Abstract
The SFjRO was created ten years ago to promote radiation oncology teaching in France. Our society has now more than 120 members from all around the country. Each year, two national courses are organized where all members are invited.
Keywords: French Young Radiation Oncologists, Teaching, Courses
1. Learning radiation therapy in France
1.1. Radiation therapy residency
Residency in oncology takes five years in France. Each resident has already studied medicine for six years before, making the total time of eleven years to complete their education. During that time, we receive courses about general oncology: cellular and molecular biology, genetics, pharmacology, medical imaging, stem cells, cell death, oncogenesis, immunity, angiogenesis, pathology, epidemiology, and chemotherapy. Specific courses about radiophysics, radiobiology, brachytherapy and radiation therapy innovations are also mandatory.
We must also complete a precise scheme for practical teaching that includes: f our semesters in radiation oncology departments, two semesters in medical oncology departments, four semesters in at least two departments approved for radiation oncology teaching such as nuclear medicine, medical imaging or pathology departments.
1.2. Demographics
During the national courses organized by the French Society of Young Radiation Oncology (SFjRO) and the French Society of Radiation Oncology (SFRO), surveys are performed yearly to analyse demography and quality. Between 2000 and 2003, 50 radiation oncologists were being trained in the whole country (about 15 per year were graduating).1 This number has increased each year to reach 75 residents in 2005 and around 120 in 2011. Men and women currently account for 48.5% and 51.5%, respectively.2 This number is still insufficient compared to the ever-increasing need for oncologists in a country such as France, where cancer prevalence should rise in the coming years, mainly due to the aging of population.
Overall, even with this recent increase in the number of young radiation oncologists, the demographic evolution of radiation oncologists only partially covers future needs.
In 2005, the first prospective study was performed among French residents: 60% of the young radiation oncologists chose it because they had already been in an oncology department before the residency.2 Students were also asked to give their point of view on the quality of the practical and theoretical training. Some needs were emphasised, such as: (1) the quality of the follow-up during the training (importance of the recent implementation of a logbook); (2) importance of theoretical and practical training in the radiotherapy department; (3) support and incentive for research and scientific publication.
Since that time, a web-based logbook system has been created for the oncology residency (both medical and radiation oncology)3 giving resident a protected and private web page with their courses program, practical training information and goals, ongoing research and curriculum vitae.
In 2008, a qualitative analysis of practical and theoretical training was performed using a visual analogical scale. The practical training received a 5.6 score, while theoretical education was scored 6.1. An analysis of the motivations for choosing the radiation oncology speciality demonstrates interests for innovation, technology, imaging and research.
By the end of 2010, twenty-seven residents graduated (16 in 2008 and 42 in 2009). Usually, a postgraduate position is necessary to complete their training as assistant professor in a university hospital or a cancer centre. Each position must be kept for at least two years for validation. However, only 36 assistant professor positions are available in France, representing half of the demand. In 2008, only 21 residents out of 104 already have a position as assistant professors. The availability of such a position remains unknown for the rest of them. Most of the remaining residents decide to pursue a career in a private practice. With the recent increase in the number of residents in radiation oncology in France, the need to create new assistant professor positions is crucial to assure quality of training for this both medical and technical speciality.
2. The French Society of Young Radiation Oncologists
2.1. History of our society
Since 2002, the SFjRO works with the SFRO (French Society of Radiation Oncologists), the CNEC (National Board of Oncology Teachers) and the INCa (National Cancer Institute) in order to improve teaching of radiation oncology in France.
Membership is free.
2.2. Missions
The goals of our society are to promote and ease the teaching of radiation oncology by developing relationships between residents and professors. By creating specific tools, giving access to scientific journals and organizing each year two theoretical courses, the SFjRO aims to give access to a better understanding of current practices in Radiation Oncology.
2.3. National courses
Our society organizes the National Radiation Therapy Courses, with a 4 year cycle, covering each fundamental fields of radiation oncology: radioanatomy (Paris, 2009), radiobiology (Lille, 2010), radiophysics (Avignon, 2011) and brachytherapy (Nancy, 2012). Each year, 120 radiation oncology residents from all around France are invited to attend our courses.
Each year, a summer school is organized and dedicated to a specific organ: head and Gynecology (Lille, 2008), Head & Neck (Tours, 2009), Sarcoma & Glioma (Bordeaux, 2010) and lung (Lyon, 2011).
2.4. French Society of Radiation Oncology Annual meeting
Our society also participates to the SFRO annual congress with delineation workshops. We have also created a Young Session, which allows 6 residents to present about a specific subject, gathering more and more young radiation oncologists each year. The best oral communication wins a travel to Canada to represent French residents in Québec for the national annual meeting.
2.5. Links to other societies
We cooperate with other young radiation oncologists’ societies throughout the world in order to create European and international exchanges. In Gothenburg (2008), the Young Scientist Session was created at the ESTRO (European Society for Therapeutic Radiology and Oncology) annual congress and has since been renewed each year (2009, Berlin and 2010, Barcelona).
3. Published studies
One of the purposes of the SFjRO is to stimulate research among young radiation oncologists. We have therefore published several studies and are working on new ones.
3.1. Delineation variability
During the French national course of radioanatomy, an expert and 120 residents were asked to use delineation stations to created three volumes of interest: GTV, CTV and PTV. They were also asked to prescribe the treatment dose. We performed a comparative study of delineation and doses prescribed for a clinical case of lung carcinoma before and after the completion of our theoretical courses. Residents were divided in 30 groups. Artiview (Aquilab SAS) was used to calculate the volume ratio (VR), common volume (CV), additional volume (AV), kappa (K) and overlap (OV) between the different volumes of interest. A comparative study by a test of Student for paired series was performed. The GTV was 89.1 cm3 for the expert, 103.4 cm3 (59.9–215.2 cm3) before versus 99.5 cm3 (39.7–202.3 cm3) after the courses for residents. The median margin prescribed to obtain CTV from GTV was 6 mm (5–10 mm), no change was noticed after the course. The expert prescribed a 6 mm margin. The median margin prescribed by the participants to obtain PTV from CTV was 7 mm (3–15 mm) before the course and 5 mm (3–15 mm) after, versus 5 mm for the expert. The dose prescribed by the expert was 66 Gy on PTV. The dose was 66.2 Gy (60–70 Gy) before and 66.5 Gy (64–70 Gy) after course for residents. No significant volume modification was found after the courses. We noticed, however, a tendency to increase the prescribed dose as well as a reduction of the delineated volume. Full results are available in the paper published in the French Society of Radiation Oncology Journal.4
3.2. Dosimetric consequences of the delineation variability
Following this study, we published a second paper about the dosimetric consequences of the delineation differences5: an increased dose to the lung as found for the residents compared to the experts (V20: 23.2% versus 36.5%) due to the larger PTV delineated. No significant difference was observed for other organs at risk. There were no significant differences for the delineation of the GTV and CTV before and after the course, although the differences tended to decrease after the course. The good initial quality of the contours could explain the lack of difference. V20 for the lung was higher in the residents group compared to the experts group (23.2% versus 36.5%). No other treatment planning consequences were observed for other critical organs.
3.3. Burn-out
While the social and psychological burden of cancer has already been the subject of studies,6 our society wanted to work on the prevalence and causes of burn-out syndrome among radiation oncology residents. In 2009, we designed and performed an anonymous survey, which was sent to every medical or radiation oncology or haematology resident in France (n = 340). An anonymous questionnaire was sent out to every medical or radiation oncology or haematology resident in France (n = 340). It included demographical data, burnout level (Maslach Burnout Inventory), sources of stress, sense of equity at work, sources of support, and general health questions. The response rate was 60% (204/340). Emotional exhaustion (EE) and Depersonalisation (DP), the major components of burnout, were reported, respectively, by 26% (n = 53) and 35% (n = 72) of the residents. Burnout prevalence was 44% (n = 89). The burnout level was not significantly different between the three specialties. Full results of the study were published in English in the European Journal of Cancer.7
This study showed that the burnout level is high amongst oncology residents and that improvements are needed to prevent and/or treat it. Discussions are currently underway to create and increase in the availability throughout France of support groups and more intense coaching by senior physicians.
4. Internet
4.1. Website creation
Since 2008, our society has created and maintained a website for all our members. In 2011 it was updated with a Community Manager System (Joomla) to provide easier updates and regular content improvement. The website is available in French, free of charge after registration. Any person working in the field of radiation oncology can register: from medical student to professor, physicist and RTTs.
4.2. Website content
The website has a database of courses covering radiophysics, radiobiology, brachytherapy, radioanatomy and cancer treatment for all primaries. Members can search and access them for free. Another part, available in French, English, German and Spanish is a biologically equivalent dose calculator created by our society. The website also features the latest news in radiation oncology in France and a calendar of the upcoming international and national scientific meetings.
Since June 2011, we have also created a radiation oncology newsletter featuring abstracts from the latest published papers. This newsletter is sent to over 300 members.
4.3. Visits
Since March 2011, the website has received over 11 000 visits with 46 000 pageviews from 96 countries, mainly France, the United States, Algeria, Marocco and Tunisia.
5. Biologically equivalent dose calculator: eLQ
SFjRO has created an iPhone application allowing for calculation of biologically equivalent doses in clinical radiotherapy using the linear-quadratic model. In November 2010, an English version was made available and downloaded since by more than 1700 people from all over the world (United States, United Kingdom, Germany, The Netherlands, etc.). It is available on iOS for iPhone, iPod Touch, and iPad.
The application was developed in order to provide radiation oncologists with a ready-to-use tool fitting in a lab coat pocket and to sensitize young radiation oncologists to radiobiology and the influence of fractionation. It was created using Apple's Xcode Developer Tool Technology with the PhoneGap open source framework and jQtouch. It is the first free calculator that is academically supported by the French Society of Radiation Oncology (SFRO).
The user can choose an organ at risk or a predefined α/β value, and enter total prescribed dose, initial dose per fraction, and new dose per fraction (Fig. 1). The equivalent dose is then calculated. Alerts based on linear-quadratic model limitations and dose constraints for each organ are activated. Since the validity of the linear-quadratic model has only been established for doses per fraction between 1 and 6–8 Gy, our application should not be used for largely hypofractionated regimens. Additionally, we have not included correction for incomplete repair between fractions or for cell proliferation; our application should not be used when the interval between 2 treatment sessions is shorter than 6–8 h or in the case of accelerated treatments.
Fig. 1.
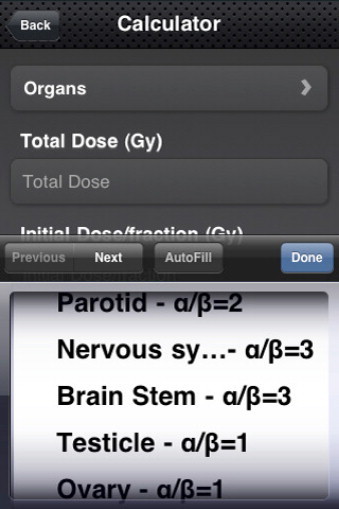
Screenshot from eLQ, the biologically equivalent dose calculator.
6. Siriade
The SFjRO, in parternship with the AFCOR (Association for In-Service Training) and the SFRO (French Society of Radiation Oncology) has developed a free radio-anatomy website for volumes delineation for radiation-oncologists (www.siriade.org). A search engine allows access to delineation characteristics of main tumours illustrated with clinical cases. However, its purpose is not to provide guidelines but a simple iconographic training support.
In 2012, a version of the atlas will be available for both the iPhone (Siriade) and the iPad (Siriade HD).
Conflict of interest
None declared.
References
- 1.Kantor G., Huguet F., Toledano A. Radiation oncology training in France: demography, analysis of motivations of the young specialists, evaluation of the training. Cancer Radiother. 2005;9(November (6–7)):435–443. doi: 10.1016/j.canrad.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 2.Dewas S., Pointreau Y., Rivera S. Demography of radiation oncology residents in France in 2008: current situation and perspectives for the next three years. Cancer Radiother. 2009;13(June (3)):153–160. doi: 10.1016/j.canrad.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Logbook de l’interne d’oncologie |CNEC| INCA [Internet]. Available de: /[cité 30.11.11].
- 4.Dewas S., Vautravers-Dewas C., Blanchard P. Delineation variation of lung cancer in conformal radiotherapy among radiation oncology residents after an educational course: a prospective study. Cancer Radiother. 2010;14(April (2)):103–110. doi: 10.1016/j.canrad.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Dewas S., Bibault J.-E., Blanchard P. Delineation in thoracic oncology: a prospective study of the effect of training on contour variability and dosimetric consequences. Radiat Oncol. 2011;6:118. doi: 10.1186/1748-717X-6-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernad D., Zysnarska M., Adamek R. Social support for cancer – selected problems. Rep Pract Oncol Radiother. 2010;15(2):47–50. doi: 10.1016/j.rpor.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blanchard P., Truchot D., Albiges-Sauvin L. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer. 2010;46(October (15)):2708–2715. doi: 10.1016/j.ejca.2010.05.014. [DOI] [PubMed] [Google Scholar]


