Abstract
The aim of this study was to investigate the odontogenic differentiation of human dental pulp stem cells (DPSCs) on nanofibrous (NF) poly(L-lactic acid) (PLLA) scaffolds in vitro and in vivo. Highly porous NF-PLLA scaffolds which mimic the architecture of collagen type I (Col I) fibers were fabricated by the combination of a phase separation technique and a porogen leaching method. The human DPSCs were then seeded onto the scaffolds and cultured in different media for odontogenic differentiation: “Control” medium without supplements; “DXM” medium containing 10−8 M dexamethasone (DXM), 50 μg/mL ascorbic acid and 5 mM β-glycerophosphate; “BMP-7 + DXM” medium containing 10−8 M DXM, 50 μg/mL ascorbic acid, 5 mM β-glycerophosphate plus 50 ng/mL bone morphogenetic protein 7 (BMP-7). For odontogenic differentiation study in vitro, alkaline phosphatase (ALP) activity quantification, reverse transcription polymerase chain reaction (RT-PCR), scanning electron microscopy (SEM), von Kossa staining and calcium content quantification were carried out. While both “DXM” medium and “BMP-7+DXM” medium induced the DPSCs to odontoblast-like cells, the “BMP-7 + DXM” medium had greater inducing capacity than the “DXM” medium. Consistent with the in vitro studies, “BMP-7 + DXM” group presented more extracellular matrix (ECM) and hard tissue formation than “DXM” group after 8 weeks of ectopic implantation in nude mice. Differentiation of DPSCs to odontoblast-like cells was identified by the positive immunohistochemical staining for dentin sialoprotein (DSP). In conclusion, odontogenic differentiation of DPSCs can be achieved on NF-PLLA scaffolds both in vitro and in vivo; the combination of BMP-7 and DXM induced the odontogenic differentiation more effectively than DXM alone. The NF-PLLA scaffold and the combined odontogenic inductive factors provide excellent environment for DPSCs to regenerate dental pulp and dentin.
Keywords: Dental pulp stem cells (DPSCs), Nanofibrous poly(L-lactic acid) (PLLA) scaffold, Odontogenic differentiation, Dentin regeneration, Bone morphogenetic protein 7 (BMP-7)
Introduction
Millions of people suffer from caries and pulpitis, which affect the quality of life of patients of all ages and result in economic burden on the healthcare systems worldwide [1]. The current therapy is to remove the lesions and to replace the dental tissues with synthetic materials, such as amalgam, resin and gutta-percha. However, these materials are incapable of replacing the biological function of the lost tissue, leading to reduced mechanical properties and reduced vitality of the teeth. In the long term, they may also affect the masticatory and digestive functions [2, 3].
A paradigm shift is taking place to apply tissue engineering techniques to repair or replace the impaired tissues. Similar to the construction of other tissues, the triad of dental pulp stem cells (DPSCs), morphogens including growth and differentiation factors, and scaffolds is needed for dental pulp tissue engineering [4–6]. Unlike embryonic stem cells, postnatal DPSCs are more ethically acceptable and can be easily acquired as a byproduct of routine tooth extraction treatment. Additionally, previous studies have shown that DPSCs have clonogenic abilities, rapid proliferative rates and multiple differentiation potentials [7, 8], providing a suitable cell source for tooth tissue engineering.
The scaffold plays a critical role in tooth tissue engineering and its performance could benefit from imitating the characteristics of the natural extracellular matrix (ECM) [9]. Collagen type I (Col I), which has a fibrous structure on the nanometer scale, is the most abundant extracellular protein in dentin and the base for primary and reparative dentin formation [10]. Natural collagen has been used as scaffolds for tooth tissue engineering [11, 12]. However, there are concerns over the potential pathogen transmission, immune reactions and the poor mechanical properties. In our laboratory, a technology has been developed to fabricate nanofibrous (NF) poly(L-lactic acid) (PLLA) scaffolds with well-interconnected macropores and good mechanical properties. This scaffold mimics the physical architecture of Col I with fiber diameter ranging from 50–500 nm, and the macroporous structure promotes cell migration and tissue ingrowth [13–15]. Our previous studies have shown encouraging results of NF-PLLA scaffolds in bone tissue engineering [16–21]. Since bone and dentin share similar components, this scaffold was selected for dentin tissue engineering in this study.
Another important component of tissue engineering is the inductive factors. BMP-7 has shown its benefits in treating a variety of bone-related diseases [22, 23]. Previous studies found that different species responded differently to BMPs for bone formation [24, 25]. In the dental field, although BMP-7 has shown encouraging results as a pulp-capping agent in animal experiments [26, 27], the effect of BMP-7 on the odontogenic differentiation of human DPSCs has not been reported before. It is crucial to evaluate the response of human DPSCs to BMP-7 to predict their potential in tooth tissue engineering. Dexamethasone (DXM) has been shown in many experiments to induce odontoblast differentiation of DPSCs [28–30]. Previous studies have showed that the combination of different inductive factors could enhance osteogenic and odontogenic differentiation [31–33]. We hypothesized that the combination of BMP-7 and DXM could more effectively induce the odontogenic differentiation of human DPSCs than DXM alone. The aims of this study were to (1) evaluate whether NF-PLLA scaffolds support the proliferation and odontogenic differentiation of human DPSCs, and (2) determine if BMP-7 combined with DXM more efficiently induces odontogenic differentiation of human DPSCs both in vitro and in vivo than DXM alone.
Materials and Methods
Preparation of NF- PLLA scaffolds
PLLA with an inherent viscosity of approximately 1.6 dl/g was purchased from Boehringer Ingelheim (Ingelheim, Germany). The scaffold preparation method has been previously reported [15]. Briefly, PLLA was dissolved in 4/1 (v/v) dioxane/methanol solvent mixture and was cast onto a paraffin sphere assembly. The polymer/paraffin composite was phase separated at −80°C overnight. Hexane was used for solvent extraction and paraffin leaching for a total of 4 days. Hexane in the scaffolds was then exchanged with cyclohexane. The polymer scaffolds were freeze-dried and cut into disks 5.2 mm in diameter and 1.5 mm in thickness. The scaffolds were sterilized with ethylene oxide at least 48 hrs before cell seeding procedure.
Cell culture and cell seeding
Human DPSCs were obtained from the Center of Craniofacial Molecular Biology, School of Dentistry, University of Southern California [8]. The thawed DPSCs were cultured in ascorbic acid-free α-modified essential medium (α-MEM) (GIBCO, Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (FBS) (Invitrogen) and 1% penicillin–streptomycin (Invitrogen) in a humidified incubator at 37°C with 5% CO2. The medium was changed every two days. DPSCs of passages 3–6 were used in the following studies.
The NF-PLLA scaffolds were soaked in 70% ethanol for 30 min to improve wetting and a vacuum pump was used to remove the air bubbles from the scaffolds. Then the scaffolds were washed with phosphate-buffered saline (PBS) (Invitrogen) for three times (30 min each) to remove the residual ethanol. After that, the scaffolds were washed twice with α-MEM containing 10% FBS (2 hours each). 1×106 human DPSCs were seeded onto each scaffold. The cell-scaffold constructs were cultured in α-MEM supplemented with 10% FBS for 24 hours, and then transferred to 12-well plates containing 2 mL medium in each well. The media used in the study were listed below: “Control” medium containing α-MEM supplemented with 10% FBS without supplements; “DXM” medium containing α-MEM supplemented with 10% FBS, 50 μg/mL ascorbic acid, 5 mM β-glycerophosphate, and 10−8 M dexamethasone (DXM); “BMP-7 + DXM” medium containing α-MEM supplemented with 10% FBS, 50 μg/mL ascorbic acid, 5 mM β-glycerophosphate, 10−8 M DXM plus 50 ng/mL BMP-7 (kindly provided by Stryker Biotech, Hopkinton, MA, USA). All the groups were cultured on an orbital shaker in an incubator at 37°C with 5% CO2.
DNA assay
To determine the proliferation of DPSCs on the NF-PLLA scaffold, the cell-scaffold constructs were homogenized in 1 mL 1× DNA assay buffer (Sigma, St. Louis, MO, USA) using a Polytron homogenizer (Brinkmann Easycare Generator, Polytron-Aggregate, Switzerland). 1 mL cell lysis buffer was added and the samples were incubated at 37°C for 1 hour. The cells lysis was spun down at 5000 g for 5 min. Total DNA was quantified using fluorescence assay with Hoechst 33258 dye according to the manual (Sigma).
Scanning electron microscopy (SEM) observation
The cell-scaffold constructs harvested at different time points were rinsed in PBS followed by fixation in 2.5% glutaraldehyde for 24 hours, then post-fixed in 1% osmium tetroxide for 1 hour. Samples were then dehydrated in a series of increasing concentrations of ethanol and hexamethyldisilizane (HMDS). The samples were then sputter-coated with gold using a sputter coater (Desk-II, Denton Vacuum Inc., Moorstown, NJ, USA) and observed under an SEM (Philips XL30 FEG) at 10 kV. The elemental contents on the surface of the scaffolds were measured by energy dispersive x-ray microanalysis (EDX) (Phoenix XEDS system).
Alkaline phosphatase (ALP) activity quantification
ALP activity was detected using SensoLyte™ pNPP Alkaline Phosphatase Assay Kit (AnaSpec, CA, USA) according to the manufacturer’s protocol. Briefly, cells on the scaffold were homogenized in 1 mL lysis buffer supplied with the kit. Lyses were centrifuged at 10000 g and 4°C for 15 min. Supernatant was collected for ALP assay using p-nitrophenyl phosphate as a phosphatase substrate and alkaline phosphatase supplied by the kit as a standard. The absorbance was measured at 405 nm and the amount of ALP in the cells was normalized against total protein content.
Reverse transcription polymerase chain reaction (RT-PCR)
The total RNA was extracted using Trizol (Invitrogen) and the first-strand cDNA was reverse transcribed with TaqMan reverse transcription reagents (Applied Biosystems, Foster City, CA, USA) from each sample. The sequences of the specific primer sets are listed below: ALP (sense 5′-ACGTGGCTAAGAATGTCATC-3′; antisense 5′-CTGGTAGGCGATGTCCTTA-3′); dentin matrix protein 1 (DMP-1) (sense 5′-TGGGGATTATCCTGTGCTCT-3′; antisense 5′-TACTTCTGGGGTCACTGTCG-3′); dentin sialophosphoprotein (DSPP) (sense 5′-AATGGGACTAAGGAAGCTG-3′; 5′-AAGAAGCATCTCCTCGGC-3′); osteocalcin (OCN) (sense 5′-CATGAGAGCCCTCACA-3′; antisense 5′-AGAGCGACACCCTAGAC-3′); glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (sense 5′-AGCCGCATCTTCTTTTGCGTC-3′; antisense 5′-TCATATTTGGCAGGTTTTTCT-3′). PCR was carried out using 2720 Thermal Cycler (Applied Biosystems) and the conditions for PCR were as follows: 94°C (30 sec), 56°C (30 sec), and 72°C (60 sec) for 35 cycles, with a final 10 min extension at 72°C. The PCR products were separated by electrophoresis on a 1.5% agarose gel and were visualized by ultraviolet-induced fluorescence.
Von Kossa staining and calcium content quantification
After 6 weeks of culture, the cell-scaffold constructs were rinsed with PBS, and then fixed with 10% (w/v) formalin. Von Kossa Method for Calcium Kit (Polysciences, Germany) was used to stain calcium deposits according to the manual. For calcium content quantification, the constructs were washed three times for 5 min each in distilled water and then homogenized in 400 μL 1 N hydrochloric acid. The lyses were incubated overnight to extract calcium. The total calcium content of each construct was determined by o-cresolphthaleincomplexone method following the manufacturer’s instructions (Calcium LiquiColor, Stanbio Laboratory, Boerne, TX, USA).
Subcutaneous implantation
The animal surgical procedure was approved by the University Committee on Use and Care of Animals (UCUCA) of the University of Michigan. Six immunocompromised nude mice (nu/nu, Charles River Laboratories) were used for implantation. Surgery was performed under general inhalation anesthesia with isofluorane. The back of the animals was shaved, washed and disinfected with povidoneiodine. One midsagittal incision was made on the dorsa and two subcutaneous pockets were created using blunt dissection. The cell-scaffold constructs were induced in different inductive media (control medium, DXM medium or BMP-7+DXM medium) for 2 weeks before subcutaneous implantation. Four samples were implanted for each group (n = 4), where each mouse received two implants at random. After placement of scaffolds, the incisions were closed with staples. Animals were euthanized and samples were retrieved after 8 weeks of transplantation. Harvested specimens were immediately fixed in 10% (w/v) formalin for 24 hours, and then processed for histological observation by hematoxylin-eosin (H-E) staining, von Kossa staining and Masson’s trichrome staining. For immunohistochemical analysis, 5-μm thick paraffin-embedded sections were deparaffinized using xylene and ethanol, and were reacted with primary dentin sialoprotein (DSP) antibody (1:100 dilution) (Santa Cruz Biotechnology, Santa Cruz, CA, USA). A Cell and Tissue Staining Kit, HRP-AEC System (R&D Systems, Minneapolis, MN, USA), was used according to the manufacturer’s instructions.
Statistical Analysis
Data were reported with the means ± standard deviations (n=3). Statistical analysis was carried out using Student’s t-test for differences among groups and a value of p<0.05 was considered to be statistically significant.
Results
Preparation of cells and NF-PLLA scaffolds
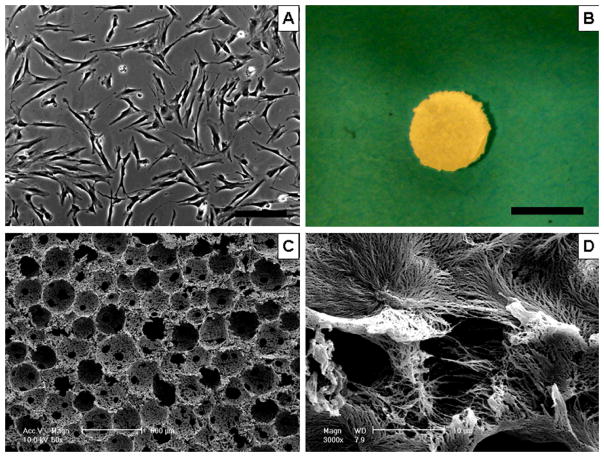
During cell culture, most of the DPSCs exhibited a spindle-like shape with extending cytoplasmic processes. The rate of cell division and cell morphology remained stable for 10 passages and DPSCs of passages 3–6 (Figure 1A) were used for the current studies. NF-PLLA scaffolds with well-defined macroporous structure were created by combining phase separation and porogen leaching methods. The scaffolds were cut into circular disks 5.2 mm in diameter and 1.5 mm in thickness (Figure 1B). The typical macroporous structure and nanofibrous architecture were observed using SEM (Figure 1C, 1D). The diameter of the nanofibers ranged from 50 to 500 nm, which is the same as that of natural collagen fiber bundles. The size of macropores ranged from 250 to 420 μm.
Fig. 1.
Cells and scaffold used in the study. (A) Micrographic view of DPSCs (Passage 3) cultured on 2D dishes (magnification 20×). (B) Gross view of the NF-PLLA scaffold (diameter: 5.2 mm; thickness: 1.5 mm). (C) SEM view of NF-PLLA scaffold at a low magnification. (D) SEM view of NF-PLLA scaffold at a high magnification. Scale bar in A represents 200 μm; scale bar in B represents 5 mm.
Cell attachment and proliferation
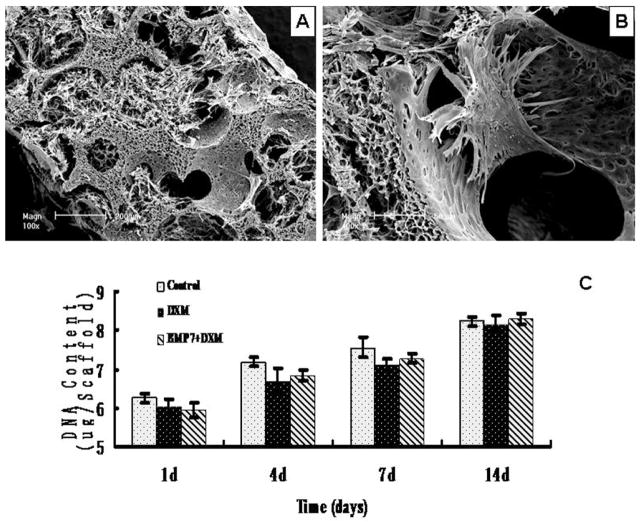
Three days after cell seeding, the SEM images showed that the DPSCs attached and fully spread on the surfaces of the NF-PLLA scaffolds. The interconnected macro pores in the scaffold were filled with cells, which had long cell processes and secreted abundant ECM (Fig. 2A–B).
Fig. 2.
(A) SEM observation of NF-PLLA scaffolds loaded with DPSCs cultured in vitro for 3 days at a low magnification. The interconnected macro pores in the scaffold were filled with DPSCs, which had long cell processes and secreted abundant ECM. (B) SEM observation of NF-PLLA scaffolds loaded with DPSCs cultured in vitro for 3 days at a higher magnification. The DPSCs attached and fully spread on the pore surfaces of the NF-PLLA scaffolds. (C) The proliferation characteristics of DPSCs cultured on NF-PLLA scaffolds in different media.
The DNA assay revealed that there was no significant difference in cell proliferation among the three groups at different time intervals (Fig. 2C). Addition of BMP-7 and DXM did not significantly affect the proliferation of human DPSCs from day 1 to days 14.
In vitro differentiation
The ALP activity gradually increased in all three groups and peaked at 3 weeks, after which the activity decreased in all three groups. “BMP-7 + DXM” group always showed significantly higher ALP levels compared to the other two groups, with the exception of being not statistically different between “BMP-7 + DXM” group and “DXM” group at 4 weeks (Fig. 3).
Fig. 3.
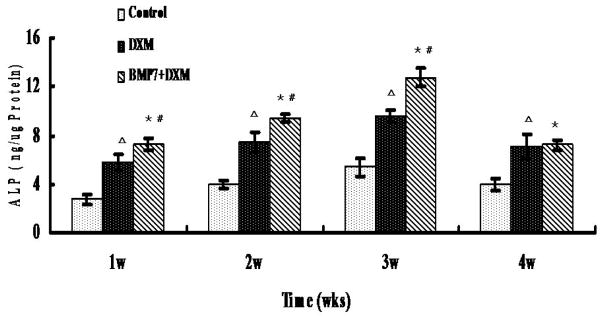
ALP activity quantification of DPSCs cultured on NF-PLLA scaffolds in different media. The bars represent means ± SD (n = 3). “BMP-7 + DXM” group compared to control group: *p<0.05; “BMP-7 + DXM” group compared to “DXM” group: #p<0.05; “DXM” group compared to control group: Δp<0.05.
Expressions of marker genes for odontogenic differentiation (ALP, OCN, DSPP and DMP-1) were examined using RT-PCR among the three groups (Fig. 4). More abundant ALP gene expression was detected in “BMP-7 + DXM” group compared to the DXM alone and control groups at 2 weeks of culture, and then the expression level decreased at 4 weeks of culture. OCN, DSPP and DMP-1 transcripts were detected at 2 weeks in both “BMP-7+DXM” and “DXM” media and the expressions increased at 4 weeks of culture. The most noticeable were that “BMP-7+DXM” group always showed more abundant expressions of OCN, DSPP and DMP-1 compared to “DXM” group at all time points studied. In the control group, gene expression levels of OCN and DSPP remained low at 4 weeks of culture time.
Fig. 4.

RT-PCR: Gene expression of human dental pulp stem cells grown on the NF-PLLA scaffolds for 2 and 4 weeks. The “BMP-7+DXM” group always showed more abundant expressions of ALP, OCN, DSPP and DMP-1 compared to “DXM” group at all time points with the exception of no significant difference in ALP activity between “BMP-7 + DXM” group and “DXM” group at 4 weeks.
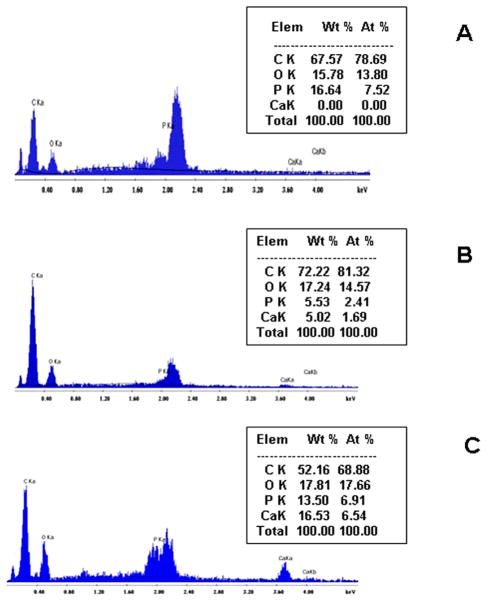
After 4 weeks of culture, the calcium deposits were verified by energy dispersive x-ray microanalysis. There was a higher calcium content (16.53%) in the “BMP-7+DXM” group than in the “DXM” group (5.02%) (Fig. 5B&C), and there was minimal calcium deposition in the control group (Fig. 5A).
Fig. 5.
Energy dispersive x-ray microanalysis of cell-scaffold constructs cultured in different media in vitro for 4 weeks: (A) control group; (B) “DXM” group; (C) “BMP-7 + DXM” group.
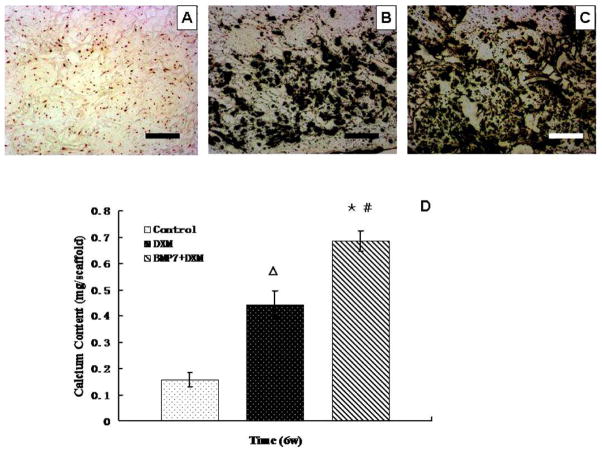
Von Kossa staining also revealed more mineral deposition in the “BMP-7+DXM” group than in the “DXM” alone group after 6 weeks of culture, while calcium deposition was minimal in the control group (Fig. 6A–C). This was further confirmed by calcium content assay, which demonstrated 50% greater amount of calcium deposition in the “BMP-7+DXM” group than in the “DXM” alone group (Fig. 6D). A small amount of calcium could also be detected in the control group without odontogenic supplements.
Fig. 6.
von Kossa staining views of DPSCs on NF-PLLA scaffolds cultured for 6 weeks in vitro (dark color indicates mineral nodules): (A) control group; (B) “DXM” group; (C) “BMP-7 + DXM” group. (D) Calcium content quantification of DPSCs on NF-PLLA scaffolds cultured for 6 weeks in vitro. The bars represent means ± SD (n = 3). “BMP-7 + DXM” group compared to control group: *p<0.05; “BMP-7 + DXM” group compared to “DXM” group: #p<0.05; “DXM” group compared to control group: Δp<0.05. Scale bars represent 100 μm. Original magnification: ×20.
In vivo study
Samples were retrieved after 8 weeks of subcutaneous implantation in nude mice. Macroscopic observation indicated that all specimens were surrounded by vascularized thin fibrous connective tissue. The H-E staining illustrated that the cells grew into the macropores of the scaffolds in all groups (Fig. 7A, B, C). The mineral, organic matrix (collagen) and immunohistochemical (DSP) stainings were minimal in the control group (Fig. 7D, G, J). In “DXM” group, relative smaller amounts of disorganized granule-like mineral deposits and organic matrix (Fig. 7E and H) were observed compared to “BMP-7+DXM” group (Fig. 7F and I). DSP secretion was demonstrated by positive immunohistochemical staining in both “DXM” and “BMP-7+DXM” groups (Fig. 7 K, L). Overall, more odontoblast-like cells and a thicker collagen-like matrix were found in a more organized form in “BMP-7+DXM” group. The collagen fibers, DSP and mineral nodules were co-located adjacent to the wall surface of the interconnected pores. Blood vessel invasion was also observed inside the pores of the scaffolds. These results indicate that the neo tissue organization in the “BMP-7+DXM” group was more similar to that of dentin than in other groups.
Fig. 7.
Cell-scaffold constructs implanted in vivo for 8 weeks: (A) Control group (H-E staining); (B) “DXM” group (H-E staining); (C) “BMP-7 + DXM” group (H-E staining). The arrow points to the orderly array of the cells on the surface of the interconnected pores. (D) Control group (von Kossa staining); (E) “DXM” group (von Kossa staining); (F) “BMP-7 + DXM” group (von Kossa staining). The arrow indicated hard tissue formation on the scaffold; (G) Control group (Masson’s trichrome staining: blue color indicates collagen and red color indicates cells); (H) “DXM” group (Masson’s trichrome staining); (I) “BMP-7 + DXM” group (Masson’s trichrome staining). The arrow points to a thicker collagen-like matrix in a more organized form along the surface of the interconnected pores; (J) Control group (immunohistochemical staining for DSP); (K) “DXM” group (immunohistochemical staining for DSP); (L) “BMP-7 + DXM” group (immunohistochemical staining for DSP). The arrow points to the positive staining of DSP arranged along the pore surfaces. Scale bars represent 100 μm. Original magnification: ×20.
Discussion
Dentin-pulp complex as the main component of the tooth plays a crucial role in maintaining tooth health. Serious stimuli such as attrition, trauma, or caries may lead to the inflammation or even death of the pulp. Traditional restorative materials can not completely restore the normal structure and function of the lost dental tissue and are incapable of repairing the tissue exposed to harmful stimuli [34]. Recent progress in tissue engineering technology has led to a growing interest in the development of regenerative dentin-pulp structure, which could provide natural replacement or repair of damaged tooth tissues [5]. The three key ingredients for successful tissue engineering are the seeded cells, the scaffold and the morphogens. In the current study, human DPSCs, nanofibrous PLLA scaffolds combined with different odontogenic inducers were applied for dental tissue engineering. The selected stem cells should have the capacity to differentiate to the desired lineage for their successful application in dental tissue engineering. Previous studies have indicated that DPSCs could differentiate into various specialized cell types [7]. In the present study, after being cultured in odontogenic media for 4–8 weeks DPSCs differentiated into odontoblast-like cells and led to dentin-like tissue formation both in vitro and in vivo, which is consistent with the previous publifications [30, 33].
The scaffold also plays a vital role in successful tissue engineering. The natural ECM has nano-sized structural features and a scaffold for tissue engineering may benefit from mimicking such features to enhance cell attachment, proliferation, migration, differentiation and neo tissue genesis [9]. Various scaffolds have been applied in the dental tissue engineering, but none of them is ideal. For example, hydroxyapatite (HA) has good biocompatibility and osteoconductivity, and therefore has been widely studied in dental tissue engineering [7, 8, 30, 33, 35]. However, HA has poor processability into highly porous structures and is often brittle. Collagen, which is the main component of many tissues, has also been used as a naturally derived scaffold in dental tissue engineering [11, 12]. However, there are concerns over the potential pathogen transmission, immune reactions and the poor mechanical properties of collagen. Polymers have great design flexibility because the composition and structure can be tailored to the specific needs, and therefore have been extensively studied in various tissue engineering applications, including tooth tissue engineering [36–38]. In our study, highly porous NF-PLLA scaffolds were developed using a phase-separation technique to mimic Col I fiber structure. By utilizing this fabrication process, we were able to control the architecture of the scaffolds including the macroscopic shape, the spherical pore size (250 – 420 μm) and the fiber diameter at the nano-size scale (50–500 nm) [8–10]. The nanofibrous architecture of the PLLA scaffolds has been previously shown to selectively enhance protein adsorption [18], which contributes to cell attachment. The highly interconnected pore structure of the NF-PLLA scaffolds was demonstrated to provide excellent environment for cell growth and angiogenesis [17, 18]. Such scaffolds showed superiority in osteogenic differentiation and bone tissue engineering over control scaffolds [16–20, 39]. Since bone and dental tissues share similar components, our hypothesis was that NF-PLLA scaffolds could also support the odontogenic differentiation of DSPSs and dental-like tissue formation. This was confirmed by our in vitro and in vivo results under odontogenic conditions. When seeded on NF-PLLA scaffolds, DPSCs grew very well and were effectively induced to odontogenic lineage. Moreover, the cells maintained their differentiated phenotype and formed hard tissue in vivo. In future studies, we will specifically evaluate if the NF-PLLA scaffolds are superior to other scaffolds (e.g., solid-walled PLLA scaffolds) for the odontogenic differentiation of DPSCs.
Another key element for the success of tissue engineering is the inductive factors. BMP-7 has been previously examined as a pulp-capping agent in monkeys, miniature swine and ferrets [27, 40, 41]. Dexamethasone is a glucocorticoid hormone and has been widely applied as a mineralization inducer for bone and dentin formation [8, 28, 35]. To the best of our knowledge, the effect of BMP-7 on the proliferation and odontogenic differentiation of human DPSCs has not been reported before, nor did the combination of BMP-7 and DXM. Our pilot study showed that BMP-7 at a high dosage significantly inhibited the proliferation of human DPSCs. Since high cell density plays an important role in cell communication and differentiation [42], it is crucial to choose the right dosage that most effectively enhances the odontogenic differentiation without inhibiting the proliferation of human DPSCs. Previous studies have showed that BMP-2 enhanced osteogenic differentiation of human MSCs and odontogenic differentiation of rat DPSCs [32, 33]. In the current study, BMP-7 at 50 ng/mL combined with 10−8 M DXM was used to induce odontogenic differentiation of the human DPSCs. Our data showed that the cell proliferation was not significantly affected by the selected BMP-7 dose for the differentiation of human DPSCs.
Our results showed that the “BMP-7 + DXM” group better supported odontogenic differentiation and hard tissue formation than the “DXM” alone group both in vitro and in vivo. For the in vitro study, ALP activity quantification, RT-PCR, SEM, von Kossa staining and calcium content quantification were carried out. ALP is usually regarded as an early marker of hard tissue formation. OCN, DSPP and DMP-1 were chosen as late markers for odontogenesis. OCN is usually regarded as a late marker for osteoblast differentiation and also plays an important role in dentin formation and regeneration [43]. DSPP and DMP-1 are regarded as the specific markers for odontoblasts [44, 45]. Mineralization is another key goal for dental regeneration. According to our results, “BMP-7 + DXM” group showed significantly higher ALP activity than the DXM alone group. The expression of OCN and DSPP, especially DSPP, demonstrated that cells cultured in “BMP-7 + DXM” medium had the greater ability to differentiate into odontoblasts. Consistently, more mineral modules were formed in the “BMP-7 + DXM” group than in the DXM alone group as revealed by von Kossa staining and confirmed by the calcium quantification. The energy dispersive x-ray microanalysis also demonstrated more calcified matrix deposition in “BMP-7 + DXM” group. It is clear that DXM alone induces substantially lower level of odontogenic differentiation of DPSCs than the combination of BMP-7 and DXM. However, we have not examined if BMP-7 alone induces lower extent of odontogenic differentiation than the combination of BMP-7 and DXM, which needs to be evaluated in future studies. Interestingly, human DPSCs could also express odontogenic markers in the control group although at a lower level. Such observations were also reported in other studies, which were believed to be a result of self-differentiation after a long-term in vitro culture [33, 35].
Although in vitro culture system offers a simplified model to investigate odontoblast development, the potential of this system for dental pulp tissue engineering needs to be verified in vivo. Our results showed that the pores of the scaffolds in all three groups were filled with connective tissue-like tissue with vascular ingrowth, which demonstrated that porous structure of NF-PLLA could facilitate cell seeding, nutritional exchange, tissue formation and angiogenesis. In the “BMP-7 + DXM” group, a more organized tissue was identified; calcium and collagen depositions were both located peripherally around the walls of the pores. In the same areas, strong positive immunohistochemical staining for DSP confirmed the differentiation of DPSCs to odontoblast-like cells. These results suggested a distinct developmental functionality of the induced DPSCs in vivo. Pulp-like tissue including soft tissue and angiogenesis were observed in the middle of the pores. Although odontoblast-like cells and hard tissue formation were confirmed, the formed tissue in the scaffold was not the typical tubular dentin tissue, further investigation in optimizing scaffold architecture and biological cues is needed to facilitate more natural dentin-pulp-like tissue formation in the future. However, the regeneration of dense mineralized tissue could also be a goal because of its clinical significance to serve as a novel biological capping material.
Conclusion
The NF-PLLA scaffold supported odontogenic differentiation of human DPSCs and dentin-like tissue formation, demonstrating its potential for dental tissue engineering application. The combination of BMP-7 and DXM better promotes the odontogenic differentiation and dentin-like tissue formation both in vitro and in vivo than DXM alone.
Acknowledgments
The authors would like to acknowledge the financial support from the National Institutes of Health (Research Grants DE015384 and DE017689: PXM). The authors thank Stryker Biotech for providing BMP-7 to our research and Kevin Downey for reading the manuscript.
References
- 1.Baelum V, van Palenstein Helderman W, Hugoson A, Yee R, Fejerskov O. A global perspective on changes in the burden of caries and periodontitis: implications for dentistry. J Oral Rehabil. 2007;34:872. doi: 10.1111/j.1365-2842.2007.01799.x. [DOI] [PubMed] [Google Scholar]
- 2.Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature--Part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38:733. [PubMed] [Google Scholar]
- 3.Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies) Quintessence Int. 2008;39:117. [PubMed] [Google Scholar]
- 4.Nakashima M, Reddi AH. The application of bone morphogenetic proteins to dental tissue engineering. Nat Biotechnol. 2003;21:1025. doi: 10.1038/nbt864. [DOI] [PubMed] [Google Scholar]
- 5.Nakashima M, Akamine A. The application of tissue engineering to regeneration of pulp and dentin in endodontics. J Endod. 2005;31:711. doi: 10.1097/01.don.0000164138.49923.e5. [DOI] [PubMed] [Google Scholar]
- 6.Sloan AJ, Smith AJ. Stem cells and the dental pulp: potential roles in dentine regeneration and repair. Oral Dis. 2007;13:151. doi: 10.1111/j.1601-0825.2006.01346.x. [DOI] [PubMed] [Google Scholar]
- 7.Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, DenBesten P, Robey PG, Shi S. Stem cell properties of human dental pulp stem cells. J Dent Res. 2002;81:531. doi: 10.1177/154405910208100806. [DOI] [PubMed] [Google Scholar]
- 8.Gronthos S, Mankani M, Brahim J, Robey PG, Shi S. Postnatal human dental pulp stem cells (DPSCs) in vitro and in vivo. Proc Natl Acad Sci U S A. 2000;97:13625. doi: 10.1073/pnas.240309797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma PX. Biomimetic materials for tissue engineering. Adv Drug Deliv Rev. 2008;60:184. doi: 10.1016/j.addr.2007.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Linde A. Dentin matrix proteins: composition and possible functions in calcification. Anat Rec. 1989;224:154. doi: 10.1002/ar.1092240206. [DOI] [PubMed] [Google Scholar]
- 11.Prescott RS, Alsanea R, Fayad MI, Johnson BR, Wenckus CS, Hao J, John AS, George A. In vivo generation of dental pulp-like tissue by using dental pulp stem cells, a collagen scaffold, and dentin matrix protein 1 after subcutaneous transplantation in mice. J Endod. 2008;34:421. doi: 10.1016/j.joen.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sumita Y, Honda MJ, Ohara T, Tsuchiya S, Sagara H, Kagami H, Ueda M. Performance of collagen sponge as a 3-D scaffold for tooth-tissue engineering. Biomaterials. 2006;27:3238. doi: 10.1016/j.biomaterials.2006.01.055. [DOI] [PubMed] [Google Scholar]
- 13.Ma PX, Zhang R. Synthetic nano-scale fibrous extracellular matrix. J Biomed Mater Res. 1999;46:60. doi: 10.1002/(sici)1097-4636(199907)46:1<60::aid-jbm7>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 14.Ma PX, Choi JW. Biodegradable polymer scaffolds with well-defined interconnected spherical pore network. Tissue Eng. 2001;7:23. doi: 10.1089/107632701300003269. [DOI] [PubMed] [Google Scholar]
- 15.Chen VJ, Ma PX. Nano-fibrous poly(L-lactic acid) scaffolds with interconnected spherical macropores. Biomaterials. 2004;25:2065. doi: 10.1016/j.biomaterials.2003.08.058. [DOI] [PubMed] [Google Scholar]
- 16.Smith LA, Liu X, Hu J, Ma PX. The influence of three-dimensional nanofibrous scaffolds on the osteogenic differentiation of embryonic stem cells. Biomaterials. 2009;30:2516. doi: 10.1016/j.biomaterials.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woo KM, Chen VJ, Jung HM, Kim TI, Shin HI, Baek JH, Ryoo HM, Ma PX. Comparative Evaluation of Nanofibrous Scaffolding for Bone Regeneration in Critical-Size Calvarial Defects. Tissue Eng Part A. 2009 doi: 10.1089/ten.tea.2008.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Woo KM, Chen VJ, Ma PX. Nano-fibrous scaffolding architecture selectively enhances protein adsorption contributing to cell attachment. J Biomed Mater Res A. 2003;67:531. doi: 10.1002/jbm.a.10098. [DOI] [PubMed] [Google Scholar]
- 19.Woo KM, Jun JH, Chen VJ, Seo J, Baek JH, Ryoo HM, Kim GS, Somerman MJ, Ma PX. Nano-fibrous scaffolding promotes osteoblast differentiation and biomineralization. Biomaterials. 2007;28:335. doi: 10.1016/j.biomaterials.2006.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Smith LA, Liu X, Hu J, Wang P, Ma PX. Enhancing osteogenic differentiation of mouse embryonic stem cells by nanofibers. Tissue Eng Part A. 2009;15:1855. doi: 10.1089/ten.tea.2008.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen VJ, Smith LA, Ma PX. Bone regeneration on computer-designed nano-fibrous scaffolds. Biomaterials. 2006;27:3973. doi: 10.1016/j.biomaterials.2006.02.043. [DOI] [PubMed] [Google Scholar]
- 22.Calori GM, Tagliabue L, Gala L, d’Imporzano M, Peretti G, Albisetti W. Application of rhBMP-7 and platelet-rich plasma in the treatment of long bone non-unions: a prospective randomised clinical study on 120 patients. Injury. 2008;39:1391. doi: 10.1016/j.injury.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 23.Giannoudis PV, Kanakaris NK, Dimitriou R, Gill I, Kolimarala V, Montgomery RJ. The synergistic effect of autograft and BMP-7 in the treatment of atrophic nonunions. Clin Orthop Relat Res. 2009;467:3239. doi: 10.1007/s11999-009-0846-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Groeneveld EH, Burger EH. Bone morphogenetic proteins in human bone regeneration. Eur J Endocrinol. 2000;142:9. doi: 10.1530/eje.0.1420009. [DOI] [PubMed] [Google Scholar]
- 25.Meijer GJ, de Bruijn JD, Koole R, van Blitterswijk CA. Cell-based bone tissue engineering. PLoS Med. 2007;4:e9. doi: 10.1371/journal.pmed.0040009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sloan AJ, Rutherford RB, Smith AJ. Stimulation of the rat dentine-pulp complex by bone morphogenetic protein-7 in vitro. Arch Oral Biol. 2000;45:173. doi: 10.1016/s0003-9969(99)00131-4. [DOI] [PubMed] [Google Scholar]
- 27.Rutherford RB. BMP-7 gene transfer to inflamed ferret dental pulps. Eur J Oral Sci. 2001;109:422. doi: 10.1034/j.1600-0722.2001.00150.x. [DOI] [PubMed] [Google Scholar]
- 28.Zhang W, Walboomers XF, Wolke JG, Bian Z, Fan MW, Jansen JA. Differentiation ability of rat postnatal dental pulp cells in vitro. Tissue Eng. 2005;11:357. doi: 10.1089/ten.2005.11.357. [DOI] [PubMed] [Google Scholar]
- 29.Laino G, Graziano A, d’Aquino R, Pirozzi G, Lanza V, Valiante S, De Rosa A, Naro F, Vivarelli E, Papaccio G. An approachable human adult stem cell source for hard-tissue engineering. J Cell Physiol. 2006;206:693. doi: 10.1002/jcp.20526. [DOI] [PubMed] [Google Scholar]
- 30.Zhang W, Walboomers XF, van Osch GJ, van den Dolder J, Jansen JA. Hard tissue formation in a porous HA/TCP ceramic scaffold loaded with stromal cells derived from dental pulp and bone marrow. Tissue Eng Part A. 2008;14:285. doi: 10.1089/tea.2007.0146. [DOI] [PubMed] [Google Scholar]
- 31.Jorgensen NR, Henriksen Z, Sorensen OH, Civitelli R. Dexamethasone, BMP-2, and 1,25-dihydroxyvitamin D enhance a more differentiated osteoblast phenotype: validation of an in vitro model for human bone marrow-derived primary osteoblasts. Steroids. 2004;69:219. doi: 10.1016/j.steroids.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 32.Jager M, Fischer J, Dohrn W, Li X, Ayers DC, Czibere A, Prall WC, Lensing-Hohn S, Krauspe R. Dexamethasone modulates BMP-2 effects on mesenchymal stem cells in vitro. J Orthop Res. 2008;26:1440. doi: 10.1002/jor.20565. [DOI] [PubMed] [Google Scholar]
- 33.Yang X, Walboomers XF, van den Beucken JJ, Bian Z, Fan M, Jansen JA. Hard Tissue Formation of STRO-1-Selected Rat Dental Pulp Stem Cells In Vivo. Tissue Eng Part A. 2009;15:367. doi: 10.1089/ten.tea.2008.0133. [DOI] [PubMed] [Google Scholar]
- 34.Smith AJ, Cassidy N, Perry H, Begue-Kirn C, Ruch JV, Lesot H. Reactionary dentinogenesis. Int J Dev Biol. 1995;39:273. [PubMed] [Google Scholar]
- 35.Zhang W, Walboomers XF, van Kuppevelt TH, Daamen WF, Bian Z, Jansen JA. The performance of human dental pulp stem cells on different three-dimensional scaffold materials. Biomaterials. 2006;27:5658. doi: 10.1016/j.biomaterials.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 36.Duailibi MT, Duailibi SE, Young CS, Bartlett JD, Vacanti JP, Yelick PC. Bioengineered teeth from cultured rat tooth bud cells. J Dent Res. 2004;83:523. doi: 10.1177/154405910408300703. [DOI] [PubMed] [Google Scholar]
- 37.Iwatsuki S, Honda MJ, Harada H, Ueda M. Cell proliferation in teeth reconstructed from dispersed cells of embryonic tooth germs in a three-dimensional scaffold. Eur J Oral Sci. 2006;114:310. doi: 10.1111/j.1600-0722.2006.00385.x. [DOI] [PubMed] [Google Scholar]
- 38.Young CS, Abukawa H, Asrican R, Ravens M, Troulis MJ, Kaban LB, Vacanti JP, Yelick PC. Tissue-engineered hybrid tooth and bone. Tissue Eng. 2005;11:1599. doi: 10.1089/ten.2005.11.1599. [DOI] [PubMed] [Google Scholar]
- 39.Hu J, Liu X, Ma PX. Induction of osteoblast differentiation phenotype on poly(L-lactic acid) nanofibrous matrix. Biomaterials. 2008;29:3815. doi: 10.1016/j.biomaterials.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rutherford RB, Spangberg L, Tucker M, Rueger D, Charette M. The time-course of the induction of reparative dentine formation in monkeys by recombinant human osteogenic protein-1. Arch Oral Biol. 1994;39:833. doi: 10.1016/0003-9969(94)90014-0. [DOI] [PubMed] [Google Scholar]
- 41.Jepsen S, Albers HK, Fleiner B, Tucker M, Rueger D. Recombinant human osteogenic protein-1 induces dentin formation: an experimental study in miniature swine. J Endod. 1997;23:378. doi: 10.1016/S0099-2399(97)80187-2. [DOI] [PubMed] [Google Scholar]
- 42.van den Dolder J, Vehof JW, Spauwen PH, Jansen JA. Bone formation by rat bone marrow cells cultured on titanium fiber mesh: effect of in vitro culture time. J Biomed Mater Res. 2002;62:350. doi: 10.1002/jbm.10189. [DOI] [PubMed] [Google Scholar]
- 43.Viereck V, Siggelkow H, Tauber S, Raddatz D, Schutze N, Hufner M. Differential regulation of Cbfa1/Runx2 and osteocalcin gene expression by vitamin-D3, dexamethasone, and local growth factors in primary human osteoblasts. J Cell Biochem. 2002;86:348. doi: 10.1002/jcb.10220. [DOI] [PubMed] [Google Scholar]
- 44.Feng JQ, Luan X, Wallace J, Jing D, Ohshima T, Kulkarni AB, D’Souza RN, Kozak CA, MacDougall M. Genomic organization, chromosomal mapping, and promoter analysis of the mouse dentin sialophosphoprotein (Dspp) gene, which codes for both dentin sialoprotein and dentin phosphoprotein. J Biol Chem. 1998;273:9457. doi: 10.1074/jbc.273.16.9457. [DOI] [PubMed] [Google Scholar]
- 45.Feng JQ, Huang H, Lu Y, Ye L, Xie Y, Tsutsui TW, Kunieda T, Castranio T, Scott G, Bonewald LB, Mishina Y. The Dentin matrix protein 1 (Dmp1) is specifically expressed in mineralized, but not soft, tissues during development. J Dent Res. 2003;82:776. doi: 10.1177/154405910308201003. [DOI] [PubMed] [Google Scholar]