Abstract
Background: The current diagnostic system for subjects at enhanced clinical risk of psychosis allows concurrent comorbid diagnoses of anxiety and depressive disorders. Their impact on the presenting high-risk psychopathology, functioning, and transition outcomes has not been widely researched. Methods: In a large sample of subjects with an At-Risk Mental State (ARMS, n = 509), we estimated the prevalence of DSM/SCID anxiety or depressive disorders and their impact on psychopathology, functioning, and psychosis transition. A meta-analytical review of the literature complemented the analysis. Results: About 73% of ARMS subjects had a comorbid axis I diagnosis in addition to the “at-risk” signs and symptoms. About 40% of ARMS subjects had a comorbid diagnosis of depressive disorder while anxiety disorders were less frequent (8%). The meta-analysis conducted in 1683 high-risk subjects confirmed that baseline prevalence of comorbid depressive and anxiety disorders is respectively 41% and 15%. At a psychopathological level, comorbid diagnoses of anxiety or depression were associated with higher suicidality or self-harm behaviors, disorganized/odd/stigmatizing behavior, and avolition/apathy. Comorbid anxiety and depressive diagnoses were also associated with impaired global functioning but had no effect on risk of transition to frank psychosis. Meta-regression analyses confirmed no effect of baseline anxiety and/or depressive comorbid diagnoses on transition to psychosis. Conclusions: The ARMS patients are characterized by high prevalence of anxiety and depressive disorders in addition to their attenuated psychotic symptoms. These symptoms may reflect core emotional dysregulation processes and delusional mood in prodromal psychosis. Anxiety and depressive symptoms are likely to impact the ongoing psychopathology, the global functioning, and the overall longitudinal outcome of these patients.
Key words: psychosis, schizophrenia, ultra high risk, ARMS, prodromal, attenuated psychosis, psychosis risk, depression, anxiety
Introduction
Over the past few years, there has been substantial growth in prodromal psychosis articles published across the electronic databases. This interest indicates that identification of individuals at high clinical risk of first-episode psychosis has become a major goal of psychiatric services worldwide.1 The exponential interest is such that a new diagnostic category was considered for inclusion in the forthcoming DSM-5.2 The recommendation from the Psychosis Disorders Working party is for it to be included in Section III, which is the section of the DSM-5 text in which conditions that require further research will be included (www.dsm5.org). This recommendation has support from researchers in the field. The detection of subjects at enhanced clinical risk for psychosis has become possible due to validated operationalized criteria and psychometric instruments used across different centers. Accumulating research evidence has shed light on the risk of transition to psychosis in high-risk subjects, which ranges from 18% at 6 months to up to 32% by 3 years.3 There is additional evidence that the majority of high-risk subjects who later develop a psychotic episode will develop a schizophrenia spectrum disorder.4 These results, in conjunction with neurocognitive5 and neurobiological6 findings, are exciting as they raise the possibility of preventative interventions for the most severe and debilitating psychiatric disorder.1
Unfortunately, specific interventions for reducing transition rates in high-risk subjects are not yet available. One of the problems limiting further advancement in this field is the high psychopathological heterogeneity of the high-risk groups. In addition to attenuated psychotic symptoms, subjects at high risk for psychosis usually present with other clinical concerns. High levels of negative symptoms, significant impairments in academic performance and occupational functioning, and difficulties with interpersonal relationships as well as substantially compromised subjective quality of life are often observed.7 Notably, many have comorbid nonpsychotic diagnoses, in particular anxiety disorders and depression.1 Anxiety and depressive symptoms have been historically suggested to frequently mark the onset of the initial prodrome of psychosis.8 The largest high-risk study (n = 377) published to date showed about 69% of participants had one or more mood/anxiety diagnoses at entry to the service.9 The second largest high-risk study (n = 245) indicated even higher comorbid rates with up to 78% of the sample presenting with nonpsychotic diagnoses at baseline.10 Although the current high-risk criteria allow concurrent comorbid diagnoses of anxiety and depressive disorders, their association with prodromal signs and symptoms is not well established. Anxiety and depressive symptoms are more often of concern to the high-risk patients than their attenuated psychotic symptoms.1 Audits on the clinical cases of our prodromal services indicate that anxiety and depressive symptoms together with impaired functioning are the core presenting complaints reported by high-risk subjects. This is mirrored by the observation that psychological interventions usually offered to these subjects are often tailored to improve anxiety and depressive symptoms rather than reducing primarily the attenuated psychotic symptoms. Despite the crucial role of these comorbidities, there is no research addressing the impact of anxiety and depressive symptoms on the psychopathology of high-risk patients. Furthermore, the high prevalence of anxiety and depressive comorbid diagnoses in high-risk subjects may be relevant to their prognosis. Copresence of psychotic symptomatology in disorders of anxiety and depression is common and associated with poorer illness course compared to anxiety and depression without these symptoms.11 A recent study has found depressive disorders, but not anxiety disorders, can predict later transition to psychosis in high-risk patients.10 However, these results conflict with the other available study indicating anxiety or depressive diagnostic comorbidity was not associated with transition to psychosis.12
To elucidate these issues, we analyzed a large database of high-risk subjects. We first measured the prevalence of anxiety and depressive disorders in subjects at high risk for psychosis. The analysis was complemented by a meta-analysis of studies that report on the prevalence of anxiety and depressive symptoms in high-risk samples. Our second aim was to address the impact of anxiety and depressive disorders on the high-risk psychopathology and general functioning. The third aim was to evaluate the longitudinal impact of anxiety and depressive symptoms on transition from a high-risk state to frank psychosis, both in our large database and at a meta-analytical level.
Methods
Definition of Clinical High Risk for Psychosis
Inclusion criteria for a high clinical risk state for psychosis (At-Risk Mental State, ARMS) require the presence of one or more of: (1) Attenuated Psychotic Syndrome (APS), (2) a brief psychotic episode of less than 1 week’s duration that spontaneously remits without antipsychotic medication or hospitalization (Brief Limited Intermittent Psychotic episode, BLIP), (3) trait vulnerability (schizotypal personality disorder or a first-degree relative with psychosis) plus a marked decline in psychosocial functioning (Genetic Risk and Deterioration syndrome, GRD).1
Sample
The total sample consisted of 509 ARMS subjects, collected at baseline from consecutive referrals to two community prodromal services: 290 participants were assessed by the OASIS service in London, UK; and 219 were assessed and treated by the Personal Assessment and Crisis Evaluation (PACE) team in Melbourne, Australia.
Setting
The Outreach and Support in South London (OASIS) is a clinical service located in Lambeth, South London.13 OASIS offers treatment to individuals between 14 and 35 years of age who meet the ARMS criteria for psychosis. The PACE team is a specialist youth mental health service covering the western metropolitan region of Melbourne, Australia.14 It provides clinical service to people aged between 15 and 25 years who are at high risk of psychotic disorder, as assessed again by the ARMS criteria. An active research and clinical collaboration between the two centers has ensured that clinical assessments and measures are standardized across these teams.
Inter-Rater Reliability
Clinical interviews were conducted by experienced clinicians in both teams who were trained in administering the Comprehensive Assessment of the At-Risk Mental State (CAARMS)15 using “The CAARMS Training DVD and Manual.” This complete training package consists of an instructional DVD and supporting workbook. Trainees learn how to use the CAARMS via case scenario interviews and self-assessment practice vignettes. Additionally, the author of the CAARMS (A.R.Y.) and the researcher coordinator at PACE (B.N.) have trained researchers at both the Melbourne and London sites. The inter-rater reliability across the OASIS and PACE has been confirmed in previous studies conducted across the two centers.
Measures
The at-risk signs and symptoms were assessed with the CAARMS. The CAARMS is a semi-structured interview designed to assess prodromal psychopathology in people at high clinical risk for psychosis. The scale has a total of 27 items, which are clustered in seven subscales: Positive Symptoms; Cognitive Change, Attention, and Concentration; Emotional Disturbance; Negative Symptoms; Behavioral Change; Motor/Physical Changes; and General Psychopathology. General level of functioning and reduction in functioning were assessed using the Global Assessment of Functioning (GAF) scale.16
ARMS subjects were followed up over time, and transition to psychosis was defined as the onset of frank psychotic symptoms (hallucinations, delusions, or formal thought disorder) lasting for longer than 1 week.17 The CAARMS criteria for a full-blown psychotic episode require the occurrence of at least one fully (positive) psychotic symptom (variably assessed on the unusual thought content, perceptual abnormality, disorganized speech scales) several times a week for over 1 week. Current anxiety, depressive, and anxiety plus depressive comorbidites were assessed during the initial assessment both at the OASIS and PACE clinics. The DSM diagnoses of current comorbid axis I disorders were assessed with the “Structured Clinical Interview for DSM-IV” (SCID-I).
Meta-Analysis
A systematic PubMed search was performed to identify high-risk studies reporting comorbid anxiety or depressive disorders in high-risk subjects at baseline. The search was conducted up to March 2012, with no time span specified for date of publication. The reference lists of the articles included in the review were manually checked for any studies not identified by the computerized literature search. Studies were included if they: (1) were reported in an original article in a peer-reviewed journal, (2) involved subjects at high risk for psychosis defined according to established international criteria,1 (3) had reported the proportion of high-risk subjects with longitudinal transition to psychosis, (4) had evaluated comorbid anxiety and depressive disorders at baseline. Duplicate studies were excluded. When the proportion of comorbid diagnoses was not indicated in the retrieved article, we contacted the corresponding author to collect the additional data. To achieve a high standard of reporting, we adopted “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines.18
Statistical Analysis
Descriptive statistics included mean and SD for continuous variables and absolute and relative frequencies for categorical variables. Independency between predictors (anxiety, depressive, anxiety and depressive disorders, no anxiety/depressive comorbidities) and CAARMS psychopathology was assessed with the Kruskall-Wallis Test and post hoc comparisons investigated with Mann-Whitney U test. The hypothesis of a linear trend across categories (no comorbid diagnoses > anxiety > depression > depression and anxiety) was tested with the Jonckheere-Terpstra test. To limit risk of false-positive (type I) errors arising from multiple comparisons, we adjusted P < .05 by dividing α with the number of post hoc comparisons. In order to examine if anxiety and depressive comorbidity predicted transition to psychosis, Cox-regression analyses were employed and hazard ratios estimated. Survival curves were calculated by Kaplan-Meier estimates along with the Log-rank test. Data were analyzed with IBM SPSS20.
The meta-analysis was performed using Comprehensive Meta-Analysis (CMA) software version 2 (Biostat, Inc).19 CMA software allows the meta-analysis of proportions using the number of events and the total sample20 and employs the same computational algorithms used by the Cochrane collaborators to weight studies by the inverse variance method.19 Meta-analysis of proportions was performed using logit transformation. The primary effect size measure was the proportion of current depressive and anxiety disorders in subjects with a baseline high-risk state for psychosis. The impact of anxiety and depressive baseline disorders on longitudinal transition risks to psychosis was tested with meta-regression analyses. The slope of meta-regression (β-coefficient: direct [+] or inverse [−]) of the regression line indicated the strength of a relationship between moderator (proportion of anxiety and proportion of depressive disorders) and outcome (risk of psychosis at follow-up).
As the Q statistic and the I 2 index21 identified consistent heterogeneity across studies, random-effect models were employed. The possibility of a small study bias, such as publication bias, was examined by visual inspection of funnel plots and Egger’s test.22
Results
Sociodemographic Characteristics
The sample comprises a total of 509 ARMS individuals. Full details of baseline characteristics for the total sample are shown in table 1.
Table 1.
Baseline Demographic and Clinical Characteristics of the ARMS Sample (n = 509)
| Variable | Level | Median (25th–75th percentiles) or Number (%) |
|---|---|---|
| Age | Years | 20 (17.7–23.7) |
| Gender | Males | 257 (49.7) |
| Females | 256 (50.3) | |
| ARMS subgroup | APS | 360 (70.7) |
| BLIP | 29 (5.7) | |
| GRD | 28 (5.5) | |
| Mixed | 92 (18.1) | |
| Comorbidities | None | 134 (26.3) |
| Anxiety | 39 (7.7) | |
| Depression | 134 (26.3) | |
| Depression and anxiety | 71 (13.9) | |
| Others | 131 (25.7) | |
| GAF | 58 (50.3–64) | |
| CAARMS | ||
| Unusual thought content | Severity | 3 (3–5) |
| Frequency | 3 (3–4) | |
| Perceptual abnormalities | Severity | 3 (2–4) |
| Frequency | 2 (1–3) | |
| Disorganized speech | Severity | 2 (0–3) |
| Frequency | 2 (0–4) | |
Note: ARMS, At-Risk Mental State; CAARMS, Comprehensive Assessment of the At-Risk Mental State; GAF, Global Assessment of Functioning; APS, Attenuated Psychosis Syndrome; BLIP, Brief Limited Intermittent Psychotic episode; GRD, Genetic Risk and Deterioration syndrome; Mixed, a mixture of the above subgroups.
Prevalence of Anxiety and Depressive Symptoms in the ARMS
Over 73% of subjects had an axis I comorbid diagnosis in addition to the at-risk signs and symptoms. About 40% of the ARMS had a comorbid diagnosis of depressive disorders alone (26%) or in association with anxiety disorders (14%). Anxiety disorders alone were less frequent (8%). Other axis I diagnoses were substance use (8%) and obsessive-compulsive disorder (2%).
Meta-Analysis of Anxiety and Depressive Symptoms in Subjects at High Clinical Risk for Psychosis
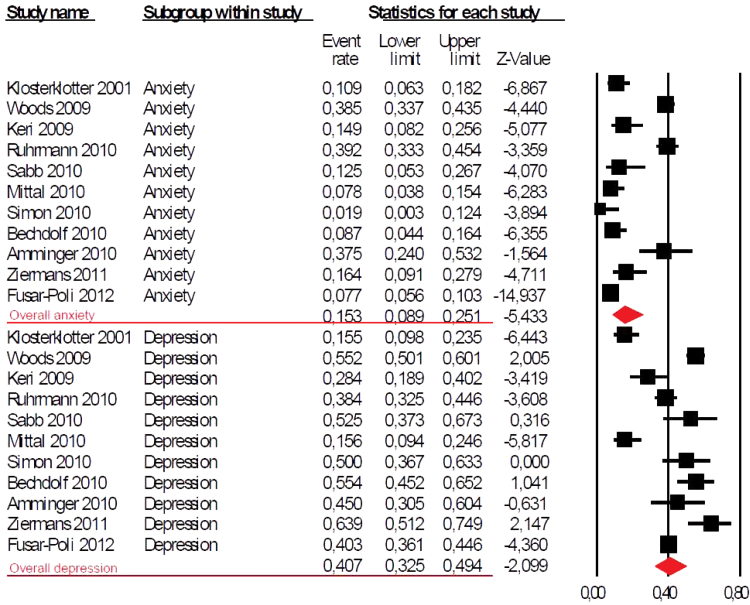
Ten studies published between 2001 and 2011 met inclusion criteria. With the present database, a total of 11 samples were included in the meta-analytical estimate for a total of 1683 subjects (age range 16–29) at high clinical risk for psychosis assessed at baseline for comorbid anxiety and depressive disorders (table 2). Most studies employed standard DSM/SCID diagnostic criteria. The formal meta-analysis revealed that comorbid baseline depressive disorders were present in 40.7% of high-risk subjects (95% CI 32.5%–49.4%; figure 1). Comorbid baseline anxiety disorders were present in 15.3% of high-risk subjects (95% CI 8.9%–25%; figure 1). Meta-regression analyses revealed no significant impact of anxiety or depressive disorders on the longitudinal risk of transition to a frank psychotic episode.
Table 2.
Meta-Analysis of High Risk Studies Reporting Current Anxiety and Depressive Baseline Comorbid Diagnoses and Longitudinal Transition Risks
| Author | Year | Research Center | Assessment Instrument | N HR | HR-T | % Females HR | Mean Age |
|---|---|---|---|---|---|---|---|
| Klosterklotter | 2001 | Multicenter (CER) | BSABS | 110 | 77 | 46.4 | 29 |
| Woodsa | 2009 | Multicenter (NAPLS) | SIPS | 377 | 59 | 37.9 | 18 |
| Keri | 2009 | Hungary | CAARMS | 67 | 31 | 46.3 | 21 |
| Ruhrmannb | 2010 | Multicenter (EPOS) | BSABS, SIPS | 245 | 37 | 44.1 | 23 |
| Sabb | 2010 | Los Angeles | SIPS | 40 | 15 | 30.0 | 17 |
| Mittal | 2010 | Multicenter (Los Angeles) | SIPS | 90 | 24 | 32.2 | 16 |
| Simon | 2010 | Bruderholz | SIPS | 52 | 7 | 40.3 | 20 |
| Bechdolf | 2010 | Melbourne (PACE) | CAARMS | 92 | 20 | 65.2 | 18 |
| Amminger | 2010 | Vienna | CAARMS | 40 | 11 | 66.7 | 16 |
| Ziermans | 2011 | Utrecht (DUPS) | BSABS, SIPS | 61 | 9 | 30.5 | 15 |
| Fusar-Poli | current | Multicenter (OASIS/PACE) | CAARMS | 509 | 76 | 50.3 | 20 |
Note: N HR, number of High Risk subjects; HR-T, number of High Risk subjects who later Transited to psychosis; % Females HR, proportion of females in the High Risk sample; EPOS, Prospective European Prediction of Psychosis Study; NAPLS, North American Prodrome Longitudinal Study; CER, Cologne Early Recognition; PACE, Personal Assessment and Crisis Evaluation; OASIS, Outreach And Support in South-London; DUPS, Dutch Predictor of Psychosis Study; CAARMS, Comprehensive Assessment of At-Risk Mental State; SIPS, Structured Interview for Prodromal Symptoms; BSABS, Bonn Scale for the Assessment of Basic Symptoms.
aRevised analysis of Cannon et al. (2008).12
bComorbidities are reported here.
Fig. 1.
Meta-analysis of comorbid baseline anxiety and depressive diagnoses in subjects at high clinical risk for psychosis. Anxiety 15.3%, 95% CI 8.9%–25%; Depression 40.7%, 95% CI 32.5%–49.4%. Random-effect models applied.
Impact of Anxiety and Depressive Symptoms on ARMS Psychopathology
The presence of anxiety and/or depressive comorbid disorders had a significant effect on the baseline CAARMS psychopathology in the current sample. Not surprisingly, there was consistent correlation with the CAARMS subscales addressing anxiety, depressive/manic symptoms, and obsessive-compulsive symptoms (table 3). More interestingly, there was a linear effect (no comorbidity < anxiety < depression < anxiety and depression) on the suicidality and self-harm scale of the CAARMS. A similar trend was observed with respect to the disorganized/odd/stigmatizing behavior and the avolition/apathy subscales. Finally, comorbid anxiety disorders were associated with higher disorganized speech scores, while comorbid depression (alone or in combination with anxiety disorders) was associated with higher scores on the anhedonia subscale (table 3).
Table 3.
Impact of SCID Anxiety and Depressive Comorbid Diagnoses on Baseline CAARMS Psychopathology
| CAARMS Subscale | Level | No SCID Anxiety or Depression | SCID Anxiety | SCID Depression | SCID Anxiety and Depression | Kruskal-Wallis (P) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Unusual thought content | PS | 4 | 3–5 | 4 | 3–5 | 3 | 2–4 | 3 | 2–4 | .126 |
| Perceptual abnormalities | PS | 3 | 2–4 | 4 | 2–4 | 3 | 2–4 | 3 | 1–4 | .682 |
| Disorganized speech | PS | 2 | 0–2 | 3 | 0.5–3 | 2 | 0–3 | 2 | 0–2.5 | .047 |
| Subjective cognitive changes | CC | 3 | 2–3 | 3 | 2–4 | 2 | 2–3 | 3 | 2–3 | .139 |
| Objective cognitive changes | CC | 0 | 0–2 | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | .187 |
| Subjective emotional disturbances | ED | 2 | 0–2.75 | 2 | 0.5–3 | 2 | 0–3 | 2 | 1–3 | .552 |
| Observed blunted affect | ED | 0 | 0–2 | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | .079 |
| Observed inappropriate affect | ED | 0 | 0 | 0 | 0–1 | 0 | 0–1 | 0 | 0–1 | .932 |
| Alogia | NS | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | 2 | 0–2 | .248 |
| Avolition/apathy | NS | 1 | 1–2 | 2 | 1.5–3.5 | 2 | 2–3 | 3 | 2.5–4 | .030* |
| Anhedonia | NS | 2 | 0–3.75 | 2 | 1–3.5 | 2 | 2–3 | 2 | 2–4 | .006 |
| Social isolation | BC | 2 | 1–3 | 3 | 0.5–3.5 | 3 | 1–3 | 3 | 2–4 | .179 |
| Impaired role function | BC | 3 | 1–4 | 2 | 0.5–4.5 | 3 | 2–4 | 3 | 2–5 | .127 |
| Disorganized, odd, stigmatizing behavior | BC | 0 | 0–1 | 1 | 0–2 | 2 | 1–2 | 3 | 2–3 | .003* |
| Aggression | BC | 3 | 2–4 | 3 | 1.5–3.5 | 3 | 2–3 | 3 | 2–3 | .998 |
| Observed motor functioning | MPC | 1 | 0–2 | 1 | 0–2 | 0 | 0 | 1 | 0–2 | .055 |
| Subjective motor functioning | MPC | 1 | 0–2 | 1 | 0–2 | 0 | 0 | 1 | 0–2 | .253 |
| Subjective bodily sensations | MPC | 0 | 0–2 | 0 | 0–1 | 0 | 0–2 | 1 | 0–2 | .052 |
| Subjective autonomic functioning | MPC | 2 | 0–3 | 2 | 0–3 | 2 | 0–3 | 2 | 0.5–3 | .463 |
| Mania | GP | 0 | 0–1.75 | 2 | 0–3 | 0 | 0–2 | 0 | 0–1.5 | .001 |
| Depression | GP | 2 | 1–2.5 | 3 | 2–4 | 3 | 3–4 | 4 | 3.5–4.5 | <.001* |
| Suicidality and self-harm | GP | 1 | 0–1 | 2 | 0–3 | 3 | 3–4 | 3 | 3–4 | .010* |
| Mood swings | GP | 2 | 0–3 | 2 | 0–2.5 | 2 | 0–3 | 2 | 0.5–3 | .928 |
| Anxiety | GP | 3 | 2–3 | 4 | 3–4 | 4 | 2–4 | 4 | 3.5–5 | <.001* |
| OCD | GP | 0 | 0–2 | 2 | 0–3 | 2 | 1–3 | 2 | 1–3.5 | .005* |
| Dissociative symptoms | GP | 0 | 0–2 | 0 | 0–2 | 0 | 0–2 | 1 | 0–2.5 | .430 |
| Tolerance to normal stress | GP | 3 | 0–3 | 3 | 1.5–4 | 3 | 1–4 | 3 | 2–4 | .051 |
Note: Values represent the median and 25th–75th percentiles; SCID, Structured Clinical Interview for the DSM axis I disorders; CAARMS, Comprehensive Assessment of the At-Risk Mental State; PS, positive symptoms; CC, cognitive change, attention/concentration; ED, emotional disturbance; NS, negative symptoms; BC, behavioral change; MPC, motor/physical changes; GP, general psychopathology; OCD, obsessive compulsive disorder.
*Jonckheere-Terpstra test P < .05.
Impact of Comorbid Anxiety and Depressive Symptoms on ARMS Functioning
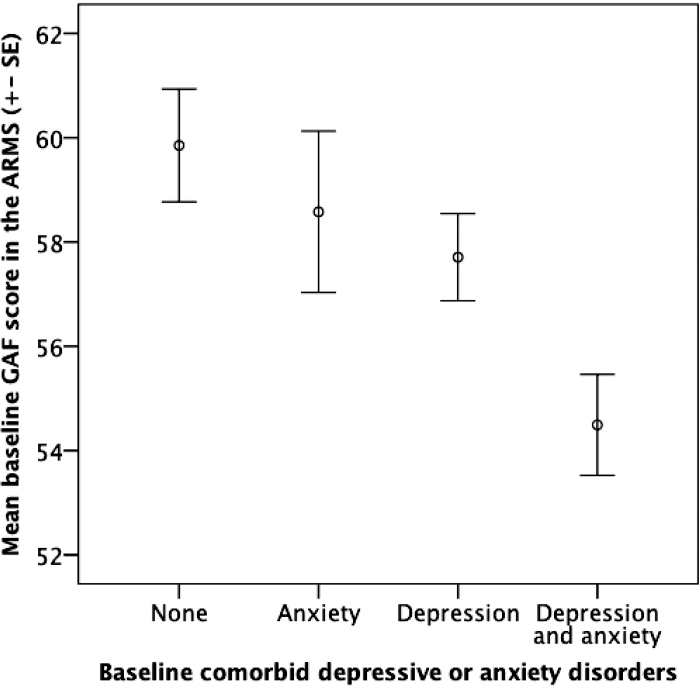
Overall, the presence of baseline comorbid axis I depressive and/or anxiety diagnoses significantly impacted the level of global functioning at baseline. There was a significant linear trend across the different categories, with highest GAF scores in ARMS with no comorbid anxiety/depressive diagnoses, lowest scores in subjects with concurrent anxiety and depressive disorders, and intermediate levels in ARMS subjects with comorbid depressive or anxiety disorders (see figure 2).
Fig. 2.
Impact of comorbid depressive and/or anxiety disorders on the baseline GAF scores of individuals with an ARMS (Kruskall-Wallis test = 0.004, Jonckheere-Terpstra < 0.001).
Impact of Comorbid Anxiety and Depressive Symptoms on Transition to Psychosis
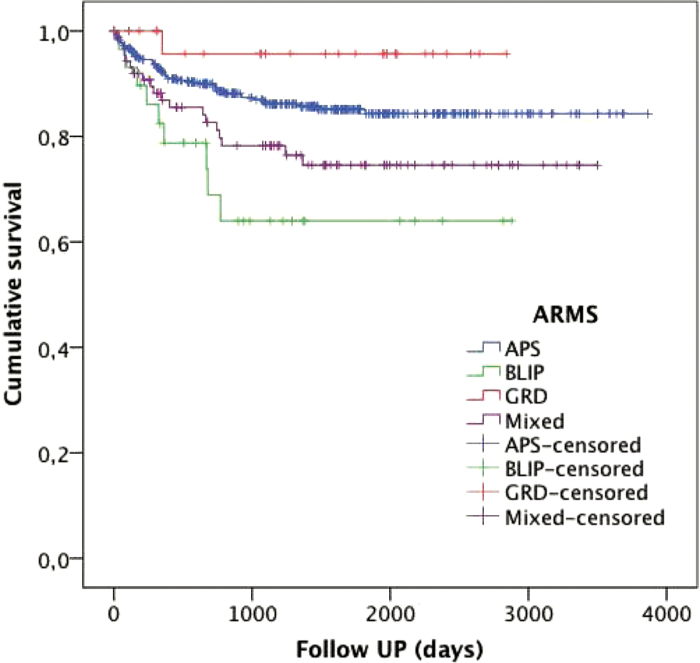
The cohort was followed up for an average of 3.65 years (mean = 1334 days, SD = 924 days), and 76 subjects developed a psychotic episode (14.9%). There was no significant effect of age or gender on the risk of transition to psychosis (P > .05). Similarly, the presence of comorbid axisI diagnoses of anxiety, depression, or concurrent anxiety and depression had no impact on transition risk (P > .05) (table 4). Conversely, there was a significant effect for the ARMS subgroups, with the highest transition risks in the BLIP (31%, HR = 2.8), intermediate transition risks in the mixed (21%, HR = 1.7) and APS (13%, HR = 1.2) subgroups, and lowest transition risks in the GRD subgroup (3.6%), consistent with previous findings17 (figure 3).
Table 4.
Univariate Cox-Regression Analysis of the ARMS Sample (n = 509)
| Variable | Level | Valid | Transition to Psychosis | HR | 95% CI | P | |
|---|---|---|---|---|---|---|---|
| n | n | % | |||||
| Gender | Male | 253 | 41 | 16.21 | 1.199 | 0.764 - 1.883 | 0.430 |
| Females | 256 | 35 | 13.67 | 0.834 | 0.531 - 1.309 | 0.429 | |
| ARMS group | APS | 360 | 47 | 13.06 | 1.163 | 0.941 - 1.403 | 0.057 |
| GRD | 28 | 1 | 3.57 | 0.266 | 0.037 - 1.925 | 0.190 | |
| BLIP | 29 | 9 | 31.03 | 2.753 | 1.347 - 5.624 | 0.005 | |
| Mixed | 92 | 19 | 20.65 | 1.744 | 1.023 - 2.971 | 0.041 | |
| Comorbidity | None | 134 | 19 | 14.18 | 0.745 | 0.415 - 1.370 | 0.355 |
| Anxiety | 39 | 6 | 15.38 | 1.089 | 0.473 - 2.508 | 0.842 | |
| Depression | 134 | 17 | 12.69 | 0.849 | 0.494 - 1.457 | 0.552 | |
| Depression and anxiety | 71 | 9 | 12.68 | 0.787 | 0.392 - 1.580 | 0.501 | |
| Others | 131 | 25 | 19.08 | 1.375 | 0.685 - 2.760 | 0.370 | |
Note: HR, hazards ratio; APS, Attenuated Psychosis Syndrome; BLIP, Brief Limited Intermittent Psychotic episode; GRD, Genetic Risk and Deterioration syndrome; Mixed, a mixture of the above subgroups; ARMS, At-Risk Mental State.
Fig. 3.
Kaplan-Meier survival estimates of transition risks stratified for ARMS subgroups (n = 509) over follow-up (mean = 3.65 years). APS, Attenuated Psychosis Syndrome; BLIP, Brief Limited Intermittent Psychotic episode; GRD, Genetic Risk and Deterioration syndrome; Mixed, a mixture of the above subgroups.
Discussion
The first aim of the present study was to measure the prevalence of comorbid anxiety and depressive diagnoses in subjects at high clinical risk for psychosis. In a large sample of 509 ARMS subjects, we found a high prevalence (73%) of comorbid axis I diagnoses in addition to the at-risk signs and symptoms. About 40% of the ARMS had a comorbid diagnosis of depressive disorders, while anxiety disorders alone were less frequent (8%). These findings were confirmed at meta-analytical level in 1683 high-risk subjects, with baseline comorbid depressive and anxiety disorders being present in 41% and 15% of subjects, respectively. These findings are also relevant to the recent discussion regarding the inclusion of an APS as a new diagnostic category in the DSM-5. This proposal included the requirement that subthreshold psychotic symptoms such as hallucinations, delusions, and disorganized speech should not be “better explained by another DSM-5 diagnosis.” However, it seems that this would be difficult to determine if comorbid axis I diagnoses are met in 73% of ARMS subjects, and psychotic experiences are reasonably common features of mood and anxiety disorders.23
Our second aim was to address the impact of these comorbid diagnoses on psychopathology and functioning. Comorbid anxiety disorders were found to be associated with higher disorganized speech scores, suggesting that high anxiety could trigger thought disorder and interfere with linguistic expression, leading to higher scores on this scale. Alternatively, the experience of thought disorder and communication difficulties may be a prominent source of anxiety in ARMS subjects. Similarly, comorbid depression was associated with higher scores on the anhedonia subscale, pointing to the close association between affective and negative psychopathological domains in prodromal psychosis. We also identified a linear effect of axis I comorbidity (no comorbidity < anxiety < depression < anxiety and depression) on the disorganized/odd/stigmatizing behavior and the avolition/apathy subscales. Although we found no evidence that anxiety or depressive symptoms are direct predictors of later development of psychosis, disorganized behavior and negative symptoms are among the most replicated predictors of transition to psychosis and poor longitudinal functioning.1,24 A similar cumulative load for accumulating anxiety and depressive comorbidities was evident on the suicidality and self-harm scale of the CAARMS. Although this is not surprising due to suicidality/self-harm being a prominent feature of depressive and anxiety disorders, it raises the clinical potential of identifying at baseline assessment the ARMS subjects at higher risk of self-harm behaviors and developing more focused therapeutic strategies and risk monitoring for this vulnerable subgroup of patients. Similar clinical applications can be inferred from the strong correlations between anxiety and depressive disorders and scores on the CAARMS subscales addressing anxiety, depressive/manic symptoms, and obsessive-compulsive symptoms. ARMS subjects with high scores on these subscales should be systematically evaluated for concurrent axis I disorders. Comorbid anxiety and depressive diagnoses at baseline were significantly associated with lower levels of baseline global functioning as indexed by the GAF scores. The experience of high-risk symptoms per se is associated with a marked impairment in psychosocial functioning,7 which appears to be a core feature of this state.25 Anxiety and depressive disorders may further impair the coping strategies of high-risk subjects and their ability to function in the social and familiar environment. This is of particular interest as psychosocial impairment is an independent predictor of longitudinal outcome7,26 and tends to be resistant to treatment, both pharmacological and psychosocial.27 It is also reflected by a considerably decreased subjective quality of life.28,29
The notion of mood and anxiety disorders as “impacting” on ARMS features (and vice versa) assumes a neat distinction between these constructs, ie, they are readily distinguishable entities that might interact or have causal impact on each other. However, these two aspects are phenomenologically connected as core unifying characteristics of the “delusional mood” predating delusion formation and psychosis onset.30 According to Conrad’s classic model, during this period (the “trema” or “stage fright”), the ARMS patient may experience an increasingly oppressive internal tension, “a feeling of nonfinality” or expectation, describing that something is “in the air” without being able to say what exactly has changed.30 These subjective experiences can vary between patients but are usually characterized by a marked change of “emotional-motivational” state, which can be expressed in anxiety and depressive symptoms. At first, the stage fright is associated with the most salient experiences but eventually spreads to pervade the patient’s entire experiential field, leading to delusion formation and aberrant interpretation of reality. At a diagnostic level, the separation of these symptom clusters into distinct disorders in ARMS subjects is based on a strict diagnostic manual-based approach (a SCID interview) that assumes the symptoms belong in separate categories. However, as these symptom clusters phenomenologically overlap in prodromal psychosis, they may not necessarily be indicative of two (or more) separate disorders but rather be an expression of an emerging single “disorder” with diverse symptoms that happen to reach threshold levels for multiple diagnosable disorders.31–33 Therefore, the concept of “comorbidity” is somewhat problematic. However, the “primary” disorder is unclear at this early stage of presentation. It is currently impossible to distinguish patients with a nonpsychotic disorder, such as depression or anxiety with associated (attenuated) psychotic symptoms, from patients with an emerging psychotic disorder with depressive and anxiety symptoms. Only longitudinal course will clarify these possibilities in individual patients. There is ongoing research into phenotypic and endophenotypic features that might provide early markers of which disorders these symptom clusters will evolve into.1 An alternative conceptualization is that depression, anxiety negative symptoms, cognitive impairment, and positive psychotic symptoms all occur on a continuum, and that apparent “disorders” reflect whichever of these, or combination of these, is most prominent. For example, schizophrenia could be seen as a syndrome with prominent negative cognitive and positive psychotic symptoms, while unipolar depression will have prominent depressive symptoms, with some anxiety and positive symptoms.
These findings are in line with our clinical experience in two of the largest prodromal centers worldwide, where we have observed that anxiety and depressive symptoms and functional disability are often of more concern to the high-risk patients than their subthreshold psychotic symptoms. This is also consistent with high prevalence of psychotic-like experiences in the general population that are not associated with subjective distress, low functioning, or psychosocial impairments34 and that, therefore, do not trigger help-seeking behaviors (see the point below on Berkson’s bias).
The third aim of the study was to examine the association between baseline comorbid anxiety and depressive diagnoses and transition to psychosis. We found that these comorbid diagnoses had no effect on risk of transition to frank psychotic illness. Meta-regression analyses in the available literature confirmed the lack of predictive value of baseline axis I anxiety and/or depressive diagnoses in determining the transition to psychosis. The lack of predictive effect of accumulating comorbid axis I depressive diagnoses is in line with the findings of the multicenter NAPLS (North American Prodrome Longitudinal Study) in Unites States.9 It is possible that this negative finding may be the result of the relatively low transition rate (14.9%) in our sample. However, the previous study (with a smaller sample) indicating a significant association between diagnosis of a nonpsychotic disorder and transition to psychosis reported a very similar transition rate (15.1%).10 Furthermore, our complementary meta-regression analyses between proportion of comorbid depressive or anxiety disorders and risk of psychosis confirmed no significant association in the available literature. There is thus converging evidence suggesting depressive and anxiety comorbidities in ARMS subjects do not impact transition to psychosis. However, the fact that most individuals defined as high risk have a diagnosis of depression or anxiety disorders at baseline may be fundamental in explaining the risk function of the whole sample. Copresence of psychotic symptomatology in disorders of anxiety and depression is common,11 and their accumulating comorbidity in help-seeking subjects can impact on prognosis.35 This effect was firstly observed by Berkson (Berkson’s bias)36 in other clinical populations. Thus, high rates of comorbidity between ARMS and depressive/anxiety symptoms may in part be an artefact of both features independently influencing help-seeking behavior and need for care.37 Accumulating comorbidities may partly or wholly mediate the treatment-seeking feature that defines the high-risk population and, in this fashion, explain the marked impairment in psychosocial functioning that appears as a core feature of the high-risk state, impacting on course and outcome.1 Although we found no direct support towards transition risk enrichment by depressive or anxiety comorbidities, our results cannot exclude the possibility that the initial selection of high-risk subjects is based in part on inclusion of those with common mental disorders and psychotic experiences, and that these as a group have poorer prognosis compared to those with common mental disorders without psychotic experiences and those with psychotic experiences without anxiety and/or depression. Future longitudinal studies are required to carefully differentiate “pseudo-comorbidities” representing emotional dysregulation features of the ARMS from true anxiety or depressive disorders not associated with psychotic outcomes. There is an additional need to clarify the impact of sampling process, because current high-risk cohorts are opportunistic, each study using a different, unique strategy that cannot be exactly replicated and ultimately leading to different proportions of anxiety or depressive comorbidities.
Furthermore, the exact meaning of “transition” is uncertain.38 The psychosis threshold employed to define the illness onset in high-risk subjects is arbitrary and poorly validated.39 If the current psychometric cut-off for psychosis were approximately correct, then individuals who make transition should have a worse course and outcome than those who do not make transition. Unfortunately, there are no studies testing this, with most studies focusing on rates of psychosis rather than symptomatic or functional outcome.39 We cannot thus exclude that the high prevalence of anxiety or depressive disorders may affect functioning not only at baseline but also longitudinally, with higher depressive and anxious symptoms in subjects who do not fully remit from their initial ARMS status.
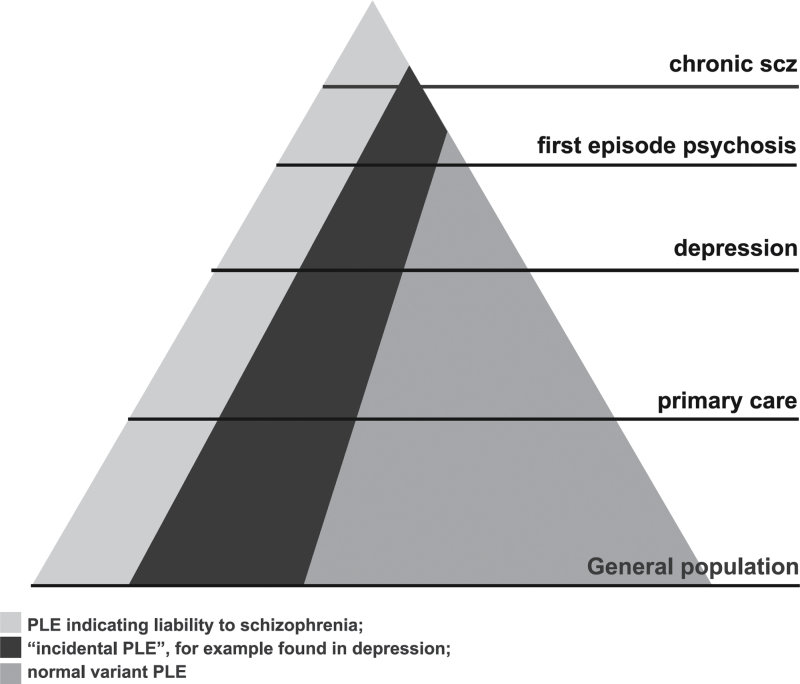
In the largest study published to date, the nonconverting high-risk group demonstrated significant improvement in attenuated positive symptoms, negative symptoms, and social and role functioning.40 However, this group kept functioning at a lower level than nonpsychiatric comparison subjects, suggesting that initial high-risk categorization is associated with persistent disability, at least for a significant proportion.40 This persistent disability may be due to the fact that patients who are assessed in prodromal services may in some instances present with symptoms belonging to different but overlapping diagnostic spectra. The nonconverting, but nonremitting, subjects who display continuous ARMS symptoms may have a higher liability to experience mental sequelae, and persistent ARMS symptoms may represent only one aspect of this. In other words, our results cannot exclude that subclinical psychotic symptoms, at least in part, can be attributed to a general susceptibility to various mental disorders. For example, the psychotic-like symptoms may be incidental to depressive disorder, as we have previously proposed.41 Our model theorized that there are different types of attenuated psychotic symptoms associated with different levels of risk for psychotic disorder. Some attenuated psychotic symptoms may reflect the emergence of an underlying “core” psychotic process; some may be “clinical noise” or epiphenomena associated with a nonpsychotic clinical condition; and some may be normal variations amongst the general population. As noted in this model, individuals with depression and incidental subthreshold psychotic symptoms would not be expected to have a high transition rate to psychotic disorder41 but would have poor functioning. In line with our theory is the finding that psychotic-like symptoms decrease in parallel with reduction in mood and anxiety symptoms in two independent clinical samples (NAPLS40 and Yung et al.42). The proportion of each of these types of psychotic-like symptoms would vary depending on the population. That is, there would be a high proportion of psychotic-like symptoms indicating schizophrenia vulnerability in a sample drawn from a tertiary psychiatric institution but a high proportion of “incidental” psychotic symptoms in a group presenting to primary care. This model is illustrated in figure 4.
Fig. 4.
Hypothesized proportion of each type of attenuated psychotic symptoms (psychotic-like experience, PLE) in different populations.
A recent study in a representative community sample of over 3000 adolescents and young adults found that copresence of psychotic symptomatology in disorders of anxiety and depression is common.23 This finding reinforces the view that the high-risk psychopathology is characterized by overlapping dimensional liabilities.23 Taken together with the new decision of moving the APS in the research appendix of DSM-5, emergence of subclinical ARMS psychotic symptoms may constitute a nonspecific marker of mental suffering31 and may occur as epiphenomena of stress or of anxiety/depressive disorders in patient samples43 without necessarily indexing actual psychosis risk. In line with this ARMS model including several outcomes other than psychosis, self-reported attenuated psychotic symptoms can predict nonpsychotic mental disorders later in life.44
Our results have clinical relevance. The largest randomized controlled trial in subjects at risk for psychosis has just been published, with inconclusive and concerning results. The study showed cognitive therapy plus monitoring did not significantly reduce transition to psychosis compared to monitoring alone but significantly reduced the frequency and intensity of psychotic experiences in 288 young people at high risk.45 More importantly, the authors noted that cognitive therapy did not significantly affect distress related to these psychotic experiences, nor levels of depression, social anxiety, and satisfaction with life.45 On the other hand, monitoring represented an enhancement over routine care because it aimed to provide warm, empathic contact and supportive listening and crisis management, with possible impact on the underlying psychopathology. Overall, this study clearly indicates that current treatments for high-risk subjects are not targeting core symptomatic domains that, beyond transition to psychosis, are highly frequent and account for persistent functional impairment, decreased quality of life, and long-term disability.
With our study and meta-analysis available, it appears clear that future interventions in the field need to address not only the preventative efficacy on psychosis transition but also their effectiveness in improving the functioning of this patient population by reducing anxiety and depressive comorbidities. Furthermore, the results of our study should be carefully considered by future studies addressing the neurobiological characteristics of the ARMS. Because anxiety and depressive symptoms have specific neuroanatomical, neurofunctional, and neurochemical features,46,47 the high prevalence of these problems in the ARMS could potentially increase heterogeneity across individual neuroimaging studies48–50 and ultimately prevent the identification of reliable and replicable markers.
Conclusions
A large majority of ARMS subjects present with comorbid axis I diagnoses, mainly depressive or anxiety disorders, in addition to their attenuated psychotic symptoms. The high prevalence of these comorbidities in ARMS subjects may phenomenologically reflect the delusional mood and emotional dysregulation processes predating the onset of attenuated positive symptoms. Anxiety and depressive symptoms are likely to influence presenting psychopathology and global functioning but do not affect the risk of transition to psychotic disorder. Psychotic-like symptoms may be nonspecific and indicative of high risk of psychotic disorder or may be epiphenomena of other mental disorders.
References
- 1. Fusar-Poli P, Borgwardt S, Bechdolf A, et al. The psychosis high risk state: a comprehensive state of the art review. Arch Gen Psychiatry. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fusar-Poli P, Yung AR. Should attenuated psychosis syndrome be included in DSM-5? Lancet. 2012; 379: 591–592 [DOI] [PubMed] [Google Scholar]
- 3. Fusar-Poli P, Bonoldi I, Yung AR, et al. Predicting psychosis: a meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry. 2012; 69: 1–10 [DOI] [PubMed] [Google Scholar]
- 4. Fusar-Poli P, Bechdolf A, Taylor M, et al. At risk for schizophrenic or affective psychosis? A meta-analysis of DSM/ICD diagnostic outcomes in individuals at high clinical risk. [published online ahead of print May 15, 2012]. Schizophr Bull. 10.1093/schbul/sbs060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fusar-Poli P, Deste G, Smieskova R, et al. Cognitive functioning in prodromal psychosis: a meta-analysis. Arch Gen Psychiatry. 2012; 69: 1–10 [DOI] [PubMed] [Google Scholar]
- 6. Fusar-Poli P, Howes OD, Allen P, et al. Abnormal prefrontal activation directly related to pre-synaptic striatal dopamine dysfunction in people at clinical high risk for psychosis. Mol Psychiatry. 2011; 16: 67–75 [DOI] [PubMed] [Google Scholar]
- 7. Velthorst E, Nieman DH, Linszen D, et al. Disability in people clinically at high risk of psychosis. Br J Psychiatry. 2010; 197: 278–284 [DOI] [PubMed] [Google Scholar]
- 8. Häfner H, Löffler W, Maurer K, Hambrecht M, an der Heiden W. Depression, negative symptoms, social stagnation and social decline in the early course of schizophrenia. Acta Psychiatr Scand. 1999; 100: 105–118 [DOI] [PubMed] [Google Scholar]
- 9. Woods SW, Addington J, Cadenhead KS, et al. Validity of the prodromal risk syndrome for first psychosis: findings from the North American Prodrome Longitudinal Study. Schizophr Bull. 2009; 35: 894–908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Salokangas RK, Ruhrmann S, von Reventlow HG, et al. Axis I diagnoses and transition to psychosis in clinical high-risk patients EPOS project: prospective follow-up of 245 clinical high-risk outpatients in four countries. Schizophr Res. 2012;138:192–197.; [DOI] [PubMed] [Google Scholar]
- 11. Wigman JT, van Nierop M, Vollebergh WA, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity—implications for diagnosis and ultra-high risk research. Schizophr Bull. 2012; 38:247–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008; 65: 28–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fusar-Poli P, Byrne M, Badger S, McGuire PK, Valmaggia L. Outreach and Support in South London (OASIS), 2001–2011: ten years of early diagnosis and treatment for young individuals at clinical high risk for psychosis. Eur Psychiatry. 10.1016/j.eurpsy.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 14. Yung AR, McGorry PD, Francey SM, et al. PACE: a specialised service for young people at risk of psychotic disorders. Med J Aust. 2007; 187: S43–S46 [DOI] [PubMed] [Google Scholar]
- 15. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005; 39: 964–971 [DOI] [PubMed] [Google Scholar]
- 16. Hall RC. Global assessment of functioning. A modified scale. Psychosomatics. 1995; 36: 267–275 [DOI] [PubMed] [Google Scholar]
- 17. Nelson B, Yuen K, Yung AR. Ultra high risk (UHR) for psychosis criteria: are there different levels of risk for transition to psychosis? Schizophr Res. 2011; 125: 62–68 [DOI] [PubMed] [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339: b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Borenstein MHL, Higgins J, Rothstein H. Comprehensive Meta-analysis Version 2. Englewood, NJ: Biostat; 2005. [Google Scholar]
- 20. Nielssen O, Large M. Rates of homicide during the first episode of psychosis and after treatment: a systematic review and meta-analysis. Schizophr Bull. 2010; 36: 702–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lipsey M, Wilson D. Practical Meta-analysis. Thousand Oaks, CA: Sage Publications; 2000; [Google Scholar]
- 22. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315: 629–634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wigman JT, van Nierop M, Vollebergh WA, et al. Evidence that psychotic symptoms are prevalent in disorders of anxiety and depression, impacting on illness onset, risk, and severity–implications for diagnosis and ultra-high risk research. Schizophr Bull. 2012; 38: 247–257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Demjaha A, Valmaggia L, Stahl D, Byrne M, McGuire P. Disorganization/cognitive and negative symptom dimensions in the at-risk mental state predict subsequent transition to psychosis. Schizophr Bull. 2012;38:351–359; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Seidman LJ, Giuliano AJ, Meyer EC, et al. North American Prodrome Longitudinal Study (NAPLS) Group Neuropsychology of the prodrome to psychosis in the NAPLS consortium: relationship to family history and conversion to psychosis. Arch Gen Psychiatry. 2010; 67: 578–588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fusar-Poli P, Byrne M, Valmaggia L, et al. Social dysfunction preducts two years clinical outcomes in people at ultrahigh risk for psychosis. J Psychiatr Res. 2009; 44: 294–301 [DOI] [PubMed] [Google Scholar]
- 27. Cornblatt B, Carrión R, Addington J, et al. Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38:1247–1257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ruhrmann S, Paruch J, Bechdolf A, et al. Reduced subjective quality of life in persons at risk for psychosis. Acta Psychiatr Scand. 2008; 117: 357–368 [DOI] [PubMed] [Google Scholar]
- 29. Bechdolf A, Pukrop R, Köhn D, et al. Subjective quality of life in subjects at risk for a first episode of psychosis: a comparison with first episode schizophrenia patients and healthy controls. Schizophr Res. 2005; 79: 137–143 [DOI] [PubMed] [Google Scholar]
- 30. Mishara AL. Klaus Conrad (1905–1961): delusional mood, psychosis, and beginning schizophrenia. Schizophr Bull. 2010; 36: 9–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Os J, Linscott RJ. Introduction: The extended psychosis phenotype–relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr Bull. 2012; 38: 227–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McGorry PD, Nelson B, Goldstone S, Yung AR. Clinical staging: a heuristic and practical strategy for new research and better health and social outcomes for psychotic and related mood disorders. Can J Psychiatry. 2010; 55: 486–497 [DOI] [PubMed] [Google Scholar]
- 33. Tyrer P, Seivewright N, Ferguson B, Tyrer J. The general neurotic syndrome: a coaxial diagnosis of anxiety, depression and personality disorder. Acta Psychiatr Scand. 1992; 85: 201–206 [DOI] [PubMed] [Google Scholar]
- 34. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009; 39: 179–195 [DOI] [PubMed] [Google Scholar]
- 35. Perlis RH, Uher R, Ostacher M, et al. Association between bipolar spectrum features and treatment outcomes in outpatients with major depressive disorder. Arch Gen Psychiatry. 2011; 68: 351–360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maric N, Myin-Germeys I, Delespaul P, de Graaf R, Vollebergh W, Van Os J. Is our concept of schizophrenia influenced by Berkson’s bias? Soc Psychiatry Psychiatr Epidemiol. 2004; 39: 600–605 [DOI] [PubMed] [Google Scholar]
- 37. Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biometrics. 1946; 2: 47–53 [PubMed] [Google Scholar]
- 38. Fusar-Poli P, Van Os J. Lost in transition: setting the psychosis threshold in prodromal research [published online ahead of print November 9, 2012]. Acta Psychiatr Scand. 10.1111/acps.12028 [DOI] [PubMed] [Google Scholar]
- 39. Yung AR, Nelson B, Thompson A, Wood SJ. The psychosis threshold in Ultra High Risk (prodromal) research: is it valid? Schizophr Res. 2010; 120: 1–6 [DOI] [PubMed] [Google Scholar]
- 40. Addington J, Cornblatt BA, Cadenhead KS, et al. At clinical high risk for psychosis: outcome for nonconverters. Am J Psychiatry. 2011; 168: 800–805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yung AR, Nelson B, Baker K, Buckby JA, Baksheev G, Cosgrave EM. Psychotic-like experiences in a community sample of adolescents: implications for the continuum model of psychosis and prediction of schizophrenia. Aust N Z J Psychiatry. 2009; 43: 118–128 [DOI] [PubMed] [Google Scholar]
- 42. Yung AR, Buckby JA, Cosgrave EM, et al. Association between psychotic experiences and depression in a clinical sample over 6 months. Schizophr Res. 2007; 91: 246–253 [DOI] [PubMed] [Google Scholar]
- 43. Varghese D, Scott J, Welham J, et al. Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr Bull. 2011; 37: 389–393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Werbeloff N, Drukker M, Dohrenwend BP, et al. Self-reported attenuated psychotic symptoms as forerunners of severe mental disorders later in life. Arch Gen Psychiatry. 2012;69:467–475; [DOI] [PubMed] [Google Scholar]
- 45. Morrison AP, French P, Stewart SL, et al. Early detection and intervention evaluation for people at risk of psychosis: multisite randomised controlled trial. BMJ. 2012; 344: e2233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sacher J, Neumann J, Fünfstück T, Soliman A, Villringer A, Schroeter ML. Mapping the depressed brain: a meta-analysis of structural and functional alterations in major depressive disorder. J Affect Disord. 2012; 140: 142–148 [DOI] [PubMed] [Google Scholar]
- 47. Radua J, van den Heuvel OA, Surguladze S, Mataix-Cols D. Meta-analytical comparison of voxel-based morphometry studies in obsessive-compulsive disorder vs other anxiety disorders. Arch Gen Psychiatry. 2010; 67: 701–711 [DOI] [PubMed] [Google Scholar]
- 48. Fusar-Poli P, Borgwardt S, Crescini A, et al. Neuroanatomy of vulnerability to psychosis: a voxel-based meta-analysis. Neurosci Biobehav Rev. 2011; 35: 1175–1185 [DOI] [PubMed] [Google Scholar]
- 49. Fusar-Poli P, Radua J, McGuire P, Borgwardt S. Neuroanatomical maps of psychosis onset: voxel-wise meta-analysis of antipsychotic-naive VBM studies. Schizophr Bull. 2012;38:1297–1307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fusar-Poli P, Stone JM, Broome MR, et al. Thalamic glutamate levels as a predictor of cortical response during executive functioning in subjects at high risk for psychosis. Arch Gen Psychiatry. 2011; 68: 881–890 [DOI] [PubMed] [Google Scholar]