Abstract
Purpose
To present the preliminary psychometric properties of the Psychosocial Assessment Tool 2.0_General (PAT2.0_GEN), a brief screener for psychosocial risk in families of children with Inflammatory Bowel Disease (IBD).
Methods
Caregivers of forty-two youth with IBD were recruited and administered a battery of measures including the PAT2.0_GEN and well-validated measures of child emotional and behavioral functioning at baseline and at a 6-month follow-up.
Results
Internal consistency for the PAT2.0_GEN Total score was good (α=.82). Baseline was significantly associated with the 6-month follow-up (r = .79, p < .001). Significant correlations between the baseline PAT2.0 _GEN total score and caregiver-reported Child Behavior Checklist (CBCL) total scores at baseline (r = .74, p < .001) and at a 6-month follow-up (r = .62, p < .001) support the content and predictive validity of the PAT2.0_GEN. Baseline PAT2.0_GEN was also significantly correlated with youth-reported CBCL total scores at baseline (r = .37, p = .02) but not at the six-month follow-up (r = .23, p = .17).
Conclusion
A number of indicators support the concurrent and predictive utility of the PAT2.0_GEN. The PAT2.0_GEN is a promising tool for screening psychosocial risk that could facilitate the provision of psychosocial services to those patients most in need.
Keywords: Inflammatory Bowel Disease, Child, Family, Assessment, Psychosocial Risk, Psychological Distress
Inflammatory bowel disease (IBD) is a chronic condition that is characterized by an intermittent and unpredictable disease course and a heterogeneous constellation of symptoms that includes abdominal pain, recurrent diarrhea, growth delay, and perianal disease 1. Unfortunately, psychosocial distress is also common among youth with IBD and their families. Youth with IBD experience high rates of psychological maladjustment (60%)2; 3 including depression (18-25%)4-6 and anxiety disorders (28%)7. Rates of parental psychological distress and greater family dysfunction are higher in families of youth with IBD when compared to healthy controls7; 8 and have been associated with significant medical and emotional outcomes of youth with IBD (i.e., increased functional disability, depressive symptoms, and frequency of bowel movements8-10). Thus, the high rates of psychological distress and family dysfunction are serious clinical concerns and have profound implications for the long-term psychological and physical well-being of these youth.
As such, there is a critical need for routine screening, assessment and management of the psychosocial needs of pediatric IBD patients and their families. Unfortunately, most IBD clinics have limited resources to implement comprehensive psychosocial screening programs. Therefore, the first step to providing more consistent and comprehensive evidence-based psychosocial care to youth with IBD is the development of a validated, standardized screening instrument that can efficiently and effectively assess the psychosocial risk of youth with IBD and their families in the context of clinical practice. The Psychosocial Assessment Tool 2.0_General (PAT2.0_GEN;11-13), completed by the patient’s caregiver (i.e., parent or legal guardian), is one such brief standardized screening instrument of psychosocial risk. It screens a broad range of patient and family needs that includes everything from financial resources to behavioral concerns. The majority of existing measures do not screen for the structural, financial, and family issues that may impact behavioral, emotional and health outcomes of the patient.
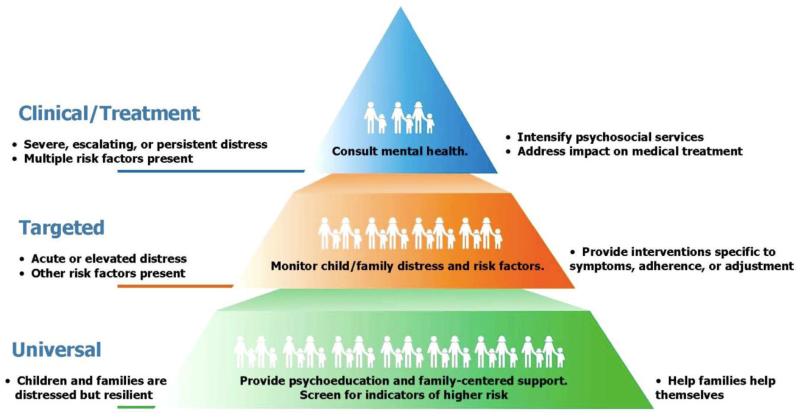
The availability of an assessment tool like the PAT2.0_GEN could facilitate the identification of youth with IBD in need of psychosocial services and for whom the promotion of psychosocial functioning is crucial for optimizing medical outcomes. The PAT2.0_Gen scores can be used to categorize patients and families into the Pediatric Psychosocial Preventative Health Model (PPPHM). The PPPHM is a parsimonious, yet comprehensive approach to conceptualizing psychosocial risk1 in pediatric populations. The PPPHM is depicted as a pyramid with three horizontally oriented risk categories: Universal (base of the pyramid), Targeted (middle of pyramid) and Clinical (apex of the pyramid)14; 15. Please see Figure 1. The level of risk for experiencing difficulties either in managing a pediatric chronic illness or other life demands is lowest in the Universal category and highest in the Clinical category. Previous studies have found the majority of families fall into the Universal risk category (55-67%), fewer score in the Targeted category (32%) and the fewest number score in the Clinical risk category (1-13%)13.
Figure 1. The Pediatric Psychology Preventative Health Model.
© 2005, 2010, Center for Pediatric Traumatic Stress, Anne E. Kazak, Ph.D., ABPP, The Children’s Hospital of Philadelphia.
Therefore, the availability of a valid psychosocial risk screening tool such as the PAT2.0_GEN could increase the feasibility of regular monitoring of psychosocial functioning, standardize the assessment methods used to identify patient’s psychosocial needs, quickly and reliably identify patients in need of psychosocial services, and allow medical teams to more effectively allocate psychosocial resources to those patients most in need.
The PAT2.0_GEN has demonstrated high reliability and substantial content and predictive validity in other pediatric populations (e.g., kidney transplant). However, the psychometric properties of the measure have not been assessed in pediatric IBD. Several characteristics of the pediatric IBD population (e.g., intermittent course, high base rates of psychological and family dysfunction, stigmatizing nature of symptoms) distinguish it from the other pediatric populations (e.g., cancer, transplant)13; 16 for which the psychometric properties of the PAT2.0_GEN have been evaluated. As such, the psychometrics of the PAT2.0_GEN must be evaluated in the IBD population prior to clinical use. Therefore, the purpose of this study is to evaluate the psychometric properties of PAT2.0_GEN in a pediatric IBD sample. Reliability, convergent, and predictive validity of the PAT2.0_GEN will be evaluated.
Method
Participants
Caregivers of 42 children diagnosed with Crohn’s disease, ulcerative colitis, or indeterminate colitis, collectively IBD, participated as a part of a larger study examining psychosocial factors related to IBD. Inclusion criteria were 1) patient age 13-17 years, 2) confirmed diagnosis of IBD for at least 6-months, 3) English fluency, and 4) current prescription of oral mesalamine and/or immunomodulator medication (required by larger study). Exclusion criteria were 1) diagnosis of a neurocognitive disorder or other chronic illness, and 2) corticosteroid treatment prescribed at greater than 1mg/kg/day (to remove confounding treatment-related psychiatric symptoms)17; 18.
Procedures
This study was approved by the institutional review board at the hospital where the study was conducted. Potential participants were identified from the outpatient IBD clinic schedule. After agreeing to hear about the study, patients and their caregivers were approached by study staff. Informed consent and parental permission was obtained from caregivers and assent was obtained from patients who agreed to participate. Measures were administered at baseline and 6-month follow-up. Caregivers and patients received modest compensation for participation.
For this study, 74 patients met inclusion/exclusion criteria, however, two were no longer eligible at time of recruitment, six were unable to be contacted for follow-up after initial recruitment, and 15 declined participation. Reasons provided for declining participation were as follows: did not like research/uninterested in research (n=6), family too busy (n=4), did not want blood draw as part of the larger study (n=3), did not want to complete questionnaires (n=1), and only came to hospital once a year (n=1). The remaining 51 patients agreed to participate in the study. Of those that consented to participate, one participant withdrew immediately after consenting (participant did not have enough time to participate), seven participants were excluded from these analyses because the PAT2.0_GEN was not completed at 6-month follow-up, and one participant was excluded from analyses due to a change in reporter (i.e., a different caregiver completed follow-up). Thus, the final sample consisted of 42 participants.
Measures
Demographic questionnaire
Parents provided information at baseline regarding family education, caregiver marital status, and child age, ethnicity, household income, and gender via a brief questionnaire.
Psychosocial Assessment Tool 2.0_General (PAT2.0_GEN)
The PAT2.0_GEN was administered to 42 primary caregivers (35 mothers, 6 fathers, 1 adoptive mother). A Total score (with a potential range of 0-7) and seven subscale scores (with a potential range of 0-1) were calculated according to scoring described in the PAT2.0 Scoring Manual13; 19. Consistent with the original PAT2.0, the PAT2.0_GEN was comprised of the following subscales: Family Structure and Resources, Family Social Support, Family Problems, Parent Stress Reactions, Child Problems and Sibling Problems. Previous studies have used the following cutoffs to categorize family psychosocial risk scores: a) below one fall in the he Universal risk category, b) scores between one and two fall in the Targeted category, and c) scores higher than two are considered to fall in the Clinical risk category13. Completion time for the PAT2.0_GEN is approximately 5-10 minutes. The PAT2.0_GEN only differs from the original PAT2.0 on three items which were removed: item 9 (Does your child know that he/she has cancer?), 15 g “People will pull away from us,” and 15i “Cancer is a death sentence.” There were no missing items on the PAT2.0_GEN for the data included in the analysis.
Child Behavior Checklist (CBCL)20
The CBCL is a measure that assesses the frequency of specific behaviors of a child during the previous 6-months. The CBCL was completed at baseline and 6-month follow-up. Two versions of the CBCL were used in this study - parent-report (113-items) and age appropriate youth-report (118-items). The CBCL is a widely used, empirically validated and reliable measure of general child psychosocial distress. It yields total scores for competence (e.g., activities, school, social skills) and problem (e.g., symptoms of depression, anxiety, delinquent behavior) subscales.
Statistical Analyses
Analyses were conducted in four steps. First, traditional descriptive statistics were calculated for all study measures. Second, internal consistency was computed for the PAT2.0_GEN total and subscales. Kuder-Richardson-20 (KR-20) coefficients were computed as measures of internal consistency due to the dichotomous nature of the item level scoring (i.e., risk/no risk). The Spearman correlations were used to provide and initial assessment of the PAT2.0_GEN over time. Two types of validity were assessed on the PAT2.0_GEN: convergent and predictive validity. Convergent validity was assessed by calculating Spearman correlations between the PAT2.0_GEN Total score and caregiver- and youth-reported CBCL Internalizing, Externalizing and Total scores. To assess predictive validity, Spearman correlations were computed between the baseline PAT2.0_GEN Total score and CBCL Internalizing, Externalizing and Total scores at the 6-month follow-up. Based on the evidence obtained in previous studies with the pediatric oncology and nephrology populations, we hypothesized that the internal consistencies for the total score will be equal to or greater than 0.80 for the total score and equal to or greater than 0.70 for subscale scores evaluated13. We also hypothesized that the PAT2.0_GEN total score would be significantly and positively correlated with the selected CBCL scores. The criterion for statistical significance for all analyses was held constant at the α = 0.05 level. All data were analyzed using SPSS Version 19 software.
Results
Descriptive Statistics
Descriptive statistics were calculated for demographic, medical and psychosocial utilization information and are reported in Table 1. The mean age of the caregivers who completed the PAT2.0_GEN was 46.42 years (SD = 6.23 years) and the mean age of the patients was 14.96 years (SD = 1.51 years). The sample was representative of the population in terms education, the majority of mothers and fathers held either a 4 year degree or graduate degree (mothers – 33% and 26.2%, respectively; fathers – 21.4% and 21.4%, respectively), and the majority of the sample (n=10, 24.4%) endorsed a yearly income ranging from $100,001-125,000. PAT2.0_GEN Total and subscale descriptive statistics are reported in Table 2. The PAT2.0_GEN scores did not differ by income or educational background of mothers or fathers (p’s >.10). PAT2.0_GEN scores were used to categorize patients into the Universal (64%; 76%), Targeted (36%; 19%) and Clinical (0%;5%) PPPHM categories for baseline and the 6-month follow-ups respectively. CBCL Total and subscale t-scores are reported in Table 3.
Table 1. Demographics and Diagnoses for Study Sample (n = 42).
| Variable | Frequency (%) |
|---|---|
| Gender (Males) | 21 (50.00) |
| Ethnicity | |
| Caucasian | 40 (95.20) |
| African American | 2 (4.80) |
| Two-Caregiver Households | 37 (88.00) |
| Caregiver Educational Background | |
| High school education or less | 7(16.70) |
| College courses or degrees | 24(57.10) |
| Some postgraduate education | 11 (26.20) |
Table 2. Descriptive Statistics and Internal Consistency for PAT2.0_GEN Total Scores and Subscales (n = 42).
| Time 1 | Time 2 | ||||||
|---|---|---|---|---|---|---|---|
| PAT2.0_GEN Scale (Items) | Range | M | SD | α | M | SD | α |
| Total | 0-7 | .77 | .48 | .82 | .65 | .56 | .87 |
| Structure/Resources (1b-d, f, education, 5, 7, 8) |
0-6 | .74 | 1.06 | .57 | .49 | .81 | .45 |
| Social Support (4a-d) | 0-4 | .10 | .37 | .44 | .00 | .00 | .00 |
| Child Problems (10a-n, p) | 0-13 | 2.81 | 2.54 | .75 | 2.76 | 2.75 | .80 |
| Sibling Problems (11a-n, p) | 0-14 | 1.34 | 1.97 | .76 | 1.21 | 1.98 | .78 |
| Family Problems (12a-j) | 0-7 | 1.27 | 1.50 | .66 | .93 | 1.52 | .76 |
| Stress Reaction (14a-c) | 0-3 | .00 | .00 | -- a | .21 | .19 | -- a |
Note. Internal consistency estimates were calculated using Kuder-Richardson-20 formula based on data provided by the caregiver.
Reliability was not calculated due to lack of variance on these subscales.
Table 3. Descriptive Statistics for CBCL Total and Subscales T-scores.
| CBCL Scale | Borderline Range |
Clinical Range |
Time 1 | Time 2 | |||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Delinquent Behavior |
Caregiver | 65-69 | > 69 | 52.10 | 3.91 | 51.97 | 4.29 |
| Youth | 51.86 | 3.37 | 52.58 | 4.61 | |||
| Aggressive Behaviors |
Caregiver | 65-69 | > 69 | 53.76 | 6.29 | 53.37 | 5.68 |
| Youth | 53.05 | 4.89 | 53.00 | 5.48 | |||
| Withdrawn | Caregiver | 65-69 | > 69 | 56.21 | 9.14 | 55.16 | 8.60 |
| Youth | 53.52 | 4.75 | 52.95 | 3.79 | |||
| Somatic Complaints |
Caregiver | 65-69 | > 69 | 58.26 | 7.91 | 58.76 | 8.77 |
| Youth | 53.60 | 4.45 | 54.34 | 6.63 | |||
| Anxious / Depressed |
Caregiver | 65-69 | > 69 | 55.12 | 6.22 | 54.13 | 6.80 |
| Youth | 53.60 | 4.75 | 54.21 | 5.50 | |||
| Social Problems |
Caregiver | 65-69 | > 69 | 53.64 | 5.91 | 53.18 | 5.20 |
| Youth | 53.90 | 5.03 | 53.45 | 5.94 | |||
| Thought Problems |
Caregiver | 65-69 | > 69 | 54.48 | 5.31 | 53.97 | 5.60 |
| Youth | 53.71 | 5.47 | 53.29 | 5.92 | |||
| Attention Problems |
Caregiver | 65-69 | > 69 | 53.76 | 6.29 | 54.45 | 8.45 |
| Youth | 53.33 | 6.61 | 54.42 | 7.70 | |||
| Externalizing Problems |
Caregiver | 60-63 | > 63 | 47.38 | 9.94 | 45.79 | 10.78 |
| Youth | 46.36 | 8.64 | 46.79 | 10.12 | |||
| Internalizing Problems |
Caregiver | 60-63 | > 63 | 53.24 | 11.53 | 51.71 | 12.09 |
| Youth | 48.74 | 9.06 | 49.37 | 9.61 | |||
| Total Problems |
Caregiver | 60-63 | > 63 | 49.36 | 11.55 | 47.42 | 12.90 |
| Youth | 47.24 | 10.30 | 47.82 | 10.41 | |||
Delinquent Behavior, Aggressive Behaviors, Withdrawn, Somatic Complaints, Anxious/Depressed, Social Problems, Thought Problems, Attention Problems, Externalizing Problems (includes Delinquent and Aggressive Behaviors), Internalizing Problems (includes Withdrawn, Somatic Complaints, and Anxiety/Depressed Problems), and Total Problems
Reliability
Internal consistency is one indicator of the degree to which a set of items are assessing the same construct. An α > .60 is considered acceptable preliminary internal consistency for subscales (i.e., Ware et al., 1980). Internal consistency for the PAT2.0_GEN total score was high (α = .83, See Table 2). The Child Problems, Sibling Problems and Family Problems subscales of the PAT2.0_GEN had KR-20 coefficients ranged between .66 - .76 (.75 Child Problems, .76 Sibling Problems, and .66 Family Problems). However, internal consistency for the Structure and Resources, Social Support and Stress Reaction subscales were unacceptably low (α’s = no variance in Stress Reaction, .57 Structure and Resources, .44 Social Support).
Convergent Validity
To assess convergent validity, Spearman correlations were conducted to determine whether the PAT2.0_GEN Total scores were significantly associated with both caregiver- and youth-reported child emotional and behavioral functioning. Baseline PAT2.0_GEN Total score was significantly associated with baseline caregiver-reported Total Competence and Problem scores on the CBCL. The Child Problems subscale of the PAT2.0_GEN was also significantly correlated with caregiver-reports of Total scores on the CBCL(See Table 4). The PAT2.0_GEN Total score was also significantly associated with youth reported CBCL Total Competence scores and trends were observed between the PAT2.0_GEN Total score and youth reported CBCL Total problems score (r = .30, p =.056).
Table 4.
Spearman Correlations between Psychosocial Assessment Tool 2.0_General Subscales and Caregiver and Youth report of patient’s emotional and behavioral functioning.
| CBCL Time 1 | CBCL Time 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Caregiver | Youth | Caregiver | Youth | |||||
| PAT2.0_GEN | Total Competence |
Total Problems | Total Competence |
Total Problems |
Total Competence |
Total Problems |
Total Competence |
Total Problems |
| Total Time 1 | − .38** | .74*** | −.51*** | .37** | −.27 | .62*** | −.29† | .23 |
| Total Time 2 | −.37** | .55*** | −.38* | .30† | −.34* | .68*** | −.41** | −.30† |
Note. p < .10 (2-tailed),
p < .05 (2-tailed),
p < .01 (2-tailed),
P <.001 (2-tailed).
Predictive Validity
To assess predictive validity, Spearman correlations were conducted to determine whether baseline PAT2.0_GEN Total scores predicted CBCL scores 6-months later. Higher PAT2.0_GEN Total scores were significantly associated with caregiver-reported CBCL Total Problems and Competence scores at the 6-month follow-up ( p’s < .05).
Discussion
Multiple theoretical models have articulated the importance of contextual factors (financial stressors school achievement, family difficulties) on the psychological and health outcomes of children with IBD (21;22;23). However, the feasibility of assessing these factors in a systematic manner is difficult at best in the clinical setting. The high base rates of poor psychological functioning and the consistent association between psychological functioning and medical outcomes in the pediatric IBD population, highlights that the valid and systematic screening of psychosocial risk is central to the comprehensive care of children and adolescents with IBD. This study examines the psychometric properties of the PAT2.0_GEN in an IBD sample; a first step in evaluating the potential clinical utility of the measure. Overall, the findings suggest that PAT2.0_GEN is a promising screener for psychosocial risk in pediatric patients with IBD tool. However, due to the sample size and mixed findings more study will be needed to fully determine the utility of this measure in the pediatric IBD population.
The internal consistency of the PAT2.0_GEN Total, Child Problems, Sibling Problems and Family Problems scores were strong. However, the Structure and Resources, Social Support, and Stress Reaction subscales demonstrated inadequate reliability when examined independently. There are a number of potential explanations for these findings including the small and relatively socioeconomically homogeneous nature of the current sample. Therefore, further study will be needed to determine whether the subscales with low reliability need to be revised or removed from the scale.
Initial concurrent and predictive validity for the PAT2.0_GEN was also established. Consistent with findings in the pediatric nephrology 16 and oncology populations, 11; 13; 24 higher PAT2.0_GEN Total scores were significantly associated with both current and future adaptive functioning and behavioral problems among youth with IBD. In short, the current findings provide initial support for use of the PAT2.0_GEN Total score as a indicator of psychosocial risk with the pediatric IBD population. Notably, a smaller proportion of families fell in the clinical category as indicated by a PAT2.0_GEN score higher than two than observed in other pediatric populations. Studies with larger sample sizes will be needed to determine whether the cutoffs used to classify patients into PPPHM categories are appropriate for the pediatric IBD population.
Clinical Implications
It is important to note that the PAT2.0_GEN should never be used to diagnose psychological problems in patients or used as a comprehensive psychological assessment tool. Rather, it is a screening tool that can serve as an indicator of families who are at risk for having difficulties adapting to their illness and treatment regimen. Further, it can indicate the need for thorough psychological assessment and monitoring the psychosocial needs of patients. With further validation, the PAT2.0_GEN will provide an additional tool to inform clinical decision-making and increase the efficient and most optimal allocation of limited psychosocial resources. For instance, scores could be used to trigger the provision of a higher level psychosocial resources (i.e., psychology referral, social work referral) that may not be delivered as the standard of care as well as identify specific treatment targets (i.e., transportation difficulties, insurance difficulties, patient anxiety, parental anxiety).
Limitations
Although the findings of the current study suggest that the PAT2.0_GEN is a promising screening tool for the pediatric IBD population, several study limitations must be considered. A relatively small sample size limited the conduct of more definitive psychometric analyses such as factor and sensitivity-specificity analyses. In addition, the PAT2.0 was originally conceptualized as a screening tool for use at the time of diagnosis 13 but patients in the current sample had been diagnosed with IBD for at least 6-months. However, testing of the PAT2.0 with other chronic illness populations have shown it to be a reliable and valid measure among patients with varying illness durations. The optimal frequency of psychosocial risk monitoring in the IBD population remains to be empirically assessed. Finally, the validity of the individual subscales should be more thoroughly evaluated with larger and more comprehensive measures of the corresponding constructs.
Future directions
The utility of the PAT2.0_GEN as a routine screening tool is promising. Yet, further empirical evaluation of the psychometric properties of this tool in the IBD is needed. Longitudinal studies are needed to establish the stability of the instrument over time and to determine the optimal frequency of PAT2.0_GEN administration and/or clinical criteria for re-administering the measure (e.g., changes in employment status, changes in family structure, changes in disease activity). Recent studies in the pediatric oncology population found that PAT2.0 scores and the PPPHM categories of families remained fairly stable over time11; 24. Future studies should also examine the sensitivity and specificity of the PAT2.0_GEN. With continued investigation, psychosocial service provision algorithms could be developed that use the PAT2.0_GEN as an initial indicator to tailor evidence-based psychosocial care.
Acknowledgements
Research supported in part by K23 DK079037; PHS Grant P30 DK 078392; Procter and Gamble Pharmaceuticals; USPHS Grant #UL1 RR026314 from the National Center for Research Resources, NIH
Footnotes
“Psychosocial risk is a constellation of individual, family, social, and economic factors that, when considered collectively, increases the likelihood that an individual or their family members will experience difficulties managing the challenges of cancer and its treatment. These difficulties may manifest as psychological symptoms or as diminished academic/professional, social or family functioning of either the patient or a family member.” 13
The PAT2.0 is a copyrighted measure. Permission to use the PAT2.0 or PAT2.0_GEN must be obtained from Dr. Anne Kazak (email: Anne.Kazak@Nemours.org). An example of the original PAT2.0 can be viewed in the article by Pai et al., 200813. The PAT2.0_Gen only differs from the oringinal PAT2.0 illustrated in this article by the removal of the cancer specific items.
Due to the poor reliability of the Family Beliefs subscale in two previous studies13; 16 and relevance of the Family Beliefs items to IBD this subscale was not included in analyses.
Conflicts of interest: None declared.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mackner LM, Sisson DP, Crandall WV. Review: psychosocial issues in pediatric inflammatory bowel disease. Journal of Pediatric Psychology. 2004;29(4):243. doi: 10.1093/jpepsy/jsh027. [DOI] [PubMed] [Google Scholar]
- 2.Engström I. Mental health and psychological functioning in children and adolescents with inflammatory bowel disease: a comparison with children having other chronic illnesses and with healthy children. Journal of Child Psychology and Psychiatry. 1992;33(3):563–582. doi: 10.1111/j.1469-7610.1992.tb00891.x. [DOI] [PubMed] [Google Scholar]
- 3.Szajnberg N, Krall V, Davis P, Treem J, Hyams J. Psychopathology and relationship measures in children with inflammatory bowel disease and their parents. Child psychiatry and human development. 1993;23(3):215–232. doi: 10.1007/BF00707151. [DOI] [PubMed] [Google Scholar]
- 4.Burke P, Meyer V, Kocoshis S, Orenstein DM, CHANDRA R, NORD DJ, COHEN E. Depression and anxiety in pediatric inflammatory bowel disease and cystic fibrosis. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28(6):948–951. doi: 10.1097/00004583-198911000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Szigethy E, Levy-Warren A, Whitton S, Bousvaros A, Gauvreau K, Leichtner AM, Beardslee WR. Depressive symptoms and inflammatory bowel disease in children and adolescents: a cross-sectional study. Journal of pediatric gastroenterology and nutrition. 2004;39(4):395. doi: 10.1097/00005176-200410000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Mackner LM, Crandall WV. Brief report: psychosocial adjustment in adolescents with inflammatory bowel disease. Journal of Pediatric Psychology. 2006;31(3):281. doi: 10.1093/jpepsy/jsj023. [DOI] [PubMed] [Google Scholar]
- 7.Burke PM, Neigut D, Kocoshis S, Sauer J, Chandra R. Correlates of depression in new onset pediatric inflammatory bowel disease. Child Psychiatry & Human Development. 1994;24(4):275–283. doi: 10.1007/BF02353203. [DOI] [PubMed] [Google Scholar]
- 8.Engstrom I. Inflammatory bowel disease in children and adolescents: mental health and family functioning. Journal of pediatric gastroenterology and nutrition. 1999;28(4):S28. doi: 10.1097/00005176-199904001-00004. [DOI] [PubMed] [Google Scholar]
- 9.Wood B, Watkins JB, Boyle JT, Nogueira J, ZlMAND E, CARROLL L. The “psychosomatic family” model: An empirical and theoretical analysis. Family Process. 1989;28(4):399–417. doi: 10.1111/j.1545-5300.1989.00399.x. [DOI] [PubMed] [Google Scholar]
- 10.Tojek TM, Lumley MA, Corlis M, Ondersma S, Tolia V. Maternal correlates of health status in adolescents with inflammatory bowel disease. Journal of psychosomatic research. 2002;52(3):173–179. doi: 10.1016/s0022-3999(01)00291-4. [DOI] [PubMed] [Google Scholar]
- 11.Alderfer MA, Mougianis I, Barakat LP, Beele D, DiTaranto S, Hwang WT, Kazak AE. Family psychosocial risk, distress, and service utilization in pediatric cancer: predictive validity of the Psychosocial Assessment Tool. Cancer. 2009;115(18 Suppl):4339–4349. doi: 10.1002/cncr.24587. [DOI] [PubMed] [Google Scholar]
- 12.Kazak A, Prusak A, McSherry M, Simms S, Beele D, Rourke M, Lange B. The Psychosocial Assessment Tool (PAT)©: Pilot data on a brief screening instrument for identifying high risk families in pediatric oncology. Families, Systems, & Health. 2001;19(3):303–317. [Google Scholar]
- 13.Pai AL, Patino-Fernandez AM, McSherry M, Beele D, Alderfer MA, Reilly AT, Kazak AE. The Psychosocial Assessment Tool (PAT2.0): Psychometric properties of a screener for psychosocial distress in families of children newly diagnosed with cancer. Journal of Pediatric Psychology. 2008;33(1):50–62. doi: 10.1093/jpepsy/jsm053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kazak A. Opportunities for the Future in Family Systems Medicine-Pediatric Psychosocial Preventative Health Model (PPPHM): Research, Practice, and Collaboration in Pediatric Family Systems Medicine. Families Systems and Health. 2006;24(4):381–395. [Google Scholar]
- 15.Health N. I. o. M. Prevention Research. National Insitiute of Mental Health (NIMH); Bethesda, MD: 1998. Priorities for prevention research: A national advisory council workshop on mental health disorders. [Google Scholar]
- 16.Pai ALH, Tackett A, Ittenbach RF, Goebel J. Psychosocial Assessment Tool 2.0 _General: Validity of a psychosocial risk screener in a pediatric kidney transplant sample. Pediatric transplantation. 2011;16(1):92–98. doi: 10.1111/j.1399-3046.2011.01620.x. [DOI] [PubMed] [Google Scholar]
- 17.Kayani S, Shannon DC. Adverse Behavioral Effects of Treatment for Acute Exacerbation of Asthma in Children*. Chest. 2002;122(2):624–628. doi: 10.1378/chest.122.2.624. [DOI] [PubMed] [Google Scholar]
- 18.Soliday E, Grey S, Lande MB. Behavioral effects of corticosteroids in steroid-sensitive nephrotic syndrome. Pediatrics. 1999;104(4):e51–e51. doi: 10.1542/peds.104.4.e51. [DOI] [PubMed] [Google Scholar]
- 19.PAT2.0 Scoring Manual. 2008. [Google Scholar]
- 20.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Univeristy of Vermont, Department of Psychology; Burlington, VT: 1991. [Google Scholar]
- 21.Bronfenbrenner U. The ecology of human development. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- 22.Kazak AE. Pediatric Psychosocial Preventative Health Model (PPPHM): Research, practice, and collaboration in pediatric family systems medicine. Families, Systems, & Health. 2006;24(4):381. [Google Scholar]
- 23.Modi AC, Pai ALH, Hommel KA, Hood KK, Cortina S, Hilliard ME, Drotar D. Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129(2):e473–485. doi: 10.1542/peds.2011-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McCarthy M, Clarke N, Vance A, Ashley D, Heath J, Anderson V. Measuring psychosocial risk in families caring for a child with cancer: The psychosocial assessment tool (PAT2. 0) Pediatric Blood & Cancer. 2009;53(1):78–83. doi: 10.1002/pbc.22007. [DOI] [PubMed] [Google Scholar]