Abstract
Depression and negative symptoms can be difficult to distinguish in schizophrenia. Assessments for negative symptoms usually account for the longitudinal nature of these symptoms, whereas instruments available to measure depression mainly assess current or recent symptoms. This construct difference may confound comparison of depressive and negative symptoms in schizophrenia because both domains may have trait-like aspects. We developed an instrument to measure both longitudinal “trait” as well as recent “state” symptoms of depression and tested this instrument (Maryland Trait and State Depression [MTSD] scale) in a sample of 98 individuals with schizophrenia or schizoaffective disorder and 115 community participants without psychotic illness. Exploratory factor analysis of the MTSD revealed 2 factors accounting for 73.4% of the variance; these 2 factors corresponded with “trait” and “state” depression inventory items. Neither MTSD-state nor MTSD-trait was correlated with negative symptoms as measured with the Brief Negative Symptom Scale (r = .07 and −.06, respectively) in schizophrenia patients. MTSD state and trait scores were significantly correlated with the Brief Psychiatric Rating Scale depression subscale (r = .58 and .53, respectively) as well as the Profile of Mood States depression subscale (r = .57 and .44). Persons with schizophrenia had significantly greater trait depressive symptoms than controls (P = .031). Individuals with schizoaffective disorder had significantly higher trait depression (P = .001), but not state depression (P = .146), compared with schizophrenia patients. Trait depressive symptoms are prominent in schizophrenia and are distinct from negative symptoms.
Key words: BNSS, schizoaffective disorder, symptom domain
Introduction
Depression and negative symptoms in schizophrenia share some phenomenological features, such as anhedonia, decreased spontaneous movements, social isolation, and decreased motivation. However, depression and negative symptoms are considered etiologically very different.1 Additionally, these symptom domains are considered to be distinct in temporal course; depressive symptoms are generally episodic, while negative symptoms are enduring aspects of a chronic illness. Studies measuring both symptom domains have produced variable results; some studies have found overlap between depressive and negative symptoms2 or higher levels of negative symptoms in schizophrenia patients with depression,3 while other studies have found no correlation between the 2 symptom domains4 or even a negative correlation.5
This variability may be due in part to conceptual issues in assessing depression in comparison to negative symptoms. Clinical depression is measured as an episodic phenomenon, with current or recent symptoms providing sufficient evidence to make a diagnosis. On the other hand, negative symptoms are an enduring aspect of schizophrenia. Most negative symptom rating scales, such as the Positive and Negative Syndrome Scale negative subscale score,6 the Scale for the Assessment of Negative Symptoms,7 the Negative Symptom Assessment Scale (NSA-16),8 and the Schedule for Deficit Syndrome,9 emphasize incorporating long-term observations of certain negative symptoms. The Brief Negative Symptom Scale (BNSS)10 emphasizes current manifestations of negative symptoms but has been found to have very high temporal stability.11 This temporal difference in the conceptualization of depression and negative symptoms complicates efforts to determine if these are separable symptom domains.12
Although trait aspects of depression have not been formally addressed, cross-sectional studies have identified frequent occurrence of depressive symptoms at all stages of schizophrenia, including prodromal, acute, and post-acute periods.13 Longitudinal studies also show that depression is a stable feature of schizophrenia independent of other symptom domains.14,15 These findings support the possibility that depression in schizophrenia may have state-based fluctuations on top of trait-like individual differences; establishing the pattern of depression may be critical for studying new ways of classifying psycho pathology based on dimensions of observable behavior and neurobiological measures.12
Outside of schizophrenia, some attempts have been made to examine trait depression. Spielberger and colleagues created the State-Trait Depression Scales (STDS), which has shown promise in distinguishing between state and trait depression in healthy populations in different cultures.16 The STDS instructs participants to answer items based on current intensity as well as frequency over time. However, this scale excludes many symptoms important in Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for clinical depression. Other studies have employed the depression subscale of the revised NEO Personality Inventory.17 The clinical relevance of this subscale in severe mental illness is unclear.
Most well-established depression instruments were developed for studies of major depression. They depend on rating current or recent depressive symptoms. This may not be a problem in major depression where evaluation of the current episode is the focus. However, relying entirely on these instruments could be an oversight in chronic illnesses such as schizophrenia. The Calgary Depression Scale for Schizophrenia has been demonstrated to be valid and reliable by taking into account the potential overlap in presentation of depressive symptoms with that of negative symptoms or antipsychotic medication side effects,18 but it still captures only state aspects of depression. Some scales, such as the Beck Depression Inventory (BDI), are based on patient self-report, but BDI total score does not fully distinguish depression from negative symptoms.19 There are no instruments for measurement of depression in schizophrenia that are designed to assess longitudinal, trait-like depressive symptoms in parallel with current or recent symptoms.
To address these issues, we developed an instrument designed to measure depressive symptoms weighted symmetrically for both current symptoms (“state” depression) and symptoms throughout life (“trait” depression). This approach is based on a dimensional view of depression, in which the experience of clinical and subclinical levels of depressive symptoms over time reflects an enduring phenotype, which may be related to the disposition to clinically defined depressive illness. Applying this instrument in schizophrenia/schizoaffective patients and community participants, this study aims to (1) establish whether our instrument can discriminate between state and trait aspects of depression and (2) determine whether depression, measured as either a trait or state construct, is related to negative symptoms in schizophrenia.
Methods
Participants
Participants with schizophrenia and schizoaffective disorder were recruited from local community mental health clinics. Community comparison participants were recruited through random digit dialing and media advertisements. All participants were examined for mental illness and diagnosed through use of the Structured Clinical Interview for DSM Disorders.20 In order to achieve a community-based sample with some representation of affective components in both cohorts, we did not exclude schizoaffective disorder patients from the schizophrenia cohort and did not exclude individuals with past or current mood disorder from the community cohort. However, subanalyses were performed splitting the individuals with psychotic disorder into schizophrenia and schizoaffective groups and splitting the community sample into those with and without history of mood disorder. The patient group consisted of 98 individuals, including 81 with schizophrenia and 17 with schizoaffective disorder. Of the 98 patients, 83 were taking antipsychotic medication: 13 were on a typical antipsychotic, 57 were on an atypical, and 13 were taking both a typical and an atypical antipsychotic. The community group consisted of 117 individuals, including 93 individuals without an Axis I diagnosis and 24 people with a past or current mood disorder diagnosis (18 with major depressive disorder, 3 with bipolar disorder type I, 1 with bipolar disorder type II, and 2 with depressive disorder not otherwise specified). Demographic characteristics of participants are given in table 1.
Table 1.
Demographics of Samples for Combined Schizophrenia Group (Schizophrenia and Schizoaffective) and Nonpsychotic Control Group
| Control | Schizophrenia | Test Statistic | P Value | |
|---|---|---|---|---|
| Total N | 117 | 98 | n/a | n/a |
| Age [years] (±SD) | 38.5 (13.5) | 39.8 (13.0) | t = 0.705 | .48 |
| % Male | 43.6 | 67.3 | χ2 = 12.1 | .00 |
| Ethnicity | ||||
| % White | 58 | 47 | χ2 = 2.7 | .10 |
| % Black | 35 | 50 | χ2 = 4.9 | .03 |
| % Other | 7 | 3 | n/a | n/a |
| % Smoker | 28.2 | 33.7 | χ2 = 3.26 | .07 |
| Taking medication | ||||
| % Antidepressant | n/a | 35.7 | n/a | n/a |
| % Antipsychotic | n/a | 82.7 | n/a | n/a |
| % Mood stabilizer | n/a | 15.3 | n/a | n/a |
Note: n/a, not available.
Development of the Maryland Trait and State Depression Scale
The Maryland Trait and State Depression (MTSD) scale (full scale and instructions provided as an Appendix) consists of 36 items rated in 5-point Likert scales, divided into 2 sections: the “state” section was intended to capture current depressive symptoms and the “trait” section was intended to capture the frequency of depressive symptoms throughout adulthood. Written instructions on each page requested the respondent to answer the items regarding their experiences throughout the past 7 days (for the state section), or for their adult life, excluding the past 1 week (for the trait section). Each section consisted of 18 items, which were similar across sections but reworded slightly (eg, “I cry because my mood is low” is a state item, while “I cried often because my mood was low” is the corresponding trait item). Items for the MTSD were developed through study of several depression rating instruments as well as criteria used to make a diagnosis for major depression in the DSM-IV, by rewording the DSM-IV items into self-reporting format. For example, the DSM-IV criterion of “markedly diminished interest or pleasure in activities” was formulated as the state item “I have lost interest in enjoyable activities” and the trait item “I have felt less interested in enjoyable activities than my peers.” The abbreviated content of the 36 questions is listed in table 2.
Table 2.
Oblique Rotated Factor Loadings for 2-Factor Model of Maryland Trait and State Depression Items, From 3 Independent Factor Analyses (Combined Sample [Comb], Schizophrenia Patients [SZ], and Nonpsychotic Controls [Control])
| State | Trait | |||||
|---|---|---|---|---|---|---|
| Item | Comb | SZ | Control | Comb | SZ | Control |
| S_1. It is hard for me to feel happy | 0.68 | 0.61 | 0.74 | |||
| S_2. I have lost interest in enjoyable activities | 0.87 | 0.84 | 0.81 | |||
| S_3. My appetite changes a lot… | 0.79 | 0.79 | 0.69 | |||
| S_4. I sleep much more than usual… | 0.74 | 0.64 | 0.74 | |||
| S_5. I feel sluggish and slow | 0.65 | 0.62 | 0.58 | |||
| S_6. I feel sad | 0.77 | 0.72 | 0.70 | |||
| S_7. I have no energy for anything | 0.84 | 0.81 | 0.78 | |||
| S_8. I cry because my mood is low | 0.64 | 0.54 | 0.73 | |||
| S_9. I cannot get motivated | 0.73 | 0.72 | 0.62 | |||
| S_10. I am burdened with feelings of guilt | 0.39 | 0.62 | 0.45 | |||
| S_11. I don’t sleep enough… | 0.39 | 0.51 | 0.52 | |||
| S_12. The blues stay with me no matter what I do | 0.71 | 0.70 | 0.63 | |||
| S_13. I spend less time doing activities… | 0.87 | 0.83 | 0.80 | |||
| S_14. I feel that I want to die | 0.54 | 0.43 | 0.87 | |||
| S_15. I have a heavy feeling in my arms or legs… | 0.38 | |||||
| S_16. …weight goes up or down a lot… | 0.58 | 0.39 | 0.88 | |||
| S_17. …felt that I deserved to be punished | 0.45 | 0.73 | 0.41 | |||
| S_18. I have no hope for my future | 0.43 | 0.70 | ||||
| T_1. It has been hard for me to feel happy… | 0.81 | 0.78 | 0.79 | |||
| T_2. …less interested in enjoyable activities | 0.75 | 0.65 | 0.90 | |||
| T_3. I often lose my appetite… | 0.49 | 0.54 | 0.54 | |||
| T_4. I sleep more than most people… | 0.65 | 0.64 | 0.67 | |||
| T_5. I feel sluggish and slow… | 0.79 | 0.73 | 0.85 | |||
| T_6. I often feel sad… | 0.80 | 0.75 | 0.78 | |||
| T_7. I have not had sufficient energy… | 0.81 | 0.76 | 0.80 | |||
| T_8. I cried often because my mood was low | 0.51 | 0.55 | 0.44 | |||
| T_9. …been hard for me to get motivated | 0.78 | 0.78 | 0.76 | |||
| T_10. …burdened with feelings of guilt… | 0.85 | 0.83 | 0.73 | |||
| T_11. I don’t sleep enough… | 0.59 | 0.57 | 0.75 | |||
| T_12. The blues have stayed with me… | 0.72 | 0.65 | 0.80 | |||
| T_13. …not spent much time doing activities… | 0.68 | 0.63 | 0.74 | |||
| T_14. I have felt that I wanted to die | 0.40 | 0.71 | 0.80 | |||
| T_15. …have a heavy feeling in my arms or legs… | 0.59 | 0.58 | 0.66 | |||
| T_16. My weight has gone up or down a lot… | 0.43 | 0.59 | 0.71 | |||
| T_17. …I often felt that I deserved to be punished | 0.84 | 0.88 | 0.61 | |||
| T_18. I feel hopeless about my future | 0.77 | 0.79 | 0.59 | |||
Note: Blanks represent loading coefficients <0.35.
Symptom severity can be assessed by frequency, intensity, or both. Intensity is more subjective compared with frequency using the self-assessment format; therefore, we chose to ask subjects to rate symptoms based only on frequency of occurrence within the specified temporal window. The responses specified frequency of the individual’s experience of the symptom along a Likert scale ranging from 0 to 4. The anchors were defined for the state scale as “not at all,” “<1 day,” “1–2 days,” “3–4 days,” and “5–7 days” (over the past 7 days) and for the trait scale as “never,” “less than once a year,” “less than once a month on average,” “experienced almost every month,” and “experienced many times in a month for almost every month of my adult life” (over the course of adult life except for past 7 days).
The scale was administered in a “self-rating under clinical interview environment” format. An interviewer sat with the subject as in a rater-administered interview and provided instructions reiterating the time course of interest for each part of the instrument. The interviewer remained in the room as the participant completed the scale but did not directly inspect what the participant was rating. Raters were permitted to answer questions from the participant to clarify items but not to assist in the actual rating. The protocol was designed to maximize consistency in understanding of the instructions and attentiveness to each question.
Negative Symptom Measure
Negative symptoms were assessed by using the BNSS, a 13-item clinician-rated scale validated for the assessment of negative symptoms in schizophrenia patients in the following areas: blunted affect, alogia, asociality, anhedonia, and avolition.10,21 The primary measure of negative symptoms is the total score. BNSS scores can also be calculated for the 2 factors inherent in the structure of the BNSS, corresponding to Motivation and Pleasure (BNSS-MP) and Emotional Expressivity (BNSS-EE).21 All raters were formally trained by the original contributor of the instrument (Dr Strauss) through use of multiple videotaped case interviews until raters achieved acceptable reliability (ICC ≥ 0.90).
Clinical Validating Measures
We chose 2 commonly used, validated depression scales for cross-validation purpose. We used the 20-item Brief Psychiatric Rating Scale (BPRS), a clinician-rated scale evaluating overall psychiatric symptom load, and its depression subscale as a validating measure for the MTSD. Raters were trained until they achieved a rater reliability of r ≥ .9 in 5 or more consecutive, gold standard rating established, videotaped sessions. All participants also completed the Profile of Mood States (POMS) 65-item version22; the POMS depression subscale provides a self-rated validation measure.
Test–Retest Reliability
A subsample of 41 participants repeated the MTSD for assessment of its test–retest reliability.
To increase variance, both schizophrenia (n = 21) and control (n = 20) participants were retested after a variable interval, range 33–220 days (median = 127, SD = 53).
Statistical Analyses
Factor analyses were conducted using Stata 1223 on the total sample and then independently in the schizophrenia and control groups in order to detect possible differences in the clustering of depressive symptoms due to diagnosis. First, a principal components factor analysis was performed. Eigenvalues, a scree plot, and the percentage variance explained by each factor were examined and utilized when deciding the number of factors to retain. Then, a principal axis factor analysis with oblique rotation was performed because we conceptualized some correlation between lifetime depressive symptomology and current depression. Discriminant validity of the 2 factors was examined through computation of average variance extracted (AVE).24 Correlations were performed using Pearson’s correlation. For group comparisons, we used ANOVA with post hoc testing done with Bonferroni correction for multiple comparisons. Test–retest reliability was based on intraclass correlation analysis using Cronbach’s alpha. All tests were 2-tailed.
Results
Factor Analysis of MTSD
The schizophrenia sample was matched in age with the controls (t = 0.71, P = .481). There were more males (χ2(df = 1) = 12.1, P < .001) and more smokers (χ2(df = 1) = 3.26, P = .071) in the schizophrenia group than in the control group (table 1).
An exploratory factor analysis (EFA) was run with an oblique rotation based on the combined sample of 215 participants. The principal axis factoring yielded 2 factors that together accounted for 73.4% of the variance in the data. All 18 “state” items loaded onto Factor 1, and all “trait” items loaded onto Factor 2. See table 2 for the loading rotated coefficients for each item.
To assess whether depressive symptoms might cluster differently between persons with schizophrenia and controls, we repeated the EFA in each group. In the controls, the principal factor analysis revealed 2 factors that combined to explain 66.1% of the variance, with 4 additional factors with eigenvalues >1.0. Similarly, the principal factor analysis in the schizophrenia sample revealed 2 factors that combined to explain 64.2% of the variance, with 3 additional factors with eigenvalues >1.0. Thus, 2 obliquely rotated solutions were examined in each sample: a 2-factor model for each sample, a 6-factor model for the control sample, and a 5-factor model for the schizophrenia sample.
As summarized in table 2, the 2-factor solutions from each sample were very similar and reflected the difference in state and trait items. The 6-factor solution for controls contained factors that closely corresponded with the trait and state factors of the 2-factor model, with the additional 4 factors having little thematic coherence. The 5-factor solution for schizophrenia patients contained 1 factor that closely corresponded with the state factor, but the remaining factors had little thematic coherence. There was very little overlap between the 6-factor solution from the control sample and the 5-factor solution from the schizophrenia sample. The overall findings from these models support a 2-scale solution for depressive symptoms of the MTSD, one representing state depression (MTSD-S) and the other representing trait depression (MTSD-T). These 2 factors were significantly correlated with each other (r = .648, P < .001 for schizophrenia group and r = .692, P < .001 for control group.)
The discriminant validity of the state and trait scales was further assessed by calculating AVE.24 The AVE was 0.516, which is higher than the shared variance of the summed trait and state factors (0.481). This provides additional support for the ability of the MTSD to discriminate between current vs lifetime load of similar sets of depressive symptoms.
Validity of MTSD in Comparison to Established Measures of Depression
We compared MTSD-S and MTSD-T with the BPRS and POMS depression subscales, which represent clinician-rated and self-reported measures of current mood, respectively. Correlations of the MTSD-S with BPRS depression subscale (r = .568, P < .001) and with POMS depression subscale (r = .530, P < .001) were both significant. The correlations of the MTSD-T with the BPRS and POMS subscales were .563 and .484, respectively (both P < .001). In comparison, the correlation between the BPRS depression subscale and the POMS depression subscale was .490 (P < .001), suggesting similar validity in measuring depressive symptoms between MTSD and these validated self-rated or clinician-rated scales.
Test–Retest Reliability of MTSD
In the subsample that repeated the MTSD, intraclass correlation coefficients (ICC) were .78 for trait depression and .82 for state depression, indicating good reliability.25 The average interval between testing was 122 days. There was no significant relationship between length of time between test and retest and absolute difference in scores for either MTSD-S (r = .07, P = .68) or MTSD-T (r = .19, P = .26).
MTSD in Schizoaffective Disorder
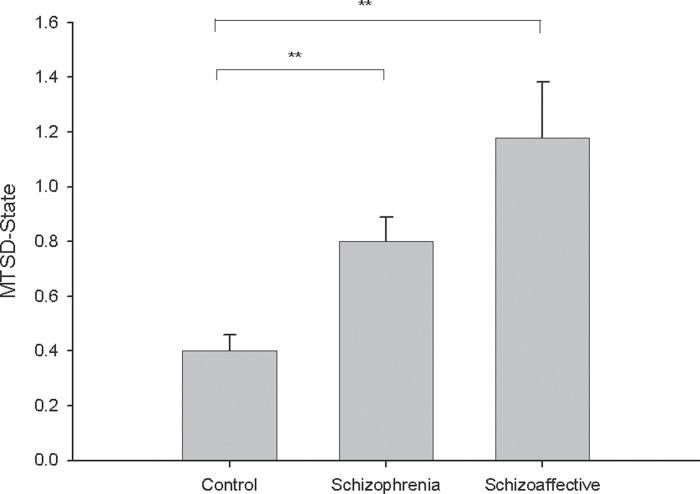
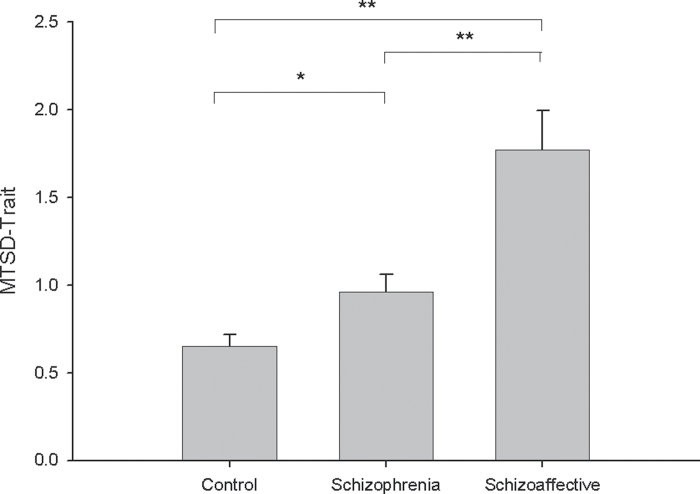
If the MTSD is valid, one should expect a higher score in persons with schizoaffective disorder, especially trait score, because mood symptoms in schizoaffective disorder are often chronic. Schizophrenia, schizoaffective disorder, and nonpsychotic control groups differed on both state (F(2,212) = 13.1, P < .001) and trait (F(2,212) = 14.8, P < .001) depressive symptoms. The schizoaffective group had the highest scores on both measures, with the schizophrenia group intermediate. For state depressive symptoms, the difference between the schizoaffective and schizophrenia groups was not significant (P = .146), while the difference between schizophrenia and control was significant (P = .000) (see figure 1). For trait depressive symptoms, the difference between schizoaffective and schizophrenia groups was significant (P = .001) as was the difference between the schizophrenia and control groups (P = .031) (see figure 2). There was not a significant difference between proportions of persons taking antidepressants in schizophrenia (34.6%) and schizoaffective (41.2%) groups (χ2 = 0.27, P = .605), suggesting that different rates of antidepressant treatment did not account for the similarity in state depressive symptoms between these groups.
Fig. 1.
Average score on Maryland Trait and State Depression—state scale by diagnosis. Bars represent SE. **P < .01.
Fig. 2.
Average score on Maryland Trait and State Depression—trait scale by diagnosis. Bars represent SE. *P < .05 and **P < .01.
In parallel, we separated the community controls into those with and without a history of mood disorder. Individuals with a current or past diagnosis of mood disorder had significantly higher MTSD-S scores (M = 0.92, SD = 1.05) than those without a history of mood disorder (M = 0.26, SD = 0.41; t(115) = 4.80, P < .001). Individuals with a current or past diagnosis of mood disorder had significantly higher MTSD-T scores (M = 1.49, SD = .96) than those without such a diagnosis (M = 0.43, SD = 0.46; t(115) = 7.76, P < .001).
Distinction of Depression and Negative Symptoms
Next, to assess whether trait depression is related to negative symptoms, we compared MTSD-T with BNSS total score and found essentially no correlation (r = −.06, P = .574) in the combined schizophrenia sample (both schizophrenia and schizoaffective disorder). MTSD-S was also not correlated with BNSS total mean in the combined patient sample (r = .07, P = .479). There were no significant correlations between MTSD-S and MTSD-T and the subfactors of the BNSS (table 3).
Table 3.
Correlations of Maryland Trait and State Depression (MTSD)—State and Trait Scores With Other Clinical Measures in Schizophrenia and Nonpsychotic Control Groups, Including Brief Psychiatric Rating Scale (BPRS) Total Score and Depression Subscale, Brief Negative Symptoms Scale (BNSS) Total Score and Subscales for Emotional Expressivity (BNSS-EE) and Motivation and Pleasure (BNSS-MP), Chlorpromazine Equivalent Dose of Antipsychotic Medication (CPZ), and Profile Of Mood States (POMS) Depression Subscale
| MTSD- Trait | BPRS Total | BNSS Total | BNSS-MP | BNSS-EE | BPRS Depression | POMS Depression | CPZ | |
|---|---|---|---|---|---|---|---|---|
| Schizophrenia | ||||||||
| MTSD-state | .65** | .22* | .07 | .12 | −.01 | .30** | .37** | −.03 |
| MTSD-trait | — | .22* | −.06 | .01 | −.13 | .41** | .41** | −.06 |
| Control | ||||||||
| MTSD-state | .69** | .65** | .50** | .57** | .21* | .71** | .46 | — |
| MTSD-trait | — | .53** | .36** | .38** | .20* | .60** | .45 | — |
Note: *P < .05 and **P < .01.
In the patient sample, both MTSD-S and MTSD-T were weakly correlated with BPRS total score (r = .22 and .22, P = .029 and .028, respectively) although this was not significant after Bonferroni correction for 2 comparisons (both P > .025). Neither were correlated with chlorpromazine equivalent dosage of antipsychotic medication (r = −.03, P = .792 for MTSD-S and r = −.06, P = .626 for MTSD-T).
Finally, BNSS was also rated in the control sample so that MTSD-S and MTSD-T could be compared with BNSS in a nonschizophrenia sample. Both MTSD-S and MTSD-T were highly correlated with BNSS (r = .50 and .36, respectively, both P < .001), an entirely different pattern compared with that of the schizophrenia patients. These results are summarized in table 3.
Discussion
We developed an instrument intended to separately quantify the longitudinal subjective experience of depression in persons with schizophrenia from current or recent depressive symptoms, so that trait depression could be compared with negative symptoms. We found clear evidence that state and trait aspects of depression can be instrumentally separated in patients with schizophrenia and that negative symptoms are distinct from depression symptoms experienced by patients either longitudinally or currently.
One challenge in developing a scale of this nature is the likely tendency for an individual’s current mood state to bias their evaluation of their lifetime experience of depression, blurring the boundary between state and trait aspects of depression. We took 2 approaches to minimize this potential bias. One was administering the scale in a clinical interview format to ensure understanding of and compliance with the instructions. Secondly, we formulated the questions to emphasize the distinction between current vs longitudinal experience (see table 2). Our approach was largely successful, as indicated by the consistent 2-factor solution in both schizophrenia patients and community controls.
Previous studies on the relationship between negative symptoms and depression in schizophrenia have varied in approaches to the problem and in their results. Several studies took a categorical approach by dividing patients into a depressed group and nondepressed group and compared negative symptoms between these groups; 2 studies found higher levels of negative symptoms in depressed patients with schizophrenia,3,13 and 1 study found no difference,26 though all concluded that negative symptoms could be distinguished from depression. Other studies have examined the correlation of depressive symptoms with negative symptoms, mostly finding no significant relationship4,5,19; however, the depression scales used in these studies only measured current depression. By using a dimensional approach and distinguishing between state and trait depression, our findings provide additional evidence that negative symptoms are distinct from depression experienced by patients with schizophrenia.
Interestingly, both state and trait depressive symptoms were highly correlated with “negative symptoms” rated in the nonpsychotic participants in this study. This likely reflects the superficial similarity between these 2 symptom domains and indicates that attempts to measure negative symptoms in a nonpsychotic sample will likely be confounded by depression. However, in the schizophrenia sample, these factors were not correlated, suggesting that depression and negative symptoms are distinct clinical phenomena in individuals suffering from schizophrenia.
The MTSD-T score was able to quantitatively capture the difference in the longitudinal course of depressive symptoms between patients diagnosed with schizophrenia and those diagnosed with schizoaffective disorder. Measurement of trait depression may be a sensitive approach to distinguish between schizophrenia and schizoaffective disorder because state depression scores were less robust in differentiating between these diagnostic groups.
The clinical presentation of schizophrenia is highly heterogeneous in symptoms and course, prompting the shift toward a dimensional approach in research.27 A critical task for elaborating a dimensional framework is to identify how symptom domains are related to each other phenomenologically, etiologically, and dynamically. Depression is a symptom domain of high importance in psychotic illnesses, leading to the use of diagnostic entities such as schizoaffective disorder to classify the many patients whose symptom profiles overlap the conventional affective/nonaffective dichotomy.28 This ambiguity creates the potential hazard of overlooking symptoms of depression in patients who are not labeled “schizoaffective.” It is important to assess depressive symptoms in patients with psychotic illness because they may require different treatment approaches.
There are several important limitations to this study. Our ability to demonstrate the construct validity of the MTSD-T measure was limited by the absence of other means of measuring trait depression in schizophrenia. Because the MTSD depends on retrospective assessment by participants, the measure may be influenced by current depressive symptoms—ie, currently depressed individuals may be more likely to perceive themselves as having been depressed throughout their life. Although this would contribute to the high correlation between state and trait ratings of depression observed in this study, this correlation also likely reflects a true intrinsic relationship of these measures, in that individuals with high levels of trait depression are more likely to be experiencing state depressive symptoms. More thorough testing of the construct validity of the MTSD would require prospective, longitudinal assessment. Ideally, such a study would include a sample of individuals with major depression and/or dysthymia.
The primary measure of negative symptoms in this study was the BNSS. The instructions for this scale specify interviewers to focus on experiences occurring over the previous week,10 although the scores on the BNSS showed high (r = .93) temporal stability over an average period of 7 months, suggesting that the BNSS likely measures both the state and much of the stable, longer term aspects of negative symptoms.11 However, our analysis is limited in interpreting the relationship of depressive symptoms to “state” vs “trait” differences of negative symptoms in schizophrenia patients, if any.
It is unclear if trait depression, as defined and measured in this study, is related to the personality trait of neuroticism or to “depressive personality disorder” as described in older diagnostic nomenclature. Higher levels of neuroticism, as measured in adolescence, are associated with greater likelihood of diagnosis in adulthood with both nonpsychotic depression and schizophrenia, suggesting shared liability to these disorders.29 People with schizophrenia are characterized by stably elevated negative affectivity and low positive affectivity, but prior studies of the relationship between these personality traits and clinical symptoms in schizophrenia have been inconsistent.30 The MTSD may be useful in clarifying this line of research.
Our results demonstrate the feasibility of measuring and differentiating both state and trait aspects of depression in patients with schizophrenia and in the general community population. We showed that negative symptoms and trait depression are distinct domains of psychopathology. Trait depression may be an important and thus far largely neglected feature of schizophrenia. Further studies are needed to define the relationships of trait depression with schizophrenia pathophysiology and other important clinical outcomes such as cognitive function, quality of life, and suicidal behavior.
Funding
National Institutes of Health (T32MH067533, R01MH085646, R01DA027680, and R21DA033817).
Acknowledgments
We thank our participants and the support staff of the Neuroimaging Research Program. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Appendix Maryland Trait and State Depression (MTSD) Scale: User Instructions and Questionnaires*
This scale is registered for copyright (pending). Under this copyright, the scale is free for not-for-profit academic, research, or patient care use. No additional inquiry is required. Disclaimer: It is the user’s full responsibility to understand the implications of using this instrument before administering to a respondent. Individuals who are not trained to evaluate and manage respondent’s reporting any of these symptoms should not attempt to use this instrument. User should bear all responsibility associated with the use of this instrument. *For-profit use of this scale, please contact Dr Hong, Maryland Psychiatric Research Center, University of Maryland School of Medicine, PO Box 21247, Baltimore, MD 21228. ehong@mprc.umaryland.edu
Instructions for Interviewers
The MTSD consists of 36 items rated in 5-point Likert scales, divided into 2 sections: the “state” section is intended to capture current depressive symptoms experienced in the past 7 days and the “trait” section is intended to capture the frequency of depressive symptoms throughout adulthood, except the past 7 days.
MTSD was developed after reviewing several depression rating instruments and finding that most existing scales were developed before the recent versions of Diagnostic and Statistical Manual of Mental Disorders (DSM). Therefore, items in the MTSD are based on criteria currently used to make a diagnosis for major depressive disorder in the DSM-V, by rewording the DSM-V items into a self-reporting format.
For example, the DSM-V criterion of “markedly diminished interest or pleasure in activities” is formulated as the following 2 “state” items:
“I have lost interest in enjoyable activities” in the past 7 days, and
“I spend less time doing activities or hobbies than I used to because my mood is low” in the past 7 days.
The same DSM-V criterion is formulated as the following 2 “trait” items:
“I have felt less interested in enjoyable activities than my peers” in the course of one’s adult life excluding the past 7 days, and
“I have not spent much time doing activities or hobbies because I feel down” in the course of one’s adult life excluding the past 7 days.
Similar reformulations of the DSM-V criteria are used for the rest of the items in MTSD.
Although the instruction is specified for “adulthood,” we have used the instrument with persons aged 12 and up. In those cases, we redefine “adulthood” as “in your whole life since age 12.”
Symptom severity can be assessed by frequency, intensity, or both. Self-rating for intensity is more subjective compared with frequency when using a self-report format, which can be a major source of noise and unreliability during group-based analyses. Therefore, MTSD is designed to ask respondents to report symptom severity based only on frequency of occurrence within the respective state or trait temporal window in this self-rating instrument. Subjective rating for intensity of the symptoms is not asked.
The responses specify frequency of the individual’s experience of the symptom along a Likert scale ranging from 0 to 4. The anchors are defined for the state and trait scales as the following.
State (in the past 7 days):
0 = “not at all”
1 = “<1 day”
2 = “1–2 days”
3 = “3–4 days”
4 = “5–7 days”
Trait (in one’s adult life except the past 7 days):
0 = “never”
1 = “experienced briefly, but less than once a year”
2 = “experienced more than once a year, but less than once a month on average”
3 = “experienced intensely for some weeks in my lifetime and in other times less frequent but still there, or experienced almost every month”
4 = “experienced many times in a month for almost every month of my adult life”
The anchors for “trait” measures are nontrivial because the anchors are trying to capture large variations in depression experience over the lifetime of many individuals using merely 5 levels. To achieve good reliability on the trait items, it is important to carefully explain the instructions to make sure the respondent understands and remember the time period and anchors.
Each section consists of 18 items. These 2 sections should be printed on 2 separate pages and presented to the respondent one at a time. Give specific instructions on the temporal window each section is intended for and explain the anchors for that section only. When a section is completed, have the respondent hand back that section, inspect it for completeness, and then give the respondent the next section along with instruction for the same.
The scale should be administered in a “self-rating under clinical interview environment” format. Treat this as a formal clinical interview. An interviewer should sit with the respondent as if this is a rater-administered interview and provide instructions reiterating the time course of interest for each part of the instrument. The interviewer should remain in the room as the respondent completes the scale but do not directly inspect what the respondent is rating so that symptom rating remains strictly self-report. Raters can explain voluntary questions from the respondent to assist them in understanding the questions but should not instruct on how to choose the actual rating. These procedures are to maximize consistency in the understanding of the questions and anchors, minimize variability in the style and judgment from interviewers, and ensure the respondent’s attentiveness to each question.
(Do not present the face page and the instruction pages to the respondent)
Maryland Trait and State Depression—State (MTSD-S) Scale
Instruction: This scale asks your general experience of depression. Please read each question carefully and then circle the number to indicate how you felt in the recent week, ie, in the past 7 days. There are no right or wrong answers. Do not spend too much time on any one statement but give the rating that most closely describes your recent feelings.
| Not at all | <1 day | 1–2 days | 3–4 days | 5–7 days | |
| 1. It is hard for me to feel happy. | 0 | 1 | 2 | 3 | 4 |
| 2. I have lost interest in enjoyable activities. | 0 | 1 | 2 | 3 | 4 |
| 3. My appetite changes a lot depending on my mood. | 0 | 1 | 2 | 3 | 4 |
| 4. I sleep much more than usual because of my mood. | 0 | 1 | 2 | 3 | 4 |
| 5. I feel sluggish and slow. | 0 | 1 | 2 | 3 | 4 |
| 6. I feel sad. | 0 | 1 | 2 | 3 | 4 |
| 7. I have no energy for anything. | 0 | 1 | 2 | 3 | 4 |
| 8. I cry because my mood is low. | 0 | 1 | 2 | 3 | 4 |
| 9. I cannot get motivated. | 0 | 1 | 2 | 3 | 4 |
| 10. I am burdened with feelings of guilt. | 0 | 1 | 2 | 3 | 4 |
| 11. I don’t sleep enough when my mood is low because I think of negative thoughts. | 0 | 1 | 2 | 3 | 4 |
| 12. The blues stay with me no matter what I do. | 0 | 1 | 2 | 3 | 4 |
| 13. I spend less time doing activities or hobbies than I used to because my mood is low. | 0 | 1 | 2 | 3 | 4 |
| 14. I feel that I want to die. | 0 | 1 | 2 | 3 | 4 |
| 15. I have a heavy feeling in my arms or legs when my mood is down. | 0 | 1 | 2 | 3 | 4 |
| 16. My weight goes up or down a lot depending on my mood. | 0 | 1 | 2 | 3 | 4 |
| 17. Even though I did not do anything wrong, I have felt that I deserved to be punished. | 0 | 1 | 2 | 3 | 4 |
| 18. I have no hope for my future. | 0 | 1 | 2 | 3 | 4 |
Maryland Trait and State Depression—Trait (MTSD-T) Scale
Instruction: This scale asks your general experience of depression, again. However, this time it is asking how you generally feel in most of your adult life, but excluding how you felt in the past 1 week. Try not to be influenced just by how you feel at this moment.
Important: The scale for rating is different here. Please read the scale a couple of times before you start.
| 0 | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| Never | Experienced briefly, but less than once a year | Experienced more than once a year, but less than once a month on average | Experienced intensely for some weeks in my lifetime and in other times less frequent but still there, or experienced almost every month | Experienced many times in a month for almost every month of my adult life | |
| 1. It has been hard for me to feel happy throughout my life. | 0 | 1 | 2 | 3 | 4 |
| 2. I have felt less interested in enjoyable activities than my peers. | 0 | 1 | 2 | 3 | 4 |
| 3. I often lose my appetite when my mood is low. | 0 | 1 | 2 | 3 | 4 |
| 4. I sleep more than most people when my mood is low. | 0 | 1 | 2 | 3 | 4 |
| 5. I felt sluggish and slow most of my life. | 0 | 1 | 2 | 3 | 4 |
| 6. I often feel sad most of my life. | 0 | 1 | 2 | 3 | 4 |
| 7. I have not had sufficient energy for most things. | 0 | 1 | 2 | 3 | 4 |
| 8. I cried often because my mood was low. | 0 | 1 | 2 | 3 | 4 |
| 9. It has usually been hard for me to get motivated. | 0 | 1 | 2 | 3 | 4 |
| 10. I have been burdened with feelings of guilt for much of my life. | 0 | 1 | 2 | 3 | 4 |
| 11. I don’t sleep enough when my mood is low because I think of negative thoughts. | 0 | 1 | 2 | 3 | 4 |
| 12. The blues have stayed with me no matter what I do. | 0 | 1 | 2 | 3 | 4 |
| 13. I have not spent much time doing activities or hobbies because I feel down. | 0 | 1 | 2 | 3 | 4 |
| 14. I have felt that I wanted to die. | 0 | 1 | 2 | 3 | 4 |
| 15. I often have a heavy feeling in my arms or legs when my mood is down. | 0 | 1 | 2 | 3 | 4 |
| 16. My weight has gone up or down a lot depending on my mood. | 0 | 1 | 2 | 3 | 4 |
| 17. Even though I did not do anything wrong, I often felt that I deserved to be punished. | 0 | 1 | 2 | 3 | 4 |
| 18. I feel hopeless about my future. | 0 | 1 | 2 | 3 | 4 |
References
- 1. Carpenter WT, Jr, Heinrichs DW, Alphs LD. Treatment of negative symptoms. Schizophr Bull. 1985; 11: 440–452 [DOI] [PubMed] [Google Scholar]
- 2. Sax KW, Strakowski SM, Keck PE, Jr, Upadhyaya VH, West SA, McElroy SL. Relationships among negative, positive, and depressive symptoms in schizophrenia and psychotic depression. Br J Psychiatry. 1996; 168: 68–71 [DOI] [PubMed] [Google Scholar]
- 3. Schennach-Wolff R, Obermeier M, Seemüller F, et al. Evaluating depressive symptoms and their impact on outcome in schizophrenia applying the Calgary Depression Scale. Acta Psychiatr Scand. 2011; 123: 228–238 [DOI] [PubMed] [Google Scholar]
- 4. Emsley RA, Oosthuizen PP, Joubert AF, Roberts MC, Stein DJ. Depressive and anxiety symptoms in patients with schizophrenia and schizophreniform disorder. J Clin Psychiatry. 1999; 60: 747–751 [DOI] [PubMed] [Google Scholar]
- 5. Rabany L, Weiser M, Werbeloff N, Levkovitz Y. Assessment of negative symptoms and depression in schizophrenia: revision of the SANS and how it relates to the PANSS and CDSS. Schizophr Res. 2011; 126: 226–230 [DOI] [PubMed] [Google Scholar]
- 6. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987; 13: 261–276 [DOI] [PubMed] [Google Scholar]
- 7. Andreasen NC. Scale for the Assessment of Negative Symptoms. Iowa City, IA: University of Iowa Press; 1983. [Google Scholar]
- 8. Alphs LD, Summerfelt A, Lann H, Muller RJ. The negative symptom assessment: a new instrument to assess negative symptoms of schizophrenia. Psychopharmacol Bull. 1989; 25: 159–163 [PubMed] [Google Scholar]
- 9. Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Carpenter WT., Jr The schedule for the deficit syndrome: an instrument for research in schizophrenia. Psychiatry Res. 1989; 30: 119–123 [DOI] [PubMed] [Google Scholar]
- 10. Kirkpatrick B, Strauss GP, Nguyen L, et al. The brief negative symptom scale: psychometric properties. Schizophr Bull. 2011; 37: 300–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Strauss GP, Keller WR, Buchanan RW, et al. Next-generation negative symptom assessment for clinical trials: validation of the Brief Negative Symptom Scale. Schizophr Res. 2012; 142: 88–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mathalon DH, Ford JM. Neurobiology of schizophrenia: search for the elusive correlation with symptoms. Front Hum Neurosci. 2012; 6: 136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Möller HJ. Occurrence and treatment of depressive comorbidity/cosyndromality in schizophrenic psychoses: conceptual and treatment issues. World J Biol Psychiatry. 2005; 6: 247–263 [DOI] [PubMed] [Google Scholar]
- 14. Marengo J, Harrow M, Herbener ES, Sands J. A prospective longitudinal 10-year study of schizophrenia’s three major factors and depression. Psychiatry Res. 2000; 97: 61–77 [DOI] [PubMed] [Google Scholar]
- 15. Cichocki L, Cechnicki A, Polczyk R. Consistency of symptomatic dimensions of schizophrenia over 20 years. Psychiatry Res. 2012; 200: 115–119 [DOI] [PubMed] [Google Scholar]
- 16. Krohne HW, Schmukle SC, Spaderna H, Spielberger CD. The State-Trait Depression Scales: an international comparison. Anxiety Stress Coping. 2002; 15: 105–122 [Google Scholar]
- 17. Terracciano A, Tanaka T, Sutin AR, et al. Genome-wide association scan of trait depression. Biol Psychiatry. 2010; 68: 811–817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lako IM, Bruggeman R, Knegtering H, et al. A systematic review of instruments to measure depressive symptoms in patients with schizophrenia. J Affect Disord. 2012; 140: 38–47 [DOI] [PubMed] [Google Scholar]
- 19. Chemerinski E, Bowie C, Anderson H, Harvey PD. Depression in schizophrenia: methodological artifact or distinct feature of the illness? J Neuropsychiatry Clin Neurosci. 2008; 20: 431–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. First MB, Spitzer RL, Gibbon M, Williams JBW. Structural Clinical Interview for DSM-IV Axis I Disorders (SCID-IV). New York, NY: New York State Psychiatric Institute, Biometrics Research; 1997. [Google Scholar]
- 21. Strauss GP, Hong LE, Gold JM, et al. Factor structure of the brief negative symptom scale. Schizophr Res. 2012; 142: 96–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McNair DM, Lorr M, Droppleman LF. EITS Manual for the Profile of Mood States. San Diego, CA: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 23. StataCorp Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 24. Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error J Market Res. 1981; 18: 39–50 [Google Scholar]
- 25. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology Psychol Assess. 1994; 6: 284–290 [Google Scholar]
- 26. Kim SW, Kim SJ, Yoon BH, et al. Diagnostic validity of assessment scales for depression in patients with schizophrenia. Psychiatry Res. 2006;144:57–63 [DOI] [PubMed] [Google Scholar]
- 27. Keller WR, Fischer BA, Carpenter WT., Jr Revisiting the diagnosis of schizophrenia: where have we been and where are we going? CNS Neurosci Ther. 2011; 17: 83–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Peralta V, Cuesta MJ. Exploring the borders of the schizoaffective spectrum: a categorical and dimensional approach. J Affect Disord. 2008; 108: 71–86 [DOI] [PubMed] [Google Scholar]
- 29. Van Os J, Jones PB. Neuroticism as a risk factor for schizophrenia. Psychol Med. 2001; 31: 1129–1134 [DOI] [PubMed] [Google Scholar]
- 30. Horan WP, Blanchard JJ, Clark LA, Green MF. Affective traits in schizophrenia and schizotypy. Schizophr Bull. 2008; 34: 856–874 [DOI] [PMC free article] [PubMed] [Google Scholar]