Abstract
Context:
Cross-sectional studies of the signs and symptoms of psychosis yield dimensional phenotypes. However, the validity and clinical utility of such dimensions remain debated. This study investigated the structure of psychotic symptomatology, the stability of the structure over time, and the concordance between symptom dimensions and categorical diagnoses.
Methods:
Sample consisted of 500 first-episode psychotic patients. A cross-sectional study (N = 500) investigated the organizational structure of symptom dimensions at the onset of psychosis and its concordance with categorical diagnoses; next, a nested longitudinal study (N = 100) examined the stability of the symptom dimensions structure after 5–10 years of follow-up.
Results:
Factor analyses identified 6 first-order factors (mania, negative, disorganization, depression, hallucinations, and delusions) and 2 high-order factors (affective and nonaffective psychoses). Cumulative variance accounted for by the first and high-order factors was 63%: 31% by the first-order factors and 32% by the high-order factors. The factorial structure of psychotic symptoms during first episode remained stable after 5–10 years of follow-up. The overall concordance between 4 categorical diagnostic groups (schizophrenia, mania with psychosis, psychotic depression and schizoaffective disorder) and dimensional symptom ranged from 62.2% to 73.1% (when the schizoaffective group was excluded).
Conclusions:
Symptoms of psychosis assume a multidimensional hierarchical structure. This hierarchical model was stable over time and showed good concordance with categorical diagnoses. The combined use of dimensional and categorical approach to psychotic disorders would be of clinical and research utility.
Key words: symptom dimensions, diagnostic classification, psychosis, DSM-5, longitudinal study
Introduction
Current primary diagnostic systems, the Diagnostic of Statistical Manual of Mental Disorders (DSM-IV) and the International Statistical Classification of Diseases and Related Health Problem (ICD-10), adopt a categorical approach to classifying psychotic disorders. Evidence, however, points to differences in premorbid course, psychopathology, treatment, cognitive performance, and outcome within the same diagnosis.1–3 Furthermore comorbidity and overlap on pharmacological pathway,4 genetic susceptibility,5,6 and neuroanatomy7 exist between schizophrenia and other psychotic disorders. Collectively, such evidence raises concerns as to the validity and reliability of the categorical diagnostic approach.8,9
Unlike the categorical diagnostic approach, the symptom approach considers psychopathology as lying on a multiple continuum dimensions.9 Symptom dimensions (also referred to as factors) are measures of discrete symptoms that are more likely to occur together than by chance alone.9–11 There is a long historical tradition of factor analytic studies that aim to identify the natural organization of symptoms of psychiatric disorders.12,13 Examples include empirical identification of clinical scales, based on factorial models, such the Positive and Negative Syndrome Scale (PANSS)14 that measures symptom severity in schizophrenia. The rationale behind such a scale is the identification of groups of symptoms that best represent the structure of psychopathology (ie, for the PANSS positive and negative symptom severity in schizophrenia).
The integration of the symptom dimensional and categorical models has been proposed in the forthcoming DSM-5.15,16 Research into the structure of psychotic symptomatology has identified multiple potential factors. Among patients with schizophrenia not only strictly symptom dimensions of schizophrenia are observed. For example, factor analytic studies of early and chronic schizophrenia both identify a positive symptom dimension that includes hallucinations and delusions,17,18 and a negative symptom dimension including restricted affect, avolition, anhedonia, and social withdrawn.19 Moreover, when mood symptoms are assessed and included in the factor analysis, manic and depressive factors are found.8,11,20,21 Thus, the overlap between dimensions is vague across diagnoses.
Although the above studies support the presence of multiple symptom dimensions across psychotic disorders, at present 3 critical questions pertinent to the validity of the dimensional approach remain unresolved. First, there is no consensus regarding the structure of the dimensional model of psychosis; it is unclear whether symptom dimensions are related to one other and whether they assume a hierarchical form. To date, 1 study has shown that psychopathology in chronic patients can be hierarchically conceptualized in a tree-organization composed by 2 main branches (affective and nonaffective psychosis) and a total of 10 basic psychopathological dimensions.22 Second, there is limited empirical evidence supporting the stability of symptom dimension structure across time. Investigation of the stability of the form that psychosis assumes is needed to establish the validity of a dimensional model. Finally, the concordance between symptom dimensions and categorical diagnoses remains largely unknown.
The current literature does not provide satisfactory answers to these 3 questions for several reasons. First, most studies used small samples that may not represent the population of individuals with psychosis. Second, generally, studies focus on schizophrenia and not on the psychotic spectrum. Third, longitudinal studies examining the structure of symptoms have been done on schizophrenia23,24 but not on large sample of first episode of psychosis. Fourth, many studies use samples of chronic or institutionalized patients that increase the risk of results to be confounded by medication and institutionalization. Here 2 studies are reported: a cross-sectional study on 500 first-episode psychotic patients and a longitudinal study of 100 of these, who were followed up in their first decade of the illness. Using symptom data systematically collected from direct assessment interviews and observations, we explore symptom dimensions in first-episode psychosis in terms of (a) their structure; (b) their concordance with diagnostic categories; and (c) their stability over the first 10 years of the psychotic illness.
Methods
Participants
Cross-sectional Study.
Five hundred first-episode psychotic patients were included in the study. The study was approved by local Ethics Committee, and each participant gave written informed consent after receiving a complete description of the study. The study identified all cases with a first episode of a functional psychosis aged 16–65 years who were presented to specialist mental health services of the South London and Maudsley National Health Service Foundation Trust that serves a well-defined catchment area. Exclusion criteria were (a) previous contact with health services for psychosis; (b) organic causes of psychotic symptoms; (c) transient psychotic symptoms due to acute intoxication (as defined by ICD-10); and (d) moderate or severe mental retardation (an intelligence quotient score below 50).
Longitudinal Study.
The following inclusion criteria were considered to select patients in the longitudinal study: (a) between 5 and 10 years from the baseline assessment and (b) presence of psychotic symptoms during the follow-up period. Data for 323 of the original 500 patients were available. However, of these 323, 186 did not have sufficient clinical information for scoring the Item Group Checklist (see paragraph “Symptom rating and diagnostic classification”), 37 did not present with psychotic symptoms. The remaining 100 patients met inclusion criteria and were used in the longitudinal study. Patients included in the longitudinal study were similar to those patients included in the cross-sectional study in terms of age at first assessment, gender, and ethnic characteristics (all P-values >.05). The average time of the follow-up assessment was 9 years. The sociodemographic and clinical characteristics of the longitudinal study sample at onset and at follow-up are presented in table 1.
Table 1.
Demographic and Clinical Characteristics of the Cross-sectional and Longitudinal Samples
| Cross-sectional | Longitudinal | |||
|---|---|---|---|---|
| Gender | ||||
| Male | 290 (58%) | 59 (59%) | ||
| Female | 210 (42%) | 41 (41%) | ||
| Ethnicity | ||||
| White British/other | 121 (24.2%) | 17 (17%) | ||
| Black Caribbean/African | 266 (53.2%) | 63 (63%) | ||
| Asian | 20 (4%) | 3 (3%) | ||
| Other | 93 (18.6%) | 17 (17%) | ||
| Diagnostic categories | ||||
| Schizophrenia spectrum disorders | 251 (50.2%) | 58 (58%) | ||
| Schizoaffective disorder | 49 (9.8%) | 4 (4%) | ||
| Mania with psychotic features | 67 (13.4%) | 12 (12%) | ||
| Psychotic depression | 50 (10%) | 9 (9%) | ||
| Other psychotic disorders | 83 (16.6%) | 17 (17%) | ||
| Mean (SD) | Range | Mean (SD) | Range | |
| Age | 29.94 (9.8) | 16–62 | 37.5 (8.8) | 24–70 |
Note: DSM-IV codes included in each diagnostic category: schizophrenia spectrum disorders (295.10, 295.30, 295.40, 295.60, 295.60, 295.90);
schizoaffective disorder (295.70); mania with psychotic features (296.04, 296.44, 296.54, 296.64); psychotic depression (296.24, 296.34);
other psychotic disorders (297.1, 298.8, 298.9).
Symptom Rating and Diagnostic Classification
Psychopathology was assessed using the Schedules for Clinical Assessment in Neuropsychiatry (SCAN).25 The SCAN was chosen because it makes no a priori assumptions about the dimensions of psychosis and avoids potential bias associated with concept-driven instrument that could reproduce dimensions that simply reflect their underlying construct.25 The 4 weeks before the admission were used as the rating time frame. Symptom assessment was based on the clinical interview with the patient, case note review, and information from other informants (eg, health professionals).
The SCAN incorporates the Present State Examina tion, tenth edition (PSE-10)—which is used to elicit symptom—the Item Group Checklist (IGC), the Clinical History Schedule, and the Glossary. Only sessions of the PSE related to psychosis were administered (eg, items concerning anxiety disorders were excluded). The PSE and IGC are the most relevant parts on the SCAN interview. The IGC combines symptoms, assessed during the PSE interview, into specific groups of symptoms that are then scored from 0 (absent) to 2 (severe). When the patient was not available for a face-to-face interview (PSE), the case notes were used to score the IGC. At baseline, 471 of the 500 patients had a face-to-face interview and review of clinical notes to verify information and complete any missing information. For the remaining patients only clinical notes were used. At follow-up, 33 patients had a face-to-face interview and review of clinical notes, while the remaining patients had only clinical notes review. Drs Demjaha and Russo, both well qualified and trained clinicians, conducted all IGC scoring. Consensus meetings were held by Drs Demjaha and Russo to discuss the cases. Therefore, no formal reliability statistics were computed.
DSM-IV diagnoses (table 1) were determined by means of previously described and validated methods26,27 using systematically collected information from case notes and discharge summaries. For the majority of participants, diagnosis was further discussed in consensus meetings between one of the principal investigators and other senior clinicians of the research team.
Analytic Approach
Preparatory Analysis.
A preparatory Principal Compo nent Analysis (PCA) with Promax rotation was conducted to determine the adequacy of the sample for the analysis. PCA is a factorial technique (we hereon use the term factor analysis and factor to refer to PCA and components) that maximizes the amount of variance associated with the factors.28 As the factors (the word ‘factor’ is used as the statistical equivalent of ‘symptom dimension’) are intrinsically intended to be correlated among them, Promax rotation was used because it allows factors to be correlated.28 Low frequency of an item (occurring in less than 15% of the sample) was considered a criteria of exclusion as it is likely to reflect a not truly representativeness of that specific symptom in first episode of psychosis. The R-Matrix was used for items retention,29 where a symptom-to-factor loading cut off point of ± 0.4 was used to interpret the factors and to remove items that were not correlated to any other item.28 This led to the exclusion of 3 items (altered perception, nonspecific psychotic experience, and miscellaneous delusions). The item removal procedure was judged appropriate as analysis on the selected 22 IGC items indicated that the Kaiser-Meyer-Olkin sample adequacy value of 0.8 exceeded the recommended value of 0.6 and Bartlett’s test of sphericity was statistically significant [χ2 (231) = 3752.89, P < .001]).28 Finally, 500 cases is an adequate sample size for the current analysis.29
Hierarchical Structure of Symptom Dimensions.
As we aimed to test the hypothesis that symptom dimensions are organized into a hierarchical structure, ie, comprising more than 1-level organization, first- and high-order factor analyses were implemented. High-order factor analysis examines correlations between factors and identifies the hierarchical structure of factors.
First-Order Factor Analysis
A PCA with Promax rotation was conducted on the 22 IGC items. Parallel scree plot was used as criterion for factor retention. Cronbach’s alpha was used to assess the reliability (internal consistency) of each factor.
High-Order Factor Analysis
A PCA with Promax rota tion was conducted using the factors obtained from the first-order factor analysis. This was then followed by a factor analysis with the Schmid-Leiman Solution (SLS).30 The SLS overcomes the limitation of high-order factor analysis that a gradual decrease of variance occurs with the computation of high-order analyses.30 The SLS transforms the factor loadings matrices obtained from a high-order factor analysis into independent loadings that show (a) the direct relationship between the original groups of symptoms (the 22 IGC items) and first-order and higher order factors and (b) the proportion of variance associated with both the first- and high-order factors.30
Concordance Between Symptom Dimensions and Categorical Diagnoses.
Discriminant function analysis was used to examine the usefulness of symptom dimensions in classifying patients into categorical diagnoses. The analysis was carried out using the 6 factors obtained from the first-order factor analysis to allocate patients into 4 diagnostic categories: schizophrenia spectrum disorder (including schizophrenia and schizophreniform disorder; n = 251), schizoaffective disorder (n = 49), mania with psychotic features (n = 67), and psychotic depression (n = 50). Patients with other psychotic disorders (n = 83; eg, delusional disorder, psychotic disorder not otherwise specified) were excluded because these diagnostic groups lacked power for a reliable analysis.
Stability of Structure of Symptom Dimensions.
Confir matory Factor Analysis
A confirmatory factor analysis (CFA) was used to examine goodness of fit of both first- and high-order factor solutions (emerged from the PCA) of psychotic symptoms at follow-up. The analysis was done using the Analysis of Moment Structure program (version 18). There were no missing data in the sample. Monte Carlo simulations of structural equation modeling suggested that for the this study, a sample size of 100 is satisfactory.31 First, the 6-factor solution was tested, each item (ie, symptom) was set to load on only 1 factor (ie, symptom dimension), and then the whole model of first- and high-order factors was tested. A good-fitting model is reflected by the chi square test (it has to be not significant) and by absolute and comparative fit indices. Absolute fit indices such as the chi square test and the Root Mean Square Error of Approximation (RMSEA) provide the most fundamental indication of how well the proposed model fit the data.32 The chi square test, however, has an asymptotic distribution (ie, it is sensitive to large sample size) and so it has been criticized as a measure of goodness of fit in CFA. To address this limitation, the “relative chi square,” the ratio between the chi square and the degree of freedom, is also reported. The recommended value for the chi square/df is around 1 and less than 2.32 For the RMSEA a cut off value of < 0.06 was set for acceptance.32 Comparative fit indices include the Comparative Fit Index (CFI) and the Tucker-Lewis Index (TLI), and their cut off value for acceptance was ≥ 0.95.32
Results
Hierarchical Structure of Symptom Dimensions
First-Order Factor Structure.
Based on the parallel scree plot (see online supplementary materials figure 1), 6 factors were identified (see table 2). The factors were manic symptoms, negative symptoms, disorganized symptoms, depressive symptoms, hallucinations, and delusions. Generally, the factors showed acceptable internal consistency given Cronbach’s α values (table 2). Only the delusions factor had low reliability (Cronbach’s α = .60) due to the low number (2) of items (ie, delusion of persecution and delusion of references) loading on it.
Table 2.
Factor Solution, Factor Loadings Obtained From the First and Higher-Order Factor Analysis
| First-Order Factor Analysis | ||||||
|---|---|---|---|---|---|---|
| Variables | Factors | |||||
| I Manic | II Negative | III Disorganization | IV Depressive | V Hallucinations | VI Delusions | |
| Heightened subjective functioning | 0.892 | 0.012 | –0.113 | –0.077 | –0.114 | –0.060 |
| Expansive mood | 0.844 | –0.056 | 0.048 | 0.070 | –0.017 | –0.014 |
| Rapid subjective tempo | 0.837 | –0.096 | 0.005 | 0.123 | 0.035 | –0.073 |
| Expansive delusions and hallucinations | 0.728 | 0.002 | –0.062 | –0.102 | 0.141 | 0.019 |
| Overactivity | 0.655 | –0.025 | 0.269 | 0.011 | 0.018 | 0.075 |
| Motor retardation | –0.001 | 0.777 | –0.271 | 0.176 | –0.078 | 0.031 |
| Nonverbal communication | 0.086 | 0.760 | 0.054 | 0.098 | –0.037 | –0.004 |
| Poverty of speech | –0.106 | 0.734 | 0.156 | –0.052 | 0.081 | –0.120 |
| Flat and incongruous affect | –0.110 | 0.686 | 0.075 | –0.050 | 0.139 | –0.081 |
| Incoherent speech | –0.107 | –0.132 | 0.902 | 0.071 | –0.036 | –0.084 |
| Other speech abnormality | 0.081 | 0.058 | 0.679 | 0.084 | 0.036 | –0.077 |
| Socially embarrassing behaviour | 0.215 | 0.215 | 0.472 | –0.184 | –0.055 | 0.080 |
| Self neglect | –0.093 | 0.392 | 0.432 | –0.037 | –0.055 | 0.132 |
| Emotional turmoil | 0.167 | 0.243 | 0.406 | –0.063 | –0.052 | 0.109 |
| Depressed mood | –0.112 | –0.034 | 0.106 | 0.887 | –0.054 | –0.044 |
| Special features of depressed mood | 0.054 | 0.059 | 0.035 | 0.885 | 0.032 | 0.008 |
| Depressive delusions and hallucinations | 0.080 | 0.105 | –0.063 | 0.667 | 0.002 | 0.089 |
| Nonaffective auditory hallucinations | 0.035 | 0.043 | –0.082 | –0.113 | 0.885 | –0.002 |
| Nonspecific auditory hallucinations | 0.026 | 0.168 | –0.162 | 0.048 | 0.821 | 0.022 |
| Experience of disordered form of thoughts | –0.038 | –0.197 | 0.381 | 0.112 | 0.580 | 0.026 |
| Delusions of persecutions | –0.131 | –0.068 | 0.034 | –0.078 | –0.031 | 0.871 |
| Delusions of reference | 0.066 | –0.069 | –0.111 | 0.135 | 0.069 | 0.798 |
| Variance (%) | 19.644 | 14.483 | 9.812 | 7.931 | 5.815 | 5.247 |
| Eigenvalue | 4.322 | 3.186 | 2.159 | 1.745 | 1.279 | 1.154 |
| Reliability (Cronbach’s α) | .87 | .76 | .71 | .78 | .68 | .59 |
| High-Order Factor Analysis | ||||||
| I Affective Psychosis | II Nonaffective Psychosis | — | — | — | — | |
| Disorganization | 0.780 | 0.257 | — | — | — | — |
| Manic | 0.743 | 0.032 | — | — | — | — |
| Depressive | –0.570 | 0.508 | — | — | — | — |
| Hallucinations | –0.061 | 0.679 | — | — | — | — |
| Negative | 0.078 | 0.560 | — | — | — | — |
| Delusions | 0.270 | 0.548 | — | — | — | — |
| Variance (%) | 27.237 | 22.268 | — | — | — | — |
| Eigenvalue | 1.632 | 1.336 | — | — | — | — |
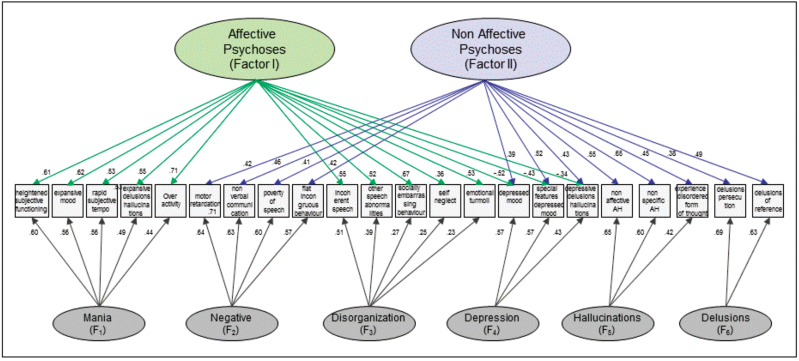
Fig. 1.
Graphical representation of the Schimd-Leiman Solution.
High-Order Factor Structure.
A PCA with Promax rotation was computed on the 6 factors obtained from the first-order factor analysis. Results showed that the initial 6 factors further grouped into 2 high-order general factors (see table 2). The disorganization and mania factors had high loadings on the first higher-order factor that seemed to be prototypical of affective psychosis. Hallucinations, negative, and delusions factors showed loadings on a second higher-order factor that can be characterized as prototypical of non affective psychosis. Depression, however with opposite signs, showed high and similar loading on both higher-order factors.
The first and high-order factors cumulatively accounted for 62.9% of the variance. The SLS was applied to investigate the independent contribution of each first-order factor (mania, negative, disorganization, depression, hallucinations, and delusions), and the 2 high-order factors (affective and nonaffective psychosis) on the 22 original IGC items (symptom groups). The SLS is graphically represented in figure 1 (variance associated with each factor is reported in online supplementary material table 1). Results suggested that the explained variance in psychotic symptoms is almost equally split between the high-order factors and the first-order ones: 50.6% and 49.4%, respectively, supporting the importance of the high-order factors. This result shows that, because the first and high-order factors cumulatively accounted for 62.9% of the variance, the individual contributions were of 31.07% from the first-order factors and of additional 31.83% from the high-order factors.
The negative loadings of the 3 depressive items listed in the affective psychosis factor indicate that the items (symptoms) within this factor behave in the opposite direction to those listed in the same factor. This means that if the 5 manic items (upper part of online supplementary material table 1) increase, the 3 depressive items decrease. Ultimately, the negative/positive loading indicates the relationship that the items have within the same factor they are listed in and not across other factors.
Concordance Between Symptom Dimensions and Categorical Diagnoses.
The discriminant function analysis accounted for 72.2% of total variance [Wilks’s Lambda = .418, χ2 (18) = 358.160, P < .001]. Overall, the 6 first-order factors correctly classified 62.2% of the original cases into categorical diagnoses (table 3). Diagnostic classification accuracy emerged as follow: 62.9% for the schizophrenia spectrum group, 82.1% for the mania with psychotic symptoms group, 78% for the psychotic depression group, and only 18.4% for the schizoaffective group (symptom dimension profiles for each categorical diagnosis are presented in online supplementary material figure 2). When the discriminant function analysis was carried out excluding the schizoaffective group (n = 49), the overall correctness of the model increased to 73.1% (bottom part of table 3).
Table 3.
Concordance (n and %) Between Diagnostic Groups and Symptom Dimensions
| Schizophrenia Spectrum | Mania With Psychotic Features | Psychotic Depression | Schizoaffective | |
|---|---|---|---|---|
| Actual Group | Predicted Group Membership (%) | |||
| Schizophrenia spectrum (n = 251) | 158 (62.9) | 18 (7.2) | 46 (18.3) | 29 (11.6) |
| Mania with psychotic features (n = 67) | 3 (4.5) | 55 (82.1) | 4 (6.0) | 5 (7.5) |
| Psychotic depression (n = 50) | 7 (14.0) | 1 (2.0) | 39 (78.0) | 3 (6.0) |
| Schizoaffective (n = 49) | 12 (24.5) | 13 (26.5) | 15 (30.6) | 9 (18.4) |
| Overall concordance rate (n = 417) | 62.2 | |||
| Schizophrenia spectrum (n = 251) | 170 (67.7) | 23 (9.2) | 58 (23.1) | — |
| Mania with psychotic features (n = 67) | 5 (7.5) | 57 (85.1) | 5 (7.5) | — |
| Psychotic depression (n = 50) | 7 (14.0) | 1 (2.0) | 42 (84.0) | — |
| Overall concordance rate (n = 368) | 73.1 | |||
Stability of Structure of Symptom Dimensions.
The factor structure characterized in the cross-sectional sample in the previous set of analyses showed longitudinal stability. The 6 first-order factor model had an excellent fit to the data collected in the longitudinal study after adjustment for covariance between errors (χ2 = 197.8, df = 183; P = .215, χ2/df ratio = 1.08, TLI = 0.967, CFI = 0.973, and RMSEA = 0.029). The hierarchical model also had excellent fit (χ2 = 219.3, df = 192; P = .086, χ2/df ratio = 1.14, TLI = 0.941, CFI = 0.951, RMSEA = 0.038).
Although the latent structure of the model remained the same, the paired samples t test showed that the absolute severity of symptom changed over time. Manic (t(99) = −4.50, P < .001; 13.6% higher) and disorganization (t(99) = −2.95, P = .004; 6.8% higher) symptoms were more severe at follow-up, while depressive symptoms (t(99) = 3.52, P= . 001; 10.5% lower) and delusions (t(99) = 3.19, P = .002; 11.2% lower) were less severe at follow-up. Changes in the severity of hallucinations and negative symptoms were not statistically significant (see online supplementary material table 2).
Discussion
This study objectives were to examine the structure at the onset and the longitudinal stability of symptom dimensions in psychotic disorders and to establish the concordance between dimensions and categorical classification methods. Within the long tradition of studies using factor analytic solutions to investigate and evaluate psychopathology,14,18,20 to the best of our knowledge, this is the first study to address these questions in a broad spectrum of patients experiencing their first episode of psychosis and then followed up through the first decade of illness.
These findings add to what is known about symptom dimensions in 3 key ways. First, the findings uniquely and robustly show that symptoms have a hierarchical structure comprising at the apex 2 high-order factors (affective and nonaffective) and underneath 6 first-order factors (mania, negative, disorganization, depression, hallucinations, and delusions). Second, the hierarchical structure is present already at the early stages of the illness, and it maintains stability into chronic illness. Third, the results suggest that symptom dimensions may supplement the traditional diagnostic classification method for psychotic disorders.
The hierarchical model of psychosis consisted of 6 factors at a lower level (manic symptoms, negative symptoms, disorganization, depressive symptoms, hallucinations, and delusions) that further clustered into 2 high-order factors of affective and nonaffective psychosis at the apex (see online supplementary material figure 3). The 6 first-order factors provide direct empirical support to the symptom dimensions that are proposed as part of the dimensional evaluation of psychosis in the forthcoming DSM-5.33 Emergence of manic and depressive symptom dimensions as the affective factors in our model is consistent with previous findings.8,11,20 Negative symptoms and disorganization emerge as 2 separate and robust factors accounting for 14.5% and 10% of variance, respectively (table 2). The separation of the positive symptom dimensions into hallucinations and delusions supports the model suggested by the forthcoming DSM-5.33 Moreover, evidence for selective efficacy of cognitive behavioral therapy models to treat hallucinations and delusions further supports such a distinction.34,35
At the apex, 2 high-order factors concord with the 2 main categories of classification of psychotic disorders, namely affective and nonaffective psychosis. The first high-order affective factor consists not only of mood factors (manic and depressive symptom dimensions) but also of the disorganization symptom dimension. This finding may be controversial because disorganization is typically related to schizophrenia rather than to affective psychosis. However, this result may explain the finding that the affective patients in our sample also presented with psychotic features and such severe cases of affective illness may therefore present with clinical features that are more typically associated with nonaffective psychotic disorders. In another hierarchical factorial model,22 disorganization loaded into the nonaffective psychosis; however, the use of chronic patients (in the above mentioned study) instead of first episode and of a different instrument to measure psychopathology can justify the divergence with the result in our study. The grouping of these 3 symptom dimensions together corroborates evidence that thought disorder is part of the disorganization symptom dimension and it is strongly associated with manic symptoms.36,37 Therefore, it may be that thought disorder is not merely associated to mood, but it may partly represent a severe form of mood disorder itself.38 This interpretation, however, remains controversial because “thought disorder” is a label for very heterogeneous language and speech disorders, some related to schizophrenia and others related to manic states. The second high-order factor of nonaffective psychosis consists of negative and depressive symptoms, hallucinations, and delusions and is more strictly typical of schizophrenia.
To the best of our knowledge, this study is the first to examine the stability of the structure of symptom dimensions in patients with their first episode of psychosis. It may therefore be claimed that the dimensional model obtained in this study is likely to be representative of the structure of psychotic disorders. However, the results demonstrate that, although the hierarchical structure is stable for 5–10 years of follow up, the severity of symptoms changed over time. This supports previous findings that report diagnostic shifts in psychotic patients over the course of illness and demonstrate instability of diagnostic categories and the necessity to reassess patients at different stages of the illness.39
At first contact, the results show that symptom dimensions can predict categorical diagnostic allocation with up to 68%–85% accuracy for 3 main diagnostic categories (schizophrenia spectrum disorder, mania with psychosis, and depression with psychotic features). Prediction from the symptom factors appears to correctly classify <1 patient in 5 with schizoaffective disorder, just over three-fifth patients with schizophrenia, and around four-fifth patients with bipolar disorder and psychotic depression. Classification accuracy was low only for the schizoaffective disorder category so consistent with prior findings showing the low reliability of the schizoaffective disorder as a diagnostic category.40 Notably, the stability over the time of the symptom structure suggests that a dimensional model may be a valid model to assess changes in severity of psychotic psychopathology at different stages of the illness. Both early and chronic patients may be assessed with the same symptom dimensions model.
Strengths of this study include the use of a large, heterogeneous sample of first-episode psychotic patients from a well-defined catchment area that supports the generalizability of the findings. Another strength is the inclusion of a longitudinal assessment of symptoms. However, limitations of the study should also be acknowledged. First, it should be acknowledged that any empirically identified dimension of psychopathology characterized using factor analytic methods will reflect, to a degree, the scales used to assess psychopathology. Second, the delusions symptom dimension had only two items and had low reliability (α = .59). However, the items emerged with high-factor loadings (0.798 and 0.871), and the factor was stable over time supporting the validity of this dimension. Third, the longitudinal study requires interpretations with caution because although 100 is a moderately acceptable sample size in CFA,31 a larger sample, or better the whole sample of 500 patients, might have led to more robust findings by a statistical standpoint (ie, without correlated error terms) and to a more exhaustive comprehension of how psychotic symptoms behave over time. Moreover, as the longitudinal sample represents just the 20% of cases used in the cross-sectional one and the 2 samples are not independent (ie, one is a subset of the other), the model fit derived from the CFA might be an overvalued estimation of the structure of psychotic symptoms over time, making crossvalidation with another sample desirable. Finally, the lack of a research diagnosis at the follow-up is a limitation. As a result it was not possible to rigorously investigate the relationship between changes in symptom dimensions and changes in diagnosis or to explore concordance between symptom dimensions and categorical diagnoses over time. Such study would have further enhanced our understanding of the relationship between the dimensional and categorical approaches. Future studies would therefore explore the concordance between the 2 approaches also at follow-up. Nevertheless, it would be fundamental to test external validity of the symptom dimensions in relationship to neuropsychological, neuroimaging, or other biological correlates.
In conclusion, these findings demonstrate that the symptoms of psychosis assume a multidimensional hierarchical structure comprising 2 higher factors at the apex and 6 lower factors underneath. The structure is consistent and stable over time. The findings support the potential benefit that the inclusion of the dimensional approach to psychotic disorders would add to classification systems such as DSM-5. We demonstrated that the dimensional and the categorical models are not mutually exclusive. While the dimensional model can be thought as a bottom-up approach looking at dissected components of psychotic psychopathology, the categorical model can be thought as a top-down approach that tends to generalize symptoms into syndromes. The use of symptom dimensions, instead of overimposed categories only, may be crucial in understanding the complex chain from observed behavior to phenotypes and to unveiling the etiology of psychotic disorders and facilitating important treatment decision, eg, the adjunctive use of antidepressant or mood stabilizers. The utility of categorical diagnoses may be emphasized to simplify clinical communications. Adopting both dimensional and diagnostic approaches as is currently under consideration for DSM-5 appears likely to prove beneficial.
Supplementary Material
Supplementary material is available at http://schizophre niabulletin.oxfordjournals.org.
Funding
This study was funded by the Medical Research Council (G 0600972); the Biomedical Research Centre for Mental Health at the Institute of Psychiatry; King’s College London; the South London and Maudsley National Health Service Foundation Trust.
Supplementary Material
Acknowledgments
We wish to acknowledge the contributions of the Aetiology and Ethnicity of Schizophrenia and Other Psychoses and Genetics and Psychosis study teams, listed online at http://www.iop.kcl.ac.uk/departments/ ?locator=398&context=997 and http://www.iop.kcl.ac. uk/departments/?locator=912. Conflicts of interest: Dr Levine has received research support and/or consultancy fees and/or travel support from F. Hoffmann-La Roche and Eli Lilly. Professor Murray has received speaker honoraria from Astra-Zeneca, Janssen, Lilly, Bristol-Myers Squibb, and Novartis. Dr Dazzan has received speaker honoraria and travel support from Astra-Zeneca, Janssen, and Sanofi. The other authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. Jablensky A. Subtyping schizophrenia: implications for genetic research. Mol Psychiatry. 2006;11:815–836 [DOI] [PubMed] [Google Scholar]
- 2. Joyce EM, Hutton SB, Mutsatsa SH, Barnes TR. Cognitive heterogeneity in first-episode schizophrenia. Br J Psychiatry. 2005;187:516–522 [DOI] [PubMed] [Google Scholar]
- 3. Stroup TS. Heterogeneity of treatment effects in schizophrenia. Am J Med. 2007;120:S26–S31 [DOI] [PubMed] [Google Scholar]
- 4. Post RM. Comparative pharmacology of bipolar disorder and schizophrenia. Schizophr Res. 1999;39:153–8 [DOI] [PubMed] [Google Scholar]
- 5. Murray RM, Sham P, Van Os J, Zanelli J, Cannon M, McDonald C. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophr Res. 2004;71:405–416 [DOI] [PubMed] [Google Scholar]
- 6. Craddock N, O’Donovan MC, Owen MJ. Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophr Bull. 2006;32:9–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McDonald C, Bullmore E, Sham P, et al. Regional volume deviations of brain structure in schizophrenia and psychotic bipolar disorder: computational morphometry study. Br J Psychiatry. 2005;186:369–377 [DOI] [PubMed] [Google Scholar]
- 8. Allardyce J, McCreadie RG, Morrison G, van Os J. Do symptom dimensions or categorical diagnoses best discriminate between known risk factors for psychosis? Soc Psychiatry Psychiatr Epidemiol. 2007;42:429–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Os J, Tamminga C. Deconstructing psychosis. Schizophr Bull. 2007;33:861–862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Van Os J, Gilvarry C, Bale R, et al. A comparison of the utility of dimensional and categorical representations of psychosis. UK700 Group. Psychol Med. 1999;29:595–606 [DOI] [PubMed] [Google Scholar]
- 11. Demjaha A, Morgan K, Morgan C, et al. Combining dimensional and categorical representation of psychosis: the way forward for DSM-V and ICD-11? Psychol Med. 2009;39:1943–1955 [DOI] [PubMed] [Google Scholar]
- 12. Blashfield RK. The classification of psychopathology: Neo-Kraepelinian and quantitative approaches. Plenum, New York; 1984. [Google Scholar]
- 13. Foulds GA, Bedford A. Hierarchy of classes of personal illness. Psychol Med. 1975;5:181–192 [DOI] [PubMed] [Google Scholar]
- 14. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276 [DOI] [PubMed] [Google Scholar]
- 15. Regier DA. Dimensional approaches to psychiatric classification: refining the research agenda for DSM-V: an introduction. Int J Methods Psychiatr Res. 2007;16 Suppl 1:S1–S5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635–645 [DOI] [PubMed] [Google Scholar]
- 17. Crow TJ. Positive and negative schizophrenic symptoms and the role of dopamine. Br J Psychiatry. 1980;137:383–386 [PubMed] [Google Scholar]
- 18. Liddle PF. The symptoms of chronic schizophrenia. A re-examination of the positive-negative dichotomy. Br J Psychiatry. 1987;151:145–151 [DOI] [PubMed] [Google Scholar]
- 19. Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39 789–794 [DOI] [PubMed] [Google Scholar]
- 20. McGorry PD, Bell RC, Dudgeon PL, Jackson HJ. The dimensional structure of first episode psychosis: an exploratory factor analysis. Psychol Med. 1998;28:935–947 [DOI] [PubMed] [Google Scholar]
- 21. Lindenmayer JP, Bossie CA, Kujawa M, Zhu Y, Canuso CM. Dimensions of psychosis in patients with bipolar mania as measured by the positive and negative syndrome scale. Psychopathology. 2008;41:264–270 [DOI] [PubMed] [Google Scholar]
- 22. Cuesta MJ, Peralta V. Integrating psychopathological dimensions in functional psychoses: a hierarchical approach. Schizophr Res. 2001;52:215–229 [DOI] [PubMed] [Google Scholar]
- 23. Arndt S, Andreasen NC, Flaum M, Miller D, Nopoulos P. A longitudinal study of symptom dimensions in schizophrenia. Prediction and patterns of change. Arch Gen Psychiatry. 1995;52:352–360 [DOI] [PubMed] [Google Scholar]
- 24. Maziade M, Bouchard S, Gingras N, et al. Long-term stability of diagnosis and symptom dimensions in a systematic sample of patients with onset of schizophrenia in childhood and early adolescence. II: Postnegative distinction and childhood predictors of adult outcome. Br J Psychiatry. 1996;169:371–378 [DOI] [PubMed] [Google Scholar]
- 25. Wing JK, Babor T, Brugha T, et al. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–593 [DOI] [PubMed] [Google Scholar]
- 26. Kirkbride JB, Fearon P, Morgan C, et al. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study. Arch Gen Psychiatry. 2006;63:250–258 [DOI] [PubMed] [Google Scholar]
- 27. Mondelli V, Dazzan P, Hepgul N, et al. Abnormal cortisol levels during the day and cortisol awakening response in first-episode psychosis: the role of stress and of antipsychotic treatment. Schizophr Res. 2010;116:234–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gorsuch RL. Factor Analysis. 2nd ed. Hillsdale, NJ: Lea; 1983. [Google Scholar]
- 29. Tabachnick BG, Fidell LS, Osterlind SJ. Using Multivariate Statistics. 4th ed. Boston, MA: Allyn and Bacon; 2001. [Google Scholar]
- 30. Wolff HG, Preising K. Exploring item and higher order factor structure with the Schmid-Leiman solution: syntax codes for SPSS and SAS. Behav Res Methods. 2005;37:48–58 [DOI] [PubMed] [Google Scholar]
- 31. Loehlin JC. Latent variable models: An introduction to factor, path, and structural analysis. Lawrence, KS: Erlbaum Associates Publishers; 1998. [Google Scholar]
- 32. Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J Educ Res. 2006;99:323–338 [Google Scholar]
- 33. American Psychiatric Association DSM-5 Development http://www.dsm5.org/ProposedRevision/Pages/proposed revision.aspx?rid=411# Accessed March 15, 2012
- 34. Addington J, Mancuso E. Cognitive-behavioral therapy for individuals at high risk of developing psychosis. J Clin Psychol. 2009;65:879–890 [DOI] [PubMed] [Google Scholar]
- 35. Velligan DI. Cognitive behavior therapy for psychosis: where have we been and where are we going? Schizophr Bull. 2009;35:857–858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cuesta MJ, Peralta V. Testing the hypothesis that formal thought disorders are severe mood disorders. Schizophr Bull. 2011;37:1136–1146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Guerra A, Fearon P, Sham P, et al. The relationship between predisposing factors, premorbid function and symptom dimensions in psychosis: an integrated approach. Eur Psychiatry. 2002;17:311–320 [DOI] [PubMed] [Google Scholar]
- 38. Raymond Lake C. Disorders of thought are severe mood disorders: the selective attention defect in mania challenges the Kraepelinian dichotomy a review. Schizophr Bull. 2008;34:109–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168:1186–1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lake CR, Hurwitz N. Schizoaffective disorder merges schizophrenia and bipolar disorders as one disease–there is no schizoaffective disorder. Curr Opin Psychiatry. 2007;20:365–379 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.