Abstract
The etiology of small and fresh rectal bleeding in neonates who are not sick is usually unknown; the only known cause is food protein-induced proctocolitis (FPIPC). It has been recently reported that FPIPC is a rare cause of rectal bleeding in newborns, and most cases have been proved to be due to idiopathic neonatal transient colitis. A recommended strategy for diagnosing suspected FPIPC in neonates is as follows. During the early stage, the etiology of small and fresh rectal bleeding in an otherwise healthy newborn need not be studied through extensive investigations. In patients showing continued bleeding even after 4 days, sigmoidoscopy and rectal mucosal biopsy may be performed. Even if mucosal histological findings indicate a diagnosis of FPIPC, further oral food elimination and challenge tests must be performed sequentially to confirm FPIPC. Food elimination and challenge tests should be included in the diagnostic criteria of FPIPC.
Keywords: Food allergy, Proctocolitis, Dietary protein, Food hypersensitivity, Neonates, Rectal bleeding
Introduction
In sick neonates with small and fresh rectal bleeding, the presence of severe illnesses such as infections, necrotizing enterocolitis, or some surgical condition should be determined through extensive investigations. However, in neonates who are not sick but show small and fresh rectal bleeding, the cause may be food protein-induced proctocolitis (FPIPC), which is a benign inflammatory colitis as a result of a non-IgE-mediated immune reaction to ingested foreign proteins1).
FPIPC may often be misdiagnosed when the rectal bleeding is approached based on an empirical understanding of clinical features or histological findings showing eosinophilic infiltration into the recto-sigmoid mucosa2-5). In fact, it has been recently reported that fresh blood in stools and eosinophilic infiltration in the rectosigmoid mucosa can spontaneously resolve in neonates; this condition is termed as neonatal transient eosinophilic colitis (NTEC)6). Moreover, previous studies3-5,7,8) have shown diverse pathological findings and diagnostic criteria in FPIPC.
Neonates with FPIPC have been treated by eliminating the suspected antigens that may have been responsible for the condition9). Parents and family are adversely affected by the high costs. Maternal diet manipulation or change of regular formula to a protein hydrolysate formula or amino acid formula and similar dietary restrictions may continue unnecessarily into later childhood10).
This review was undertaken to suggest a diagnostic strategy for FPIPC in neonates with small amount of fresh rectal bleeding by discussing the diagnostic approaches to FPIPC.
Diagnostic dilemma of FPIPC
1. Clinical history and laboratory tests
In a survey conducted by the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition, 84% of the members agreed that they would empirically change the diet of a neonate or infant with rectal bleeding in order to treat suspected FPIPC. However, only 64% of the neonates or infants with rectal bleeding were pathologically diagnosed with FPIPC2). Since the diagnosis is usually obtained on the basis of clinical manifestations, a significant proportion of neonates or infants appeared to be misdiagnosed with FPIPC and underwent unnecessary dietary changes.
In clinical practice, FPIPC is diagnosed when patients respond positively to the elimination of a suspected triggering food element4). Although the clinical history detailing the reactions to various food items may be useful, these features have not proven to be valuable in predicting and identifying infants with FPIPC11). Since FPIPC onset is often insidious after the ingestion of the specific food, adverse reactions may be difficult to identify9). Moreover, any single laboratory test (e.g., Uni-cap, multi allergy screening test, radioallergosorbent test, skin prick test) has not been reported to be useful for the diagnosis of FPIPC4).
Even though FPIPC was originally described in exclusively breast-fed infants12), it has also been reported in infants receiving cow's milk or soy formula9). However, the findings of recent studies8) suggest that FPIPC occurs more frequently in exclusively breast-fed infants. Lake et al.12) documented that the triggering dietary proteins in the mother's milk pass to neonates with FPIPC. Laitinen et al.13) reported that the increased concentrations of prostaglandin E2 and cysteinyl leukotrienes in breast milk reduce the gross amount of blood in the stools of breast-fed infants with FPIPC. They concluded that a combination of immunomodulatory factors appeared to protect breast-fed infants from having gross blood in stools.
2. Endoscopic findings
The endoscopic findings in FPIPC are diffuse erythema, friability, nodular hyperplasia and/or erosions, and ulcerations2-4,7,8,14,15). Xanthakos et al.2) suggested that endoscopic findings alone are not helpful in diagnosing FPIPC. However, nodular hyperplasias with characteristic circumscribed and/or central pit-like erosions have been noted to be specific findings of infantile FPIPC8).
Lymphoid nodular hyperplasia (LNH) is considered a sign of food allergy in children16,17). However, several infants with LNH show spontaneous resolution of bleeding over a few weeks without any dietary changes2). Since LNH is also found in patients with inflammatory colitis or even in normal controls5), it has not been considered to be disease specific in FPIPC.
3. Histopathologic findings
Prominent eosinophilic infiltration into the rectosigmoid mucosa is a hallmark of FPIPC and suggests that eosinophils play an important role in the pathogenesis of this allergic disorder. The guidelines suggested by Odze et al.3,4) and Machida et al.7) are important for the histopathologic diagnosis of FPIPC. Odze et al.3,4) considered an eosinophilic infiltration of ≥60 cells/10 high-power fields (HPFs) in the lamina propria as a diagnostic criterion, whereas Machida et al.7) suggested that an infiltration of >20 cells/HPF is sufficient to obtain a diagnosis. These diverse levels of eosinophil infiltration hamper histopathological diagnosis of FPIPC.
When the oral food elimination and challenge test (ECT) was performed to the patients for confirmation of FPIPC to determine the confidence of the histopathologic diagnostic criteria8), it revealed that only 63.2% of patients met Machida's diagnostic criterion and that 97.4% satisfied Odze's diagnostic criterion. These findings suggested that Machida's diagnostic guideline is an inappropriate diagnostic criterion for FPIPC.
The histopathologic findings reported in previous studies3-5,7,8) make it difficult to differentially diagnose FPIPC from other rectal bleeding diseases. These findings may also delay the confirmation of FPIPC. Moreover, two cases of NTEC have been reported in neonates with lower gastrointestinal bleeding6). The rectal bleeding disappeared around the eighth day of life with a decline in eosinophil counts without any dietary changes.
Although peripheral blood eosinophilia in newborns has been considered to be associated with infections18,19), the causes and clinical significance of the condition are not known. Moreover, eosinophils are normally found in the rectal mucosa of children (average, 8 cells/HPF)2). These findings indicate that a histological diagnosis of FPIPC based on eosinophilic infiltration alone must be avoided.
FPIPC in neonates
1. Study design
To identify the cause of rectal bleeding in neonates and the frequency of FPIPC, we prospectively analyzed the data of 16 neonates (5 females, 11 males) who were not sick and had small and fresh rectal bleeding without diarrhea, fever, or abdominal distension20). The study protocol was as follows: 1) For the initial 4 days, we observed the patients without any dietary intervention. During this period, laboratory examinations and endoscopic biopsies were performed to detect any infections or other causes of rectal bleeding. 2) If the rectal bleeding stopped without any evidence of infection or any other cause, we considered the case as idiopathic neonatal transient colitis (INTC). When rectal bleeding persisted, a food elimination test was performed to rule out FPIPC. 3) When the rectal bleeding stopped, a food challenge test was performed for confirming FPIPC. If the rectal bleeding recurred with the food challenge test, we confirmed the diagnosis of FPIPC, but if the rectal bleeding did not recur, we regarded this as a case of INTC. 4) In cases of persistent rectal bleeding, we considered the cause to be some condition other than FPIPC or INTC.
We noted the age at onset of symptoms, food type at onset of bleeding, time of disappearance of bleeding, findings of stool smear and culture, endoscopic findings, and the histopathologic findings in biopsy specimens in the 16 otherwise healthy neonates with rectal bleeding. All patients underwent hematological and serological tests, including assessment of complete blood count, erythrocyte sedimentation rate, C-reactive protein, serum immunoglobulins, total serum protein, prothrombin and partial thromboplastin times, and fibrinogen. Urinalysis was also performed. Rotavirus and TORCH (toxoplasmosis, rubella, cytomegalovirus, and herpes infection) screens were run to identify viral infection. Presence of cytomegalovirus and herpes virus was also checked in immunohistochemically stained sections of mucosal biopsy specimens.
Since the elimination or challenge test with the offending food allergen usually resolved or reinitiated the gross bleeding within 72 hours in FPIPC patients2), the state of rectal bleeding was observed for 3 days after the elimination or challenge test. In breast-feeding mothers, 5 highly allergenic food groups, namely, dairy products (e.g., cow's milk), eggs, nuts and soybean, fish and shellfish, and wheat and buckwheat, were eliminated from the maternal diet. When rectal bleeding disappeared, foods were added sequentially to the maternal diet8,21). In formulafed patients, diet change to a protein hydrolysate formula (HA, Maeil Dairy Industry Co., Seoul, Korea) was introduced. In the case of the patients showing rectal bleeding even after the dietary change, an amino acid-based formula (Neocate, SHS International Ltd., Liverpool, UK) was started1,8).
2. Results
In the 16 newborns, median (range) age at symptom onset was 8.5 (1 to 43) days. No neonates showed any other allergic symptoms such as vomiting, eczema, wheezing, or failure to thrive after formula or breast milk feeding.
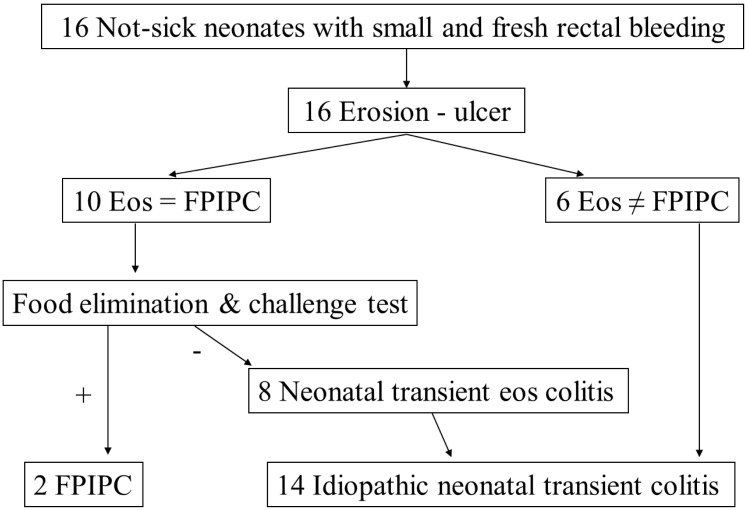
Results of blood chemistry and coagulation screening tests and levels of C-reactive protein and serum IgE were normal in all 16 patients, and hemoglobin and platelet counts were within the normal range. Median (range) peripheral blood eosinophil count was 320 (139 to 1,360)/mm3, and eosinophilia (eosinophil count, >450/mm3) was observed in 6 patients (37.5%). Serum immunoglobulin levels were all within normal limits. Results of blood, urine, and stool cultures were all negative, and results of stool examinations for rotavirus were also negative. Results of serologic studies for TORCH were negative, as were those of immunohistochemical stainings for cytomegalovirus and herpes virus in colonic mucosa. The cause of rectal bleeding was not identified in any of the cases by the various investigations conducted during the first 4 days of observation. These findings are summarized in Fig. 120). Endoscopic abnormalities were observed in all 16 patients. Rectosigmoid lesions showed various characteristics, such as mild erythema, multiple or diffuse erosions, ulcerations, and nodular hyperplasia. From the histological perspective, 10 of the 16 patients satisfied the pathologic criteria3,4) for FPIPC. In 4 patients, rectal bleeding spontaneously resolved within the first 4 days; therefore, they were diagnosed with NTEC and finally INTC. In the other 6 patients, the rectal bleeding resolved when the food elimination test was performed. However, the bleeding recurred in 2 of the 6 after the food challenge test. Therefore, FPIPC was finally confirmed in these 2 cases. Thus, 8 patients were diagnosed with NTEC. In 6 cases, which did not satisfy the pathologic diagnostic criteria, rectal bleeding disappeared spontaneously within the first 4 days; these patients were diagnosed with INTC. Finally, 14 of the 16 patients (87.5%) achieved spontaneous recovery within an average (range) of 4 (1 to 8) days after onset of symptoms; these patients were diagnosed with INTC.
Fig. 1.
Results of tests for small and fresh rectal bleeding in neonates who were not sick. Eos, eosinophilic; FPIPC, food protein-induced proctocolitis; Eos = FPIPC, satisfying eosinophilic infiltration guideline of FPIPC3,4); Eos ≠ FPIPC, not satisfying eosinophilic infiltration guideline of FPIPC.
In one case of FPIPC, rectal bleeding persisted despite the administration of protein hydrolysate, and it only disappeared after administering an amino acid-based formula. In this case, diagnosis of FPIPC was confirmed because rectal bleeding recurred after administration of cow's milk-based formula. One of the breast-fed newborn showed a positive response to oral food ECT with fish and eggs in the maternal diet, and was also confirmed to have FPIPC.
Diagnostic strategy for FPIPC in neonates
The results of this study reveal that FPIPC is a rare condition in otherwise healthy neonates with small and fresh rectal bleeding20). Most cases are categorized as INTC, which is similar to FPIPC in terms of symptoms and histopathological findings. INTC resolves spontaneously without any dietary modifications or medical treatment in approximately 4 days. Therefore, it is essential to perform an oral food ECT to confirm FPIPC, which should not be diagnosed on the basis of clinical suspicion or pathological findings alone.
Based on initial clinical symptoms, the 14 patients with INTC (14/16, 88%) would have been misdiagnosed with FPIPC. If we had adopted the clinical and pathological guidelines for the diagnosis of FPIPC, 8 patients (8/10, 80%) with NTEC would have been misdiagnosed with FPIPC. If we had adopted only the elimination test without challenge testing for the diagnosis of FPIPC, 4 patients (4/6, 67%) would have been misdiagnosed with false-positive FPIPC. These results20) reveal the diagnostic importance of the food challenge test. It is a safe diagnostic tool for FPIPC because it does not cause severe adverse reactions in FPIPC patients.
Arvola et al.22) followed up 40 young infants with rectal bleeding for 1 year. They reported that milk allergy accounted for only 18% of cases; the etiology of rectal bleeding remained unknown in most patients, and an association with viruses was noted in a minority. They concluded that the food challenge test was essential in infants who become symptom-free on a cow's milk-free diet in order to reduce the number of false-positive diagnoses of cow's milk allergy.
Small and fresh rectal bleeding in a newborn is generally a benign and self-limiting disorder. FPIPC among these patients is rarer than previously believed. A diagnostic strategy for small and fresh rectal bleeding in neonates who are not sick may be as follows: 1) During the early stage, extensive investigations are not needed; 2) In patients showing continued bleeding even after 4 days, sigmoidoscopy and mucosal biopsy should be performed; 3) Oral food ECT must be performed thereafter to confirm FPIPC. Oral food ECT should be considered to be the diagnostic criterion of FPIPC.
Conclusions
FPIPC is a rare cause of rectal bleeding in newborns, and most of the cases are likely to be INTC. Although the clinical features and pathologic findings of FPIPC are concordant with previously reported diagnostic criteria, oral food ECT should be performed to confirm FPIPC.
Furthermore, further studies are required to determine the causes and the pathogenic significances of eosinophilia in peripheral blood and eosinophilic infiltration in rectosigmoid mucosa of INTC in newborns.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Maloney J, Nowak-Wegrzyn A. Educational clinical case series for pediatric allergy and immunology: allergic proctocolitis, food protein-induced enterocolitis syndrome and allergic eosinophilic gastroenteritis with protein-losing gastroenteropathy as manifestations of non-IgE-mediated cow's milk allergy. Pediatr Allergy Immunol. 2007;18:360–367. doi: 10.1111/j.1399-3038.2007.00561.x. [DOI] [PubMed] [Google Scholar]
- 2.Xanthakos SA, Schwimmer JB, Melin-Aldana H, Rothenberg ME, Witte DP, Cohen MB. Prevalence and outcome of allergic colitis in healthy infants with rectal bleeding: a prospective cohort study. J Pediatr Gastroenterol Nutr. 2005;41:16–22. doi: 10.1097/01.mpg.0000161039.96200.f1. [DOI] [PubMed] [Google Scholar]
- 3.Odze RD, Bines J, Leichtner AM, Goldman H, Antonioli DA. Allergic proctocolitis in infants: a prospective clinicopathologic biopsy study. Hum Pathol. 1993;24:668–674. doi: 10.1016/0046-8177(93)90248-f. [DOI] [PubMed] [Google Scholar]
- 4.Odze RD, Wershil BK, Leichtner AM, Antonioli DA. Allergic colitis in infants. J Pediatr. 1995;126:163–170. doi: 10.1016/s0022-3476(95)70540-6. [DOI] [PubMed] [Google Scholar]
- 5.Winter HS, Antonioli DA, Fukagawa N, Marcial M, Goldman H. Allergy-related proctocolitis in infants: diagnostic usefulness of rectal biopsy. Mod Pathol. 1990;3:5–10. [PubMed] [Google Scholar]
- 6.Ohtsuka Y, Shimizu T, Shoji H, Kudo T, Fujii T, Wada M, et al. Neonatal transient eosinophilic colitis causes lower gastrointestinal bleeding in early infancy. J Pediatr Gastroenterol Nutr. 2007;44:501–505. doi: 10.1097/01.mpg.0000252194.06955.18. [DOI] [PubMed] [Google Scholar]
- 7.Machida HM, Catto Smith AG, Gall DG, Trevenen C, Scott RB. Allergic colitis in infancy: clinical and pathologic aspects. J Pediatr Gastroenterol Nutr. 1994;19:22–26. doi: 10.1097/00005176-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Hwang JB, Park MH, Kang YN, Kim SP, Suh SI, Kam S. Advanced criteria for clinicopathological diagnosis of food protein-induced proctocolitis. J Korean Med Sci. 2007;22:213–217. doi: 10.3346/jkms.2007.22.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norwak-Wegrzyn A. Food protein-induced enterocolitis, enteropathy, and proctocolitis. In: Metcalfe DD, Sampson HA, Simon RA, editors. Food allergy: adverse reactions to foods and food additives. 3rd ed. Baltimore: Blackwell Publishing Inc.; 2003. pp. 227–241. [Google Scholar]
- 10.Forsyth BW, McCarthy PL, Leventhal JM. Problems of early infancy, formula changes, and mothers' beliefs about their infants. J Pediatr. 1985;106:1012–1017. doi: 10.1016/s0022-3476(85)80260-2. [DOI] [PubMed] [Google Scholar]
- 11.Bock SA. The natural history of food sensitivity. J Allergy Clin Immunol. 1982;69:173–177. doi: 10.1016/0091-6749(82)90096-3. [DOI] [PubMed] [Google Scholar]
- 12.Lake AM, Whitington PF, Hamilton SR. Dietary protein-induced colitis in breast-fed infants. J Pediatr. 1982;101:906–910. doi: 10.1016/s0022-3476(82)80008-5. [DOI] [PubMed] [Google Scholar]
- 13.Laitinen K, Arvola T, Moilanen E, Lampi AM, Ruuska T, Isolauri E. Characterization of breast milk received by infants with gross blood in stools. Biol Neonate. 2005;87:66–72. doi: 10.1159/000081955. [DOI] [PubMed] [Google Scholar]
- 14.Anveden-Hertzberg L, Finkel Y, Sandstedt B, Karpe B. Proctocolitis in exclusively breast-fed infants. Eur J Pediatr. 1996;155:464–467. doi: 10.1007/BF01955182. [DOI] [PubMed] [Google Scholar]
- 15.Pumberger W, Pomberger G, Geissler W. Proctocolitis in breast fed infants: a contribution to differential diagnosis of haematochezia in early childhood. Postgrad Med J. 2001;77:252–254. doi: 10.1136/pmj.77.906.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kokkonen J, Karttunen TJ, Niinimäki A. Lymphonodular hyperplasia as a sign of food allergy in children. J Pediatr Gastroenterol Nutr. 1999;29:57–62. doi: 10.1097/00005176-199907000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Kokkonen J, Karttunen TJ. Lymphonodular hyperplasia on the mucosa of the lower gastrointestinal tract in children: an indication of enhanced immune response? J Pediatr Gastroenterol Nutr. 2002;34:42–46. doi: 10.1097/00005176-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Patel L, Garvey B, Arnon S, Roberts IA. Eosinophilia in newborn infants. Acta Paediatr. 1994;83:797–801. doi: 10.1111/j.1651-2227.1994.tb13146.x. [DOI] [PubMed] [Google Scholar]
- 19.Yen JM, Lin CH, Yang MM, Hou ST, Lin AH, Lin YJ. Eosinophilia in very low birth weight infants. Pediatr Neonatol. 2010;51:116–123. doi: 10.1016/S1875-9572(10)60021-6. [DOI] [PubMed] [Google Scholar]
- 20.Jang HJ, Kim AS, Hwang JB. The etiology of small and fresh rectal bleeding in not-sick neonates: should we initially suspect food protein-induced proctocolitis? Eur J Pediatr. 2012;171:1845–1849. doi: 10.1007/s00431-012-1825-2. [DOI] [PubMed] [Google Scholar]
- 21.Choi SY, Park MH, Choi WJ, Kang U, Oh HK, Kam S, et al. Clinical features and the natural history of dietary protein induced proctocolitis: a study on the elimination of offending foods from the maternal diet. Korean J Pediatr Gastroenterol Nutr. 2005;8:21–30. [Google Scholar]
- 22.Arvola T, Ruuska T, Keranen J, Hyoty H, Salminen S, Isolauri E. Rectal bleeding in infancy: clinical, allergological, and microbiological examination. Pediatrics. 2006;117:e760–e768. doi: 10.1542/peds.2005-1069. [DOI] [PubMed] [Google Scholar]