Abstract
Object: Sevoflurane and propofol are both widely used in clinical anesthesia. The aim of this study is to compare the effects of sevoflurane and propofol on right ventricular function and pulmonary circulation in patients receiving esophagectomy. Methods: Forty adult patients undergoing an elective open-chest thoracotomy for esophagectomy were randomized to receive either propofol (n=20) or sevoflurane (n=20) as the main anesthetic agent. The study was performed in Changzheng Hospital. Hemodynamic data were recorded at specific intervals: before the surgery (T0), BIS values reaching 40 after anesthesia induction (T1), two-lung ventilation (T2), ten minutes after one-lung ventilation (T3), the end of the operation (T4) using PiCCO2 and Swan-Ganz catheter. Results: CI, RVEF, RVSWI and RVEDVI were significantly smaller in propofol group than those in sevoflurane group throughout the surgery (P<0.05). However, SVRI was significantly greater in propofol group than that in sevoflurane group (P<0.05). Compared with the patients in propofol group, the patients who received sevoflurane had a greater reduction in OI and increase in Os/Ot (P<0.05). And, PVRI was significantly smaller in sevoflurane group than in propofol group (P<0.05). Conclusion: Anesthesia with sevoflurane preserved better right ventricular function than propofol in patients receiving esophagectomy. However, propofol improved oxygenation and shunt fraction during one-lung ventilation compared with sevoflurane anesthesia. To have the best effect, anesthesiologists can choose the two anesthetics flexibly according to the monitoring results.
Keywords: Sevoflurane, propofol, right ventricular function, pulmonary circulation, esophagectomy
Introduction
Mortality from esophagectomy has declined over the past 30 years [1]. Anastomotic and cardiopulmonary complications contribute to the majority of perioperative morbidity and mortality. How to reduce the incidence of these complications has become more and more concerned. Some studies have demonstrated that the choice of an appropriate anesthesia method may achieve a good outcome. So we are intended to investigate the effects of different anesthetics on patients who are undergoing esophagectomy.
Esophagectomy has obvious effects on hemodynamics. One-lung ventilation can result in increased pulmonary vascular resistance (PVR) induced by hypoxic pulmonary vasoconstriction (HPV), increased ventilation pressure, hypoxemia or hypercarbia [2]. These consequences can lead to hemodynamic instability. A great number of disputes have risen about volatile anesthetics and intravenous anesthetics in the open chest surgery. Researches showed that fluoroalkenes and sevoflurane could reduce pulmonary inflammatory reaction when compared with propofol. However, other studies found that sevoflurane would cause more serious inflammation reactions than propofol in thoracic surgery [3].
As well known, several studies have reported that right ventricular function (RVF) directly influences systemic circulation [4]. Thus, monitoring RVF and pulmonary circulation can be useful to optimize hemodynamic management of patients undergoing esophagectomy. However, there are few researches on the impact of sevoflurane and propofol on RVF in esophageal surgery. This study is aimed to investigate the effects of sevoflurane and propofol on the right ventricular function and the pulmonary circulation of patients receiving esophagectomy. We hypothesized that oxygenation and right ventricular function might become better during propofol and during sevoflurane respectively. There are many methods to monitor the right heart function. The Swan-Ganz catheter methods as the golden standard of hemodynamic monitoring have been used for many years [5]. In addition, this study adopted PiCCO2 as an advanced hemodynamic monitoring indicator which allowed the anesthesiologists to improve fluid management, hemodynamics and pulmonary gas exchange.
Methods
Patient population
The study was approved by the Institutional Ethical Committee (Second Military Medical University) and written informed consent was obtained. 40 patients (between 50 and 75 years old) undergoing an elective open-chest thoracotomy for esophagectomy were prospectively enrolled whose ASA physical status were I-II. Patients with cardiac disease, heart failure, arrhythmia, bronchial inflammation, coagulation disorders, hepatic and renal insufficiency were excluded. Patients were randomly (by opening of an envelope) allocated to receive either propofol (group P) or sevofl urane (group S).
Anesthesia and surgery
In the operating room, the patients received routine monitoring, including electro-cardiogram, pulse oximetry, capnogram, arterial pressure, and bispectral index (BIS). A Swan-ganz catheter was placed into the right external jugular vein. A thermistor-tipped catheter (4 F, PiCCO Catheter, Pulsion, Munich, Germany) was placed into the right femoral artery in the purpose of detecting transcardiopulmonary thermodilution. In group P, anesthesia was induced with a target-controlled infusion of propofol at a target plasma concentration of 6 μg/ml, adjusting BIS value between 40-60. In group S, sevofl urane was initially given at the concentration of 8% (6 L/min) so as to prime the anesthesia machine pipeline for 3 minutes. As soon as the patients lost consciousness and BIS values dropped to 40, remifentanil was given at a target plasma concentration of 4 ng/ml. The patients were intubated with a left-sided double-lumen tube (DLT) (Smiths, Hythe, Kent, UK: 39 F for males and 37 F for females) after cisatracurium (0.15 mg kg-1) was given. Fiberoptic bronchoscopy was used to confi rm the correct positioning of the DLT immediately after its blind insertion. The lungs were ventilated with a Primus Ventilator (Drager, Lubeck, Germany). VT was set at 8 ml kg-1 and FiO2 was 100%. Respiratory frequency was adjusted to 12-14/min to maintain end-tidal-carbon-dioxide tension (EtCO2) between 35-45 cmH2O.
Hemodynamic data analysis
The following parameters were recorded: mean arterial pressure (MAP), central venous pressure (CVP), mean pulmonary artery pressure (PMAP), pulmonary artery wedge pressure (PAWP), stroke volume index (SVI), cardiac index (CI), and systemic vascular resistance index (SVRI), RV hemodynamic data (right ventricular ejection fraction [RVEF], RV end-diastolic volume index [RVEDVI], RV stroke work index [RVSWI]), pulmonary vascular resistance index (PVRI), transmembrane pressure, mixed-venous and arterial blood gas analysis. Pulmonary shunt fraction (Qs/Qt) and oxygenation index (OI) were calculated by the following formula:
Qs/Qt = (PAa-DO2×0.0331)/PA-aDO2×0.0331+ (CaO2-CvO2) OI = PaO2/FiO2
These parameters were all recorded at specific intervals: before the surgery (T0), BIS values reaching 40 after anesthesia induction (T1), two-lung ventilation (T2), 10 minutes after one-lung ventilation (T3) and the end of the operation (T4). Each interval lasted for 10 minutes after stability, and we took the average value in three times as the final data for all the patients.
Statistical analysis
Continuous data were presented as means ± standard deviation. Independent sample t-test and variance analysis of repeated measurement were performed. For count data, constituent ratio and chi-square analysis were used. Wilcoxon rank-sum test was used in comparison of non-normal distribution and variance heterologous measurement data. For all data analyzed, a P value≤0.05 was considered statistically significant. Statistical tests were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
There were no signifi cant differences in the characteristics of the patients (Table 1). And there were no differences between these two groups in the duration of operation, anesthesia and one-lung ventilation, the amount of bleeding, the total amount of fluid infusion and urine volume. Compared with group P, the incident of hypoxemia in the operation was higher in group S. One patient in group P developed and died of anastomotic leakage after operation. Another three patients in group S also died, in which one died of massive hemorrhage in the digestive tract, and two died of anastomotic leakage. There were no differences in the number of days in hospital and the time of removing gastric tube. But the number of days staying at intensive care unit in group P was much more than that in group S (Table 2).
Table 1.
Patient characteristics and baseline findings
| Propofol (n=20) | Sevoflurane (n=20) | |
|---|---|---|
| Age (yr) | 59.0±7.8 | 60.6±6.6 |
| BMI (kg/m2) | 22.1±2.2 | 23.1±2.2 |
| Sex (M/F) | 15/5 | 14/6 |
| ASA (I/II) | 16/4 | 17/3 |
Data were expressed as mean ± SD. There were no differences between two groups.
Table 2.
Other data in perioperative
| Propofol (n=20) | Sevoflurane (n=20) | |
|---|---|---|
| Operation time (min) | 281.15±90.01 | 226.77±58.84 |
| Anesthesia time (min) | 329.77±67.65 | 298.00±54.83 |
| One lung ventilation time (min) | 143.23±34.02 | 147.08±28.62 |
| hypoxemia (n) | 2 | 8* |
| Mount of bleeding (ml) | 337.5±102.52 | 250.00±67.7 |
| Mount of fluid infusion (ml) | 2269.23±655.92 | 1929.85±585.15 |
| Urine volume (ml) | 784.62±256.89 | 789.23±404.67 |
| Intensive care unit stay (d) | 4.69±3.66 | 2.23±1.36* |
| Hospital stay (d) | 19.92±14.22 | 26.60±24.87 |
| Time of removing gastric tube (d) | 10.31±8.42 | 14.90±17.55 |
| Complication: | ||
| ARDS | 1 | 0 |
| Pulmonary infection | 2 | 0 |
| Anastomotic leakage | 3 | 6 |
| arrhythmia | 1 | 0 |
| Cardiac insufficiency | 0 | 1 |
| death | 1 | 3 |
Data were expressed as mean ± SD.
P<0.05 sevoflurane group vs propofol group.
The patients were comparable for all measured and derived variables at baseline (Table 3). The values for MAP, SVI, PMAP, CVP and PAWP did not significantly differ between two groups (Figure 1). Both groups exhibited a significant reduction in CI from baseline to TLV. CI was significantly smaller in the propofol group than that in the sevoflurane group throughout the surgery (Figure 1). However, SVRI was significantly greater in the propofol group than that in the sevoflurane group (Figure 1). Similarly, RVEF, RVSWI and RVEDVI of the patients who received sevoflurane were significantly greater all the time after baseline than those of the patients who received propofol (Figure 2).
Table 3.
Hemodynamic findings at baseline
| Propofol (n=20) | Sevoflurane (n=20) | |
|---|---|---|
| MAP (mmHg) | 109.5±13.9 | 107.7±12.3 |
| CVP (mmHg) | 5.8±2.8 | 5.4±2.0 |
| PMAP (mmHg) | 19.2±5.6 | 15.8±2.5 |
| PAWP (mmHg) | 9.8±3.5 | 8.5±2.5 |
| CI (L/min·m2) | 3.9±0.8 | 3.9±0.6 |
| RVEF (%) | 38.4±7.3 | 37.3±7.8 |
| RVSWI (g·m/m2) | 7.8±2.8 | 7.0±2.4 |
| RVEDVI (ml/m2) | 122.6±22.3 | 135.1±23.0 |
| GEDVI (ml/m2) | 755.5±132.8 | 832.8±152.1 |
| EVLWI (ml/kg) | 6.9±2.0 | 8.2±4.0 |
| OI (mmHg) | 425.7±41.5 | 427.8±74.0 |
| PVRI (dyn·s-1·cm-5) | 185.1±62.2 | 157.5±60.6 |
| Qs/Qt (%) | 12.8±3.2 | 13.6±3.6 |
Data were expressed as mean ± SD. There were no differences between two groups.
Figure 1.
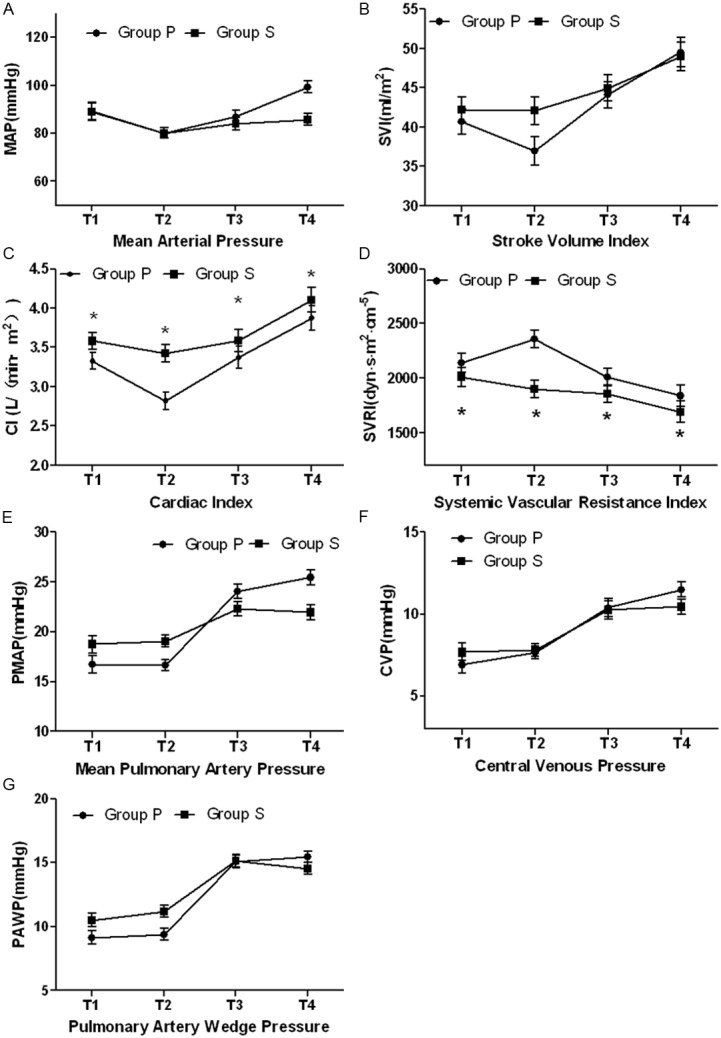
Changes in hemodynamic data at after anesthesia induction (T1), two lung ventilation (T2), one lung ventilation (T3) and the end of the operation (T4) in propofol group and sevoflurane group. A was mean arterial pressure (MAP), B was stroke volume index (SVI), C was Cardiac index (CI), D was stroke volume index (SVI), E was mean pulmonary artery pressure (PMAP), F was central venous pressure (CVP), G was pulmonary artery wedge pressure (PAWP). The values for MAP (P=0.140), SVI (P=0.369), PMAP (P=0.790), CVP (P=0.899), and PAWP (P=0.203) did not significant differ between two groups. CI was significantly smaller in propofol group than in sevoflurane group throughout the surgery (P=0.007). SVRI was significantly greater in propofol group than in sevoflurane group (P=0.022). *P<0.05 between groups.
Figure 2.
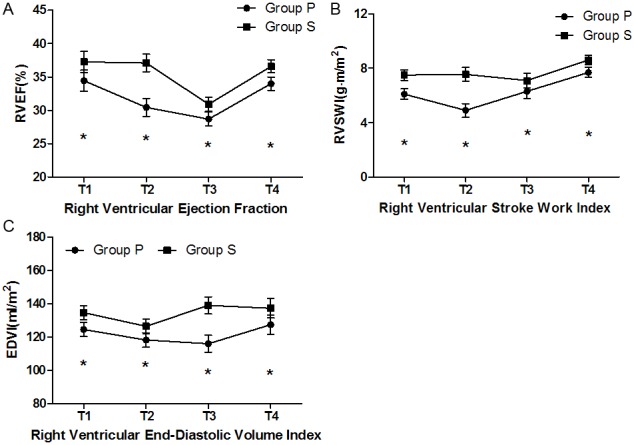
Changes in right ventricular function data at after anesthesia induction (T1), two lung ventilation (T2), one lung ventilation (T3) and the end of the operation (T4) in propofol group and sevoflurane group. A was right ventricular ejection fraction (RVEF), B was RV stroke work index (RVSWI), C was RV end-diastolic volume index (RVEDVI). RVEF (P=0.008), RVEDVI (P=0.019), RVSWI (P=0.003) were significantly smaller in propofol group than in sevoflurane group throughout the surgery. *P<0.05 between groups.
Conversion from TLV to OLV caused a significant decrease in OI (p=0.000) and an increase in Qs/Qt (p=0.000) in both groups. Compared with the patients who received propofol, those who received sevoflurane got even greater reduction in OI and increase in Os/Ot (Figure 3). However, PVRI was significantly smaller in the sevoflurane group than in the propofol group. And there were no significant differences in transmembrane pressure between the two groups (Figure 3).
Figure 3.
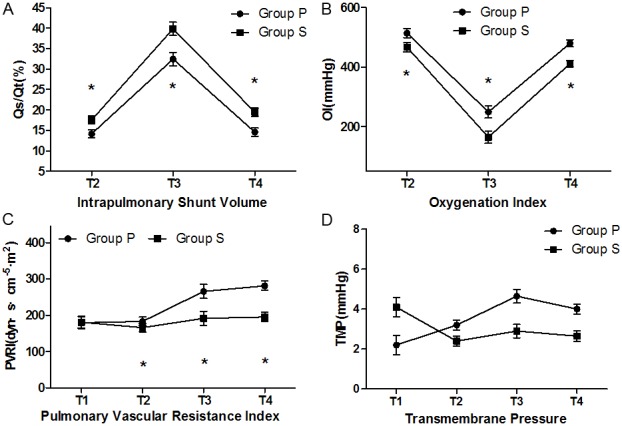
Changes in pulmonary circulation data at two lung ventilation (T2), one lung ventilation (T3) and the end of the operation (T4) in propofol group and sevoflurane group. A was pulmonary shunt fraction (Qs/Qt), B was oxygenation index (OI), C was pulmonary vascular resistance index (PVRI), D was transmembrane pressure. OI decreased more greatly in sevoflurane group than in propofol group (P=0.000). Qs/Qt increased more greatly in sevoflurane group than in propofol group (P=0.000). PVRI was significantly smaller in sevoflurane group than in propofol group (P=0.016). *P<0.05 between groups.
Discussion
In order to reduce the postoperative complication, anesthesiologists have adopted plenty of approaches, including the choice of appropriate way of anesthesia way, dose of anesthetics, respiratory parameters, ventilation mode, goal-directed fluid therapy, oxygenation improvement with drugs, ventilation side lung protection and etc. Propofol and sevoflurane are common regimen in clinical anesthesia. This study employed PiCCO2 and Swan-Ganz catheter methods to compare the influence of sevoflurane and propofol on the right heart function and pulmonary circulation.
Patients’ characteristics, the duration of operation, anesthesia and one-lung ventilation were similar in both groups. The intraoperative bleeding loss, the total amount of fluid infusion, and urine volume were also similar among all the patients, which suggested that the differences in cardiac function between the groups were not caused by the differences in patients’ characteristics and intraoperative events but were related to the choice of anesthetic agent.
The results of the present study indicated that the choice of the anesthetic regimen infl uenced cardiac function and pulmonary circulation. Indeed, the patients who were anesthetized with sevofl urane obtained signifi cantly better cardiac function, but lower oxygenation than the patients who were anesthetized with propofol. And sevoflurane had greater influence on the peripheral vascular resistance than propofol.
In this study, we had shown that although there were no significant differences in MAP, SVI, CVP and PMAP between the two groups, the patients who received propofol experienced a greater and more sustained reduction in CI, RVEDVI, RVSWI and RVEF when compared with those who received sevoflurane. Some studies have found that sevoflurane preserved myocardial function better than propofol in myocardial ischemia-reperfusion [6,7]. These results may be explained by the vasodilatory effects of propofol and a reduction in cardiac baroreflex sensitivity by propofol. Immunoregulatory effects of volatile anesthetic might contribute to our results. Recent studies have identified an immunoregulatory role of sevofl urane that had signifi cant reduction of infl ammatory mediators and a remarkably better clinical outcome (defi ned by postoperative adverse events) during anesthesia in patients undergoing thoracic surgery with OLV [8,9]. But some scholars have an opposite opinion. Sevoflurane was found to cause a greater proinflammatory response than propofol during thoracic surgery [10]. Therefore, the contribution of the anesthetic type to the inflammatory response during esophagectomy and clinical outcome remains unknown. Along with the progress of monitoring methods, researchers have been paying more attention to the right ventricular function. But data about the effects of sevoflurane and propofol on it were limited. In one study, investigators found the patients who received propofol obtaining significantly smaller CI and RVEF, but greater end-systolic volume index (ESVI) than those who received isoflurane [11]. Although the type of volatile anesthetics was different, two studies demonstrated that patients who received isoflurane and sevoflurane made smaller influences on RVF than those who received propofol.
The patients who received propofol had higher SVRI and PVRI than the patients who received sevoflurane, in consistent with some other studies. One study examined the dose-related effects of sevoflurane and isoflurane on systemic vascular resistance during cardiopulmonary bypass in patients suffering elective coronary artery surgery. The result showed that there were no significant changes of SVRI in patients receiving 1.0 and 2.0 vol% sevoflurane. However, 3 vol% sevoflurane decreased SVRI significantly [12]. De Blasi compared the effects of remifentanil-based general anaesthesia with propofol or sevoflurane on muscle microcirculation. He found that in patients who received general anesthesia with remifentanil–propofol, muscle blood fl ow increased greater than in those who received remifentanil–sevofl urane [13].
Another finding of this study was that the OI in the propofol group was greater than that in the sevoflurane group, and Qs/Qt in the propofol group was lower than that in the sevoflurane group. Kazuo Abe observed the same consequence as our study. He demonstrated that propofol improved oxygenation and shunt fraction during one-lung ventilation compared with sevoflurane and isoflurane [14]. The reason was intravenous anesthetic agents had little effect on HPV. However, some studies showed different outcomes. D.H. Beck found the administration of sevoflurane (1 MAC) resulted in smaller increase in shunt fraction during thoracic surgery with OLV, when compared with propofol [15]. And the reason was the inhibition of HPV by sevoflurane. The low concentration of sevoflurane resulted in small changes in shunt fraction as mechanism of propofol.
In conclusion, anesthesia with sevofl urane preserved the right ventricular function, when compared with propofol in esophagectomy. However, propofol improved better oxygenation and shunt fraction during one-lung ventilation sevoflurane. Two anesthetics take their own advantages and disadvantages. Accordingly, anesthesiologists should choose them according to the different requirements of operation. However, further studies are required to verify and optimize these beneficial effects as well as the underlying mechanism.
Acknowledgements
The study was supported by the project of Health Department of General Logistics Department of Chinese People’s Liberation Army (13QNP097).
Disclosure of conflict of interest
None.
References
- 1.Chang AC, Ji H, Birkmeyer NJ, Orringer MB, Birkmeyer JD. Outcomes after transhiatal and transthoracic esophagectomy for cancer. Ann Thorac Surg. 2008;85:424–9. doi: 10.1016/j.athoracsur.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Trepte C, Haas S, Meyer N, Gebhardt M, Goepfert MS, Goetz AE, Reuter DA. Effects of one-lung ventilation on thermodilution-derived assessment of cardiac output. Br J Anaesth. 2012 Jun;108:922–8. doi: 10.1093/bja/aes032. [DOI] [PubMed] [Google Scholar]
- 3.Ng JM. Update on anesthetic management for esophagectomy. Curr Opin Anaesthesiol. 2011 Feb;24:37–43. doi: 10.1097/ACO.0b013e32834141f7. [DOI] [PubMed] [Google Scholar]
- 4.Redington AN. Right ventricular function. Cardiol Clin. 2002;20:341–9. v. doi: 10.1016/s0733-8651(02)00005-x. [DOI] [PubMed] [Google Scholar]
- 5.Munro HM, Wood CE, Taylor BL, Smith GB. Continuous invasive cardiac output monitoring--the Baxter/Edwards Critical-Care Swan Ganz IntelliCath and Viligance system. Clin Intensive Care. 1994;5:52–5. [PubMed] [Google Scholar]
- 6.Bein B, Renner J, Caliebe D, Scholz J, Paris A, Fraund S, Zaehle W, Tonner PH. Sevoflurane but not propofol preserves myocardial function during minimally invasive direct coronary artery bypass surgery. Anesth Analg. 2005 Mar;100:610–6. doi: 10.1213/01.ANE.0000145012.27484.A7. [DOI] [PubMed] [Google Scholar]
- 7.Nader ND, Li CM, Khadra WZ, Reedy R, Panos AL. Anesthetic myocardial protection with sevoflurane. J Cardiothorac Vasc Anesth. 2004 Jun;18:269–74. doi: 10.1053/j.jvca.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 8.De Conno E, Steurer MP, Wittlinger M, Zalunardo MP, Weder W, Schneiter D, Schimmer RC, Klaghofer R, Neff TA, Schmid ER, Spahn DR, Z’graggen BR, Urner M, Beck-Schimmer B. Anesthetic-induced improvement of the inflammatory response to one-lung ventilation. Anesthesiology. 2009 Jun;110:1316–26. doi: 10.1097/ALN.0b013e3181a10731. [DOI] [PubMed] [Google Scholar]
- 9.Sugasawa Y, Yamaguchi K, Kumakura S, Murakami T, Suzuki K, Nagaoka I, Inada E. Effects of sevoflurane and propofol on pulmonary inflammatory responses during lung resection. J Anesth. 2012 Feb;26:62–9. doi: 10.1007/s00540-011-1244-y. [DOI] [PubMed] [Google Scholar]
- 10.Abou-Elenain K. Study of the systemic and pulmonary oxidative stress status during exposure to propofol and sevoflurane anaesthesia during thoracic surgery. Eur J Anaesthesiol. 2010 Jun;27:566–71. doi: 10.1097/EJA.0b013e3283392c1d. [DOI] [PubMed] [Google Scholar]
- 11.Ewalenko P, Brimioulle S, Delcroix M, Lejeune P, Naeije R. Comparison of the effects of isoflurane with those of propofol on pulmonary vascular impedance in experimental embolic pulmonary hypertension. Br J Anaesth. 1997 Nov;79:625–30. doi: 10.1093/bja/79.5.625. [DOI] [PubMed] [Google Scholar]
- 12.Rödig G, Keyl C, Wiesner G, Philipp A, Hobbhahn J. Effects of sevoflurane and isoflurane on systemic vascular resistance: use of cardiopulmonary bypass as a study model. Br J Anaesth. 1996 Jan;76:9–12. doi: 10.1093/bja/76.1.9. [DOI] [PubMed] [Google Scholar]
- 13.De Blasi RA, Palmisani S, Boezi M, Arcioni R, Collini S, Troisi F, Pinto G. Effects of remifentanil-based general anaesthesia with propofol or sevofl urane on muscle microcirculation as assessed by near-infrared spectroscopy. Br J Anaesth. 2008 Aug;101:171–7. doi: 10.1093/bja/aen136. [DOI] [PubMed] [Google Scholar]
- 14.Abe K, Shimizu T, Takashina M, Shiozaki H, Yoshiya I. The effects of propofol, isoflurane, and sevoflurane on oxygenation and shunt fraction during one-lung ventilation. Anesth Analg. 1998 Nov;87:1164–9. doi: 10.1097/00000539-199811000-00035. [DOI] [PubMed] [Google Scholar]
- 15.Beck DH, Doepfmer UR, Sinemus C, Bloch A, Schenk MR, Kox WJ. Effects of sevoflurane and propofol on pulmonary shunt fraction during one-lung ventilation for thoracic surgery. Br J Anaesth. 2001 Jan;86:38–43. doi: 10.1093/bja/86.1.38. [DOI] [PubMed] [Google Scholar]


