Abstract
Alveolar rhabdomyosarcoma (ARMS) is remarkably rare in adults older than 45 years. Histologically, the tumor is composed of blue round cells with frequent expression of CD56 in addition to myogenic markers. Recent studies of ARMS have shown two specific recurrent translocations: PAX3-FKHR [t(2;13)(q35;q14)] or PAX7-FKHR [t(1;13)(p36;q14)]. Extranodal natural killer (NK)/T-cell lymphoma (ENKTL) occurs most frequently in the upper aerodigestive tract with a male preference in East Asia and Central and South Americas with neoplastic cells frequently expressing CD56. We report a 53-year-old Taiwanese man presenting with a nasopharyngeal mass, cervical lymphadenopathy, and multiple bone metastases. Histologically, the nasopharyngeal biopsy revealed diffuse sheets of small blue round tumor cells without obvious alveolar pattern, angioinvasion or tumor necrosis. An initial erroneous diagnosis of ENKTL was made due to CD56 expression using fresh tumor tissue with flow cytometric analysis and the patient was treated accordingly. Retrospective study showed that the tumor cells expressed CD56, desmin, and myogenin. Fluorescence in situ hybridization revealed that the tumor cells were positive for FKHR gene rearrangement, confirming the diagnosis of ARMS. Our case illustrates that a diagnosis of ENKTL based solely on CD56 expression can be misleading for a nasopharyngeal small blue round cell tumor. ARMS should be included as a differential diagnosis, and a correct diagnosis can be reached only after a high index of suspicion and a thorough histological examination with the aid of ancillary studies.
Keywords: Alveolar rhabdomyosarcoma, CD56, extranodal natural killer/T-cell lymphoma, flow cytometry, rhabdomyosarcoma
Introduction
Rhabdomyosarcoma (RMS) is a malignant soft tissue tumor of myogenic lineage, more common in childhood [1]. It is remarkably rare in adults older than 45 years, making up less than 1% of all adult malignancies and about 3% of all soft tissue sarcomas with head and neck region commonly affected. Alveolar (ARMS) and embryonal rhabdomyosarcoma (ERMS) represent the two main histologic patterns. The diagnosis of ARMS is made by a combination of histopathology, immunohistochemistry and cytogenetic or fluorescence in situ hybridization (FISH) studies. The tumor cells in ARMS classically express both myogenin and myo-D1, which are both highly sensitive and specific. Cytogen-etic abnormalities such as PAX3-FKHR [t(2;13)(q35;q14)] or PAX7-FKHR [t(1;13)(p36;q14)] have been observed in most ARMS cases [2]. Recently, Bahrami et al demonstrated expression of neuroendocrine markers such as CD56 or synaptophysin in 30-40% of ARMS cases [3]. Extranodal natural killer (NK)/T cell lymphoma (ENKTL) occurs predominantly in the upper aerodigestive tract and more frequently affect adult males, with a median age in the sixth decade of life. ENKTL is most common in Asians and is strongly associated with Epstein-Barr virus (EBV) [4]. The neoplastic cells are universally associated with EBV by in situ hybridization and frequently express CD56. ARMS and ENKTL may sometimes share overlapping features of small blue round cell tumors and CD56 expression, and such tumors in the head and neck regions may pose a diagnostic challenge. Here we present our experience with such a case.
Case report
A 53-year-old Taiwanese male presented with left nasal obstruction and cervical masses. Both MRI and PET-CT scan showed a nasopharyngeal tumor involving skull base with lymphadenopathies in bilateral neck and multiple bony lesions. A nasopharyngeal carcinoma with nodal and bone metastases or a malignant lymphoma with bone marrow involvement was suspected clinically and radiologically. The patient underwent nasopharyngeal biopsy and a wedge of the fresh tissue was sent for flow cytometric analysis under the clinical suspicion of lymphoma. The flow cytometric immunophenotyping revealed a population of tumor cells with CD56-positive phenotype, while other lymphoid markers were all negative (Figure 1). Histologically, the nasopharyngeal biopsy showed a dense collection of discohesive blue round cells in solid sheets without angiocentric and/or angiodestructive pattern or geographical necrosis (Figure 1). Immunohistochemically, the tumor cells showed the same phenotypes as those in the flow cytometry, i.e., CD56 expression without CD3, CD20, or CD16 (Figure 1). Based on the CD56 expression, a diagnosis of ENKTL was rendered, although serum antibodies, viral load or in situ hybridization for EBV were not checked. Chemotherapy with ifosfamide, carboplatin and etoposide (ICE), a regimen for ENKTL, was initiated immediately after performing bone marrow biopsy. Bone marrow biopsy, however, disclosed a diffuse infiltration of small blue round cells with occasional eccentric nuclei and abundant eosinophilic cytoplasm arranged in an alveolar pattern. Immunohisto-chemically, the tumor cells expressed CD56 and desmin (Figure 2) but not leukocyte common antigen (LCA; CD45) or cytokeratin. The initial nasopharyngeal biopsy was retrospectively reviewed and additional immunostaining showed that the nasopharyngeal tumor expressed desmin and myogenin (Figure 1). FISH assay using dual color break apart probe (Abbott Molecular Inc., Des Plaines, IL) demonstrated FKHR gene rearrangement (Figure 2), confirming the diagnosis of ARMS. After the revision of the diagnosis, the treatment regimen was changed to VAC/IE (vincristine, doxorubicin, and cyclophosphamide, alternating with ifosfamide and etoposide), and the nasopharyngeal mass and cervical lymphadenopathies re-gressed accordingly. Unfortunately, a relapse at the cervical nodes and bone marrow were noted four months later. The patient was then treated with MAID (mesna, doxorubicin, ifosfamide and dacarbazine) and radiotherapy (2000 cGy in 5 fractions). After that, he was lost to follow-up.
Figure 1.
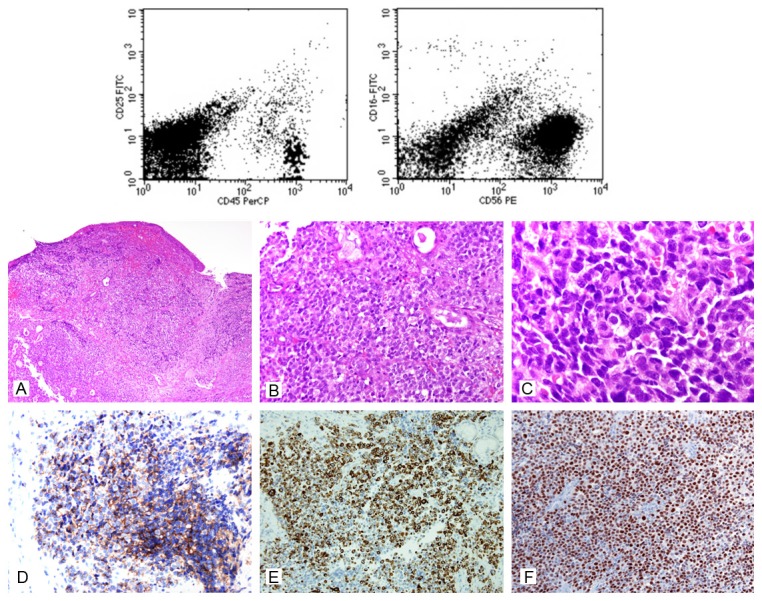
Nasopharyngeal biopsy. Flow cytometric immunophenotyping (the two panels in the first row) shows that the nasopharyngeal tumor cells express CD56, but not CD45 or CD16. Lower panels show mosaic images of nasopharyngeal ARMS. (A & B) A diffuse Infiltration around the submucosal glands (H&E, Magnification x 100 and x 400, respectively). (C) High-power view of the tumor cells showing round to oblong nuclei and scanty cytoplasm (H&E, 1,000 x). Immunohistochemically, the tumor cells express CD56 (D), desmin (E) and myogenin (F: immunohistochemical stains, all 200 x).
Figure 2.
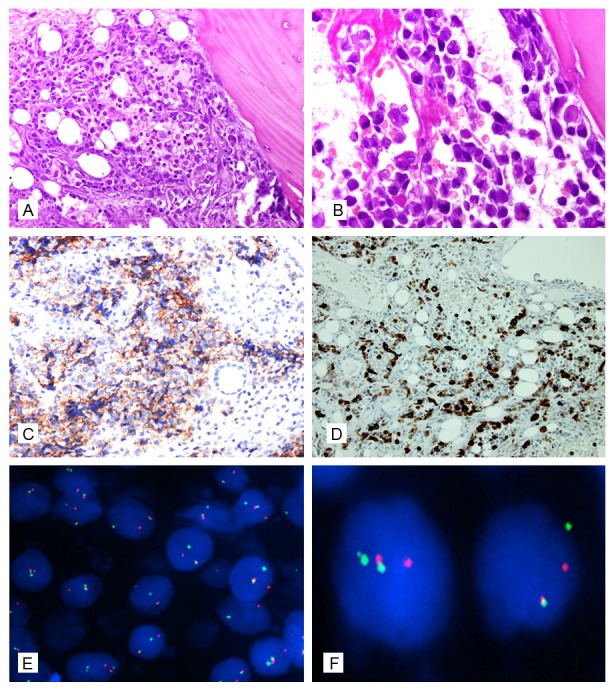
A-D: Bone marrow biopsy. A diffuse infiltration in the marrow by discohesive tumor cells with eccentric nuclei (A & B: H&E, x 400 and x 1,000, respectively). The tumor cells express CD56 (C: immunohistochemical stain, x 200) and desmin (D: 100 x). E and F: FISH on a section of the nasopharyngeal biopsy with FKHR (FOXO1) (13q14) dual color, break-apart probe sets reveals multiple split signals indicative of the disruption of the FOXO1 locus in >95% of the interphase cells analyzed.
Discussion
We present a rare case of disseminated nasopharyngeal ARMS and the detection of CD56-expression led to an erroneous diagnosis of ENKTL, which is prevalent in this geographic locale. Advances in flow cytometric immunophenotyping have greatly assisted the routine diagnosis of hematological malignancies as it is relatively simple, rapid, and efficient [6]. However, careful interpretation of the flow cytometric data and correlation with the histopathology are crucial for an accurate diagnosis. In our case, although the tumor cells expressed CD56, we should have been alerted by the CD45 negativity, which is unusual for ENKTL. Furthermore, we failed to recognize the recent finding that ARMS may express neuroendocrine markers, including CD56 [3,6,7]. And most importantly, we did not perform in situ hybridization for EBV, which is required for the diagnosis of ENKTL. In the end, the diagnosis of ARMS was reached only after the finding of a distinctive alveolar pattern in the marrow biopsy and was then confirmed with immunohistochemistry and FISH.
A valuable diagnostic adjunct in ARMS is the identification of translocations t(2;13)(q35;q14)/PAX3-FKHR and t(1;13) (p36;q14/PAX7- FKHR) in 55% and 22%, respectively [2,8]. In keeping with this, our case revealed FKHR gene rearrangement by FISH assay. Interestingly, there are a few case reports in the literature illustrating the diagnostic delays in patients whose ARMS mimicked a leukemia or lymphoma [9-11]. Recently Yasuda T et al. investigated 7 cases of ARMSs of head and neck regions in older adults with a median age of 61 years [7]. In that study, their initial diagnostic workup did not include myogenic markers due to an initial diagnostic impression of hematologic malignancy or neuroendocrine carcinoma. They concluded that establishing the diagnosis of ARMS in older adults was often neglected due to its rarity in this age group, lack of a characteristic alveolar pattern, and initially misleading immunoprofiles (CD56, cytokeratin, and synaptophysin immunoreactivity).
Clinically, rhabdomyosarcoma is one of the few soft tissue sarcomas with a known propensity for metastasis to the regional lymph nodes and bone marrow [12]. A clinical picture of disseminated rhabdomyosarcoma may mimic hematologic malignancies. In such a setting, establishing a precise diagnosis is important not only in determining how aggressive the tumor might be, but is particularly critical in administering an appropriate and timely management. Treatment of rhabdomyosarcoma usually invo-lves a combination of surgery, radiotherapy and chemotherapy. Multidisciplinary treatment of chemoradiotherapy following complete surgical resection may confer the most favorable treatment outcome [13-15]. On the other hand, chemotherapy is the main stream therapeutic management for lymphoma. In our patient, an appropriate therapy was hindered by the initial misdiagnosis but was immediately revised after the first course of chemotherapy.
In conclusion, pathologists should always include ARMS as a differential diagnosis when dealing with small round cell tumors in the head and neck regions, even in older adults. A correct diagnosis can then be reached by a carefully selected panel of immunohistochemical markers, cytogenetic and/or molecular studies, especially when a small blue round cell tumor is expressing CD56.
Disclosure of conflict of interest
No conflicts of interests declared.
References
- 1.Turner JH, Richmon JD. Head and neck rhabdomyosarcoma: a critical analysis of population-based incidence and survival data. Otolaryngol Head Neck Surg. 2011;145:967–973. doi: 10.1177/0194599811417063. [DOI] [PubMed] [Google Scholar]
- 2.Barr FG. Gene fusions involving PAX and FOX family members in alveolar rhabdomyosarcoma. Oncogene. 2001;20:5736–5746. doi: 10.1038/sj.onc.1204599. [DOI] [PubMed] [Google Scholar]
- 3.Bahrami A, Gown AM, Baird GS, Hicks MJ, Folpe AL. Aberrant expression of epithelial and neuroendocrine markers in alveolar rhabdomyosarcoma: a potentially serious diagnostic pitfall. Mod Pathol. 2008;21:795–806. doi: 10.1038/modpathol.2008.86. [DOI] [PubMed] [Google Scholar]
- 4.Wenig BM. Undifferentiated malignant neoplasms of the sinonasal tract. Arch Pathol Lab Med. 2009;133:699–712. doi: 10.5858/133.5.699. [DOI] [PubMed] [Google Scholar]
- 5.Liang R, Todd D, Chan TK, Chiu E, Choy D, Loke SL, Ho FC. Nasal lymphoma. A retrospective analysis of 60 cases. Cancer. 1990;66:2205–2209. doi: 10.1002/1097-0142(19901115)66:10<2205::aid-cncr2820661027>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 6.de Tute RM. Flow cytometry and its use in the diagnosis and management of mature lymphoid malignancies. Histopathology. 2011;58:90–105. doi: 10.1111/j.1365-2559.2010.03703.x. [DOI] [PubMed] [Google Scholar]
- 7.Yasuda T, Perry KD, Nelson M, Bui MM, Nasir A, Goldschmidt R, Gnepp DR, Bridge JA. Alveolar rhabdomyosarcoma of the head and neck region in older adults: genetic characterization and a review of the literature. Hum Pathol. 2009;40:341–348. doi: 10.1016/j.humpath.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turc-Carel C, Lizard-Nacol S, Justrabo E, Favrot M, Philip T, Tabone E. Consistent chromosomal translocation in alveolar rhabdomyosarcoma. Cancer Genet Cytogenet. 1986;19:361–362. doi: 10.1016/0165-4608(86)90069-5. [DOI] [PubMed] [Google Scholar]
- 9.Chen L, Shah HO, Lin JH. Alveolar rhabdomyosarcoma with concurrent metastases to bone marrow and lymph nodes simulating acute hematologic malignancy. J Pediatr Hematol Oncol. 2004;26:696–697. doi: 10.1097/01.mph.0000140654.50344.92. [DOI] [PubMed] [Google Scholar]
- 10.Tsai SC, Reale LD, Flomenberg N, Schwarting R, Enck RE. Alveolar rhabdomyosarcoma mimicking a lymphoma at presentation. J. Clin. Oncol. 2006;24:4031–4032. doi: 10.1200/JCO.2006.05.8917. [DOI] [PubMed] [Google Scholar]
- 11.Yamaguchi K, Koga Y, Suminoe A, Saito Y, Matsuzaki A, Kanno S, Takimoto T, Suda M, Oda Y, Muto T, Takatsuki H, Hara T. [Alveolar rhabdomyosarcoma of unknown origin mimicking acute leukemia at the initial presentation] . Rinsho Ketsueki. 2007;48:315–320. [PubMed] [Google Scholar]
- 12.Mazeron JJ, Suit HD. Lymph nodes as sites of metastases from sarcomas of soft tissue. Cancer. 1987;60:1800–1808. doi: 10.1002/1097-0142(19871015)60:8<1800::aid-cncr2820600822>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 13.Bonilla JA, Healy GB. Management of malignant head and neck tumors in children. Pediatr Clin North Am. 1989;36:1443–1450. doi: 10.1016/s0031-3955(16)36799-2. [DOI] [PubMed] [Google Scholar]
- 14.Kraus DH, Saenz NC, Gollamudi S, Heller G, Moustakis M, Gardiner S, Gerald WL, Ghavimi F, LaQuaglia MP. Pediatric rhabdomyosarcoma of the head and neck. Am J Surg. 1997;174:556–560. doi: 10.1016/s0002-9610(97)00171-2. [DOI] [PubMed] [Google Scholar]
- 15.Wurm J, Constantinidis J, Grabenbauer GG, Iro H. Rhabdomyosarcomas of the nose and paranasal sinuses: treatment results in 15 cases. Otolaryngol Head Neck Surg. 2005;133:42–50. doi: 10.1016/j.otohns.2005.03.023. [DOI] [PubMed] [Google Scholar]


