Abstract
The purpose of this study is to improve understanding of HIV vulnerability and opportunities for HIV prevention within the social networks of male-to-female transgender persons in San Salvador, El Salvador. We compare HIV prevalence and behavioral data from a sample of gay-identified men who have sex with men (MSM) (n = 279), heterosexual or bisexual identified MSM (n = 229) and transgender persons (n = 67) recruited using Respondent Driven Sampling. Transgender persons consistently reported higher rates of HIV risk behavior than the rest of the study population and were significantly more likely to be involved in sex work. While transgender persons reported the highest rates of exposure to HIV educational activities they had the lowest levels of HIV-related knowledge. Transgender respondents’ social networks were homophilous and efficient at recruiting other transgender persons. Findings suggest that transgender social networks could provide an effective and culturally relevant opportunity for HIV prevention efforts in this vulnerable population.
Keywords: El Salvador, Transgender, HIV, Men who have sex with men, Sexually transmitted infections, Respondent driven sampling
Introduction
The first case of HIV in El Salvador was reported in 1984 [1]. According to data from the Salvadoran National HIV/AIDS Program, 1641 new cases of HIV and 268 cases of AIDS were identified in 2008, of which the majority (80.4%) occurred in 15–49 year olds and 61.6% occurred in males [1]. National level HIV prevalence among 15–49 year olds is estimated to be 0.8% and the epidemic in El Salvador is classified as “concentrated”, with specific vulnerable populations demonstrating a disproportionate burden of HIV compared to the general population. According to the 2002 Central American Multi-Center Study, which measured HIV-related behaviors and HIV prevalence in five Central American countries, HIV prevalence among female sex workers (n = 491) in El Salvador was 3.2% and prevalence among men who have sex with men (MSM) (n = 347) was 15.3% [2].
Male-to-female transgender persons have traditionally been included as a sub-group of MSM in behavioral and disease surveillance studies, including the aforementioned Multi-Center Study, in which self-indentifying transgender persons represented 10% of the MSM sample [2]. There is a dearth of data from the Central American region, including El Salvador, specifically describing the epidemiology of HIV among transgender persons and identifying individual and contextual factors associated with HIV vulnerability. Studies from the US that do provide data specifically for transgender persons consistently show disproportionately high rates of HIV, both compared to the general population as well as to the MSM population [3, 4]. The transgender population is increasingly being recognized as the “new face” of the HIV epidemic [5]. De Santis [5] conducted a systematic review of studies conducted with male-to-female transgender persons in the US and found HIV prevalence ranged from 12 to 52% while Herbst et al. [4] calculated a 27.7% HIV prevalence in a systematic review of studies conducted with transgender participants.
To date, the focus of HIV prevention efforts with MSM and transgender populations in El Salvador, and the Central American region as a whole, has been on condom promotion and distribution and increasing HIV knowledge. Such individual-level efforts frequently use peer-led outreach and behavior change communication strategies in public venues frequented by MSM and transgender persons including discos, bars, and motels [6, 7]. There is increasing recognition across the Central American region of the need to develop innovative intervention strategies that build upon these existing efforts to respond to the unique reality of transgender persons and address the social and structural context of stigma and discrimination around “non-normative” sexual and gender identities. The design of such efforts requires the integration of epidemiological and social science research strategies to provide a comprehensive and situated understanding of the context surrounding HIV vulnerability among transgender persons [3,5]. While there are no laws explicitly penalizing homosexuality or same-sex behavior in El Salvador, homophobia and discrimination have been identified as major barriers to effective programming and service provision. Recent decrees by the Salvadoran Ministry of Health seek to guarantee the rights of all individuals to HIV prevention, care and support services regardless of sexual orientation, but the impact of this measure has yet to be evaluated [8].
At the social and structural levels, discrimination and social marginalization limit access to information, services and economic opportunities for transgender persons [5, 9,10]. Involvement in commercial sex work has been reported by as much as 44% of transgender populations in previous studies [11]. Over one-third (37.3%) of MSM in El Salvador reported having received payment for sex in a survey conducted by the international non-governmental organization Population Services International, but this report does not specify what proportion of respondents were transgender [12]. At the relational level, power dynamics and violence with sex partners, both paying and non-paying, may limit transgender persons’ ability to negotiate consistent condom use, with commercial and non-commercial partners [5, 9]. At the individual level, drug and alcohol use and psychosocial factors such as lack of information, limited condom use negotiation skills, and fatalism towards survival may create more proximal barriers to condom use [5, 9, 13]. These multiple layers of vulnerability experienced by transgender persons require a multifaceted and holistic response that goes beyond provision of information and condoms and seeks to create a social environment in which people are able to thrive and protect their health [10, 14, 15].
One potential opportunity to address the social marginalization and HIV vulnerability among transgender persons is to utilize their existing social networks as an entry point for HIV prevention programs. Peer networks may be particularly important among transgender persons, who are socially excluded from neighborhoods, families, and other social structures [16]. Social network approaches to HIV prevention have achieved significant reductions in HIV risk behaviors with diverse vulnerable populations including drug users [17–19] and MSM [20–22].
The purpose of this study is to improve understanding of HIV vulnerability and opportunities for HIV prevention within the social networks of male-to-female transgender persons in San Salvador, the capital city of El Salvador. The first objective is to describe and compare HIV-related risk behaviors, prevalence of sexually transmitted infections (including HIV), and exposure to HIV prevention interventions among gay-identified MSM, heterosexual or bisexual-identified MSM, and male-to-female transgender persons. The second objective is to examine characteristics of social networks, including homophily (defined in “Methods” section), affiliation, and network size, of the transgender population. These data will be used to consider how social networks could be used as tools for HIV prevention to reach and effectively engage transgender persons and networks at heightened risk for HIV infection.
Methods
Study Site, Eligibility and Sampling
Data were collected from March until September 2008 in the city of San Salvador. Respondent-Driven Sampling (RDS) methodology was used to recruit males and male-to-female transgender persons. Eligibility criteria included being 18 years and older, having engaged in anal sex with another biological man in the previous year, and living or working in San Salvador. Excluding seeds (see below), a sample of 602 was obtained including 279 gay-identified MSM, 229 hetero/bisexual MSM, 67 transgender and 27 persons of unknown or missing identification. RDS recruitment is similar to snowball or chain-referral; however, by collecting data on social network size and limiting recruitment through coupons, the results can be adjusted to represent the network population sampled [23–25]. The RDS methodology also facilitates recruitment of individuals who do not visit typical sites for place-based outreach recruitment approaches (such as time location sampling) and/or who are not directly linked to community-based organizations. Standard RDS methodology was followed for the recruitment and data collection process [26, 27].
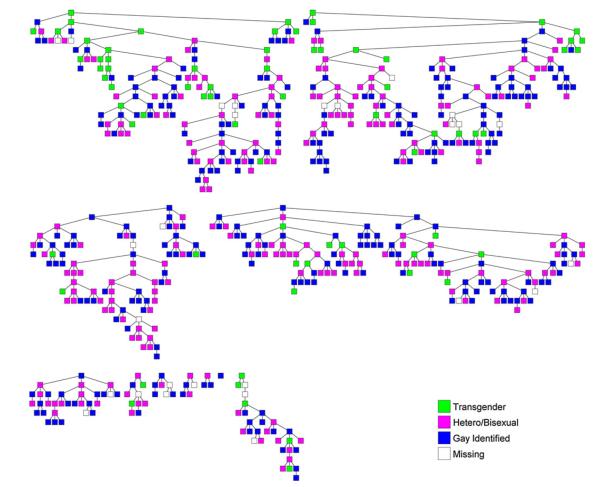
We conducted a formative study of MSM and transgender persons in San Salvador to ensure social networks were strong enough to support the RDS methodology and to inform the questionnaire development [28]. To start the recruitment, participants referred to as ‘seeds’ were identified through local organizations working with the MSM and transgender populations. We identified eleven seeds, who were diverse with respect to age, place of work, educational level and self-identification (transgender seeds n = 3, gay identified seeds n = 5, hetero/bisexual identified seeds n = 3). All participants, including seeds, received up to three recruitment coupons to recruit other eligible participants, based on the aforementioned criteria, from their social networks. Of the 11 seeds, six resulted in long chains reaching at least 5 waves of recruitment. The longest recruitment chain included 18 waves (Fig. 1). Only one seed failed to produce any recruits. All coupons had a unique number which was used to track recruitment chains and to ensure anonymity in linking the questionnaire and biological specimens. Recruits who presented a valid coupon to the study site were screened for eligibility, provided information about the study, asked to provide written informed consent and asked questions in Spanish in a face-to-face interview regarding network size and demographic information. Audio Computer-Assisted Self-Interviewing (ACASI) was used for the behavioral questionnaire. Our team validated the use of ACASI with MSM in a previous study in Honduras and has used ACASI with MSM populations throughout the Central American region [29]. Upon completion of the survey, participants received promotional materials and condoms and their choice of other incentives (e.g. T-shirt, towel, make-up kit, lubricants, and additional condoms) for recruiting up to three eligible peers. No cash incentives were used.
Fig. 1.
RDS recruitment chains
The ethical review board of the Rosales National Hospital (RNH) in San Salvador reviewed and approved the study protocol.
Clinical Examinations and Biological Testing
Participants at all sites were asked to provide biological specimens for testing and undergo a physical exam conducted by a physician to evaluate signs and symptoms of sexually transmitted infection (STI). Intravenous blood and urine samples were collected. Participants could refuse to provide one or more of these samples and still participate in the study. Urine was screened by polymerase chain reaction (PCR) for Trichomanas vaginalis, Mycoplasma genitalium, Neisseria gonorrhoeae, and Chlamydia trachomatis. Blood samples were tested for HIV-1 and HSV-2 in all participants. HIV testing was performed on site with two rapid HIV tests (Determine® HIV-1/2 and OraQuick® Rapid HIV-1 Antibody Test); preliminary HIV-positive results were confirmed with HIV enzyme-linked immunosorbent assay (ELISA) confirmatory tests. Participants received post-test counseling and received HIV test results 30 min after testing. HSV-2 was screened using the HSV-2 ELISA test. Syphilis sero-positivity was estimated based on reactive rapid plasma reagin (RPR) and positive Treponemal particle-agglutination assay (TPPA) results. STI test results were provided 4 weeks later through the participating government health centers. Free treatment was provided to participants with STI symptoms or a laboratory-diagnosed STI, per the guidelines of the Ministry of Health of El Salvador. Participants with STI symptoms or a laboratory-diagnosed STI were also asked to refer their sex partners for treatment.
Measures
Participants were asked to self-identify as either (1) heterosexual, (2) bisexual, (3) homosexual or gay-identifying, or (4) transgender. Those who self-identified as heterosexual or bisexual were combined to preserve sample size. Participants were not asked to provide their gender. Socio-demographic characteristics included age, highest educational level attained, and average monthly income. Sexual risk behaviors and condom use were measured through dichotomous responses (yes/no) to questions about the following behaviors: having sold sex in the last 12 months, current involvement in selling sex, alcohol consumption in the last 30 days, having 5 or more drinks at one time in the last 30 days, ever used illicit drugs, used any such drug use in the last 30 days, had 1 or more casual partners in the last 12 months, used a condom at last sex with a casual partner, and used a condom at last sex with a stable partner. Frequent condom use with all partners was dichotomized as those who reported using condoms with all partners “frequently” or “always” versus anything less. The variable curable active STI was defined as having any positive test for to Treponema pallidum, T. vaginalis, M. genitalium, N. gonorrhoeae or C. trachomatis. HIV and Herpes were measured as described above. Exposure to HIV prevention interventions included measures of any participation in HIV educational sessions (charlas) or discussions in the last 12 months (yes/no) or ever having received HIV testing and counseling (yes/no). Following recent UNAIDS guidelines [30], knowledge about ways to prevent HIV transmission is a dichotomous score based on responses to five questions regarding the individual’s knowledge of ways to prevent HIV:
Can a healthy-looking person have HIV?
Can a person get HIV from mosquito bites?
Can a person get HIV by sharing a meal with someone who is infected?
Can having sex with only one faithful, uninfected partner reduce the risk of HIV transmission?
Can using condoms reduce the risk of HIV transmission?
Respondents who answer all five questions correctly were considered to have knowledge of ways to prevent HIV.
Social network size, or degree, is measured through self-reports of the number of individuals each respondent knows within the target population. Network size was determined using the following four questions regarding the size of the participants’ social network:
How many men who have sex with men do you know and who know you who live in this city?
Of these people that you know, how many are over 18 years old?
With how many of these do you get together regularly?
How many of these people have you seen or spoken with in the last 30 days?
Data Analysis
Proportion estimates and 95% confidence intervals (CI) were calculated using the RDS Analysis Tool 5.6 (RDSAT), a software package specifically developed to analyze data collected through RDS (www.respondentdrivensampling.org). RDSAT was developed to adjust for biases associated with chain referral sampling by weighting participants’ probability of recruitment (social network size) into the RDS sample and controlling for social network and recruitment patterns [23, 24]. Confidence intervals were calculated using the “estimate prevalence” function with 10,000 resamples for bootstrapping, single tailed α = 0.025, and default settings for all other options [31]. Statistical significance of differences was estimated based on the overlap of confidence intervals between groups. The bootstrap algorithm used by RDSAT to estimate non-symmetric confidence intervals precludes P-value calculation and reporting. All variables were categorized. RDSAT was also used to stratify HIV and STI results by various risk factors. All variables analyzed were assessed for equilibrium with convergence set at 0.2% of the sample estimate [32].
Social network characteristics (homophily, affiliation, and network size) were also analyzed using RDSAT 5.6 [31]. Homophily is the tendency for individuals to associate with peers who are similar to themselves, commonly known as the “birds of a feather flock together” principle [33]. The RDS homophily measure is defined as the proportion of in-group recruitments beyond those expected through random mixing, where random mixing is defined by the estimated population proportion of the group [32]. The measure varies from −1 to +1:−1 signifies complete avoidance where there are no in-group ties at all, 0 signifies the number of in-group ties is proportional to group size and suggests the analyzed variable does not play a role in who is connected to whom, and +1 signifies complete preference where group members only make ties within the group. Affiliation is a generalized form of homophily which measures preference and avoidance across different groups. Two-tailed P-values for homophily and affiliation are calculated by comparing observed proportion of in-group recruitments to that expected under random mixing where the null hypothesis is defined as the estimated proportional size of the recruited group [34]. The relationship between the recruiter and recruit was not tracked. In analysis, responses to the fourth network size question listed above were used to calculate weighted estimates. Average personal network size for a specific group is then estimated by adjusting these data for the greater likelihood that high degree individuals will be preferentially sampled by RDS [23]. Respondents were asked the number of MSM they know without reference to transgender persons. It is unknown how or if responses would differ had respondents been asked the number of MSM or transgender persons they know.
Results
Estimates of Population Demographics
Table 1 shows estimated population demographics by self-identified subgroup. The majority of the population was composed of self-identified heterosexual or bisexual MSM (n = 229, 38%) and gay-identified MSM (n = 279, 46%). Transgender persons made up 9% (n = 67, 11%) of the study population. Overall, no significant differences between these groups were found on age or income. However, transgender persons reported significantly lower levels of education than the rest of the study population.
Table 1.
Estimated population demographics
| Overall (n = 602a) |
Transgender (n = 67) |
Hetero- or bi-sexual (n = 229) |
Gay identified (n = 279) |
|
|---|---|---|---|---|
| Overall | 0.09 | 0.45 | 0.46 | |
| 95% CI | 0.06–0.13 | 0.38–0.51 | 0.40–0.53 | |
| Age | ||||
| 18–24 | 0.60 | 0.63 | 0.54 | 0.64 |
| 95% CI | 0.53–0.67 | 0.45–0.8 | 0.45–0.65 | 0.51–0.7 |
| 25–34 | 0.28 | 0.20 | 0.34 | 0.26 |
| 95% CI | 0.22–0.34 | 0.11–0.39 | 0.24–0.42 | 0.21–0.37 |
| 35+ | 0.12 | 0.17 | 0.13 | 0.10 |
| 95% CI | 0.08–0.17 | 0.02–0.3 | 0.07–0.2 | 0.06–0.16 |
| Education | ||||
| No school/primary | 0.10 | 0.34 | 0.08 | 0.05 |
| 95% CI | 0.06–0.14 | 0.15–0.55 | 0.04–0.14 | 0.02–0.11 |
| Secondary | 0.60 | 0.54 | 0.64 | 0.59 |
| 95% CI | 0.54–0.65 | 0.35–0.74 | 0.53–0.7 | 0.5–0.67 |
| Some college | 0.30 | 0.12 | 0.29 | 0.36 |
| 95% CI | 0.25–0.36 | 0.03–0.24 | 0.22–0.33 | 0.23–0.44 |
| Monthly income | ||||
| None | 0.05 | – | 0.04 | 0.08 |
| 95% CI | 0.02–0.09 | – | 0.01–0.06 | 0.02–0.15 |
| <$180 USD | 0.36 | 0.41 | 0.36 | 0.31 |
| 95% CI | 0.3–0.42 | 0.18–0.62 | 0.27–0.47 | 0.22–0.4 |
| $181–$500 USD | 0.44 | 0.51 | 0.49 | 0.40 |
| 95% CI | 0.38–0.51 | 0.29–0.74 | 0.4–0.59 | 0.32–0.49 |
| >$500 USD | 0.15 | 0.08 | 0.11 | 0.21 |
| 95% CI | 0.11–0.2 | 0.02–0.19 | 0.06–0.17 | 0.15–0.29 |
95% CI 95% confidence interval
Includes 27 respondents with missing sexual identity data
HIV-Related Risk Factors
Transgender persons consistently reported higher rates of HIV risk behavior than the rest of the study population. While transgender persons made up less than 10% of the study population, this group accounted for 25% (95% CI 14–40%) of those who reported having sold sex in the past 12 months. Over half of transgender respondents reported having sold sex in the past 12 months. Among those reporting having sold sex in the past 12 months, a significantly higher proportion of transgender persons (87%) were currently engaged in sex work than gay-identified MSM (37%). Transgender persons reported higher rates of having 1 or more casual sex partners in the last 12 months, alcohol and drug use, Herpes and HIV infection than self-identified heterosexual or bisexual and gay-identified MSM. Transgender persons also reported higher rates of condom use and low rates of active curable STI. These differences, however, were not statistically significant.
Table 2 also shows results measuring exposure to and knowledge of HIV prevention messages. Transgender persons had higher exposure to HIV prevention activities than their counterparts. Transgender persons reported significantly higher rates of attending HIV prevention charla (86%) and having ever had an HIV test (81%) than heterosexual/bisexual MSM (53 and 48%, respectively). Higher rates of exposure, however, did not translate into greater knowledge of HIV prevention practices. On a dichotomous score measuring knowledge of HIV prevention practices, 45% of transgender persons were found to have knowledge of HIV prevention practices, while 49% of hetero/bisexual MSM and 59% of gay-identified MSM were found to have knowledge. Consequently increased exposure to HIV prevention messages does not appear to have results in greater HIV prevention knowledge among transgender persons.
Table 2.
HIV-related risk factors and self-reported sexual identity
| Overall (n = 602a) |
Transgender (n = 67) |
Hetero- or bi-sexual (n = 229) |
Gay identified (n = 279) |
|
|---|---|---|---|---|
| Sexual risk behaviors | ||||
| Sold sex past 12 months | 0.18 | 0.54 | 0.13 | 0.14 |
| 95% CI | 0.14–0.23 | 0.34–0.76 | 0.08–0.2 | 0.09–0.21 |
| Currently selling sex (of those who sold sex in last 12 months) | 0.57 | 0.87 | 0.64 | 0.37 |
| 95% CI | 0.43–0.72 | 0.71–0.96 | 0.4–0.85 | 0.16–0.61 |
| One or more casual sex partners | 0.60 | 0.78 | 0.55 | 0.64 |
| 95% CI | 0.53–0.66 | 0.64–0.95 | 0.43–0.64 | 0.56–0.73 |
| Condom use | ||||
| Frequent condom use-all partnersb (n = 574) | 0.61 | 0.74 | 0.56 | 0.63 |
| 95% CI | 0.55–0.67 | 0.56–0.91 | 0.45–0.64 | 0.55–0.74 |
| Used condom at last sex with casual partner (n = 313) | 0.66 | 0.72 | 0.63 | 0.67 |
| 95% CI | 0.54–0.75 | 0.39–0.95 | 0.47–0.83 | 0.50–0.84 |
| Used condom at last sex with stable partner (n = 202) | 0.68 | 0.88 | 0.64 | 0.69 |
| 95% CI | 0.47–0.85 | 0.47–1.0 | 0.45–0.96 | 0.47–0.90 |
| Alcohol and drug use | ||||
| Drank alcohol in last 30 days | 0.54 | 0.72 | 0.52 | 0.50 |
| 95% CI | 0.47–0.59 | 0.5–0.84 | 0.43–0.61 | 0.41–0.59 |
| Had five or more drinks on four or more occasions in last 30 days | 0.29 | 0.44 | 0.29 | 0.22 |
| 95% CI | 0.23–0.34 | 0.23–0.62 | 0.21–0.38 | 0.14–0.28 |
| Ever used drugs | 0.23 | 0.42 | 0.27 | 0.16 |
| 95% CI | 0.19–0.29 | 0.2–0.6 | 0.19–0.36 | 0.1–0.23 |
| Used drugs last 30 days | 0.08 | 0.27 | 0.09 | 0.04 |
| 95% CI | 0.05–0.12 | 0.06–0.43 | 0.03–0.16 | 0.01–0.06 |
| STD prevalence | ||||
| Has active curable STD | 0.14 | 0.14 | 0.14 | 0.17 |
| 95% CI | 0.1–0.19 | 0.04–0.26 | 0.08–0.2 | 0.1–0.23 |
| Herpes positive | 0.46 | 0.64 | 0.36 | 0.51 |
| 95% CI | 0.4–0.53 | 0.41–0.81 | 0.27–0.45 | 0.44–0.62 |
| HIV positive | 0.11 | 0.19 | 0.10 | 0.11 |
| 95% CI | 0.08–0.15 | 0.05–0.39 | 0.05–0.15 | 0.06–0.16 |
| HIV prevention and knowledge | ||||
| Attended HIV lecture in past 12 months | 0.64 | 0.86 | 0.53 | 0.69 |
| 95% CI | 0.58–0.7 | 0.71–0.97 | 0.42–0.61 | 0.62–0.77 |
| Ever had HIV test | 0.58 | 0.81 | 0.48 | 0.60 |
| 95% CI | 0.53–0.64 | 0.66–0.93 | 0.39–0.58 | 0.52–0.7 |
| Has knowledge of HIV prevention | 0.54 | 0.45 | 0.49 | 0.59 |
| 95% CI | 0.46–0.58 | 0.26–0.68 | 0.39–0.57 | 0.51–0.68 |
95% CI 95% confidence interval
Includes 27 respondents with missing sexual identity data
Less than five respondents reported “always” using condoms with all partners
RDS Recruitment and Social Network Characteristics
Figure 1 shows a graph of recruitment chains collected in the sample. Our observed recruitment characteristics show RDS sampling was successful. A concern for many RDS studies is the presence of network bottlenecks that may impede recruitment from one group to another [35]. Table 3 shows our recruitment matrix by sub-group. Each cell represents the count of column recruitments made by row. For example, transgender respondents recruited a total of 38 gay-identified respondents (1st row, 3rd column). In this study, we observed relatively large numbers of recruitments from each group to every other group (i.e., no zero cells), showing that network bottlenecks were not a major concern in this sample.
Table 3.
RDS sample and social network characteristics by self-reported sexual identity
| Transgender | Hetero- or bi-sexual |
Gay identified |
Missing | Total | |
|---|---|---|---|---|---|
| Distribution of recruits | 67 | 229 | 279 | 27 | 602 |
| Estimated population proportion | 0.09 | 0.45 | 0.46 | 1.00 | |
| 95% CI of estimated proportion | 0.06–0.13 | 0.38–0.51 | 0.40–0.53 | ||
| Sample proportion | 0.11 | 0.38 | 0.46 | 0.04 | 1.00 |
| Average network sizea | 5.21 | 3.76 | 4.43 | 5.53 | |
| Homophily | 0.20 | −0.08 | 0.08 | 0.19 | |
| Recruitment matrix | |||||
| Transgender | 24 | 25 | 38 | 2 | 89 |
| Hetero- or bi-sexual | 20 | 92 | 109 | 8 | 229 |
| Gay identified | 19 | 103 | 127 | 12 | 261 |
| Missing | 4 | 9 | 5 | 5 | 23 |
| 602 | |||||
| Affiliation matrix | |||||
| Transgender | 0.20 | −0.30 | −0.15 | 0.02 | |
| Hetero- or bi-sexual | −0.03 | −0.08 | 0.06 | 0.01 | |
| Gay identified | 0.00 | −0.09 | 0.08 | −0.06 | |
| Missing | 0.03 | −0.22 | −0.25 | 0.19 |
Respondents were asked the number of MSM they know without reference to transgender persons. It is unknown how or if responses would differ had respondents been asked the number of MSM or transgender persons they know
Table 3 shows the results of our analysis of social network characteristics. Transgender respondents disproportionately recruited each other, as evidenced by a high homophily score of 0.20, which is significantly different to what would be expected under random mixing (P < 0.001) [34]. That is, transgender persons tended to preferentially seek out and associate with other transgender persons. Furthermore, transgender persons’ preference for forming and maintaining social ties with other transgender persons comes at the expense of forming ties with hetero/bisexual, but not gay-identified MSM as evidenced by the negative affiliation values from transgender respondents to hetero/bisexual respondents (−0.30, P < 0.01) and to gay-identified respondents (−0.15, P = 0.53). Equally important, hetero/bisexual and gay-identified MSM have near zero, non-significant homophily (−0.08, P = 0.13 and 0.08, P = 0.33, respectively) signifying that they frequently intermix with other groups. While transgender homophily is significantly higher than the other subgroups, it is not extreme, signifying that while transgender persons are more densely connected to each other, they remain an integrated part of the greater MSM population. This is evident in the recruitment patterns shown in Fig. 1. In some cases, transgender persons recruit one another, forming clusters, but in other cases, transgender persons are recruited by and recruit non-transgender persons. While visually distinct, each chain represent a portion of the same social network; that some chains have more transgender clustering than others is coincidental. Another finding was that transgender persons on average maintain larger personal network sizes (5.2) than their hetero/bisexual (3.8) or gay-identified (4.4) counterparts (Table 3). These characteristics result in over-representation of transgender persons in our data (11%) relative to the estimated proportion of transgender persons in the greater MSM population (9%).
Discussion
HIV prevalence among MSM in San Salvador continues to be disproportionately high compared to national-level prevalence. Persons who self-identify as transgender reported high rates of involvement in commercial sex, sex with casual sex partners, and drug/alcohol use that could make them especially vulnerable to HIV/AIDS. While our data indicate that the transgender population is being reached by HIV prevention interventions, with over 80% reporting participation in an HIV educational session, these activities appear to have limited impact on reducing HIV vulnerability in this population. In addition to providing critical information regarding the HIV vulnerability of the transgender population of San Salvador, this study highlights how data collected using RDS can be used to improve understanding of social network structures.
Our results suggest the need for effective prevention efforts targeting the transgender population in San Salvador that go beyond individual-level outreach to address the broader context surrounding HIV vulnerability. While the few evaluated HIV prevention interventions specifically designed for the transgender population in the US have focused on health education as the core intervention strategy, their lessons learned are still useful to consider. Findings from a health promotion intervention with transgender women in San Francisco stress the importance of creating a safe physical space for community-building and networking as well as the delivery of interventions by transgender peers [36]. The importance of safe space and working with peers has also been identified in research focused on the provision of health care services to the transgender population [5]. Bockting et al. [14] implemented a transgender-specific sexual health seminar in community-based venues in Minneapolis. While these authors reported positive trends in attitudes, self-efficacy and sexual risk behaviors, they emphasized the need to develop alternate intervention models to reach a broader transgender population that may not participate in traditional health education approaches. Taken together, our findings and the literature support the need to expand beyond our traditional health education and health service models to reach the most vulnerable transgender populations with effective HIV prevention programs and sexual health services in an effective manner.
Transgender persons were overrepresented in our data. Overrepresentation of any group in a sample signifies that including members of that group is, for whatever reason, more likely than other groups. In a respondent-driven sample, which relies on network connections as well as individual motivation to recruit participants, overrepresentation suggests that the transgender population forms a densely connected sub-group that is highly motivated to mobilize each other’s participation. Based on these findings, the transgender population in San Salvador could be especially well-suited for programs utilizing network-based recruitment and HIV prevention intervention strategies.
Several models of social network-based HIV prevention interventions involving peers have been associated with changes in HIV risk behaviors among diverse vulnerable populations including MSM [20–22], “at-risk” women [37] and drug users [17–19]. While some variation exists, most social-network based models use ethnographic methods to identify popular members of social networks who are willing to be trained in HIV prevention information and techniques for diffusing HIV protective norms and behaviors within their networks [19]. These approaches go beyond traditional peer education models of health promotion by utilizing natural conversation and existing social structures to facilitate ongoing processes of communication, normative influence and social support [37, 38]. Peers are trained not only in HIV-related information but also in persuasive communication. Such approaches have been designed in response to the social marginalization of the target populations, which can create a lack of trust of outsiders and limit the ability of interventions to reach the most vulnerable [19, 20, 22]. The use of naturally existing social structures may also achieve more sustainable changes beyond the intervention period than traditional peer education approaches by engaging peer leaders to actually change the social environment of high-risk networks and stimulate processes of diffusion and reinforcement [19].
The data presented here were collected using RDS, a sampling and analysis procedure that relies on peer-recruitment to generate a sample. The success of this sample shows the transgender population to be highly receptive to a peer-recruitment scheme. Future research should examine whether the receptivity to peer recruitment would translate into receptivity to peer-driven HIV prevention interventions. In-depth qualitative methods would be particularly well-suited to examine the meaning of cohesion within transgender networks and identify any potential threats to peer driven approaches within these networks. Another area for further research is to improve understanding of the communication patterns within transgender networks to inform the training and intervention strategies. Key questions include how people talk about HIV and what forms of communication are most persuasive and influential among this population. Finally, formative research methods, ideally including both interview and observation-based approaches, should be used to describe the profile of popular and influential social network leaders and to identify effective strategies for reaching these individuals [20].
Another logistical question that will need to be addressed through formative research is how the role of peers should be defined. Some models, such as the Peer-Driven Intervention (PDI) model, employ members of at-risk populations to recruit their peers into interventions and, through a system of incentives, encourage them to educate their peers in prevention practices [39]. This model was developed based on the same principles of RDS. Such an intervention improves retention of HIV prevention information by (1) doubling the number of times each participant is taught the material (once by the recruiter and once by project staff) and (2) by encouraging participants to learn the material well enough to teach it to up to three of their peers. Other models provide compensation for the time in training but do not provide additional monetary incentives to maintain the role clearly as a natural leader rather than an outside educator [19, 20, 38]. The appropriate form of compensation is a critical topic that requires further exploration in the specific context in which the intervention will be implemented.
Our data have several limitations. First and foremost, while our overall sample size (n = 602) is relatively large for such studies, the number of self-identified transgender respondents (n = 67) limits our analysis. Specifically, our data are suggestive, but often fall short of being statistically significant. Second, recent theoretical work on RDS has found that RDS estimates lose accuracy as the sample approaches a census because RDS weighting assumes a small sampling fraction [40]. In studies where the sample approaches a census, the raw sample characteristics provide a better estimate of population characteristics than weighted estimates. Studies focusing on small subsets of minority populations, such as transgender persons, are especially at risk. In our study, weighting tended to reduce differences between the transgender group and other groups (results not shown). Therefore we confidently present the weighted estimates as conservative measures. For interventions where reaching a large portion of a population is ideal, a large sampling fraction is not problematic.
Male-to-female transgender persons in San Salvador are highly vulnerable to HIV and there is an urgent need for HIV prevention strategies that are culturally and contextually relevant and appropriate for this population. Our data suggest engaging with the existing social networks among transgender persons may be an effective way to reach this population to deliver HIV prevention interventions that go beyond HIV prevention education and address the broader social context.
Acknowledgments
This study was funded by the United States Centers for Disease Control and Prevention, United States Agency for International Development, the Ministry of Health of El Salvador and the World Bank. We would like to express our gratitude to the Ministry of Health of El Salvador for leading this study and providing permission to use government health facilities. We would especially like to thank the study staff and the study participants who made this survey possible. We also thanks thank Ron Ballard and Lisa Steele for providing quality control for laboratory testing at the Centers for Disease Control and Prevention STI Laboratory and to Nelly Arguera from the National Laboratory of the Ministry of Health in El Salvador for processing all serological testing locally. Many thanks to Maricarmen Estrada from the United States Agency for International Development, Edgar Monterroso from the Centers for Disease Control and Prevention and Jacob Creswell from del Valle University for their participation and support during the study design and data collection and to Ann Gottert from UNC-Chapel Hill for assisting with the literature review. Thanks to the Panamerican Social Marketing Organization (PASMO) for their collaboration in managing the study. Special thanks to William Hernandez from Entreamigos and Monica Hernandez from Arco Iris for facilitating data collection and dissemination of results.
Contributor Information
Clare Barrington, Department of Health Behavior and Health Education, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, 317 Rosenau Hall, CB #7440, Chapel Hill, NC 27599-7440, USA cbarring@email.unc.edu.
Cyprian Wejnert, Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, GA, USA.
Maria Elena Guardado, Tephinet, Inc., Atlanta, GA, USA.
Ana Isabel Nieto, National AIDS Program, Ministry of Health, San Salvador, El Salvador.
Gabriela Paz Bailey, Center for Health Studies, Del Valle University, Guatemala City, Guatemala; Tephinet, Inc., Atlanta, GA, USA.
References
- 1.MSPAS Situación del VIH/SIDA en El Salvador: Programa Nacional de VIH/SIDA de El Salvador. 2008 [Google Scholar]
- 2.Soto RJ, Ghee AE, Nunez CA, Mayorga R, Tapia KA, Astete SG, et al. Sentinel surveillance of sexually transmitted infections/HIV and risk behaviors in vulnerable populations in 5 Central American countries. J Acquir Immune Defic Syndr. 2007;46(1):101–11. [PubMed] [Google Scholar]
- 3.Beyrer C. Hidden yet happening: the epidemics of sexually transmitted infections and HIV among men who have sex with men in developing countries. Sex Transm Infect. 2008;84(6):410–2. doi: 10.1136/sti.2008.033290. [DOI] [PubMed] [Google Scholar]
- 4.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 5.DeSantis HIV infection risk factors among male-to-female transgender personas: a review of the literature. J Assoc Nurses AIDS Care. 2009;20(5):362–72. doi: 10.1016/j.jana.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 6.PSI Interpersonal Communication at PSI. 2006 Available from: http://www.aidsmark.org/intervention/ipc-brochure.pdf.
- 7.PASMO Perfil PASMO. 2009 Available from: http://www.comunitatis.com/pasmorg/pdf/Perfil_09.pdf.
- 8.UNAIDS El Salvador: Ministerial decree to reduce homophobia in health services 2009. http://www.unaids.org/en/Resources/PressCentre/Featurestories/2009/April/20090403MinisterialDecreeSalvador.
- 9.Nemoto T, Sausa LA, Operario D, Keatley J. Need for HIV/AIDS education and intervention for MTF transgenders: responding to the challenge. J Homosex. 2006;51(1):183–202. doi: 10.1300/J082v51n01_09. [DOI] [PubMed] [Google Scholar]
- 10.Reisner SL, Mimiaga MJ, Bland S, Mayer KH, Perkovich B, Safren SA. HIV risk and social networks among male-to-female transgender sex workers in Boston, Massachusetts. J Assoc Nurses AIDS Care. 2009;20(5):373–86. doi: 10.1016/j.jana.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulden JD, Song B, Barros A, Mares-DelGrasso A, Martin CW, Ramirez R, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep. 2008;123(Suppl 3):101–14. doi: 10.1177/00333549081230S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.PSI El Salvador (2007): Estudio TRaC de VIH/SIDA entre hombres que tienen sexo con hombres en San Salvador, Sonsonate, Santa Ana, San Miguel y La Paz. 2008 [Google Scholar]
- 13.Sevelius JM, Reznick OG, Hart SL, Schwarcz S. Informing interventions: the importance of contextual factors in the prediction of sexual risk behaviors among transgender women. AIDS Educ Prev. 2009;21(2):113–27. doi: 10.1521/aeap.2009.21.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bockting WO, Robinson BE, Forberg J, Scheltema K. Evaluation of a sexual health approach to reducing HIV/STD risk in the transgender community. AIDS Care. 2005;17(3):289–303. doi: 10.1080/09540120412331299825. [DOI] [PubMed] [Google Scholar]
- 15.Melendez RM, Pinto RM. HIV prevention and primary care for transgender women in a community-based clinic. J Assoc Nurses AIDS Care. 2009;20(5):387–97. doi: 10.1016/j.jana.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinto RM, Melendez RM, Spector AY. Male-to-female trans-gender individuals building social support and capital from within a gender-focused network. J Gay Lesbian Soc Serv. 2008;20(3):203–20. doi: 10.1080/10538720802235179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Broadhead RS, Heckathorn DD, Weakliem DL, Anthony DL, Madray H, Mills RJ, et al. Harnessing peer networks as an instrument for AIDS prevention: results from a peer-driven intervention. Public Health Rep. 1998;113(Suppl 1):42–57. [PMC free article] [PubMed] [Google Scholar]
- 18.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol. 2003;22(4):332–9. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- 19.Weeks MR, Li J, Dickson-Gomez J, Convey M, Martinez M, Radda K, et al. Outcomes of a peer HIV prevention program with injection drug and crack users: the Risk Avoidance Partnership. Subst Use Misuse. 2009;44(2):253–81. doi: 10.1080/10826080802347677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amirkhanian YA, Kelly JA, Kabakchieva E, Kirsanova AV, Vassileva S, Takacs J, et al. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19(16):1897–905. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- 21.Kelly JA, St Lawrence JS, Stevenson LY, Hauth AC, Kalichman SC, Diaz YE, et al. Community AIDS/HIV risk reduction: the effects of endorsements by popular people in three cities. Am J Public Health. 1992;82(11):1483–9. doi: 10.2105/ajph.82.11.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang H, Wu Z, Zheng Y, Wang J, Zhu J, Xu J. A pilot intervention to increase condom use and HIV testing and counseling among men who have sex with men in Anhui, China. J Acquir Immune Defic Syndr. 2010;53(Suppl 1):S88–92. doi: 10.1097/QAI.0b013e3181c7de63. [DOI] [PubMed] [Google Scholar]
- 23.Salganik MJ, Heckathorn DD. Sampling and estimation in hidden populations using respondent driven sampling. Sociol Methodol. 2004;34:193–239. [Google Scholar]
- 24.Volz E, Heckathorn DD. Probability-based estimation theory for respondent driven sampling. J Off Stat. 2008;24:79–97. [Google Scholar]
- 25.Wejnert C. An empirical test of respondent driven sampling: point estimates, variance, degree measures, and out-of-equilibrium data. Sociol Methodol. 2009;39:73–116. doi: 10.1111/j.1467-9531.2009.01216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnston LG, Malekinejad M, Kendall C, Iuppa IM, Rutherford GW. Implementation challenges to using respondent-driven sampling methodology for HIV biological and behavioral surveillance: field experiences in international settings. AIDS Behav. 2008;12(4 Suppl):S131–41. doi: 10.1007/s10461-008-9413-1. [DOI] [PubMed] [Google Scholar]
- 27.Malekinejad M, Johnston LG, Kendall C, Kerr LR, Rifkin MR, Rutherford GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS Behav. 2008;12(4 Suppl):S105–30. doi: 10.1007/s10461-008-9421-1. [DOI] [PubMed] [Google Scholar]
- 28.Creswell J, Guardado ME, Molina G, Hernandez W, Bellare N, Batres J, et al. Informe Final. San Salvador, El Salvador; 2008. Evaluacion formative de las experiencias de los trabajadores sexuales para informar la encuesta de comportamientos en San Salvador y San Miguel. [Google Scholar]
- 29.UVG Pilot study using audio computer-assisted self-interviewing (ACASI) methodology in the following vulnerable populations: sex workers, MSM, people living with HIV/AIDS and Garifuna in three areas in Guatemala. Guatemala City: Centro de Estudios para la Salud Universidad del Valle de Guatemala. 2005 [Google Scholar]
- 30.UNAIDS . UNGASS guidelines on construction of core indicators. UNAIDS; Geneva: 2009. [Google Scholar]
- 31.Volz E, Wejnert C, Degani I, Heckathorn DD. Respondent driven sampling analysis tool (RDSAT) Cornell University; Ithaca: 2007. version 5.6. [Google Scholar]
- 32.Heckathorn DD. Respondent driven sampling II: deriving valid population estimates from chain referral samples of hidden populations. Soc Probl. 2002;49:11–34. [Google Scholar]
- 33.McPherson M, Smith-Lovin L, Cook JM. Birds of a feather: homophily in social networks. Annu Rev Sociol. 2001;27:415–44. [Google Scholar]
- 34.Wejnert C. Social network analysis with respondent-driven sampling data: a study of racial integration on campus. Soc Netw. 2010;1(32):112–24. doi: 10.1016/j.socnet.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci USA. 2010;107(15):6743–7. doi: 10.1073/pnas.1000261107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nemoto T, Operario D, Keatley J, Nguyen H, Sugano E. Promoting health for transgender women: Transgender Resources and Neighborhood Space (TRANS) program in San Francisco. Am J Public Health. 2005;95(3):382–4. doi: 10.2105/AJPH.2004.040501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramos RL, Ferreira-Pinto JB, Rusch ML, Ramos ME. Pasa la voz (spread the word): using women’s social networks for HIV education and testing. Public Health Rep. 2010;125(4):528–33. doi: 10.1177/003335491012500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelly JA. Popular opinion leaders and HIV prevention peer education: resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16(2):139–50. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- 39.Heckathorn DD, Broadhead RS, Anthony DL, Weakliem DL. AIDS and social networks: HIV prevention through network mobilization. Sociol Focus. 1999;32:159–79. [Google Scholar]
- 40.Gile KJ, Handcock MS. Respondent driven sampling: an assessment of current methodology. Sociol Methodol. 2010;40:285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]