Abstract
Interdigitating dendritic cell sarcoma (IDCS) and histiocytic sarcoma (HS) are two distinct rare hematolymphoid neoplasms, and HS derived from a likely pre-existing IDCS has never been reported in the English literature. Diagnosis of such entities in excised specimens is difficult, but becomes more difficult with the scant amount of materials obtained with fine needle aspiration (FNA) and core needle biopsy. Here we present an interesting and unique case of an IDCS located within a mesenteric mass, which was initially diagnosed as IDCS from the cytology of FNA and core needle biopsy specimens. After brief chemotherapy, the patient again developed abdominal pain, and a HS was diagnosed based on the excised segmental small intestinal specimen. While the exact relationship between the IDCS and HS cannot be ascertained, it is most likely that the HS is derived from the IDCS, although co-existing HS in addition to IDCS from the cytology specimen cannot be completely ruled out.
Keywords: Interdigitating dendritic cell sarcoma, histiocytic sarcoma, fine needle aspiration
Introduction
Dendritic cells (DCs) are specialized professional antigen-presenting cells, which are important in the cell-mediated adaptive immune response to foreign antigens through the activation of T-cells [1]. Within the lymph node, DCs can be further sub-classified into migratory DCs and resident DCs. Migratory DCs, such as Langerhans cells and dermal dendritic cells, are responsible for transporting antigens from distant sites to the lymph node for cross-presentation to T-cells [1]. Resident DCs include follicular dendritic cells, which are located in germinal centers, and interdigitating dendritic cells (IDCs), which reside in t-zones in the peripheral lymphoid tissues, such as the paracortex and deep cortex of lymph nodes, tonsils, inter-follicular regions of mucosa-associated lymphoid tissue, and splenic peri-arteriolar lymphoid sheaths [2,3]. Unlike follicular DCs, IDCs are derived from the hematopoietic stem cells from bone marrow [4].
Neoplasia derived from IDCs, namely, interdigitating dendritic cell sarcoma (IDCS), is an extremely rare sarcoma with approximately 63 reported cases in the English literature worldwide. The vast majority of the IDCS are presented as case reports with the earliest large series of 4 cases by Nakamura and associates [5]. All except 2 reported cases of IDCS were diagnosed based on excisional biopsy [6,7].
Histiocytic sarcoma (HS) is a malignant epithelioid neoplasia with a cell origin of mature histiocytes, which are also derived from hematopoietic stem cells of bone marrow. IDCs and histiocytes have the same cell origin, namely, CD34(+) myeloid stem cells [8], therefore, it is not surprising that IDCS and HS have overlapping features as reported by the International Lymphoma Study Group (ILSG) [2]. While HS with interdigitating dendritic cell differentiation has been reported on 2 previous cases [7,9], possible differentiation of IDCS into HS has not yet been reported in the English literature to the best of our knowledge. Herein we report a case of IDCS as an initial diagnosis based on the core biopsy, with HS diagnosed a few months later following chemotherapy.
Case report
The patient is a 58-year-old female with a past medical history significant for cervical dysplasia and a benign breast nodule, who presented to her primary care physician in November 2011 with intermittent abdominal pain and intentional weight loss of 40 pounds due to strict diet over one year. Work-up included a computed tomography (CT) and positron emission tomography (PET) CT scans of her abdomen, which showed multiple abnormalities including (1) a 3-cm circumferential focal thickening of the distal ileum; (2) peritoneal thickening and mesenteric/omental stranding; and (3) a single 3.1 cm central mesenteric mass within the right mid-abdomen and mesentery. Additionally there was free fluid within the peritoneal cavity, as well as subtle peritoneal enhancement and vague induration within the mesenteric fat. No additional lymphadenopathy was noted in the pelvis, mesentery or retroperitoneum and there was no cervical lymphadenopathy or splenomegaly. Subsequently in December, a CT-guided FNA and core needle biopsy of the mesenteric mass was performed.
A cellular specimen was obtained by FNA. In the background of small mature lymphoid cells and blood are scattered mononucleated large atypical cells with oval nuclear contours, fine nuclear chromatin, and conspicuous nucleoli (Figure 1A & 1B). The H&E sections of the concurrent core needle biopsy showed several scattered reactive secondary follicles (Figure 1C & 1D) and interfollicular regions consisting of medium sized to large atypical cells (Figure 1D-F). These atypical cells showed oval to spindle-shaped nuclear contours, homogenous smooth chromatin, and conspicuous nucleoli (Figure 1E & 1F).
Figure 1.
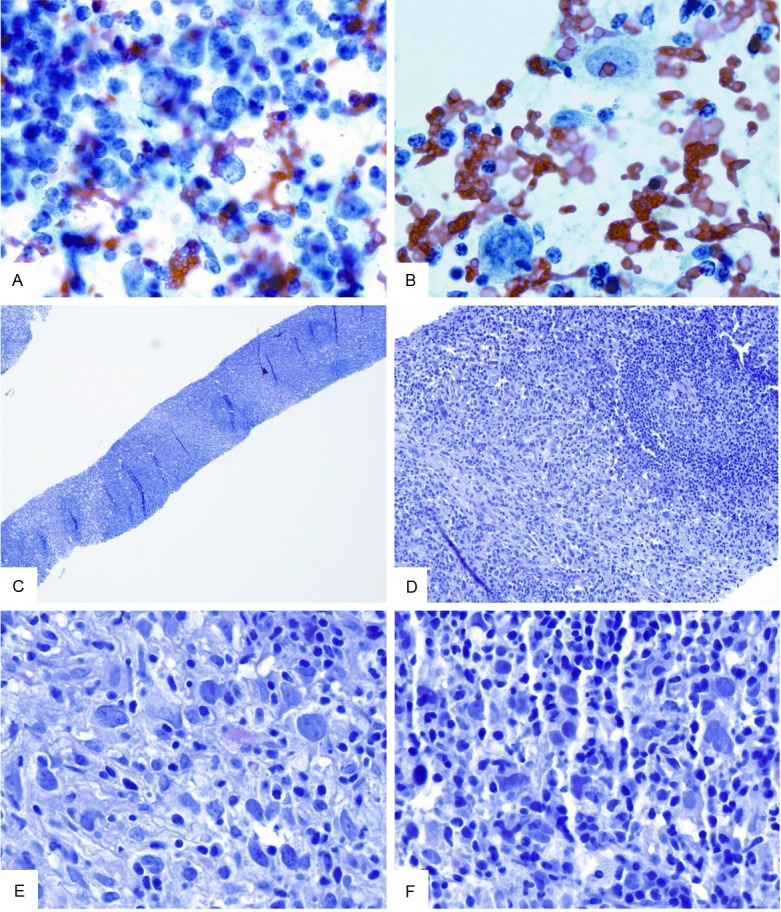
Biopsy specimen. A & B: Scattered large atypical mononucleated cells are present in the background of blood and small mature lymphoid cells (PAP, original magnification 500x); C & D: Core needle biopsy shows expansion of interfollicular regions among reactive secondary follicles (C: H&E, original magnification 20x; D: H&E, original magnification 100x); E & F: Scattered large atypical mononucleated cells with oval to spindle-shaped nuclear contours are easily appreciated in the background of small mature lymphoid cells and rare fibroblasts (E & F: H&E, original magnification 400x, respectively).
To characterize the nature of these atypical medium to large sized cells, a panel of immunohistochemistry was performed. The atypical cells were positive for CD68 (weak) (Figure 2A), lysozyme (partial) (Figure 2B), S100 (strong) (Figure 2C), and vimentin (strong) (Figure 2D), but negative for CD45 (Figure 2E), CD30 (Figure 2F), AE1/AE3, ALK-1, CD1a, CD3, CD19, CD21, CD23, CD35, CD117, HMB-45, and smooth muscle actin (SMA) (data not shown). A malignant neoplasia most compatible with an IDCS was rendered based on the combined morphologic and immunohistochemical findings.
Figure 2.
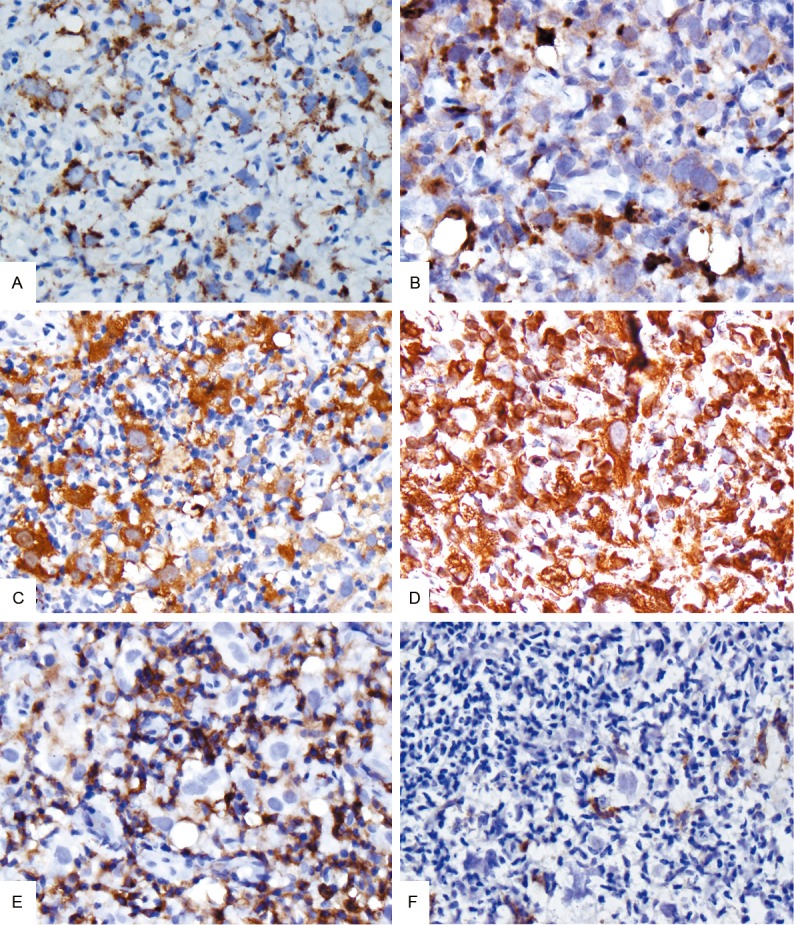
Biopsy specimen, special stains. The atypical large mononucleated cells from the retroperitoneal “mass” are weakly positive for CD68 (A), variably positive for lysozyme (B), strongly positive for S-100 (C), vimentin (D), but negative for CD45 (E) and CD30 (F). (A-F: Original magnification 400x, 400x, 400x, 400x, 400x, and 400x, respectively).
A staging bone marrow biopsy performed in the same month showed normocellular bone marrow with trilineage hematopoiesis and no evidence of involvement by IDCS. The patient was thus scored as 0 by ECOG criteria.
Due to possible multi-focal involvement based on imaging studies, the patient was treated with 6 cycles of CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone), which ended in May. The patient tolerated the chemotherapy well, and the post-chemotherapy scan showed some response but the circumferential mass in the distal ileum still persisted. Therefore, the patient was readmitted into the hospital in September and laparoscopic resection of the mass was performed.
The resection specimen consisted of an 8 cm long segment of small bowel with an attached portion of omentum measuring 12 x 6 x 2.5 cm. Upon opening, the small bowel lumen was found to be completely obstructed by a circumferential submucosal mass with yellow-tan cut surfaces that measured 4.0 cm in greatest dimension.
H&E sections of the excised segment of small bowel show unremarkable small intestinal epithelium with a transmural infiltrate spanning from the serosal surface to the deep layer of the lamina propria (Figure 3A). Within a background ranging from xanthomatous histiocytes (Figure 3B) to spindle fibroblasts (Figure 3C) are easily appreciated scattered large atypical mononucleated cells with irregular nuclear contours (Figure 3B & 3D). In addition, there are focal clusters and sheets of these cells (Figure 3D), some of which show bizarre features such as multi-lobation or multi-nucleation (Figure 3D).
Figure 3.
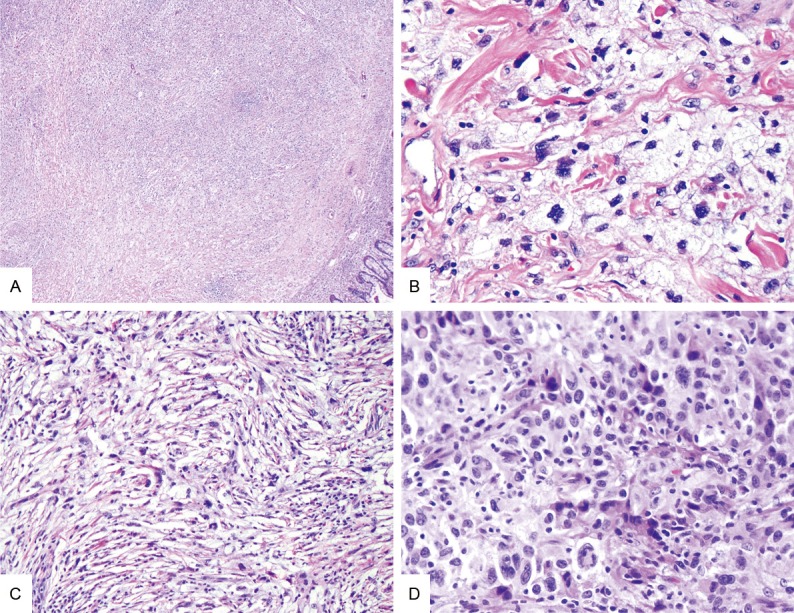
Small intestine resection specimen. At low power, the infiltrate (A) spans from deep lamina propria (lower right) to serosal surface (not shown) (H&E, original magnification 20x). Scattered atypical large mononucleated cells lie from the pauci-cellular xanthomatous (B) and fibrous background (C), to overt cellular regions (D) composed of predominantly large atypical mononucleated cells with occasional large bizarre-appearing cells (D). (B-D: H&E, original magnification 200x, 100x, and 200x, respectively).
To further characterize the nature of the atypical cells and to elucidate the relationship between these cells and the previous core needle biopsy specimen, an array of immunohistochemistry was employed. As showed in Figure 4, these cells are positive for CD68 (Figure 4A) (strong), lysozyme (Figure 4B), and CD163 (Figure 4C), but are negative for S100 (Figure 4D), AE1/AE3, CD1a, CD3, CD15, CD20, CD21, CD23, CD30, CD35, CD45, and SMA (data not shown). Based on the combined morphologic and immunohistochemical features, a diagnosis of HS was rendered. The mesenteric lymph nodes were found to be free of HS.
Figure 4.
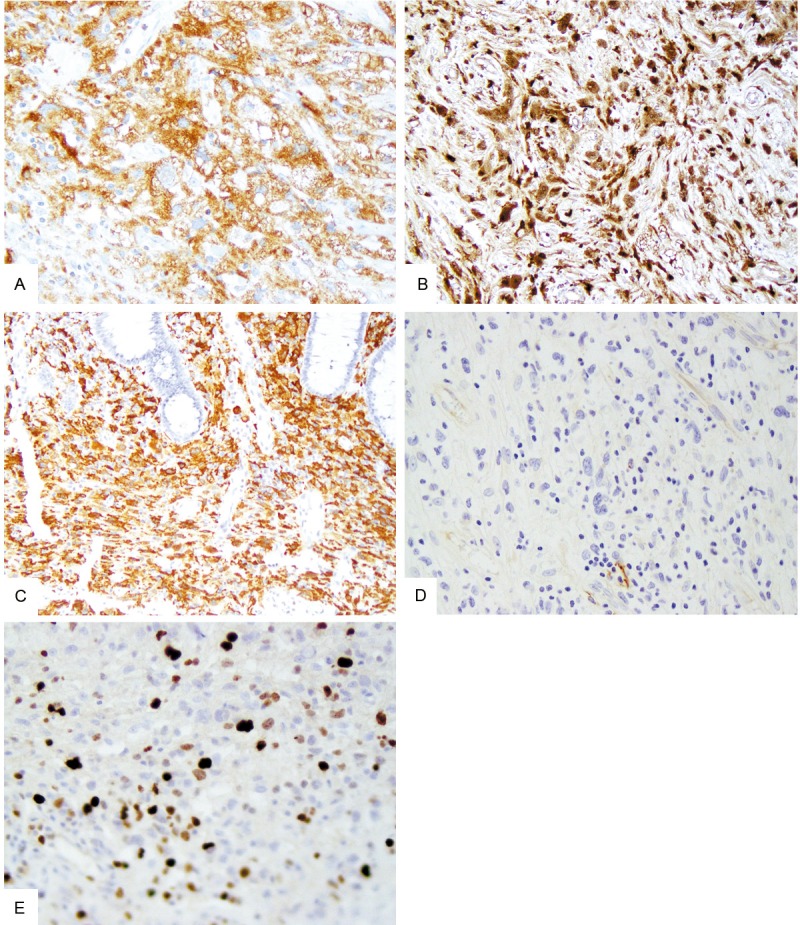
Small intestine resection specimen, special stains. The atypical large mononucleated cells from the intestinal mass are strongly positive for CD68 (A), lysozyme (B), and CD163 (C), but negative for S-100 (D). (A-D: original magnification 200x, 100x, 100x, and 200x, respectively). A proportion of the atypical cells are positive for Ki-67 (E) (original magnification 200x).
Discussion
This is an unusual and unique case from the following two aspects: first, the initial diagnosis of IDCS using FNA and core needle biopsy materials was challenging given the scant amount of material to work with and the rarity of IDCS; secondly, the diagnosis of HS was a surprise from the excised intestinal specimen given the initial diagnosis of IDCS. While a co-existing HS in addition to the IDCS from the initial core biopsy cannot be excluded due to the nature of the limited core biopsy, an immediate question one would like to ask is: what is the relationship between IDCS and HS? Is HS an evolution of IDCS? What is the effect of chemotherapy, if any, in this process?
IDCS and HS are neoplasia derived from IDCs and mature histiocytes, respectively [6]. While both IDCs and histiocytes are from CD34(+) myeloid stem cells in the bone marrow [8], and IDCS and HS share overlapping immunohistochemical features [10,11], IDCS and HS are distinct entities well-recognized by World Health Organization classification of tumors of hematopoietic and lymphoid tissue. In contrast to commonly held notions, IDCs and histiocytes have plasticity based on the well-documented trans-differentiation to IDCS and HS from follicular lymphoma [12], chronic lymphocytic leukemia/small lymphocytic lymphoma [13], mantle cell lymphoma [14], and even precursor B-lymphoblasts [15]. As further reported by Chen and associates, the presence of high frequency of clonal immunoglobulin receptor gene rearrangements in sporadic histiocytic/dendritic cell sarcomas suggests that a large subset of histiocytic/dendritic cell sarcomas have inherited B-cell genotypes [16]. Despite the reported trans-differentiation to histiocytic/dendritic cell sarcoma from mature and immature B-cell lymphoma/leukemia [11-15], trans-differentiation/de-differentiation to HS from IDCS has never been reported before, thus this is likely the first of such a case. Of note, due to the nature of the core needle biopsy, sampling bias cannot be completely eliminated from the original FNA and core needle biopsied specimen. In addition, there was no evidence of B-cell lymphoma or a history of B-cell lymphoma in the patient.
From a cytological point of view, diagnosis of IDCS on FNA and core needle biopsy is difficult but not impossible. Besides detailed and accurate cytohistologic examination along with judicial immunohistochemical characterization in all possible circumstances, the key for such a diagnosis is the high level of suspicion. The differential diagnosis for large atypical cells in the background of inflammatory cells based on the pure morphologic ground includes but is not limited to IDCS, HS, follicular dendritic cell sarcoma, classical Hodgkin lymphoma, large B-cell lymphoma, anaplastic large T-cell lymphoma, metastatic melanoma, metastatic carcinoma, and spindle cell sarcoma. Thus, a multi-modality approach combining cytohistomorphology, flow cytometry, and immunohistochemistry is the key to ensuring an accurate diagnosis.
HS can occur in nodal and extra-nodal sites including skin, soft tissue and gastrointestinal tract. Among 14 well-studied HS cases, 36% (5/14) were found in gastrointestinal tract [17]. Due to presence of bi-nucleated and even giant tumor cells and universally presence of background inflammatory cells, classical Hodgkin lymphoma, large B-cell lymphoma, metastatic carcinoma and melanoma all should be ruled out.
Of interest, S100 is consistently expressed in IDCS, but only expressed in approximately 50% of HS [17]. If a co-existing HS can be excluded from the initial core needle biopsy/FNA specimen, and if the HS were truly derived from the IDCS, then the exact reason why HS showed no S100 immunoreactivity is not known. We can only speculate that immunophenotypical evolution and/or effect of chemotherapy could play a role. Since there was no material left from the initial core needle biopsy, further parallel testing such as molecular/genetic studies using both the initial core needle biopsy and subsequent excisional specimen could not be conducted. Furthermore, there are no reported recurrent gene mutations or chromosomal translocations in IDCS and HS.
Due to rarity of the IDCS and HS, no standard chemotherapy was available. Recently, complete and major responses were achieved with alemtuzumab (anti-CD52 antibody) as a single agent in 2 patients with refractory HS, respectively [18]. Given the partial response to chemotherapy in our patient, the clinical team elected to continue with additional cycles of CHOP chemotherapy and monitor the disease response.
Disclosure of conflict of interest
The authors report no conflicts of interest.
References
- 1.Liu K, Nussenzweig MC. Origin and development of dendritic cells. Immunol Rev. 2010;234:45–54. doi: 10.1111/j.0105-2896.2009.00879.x. [DOI] [PubMed] [Google Scholar]
- 2.Pileri SA, Grogan TM, Harris NL, Banks P, Campo E, Chan JK, Favera RD, Delsol G, De Wolf-Peeters C, Falini B, Gascoyne RD, Gaulard P, Gatter KC, Isaacson PG, Jaffe ES, Kluin P, Knowles DM, Mason DY, Mori S, Muller-Hermelink HK, Piris MA, Ralfkiaer E, Stein H, Su IJ, Warnke RA, Weiss LM. Tumours of histiocytes and accessory dendritic cells: an immunohistochemical approach to classification from the International Lymphoma Study Group based on 61 cases. Histopathology. 2002;41:1–29. doi: 10.1046/j.1365-2559.2002.01418.x. [DOI] [PubMed] [Google Scholar]
- 3.Tew JG, Thorbecke GJ, Steinman RM. Dendritic cells in the immune response: characteristics and recommended nomenclature (A report from the Reticuloendothelial Society Committee on Nomenclature) J Reticuloendothel Soc. 1982;31:371–380. [PubMed] [Google Scholar]
- 4.Geissmann F, Manz MG, Jung S, Sieweke MH, Merad M, Ley K. Development of monocytes, macrophages, and dendritic cells. Science. 2010;327:656–661. doi: 10.1126/science.1178331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakamura S, Koshikawa T, Kitoh K, Nakayama A, Yamakawa M, Imai Y, Ishii K, Fujita M, Suchi T. Interdigitating cell sarcoma: a morphologic and immunologic study of lymph node lesions in four cases. Pathol Int. 1994;44:374–386. doi: 10.1111/j.1440-1827.1994.tb02938.x. [DOI] [PubMed] [Google Scholar]
- 6.Banner B, Beauchamp ML, Liepman M, Woda BA. Interdigitating reticulum-cell sarcoma of the intestine: a case report and review of the literature. Diagn Cytopathol. 1997;17:216–222. doi: 10.1002/(sici)1097-0339(199709)17:3<216::aid-dc10>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 7.Yang GC, Besanceney CE, Tam W. Histiocytic sarcoma with interdigitating dendritic cell differentiation: a case report with fine needle aspiration cytology and review of literature. Diagn Cytopathol. 2010;38:351–356. doi: 10.1002/dc.21215. [DOI] [PubMed] [Google Scholar]
- 8.Jaffe RA, Pileri SA, Facchetti F, Jones DM, Jaffe ES. Histiocytic and dendritic cell neoplasms. In: Swerdlow SH, editor. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. Lyon: International Agency for Research on Cancer; 2008. pp. 354–355. [Google Scholar]
- 9.Porter DW, Gupte GL, Brown RM, Spray C, English MW, deVille DeGoyet J, McKiernan PJ. Histiocytic sarcoma with interdigitating dendritic cell differentiation. J Pediatr Hematol Oncol. 2004;26:827–830. [PubMed] [Google Scholar]
- 10.Grogan TM, Pileri SA, Chan JKC, Weiss LM, Fletcher CDM. Histiocytic sarcoma. In: Swerdlow SH, editor. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. Lyon: International Agency for Research on Cancer; 2008. pp. 356–357. [Google Scholar]
- 11.Weiss LM, Grogan TM, Chan JKC. Interdigitating dendritic cell sarcoma. In: Swerdlow SH, editor. WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. Lyon: International Agency for Research on Cancer; 2008. pp. 361–362. [Google Scholar]
- 12.Feldman AL, Arber DA, Pittaluga S, Martinez A, Burke JS, Raffeld M, Camos M, Warnke R, Jaffe ES. Clonally related follicular lymphomas and histiocytic/dendritic cell sarcomas: evidence for transdifferentiation of the follicular lymphoma clone. Blood. 2008;111:5433–5439. doi: 10.1182/blood-2007-11-124792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shao H, Xi L, Raffeld M, Feldman AL, Ketterling RP, Knudson R, Rodriguez-Canales J, Hanson J, Pittaluga S, Jaffe ES. Clonally related histiocytic/dendritic cell sarcoma and chronic lymphocytic leukemia/small lymphocytic lymphoma: a study of seven cases. Mod Pathol. 2011;24:1421–1432. doi: 10.1038/modpathol.2011.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hure MC, Elco CP, Ward D, Hutchinson L, Meng X, Dorfman DM, Yu H. Histiocytic sarcoma arising from clonally related mantle cell lymphoma. J. Clin. Oncol. 2012;30:e49–53. doi: 10.1200/JCO.2011.38.8553. [DOI] [PubMed] [Google Scholar]
- 15.Kumar R, Khan SP, Joshi DD, Shaw GR, Ketterling RP, Feldman AL. Pediatric histiocytic sarcoma clonally related to precursor B-cell acute lymphoblastic leukemia with homozygous deletion of CDKN2A encoding p16INK4A. Pediatr Blood Cancer. 2011;56:307–310. doi: 10.1002/pbc.22810. [DOI] [PubMed] [Google Scholar]
- 16.Chen W, Lau SK, Fong D, Wang J, Wang E, Arber DA, Weiss LM, Huang Q. High frequency of clonal immunoglobulin receptor gene rearrangements in sporadic histiocytic/dendritic cell sarcoma. Am J Surg Pathol. 2009;33:863–873. doi: 10.1097/PAS.0b013e31819287b8. [DOI] [PubMed] [Google Scholar]
- 17.Hornick JL, Jaffe ES, Fletcher CD. Extranodal histiocytic sarcoma: clinicopathologic analysis of 14 cases of a rare epithelioid malignancy. Am J Surg Pathol. 2004;28:1133–1144. doi: 10.1097/01.pas.0000131541.95394.23. [DOI] [PubMed] [Google Scholar]
- 18.Shukla N, Kobos R, Renaud T, Teruya-Feldstein J, Price A, McAllister-Lucas L, Steinherz P. Successful treatment of refractory metastatic histiocytic sarcoma with alemtuzumab. Cancer. 2012;118:3719–3724. doi: 10.1002/cncr.26712. [DOI] [PubMed] [Google Scholar]


