Stewart EG. Prevalence and predictors of chronic lower genital tract discomfort. Am J Obstet Gynecol. 2001;185:545–50. doi: 10.1067/mob.2001.116748. [DOI] [PubMed] [Google Scholar]
- 14.Reed BD, Haefner HK, Harlow SD, Gorenflo DW, Sen A. Reliability and validity of self-reported symptoms for predicting vulvodynia. Obstet Gynecol. 2006;108:906–13. doi: 10.1097/01.AOG.0000237102.70485.5d. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen RHN, MacLehose RF, Veasley C, Turner RM, Harlow BL, Horvath KJ. Comfort in discussing vulvar pain in social relationships among women with vulvodynia. J Reprod Med. 2012;57(3–4):109–14. [PubMed] [Google Scholar]