Summary
Background
Kidney disease is under-documented in physician notes. The use of template-guided notes may improve physician recognition of kidney disease early in training.
Objective
The objective of this study was to determine whether a computerized inpatient renal template note with clinical decision support improves resident knowledge and documentation of kidney disease.
Methods
In this prospective study, first year medical residents were encouraged to use the renal template note for documentation over a one-month period. The renal template note included an option for classification of acute kidney injury (AKI) and chronic kidney disease (CKD) categories with a link to standard classifications. Pre- and post-knowledge of AKI and CKD categories was tested with a quiz and surveys of resident experience with the intervention were conducted. Appropriate AKI and/or CKD classification was determined in 100 renal template notes and 112 comparable historical internal medicine resident progress notes from approximately one year prior.
Results
2,435 inpatient encounters amongst 15 residents who participated were documented using the renal template note. A significantly higher percent of residents correctly staged earlier stage CKD (CKD3) using the renal template note compared to historical notes (9/46 vs. 0/33, p<0.01). Documentation of AKI and more advanced CKD stages (CKD4 and 5) did not improve. Knowledge based on quiz scores increased modestly but was not significant. The renal template note was well received by residents and was perceived as helping improve knowledge and documentation of kidney disease.
Conclusion
The renal template note significantly improved staging of earlier stage CKD (CKD3) with a modest but non-significant improvement in resident knowledge. Given the importance of early recognition and treatment of CKD, future studies should focus on teaching early recognition using template notes with supplemental educational interventions.
Key words: Clinical decision support systems, kidney disease, medical education, electronic medical records, templates
1. Introduction
Kidney disease is highly prevalent in the United States, affecting over 20 million Americans [1]. The key step in preventing progression of kidney disease is early recognition and treatment [2, 3]. Despite this, kidney disease has been shown to be under-documented in physician notes, suggesting lack of recognition [4-6]. In a retrospective chart review performed at 2 inner city academic health care clinics in the United States, Rothberg et al. reported that only 38% of elderly patients with moderate chronic kidney disease (CKD) (estimated glomerular filtration rate (eGFR) <60 mL/min) were documented as having CKD in their outpatient chart [4]. Furthermore, a cross-sectional analysis of the National Health and Nutrition Examination Survey (1999–2004) has shown that only 8% of patients with moderate CKD in the United States are aware of this diagnosis, a clear surrogate of poor physician recognition [7].
The recent widespread, government-supported implementation of electronic medical records (EMRs) for outpatient and inpatient documentation serves as an opportunity to increase recognition of kidney disease among physicians at all levels through the use of educational tools embedded into the EMR. There is some evidence that clinical decision support (CDS) tools can improve recognition and documentation of chronic kidney disease (CKD) [8, 9]. In a study by Fox et al., the implementation of a quality improvement intervention which included a computerized decision-making support system in 2 underserved primary care clinics improved CKD recognition as defined by billing codes significantly from 21% to 79% [8]. In addition to improving CKD recognition, CDS tools have been effectively embedded into the EMR to augment resident learning [10-12]. However, studies examining the effect of template-based notes with embedded educational tools on resident learning are lacking.
This study was conducted at an academic medical center which will be transitioning to complete electronic progress note documentation by 2014. In order to attempt to optimize resident learning with electronic documentation, a computerized renal template note with clinical decision support (CDS) was created. The purpose of this study was to determine whether a computerized renal template note with CDS used for documentation of inpatient follow-up encounters would improve resident documentation and knowledge of kidney disease.
2. Methods
2.1 Participants and Setting
This study was a single-center, prospective study of post-graduate year 1 (PGY-1) internal medicine residents. This study was conducted at Winthrop University Hospital in Mineola, NY, an academic medical center with 591 beds, 1,872 attending physicians, and approximately 84 internal medicine residents. 21 PGY-1 residents (categorical and preliminary) starting a one-month general internal medicine ward block on either December 18th 2012 or January 18th 2013 were eligible for study participation, and all 21 signed a consent form agreeing to participate in this study. The consent form described the voluntary nature of the study, including their ability to withdraw at any time. The intervention period consisted of 2 separate one-month ward blocks. 12 residents consented and participated from December 18th 2012 to January 17th 2013 and 9 residents consented and participated from January 18th 2013 to February 18th 2013. During the study, rates of participation were determined by self report. Eighteen residents self-reported that they used the template note for patient encounters during the study period, with 12 of 18 (67%) reporting using the note for all patient encounters. Three participants reported not using the note at all during the study period. For residents not documenting patient encounters using the renal template note, one reminder was given encouraging its use. No further reminders were given during the study. After the study, rates of renal template note documentation by the study participants were assessed. Of the 18 residents who self-reported using the renal template note, we were unable to extract any notes for 3 of them, hence their surveys and quizzes were excluded from the study analysis. For the remaining study participants (n=15), the average number of notes entered was 160 (±67), with a range of 12 to 299 notes written.
2.2 Intervention
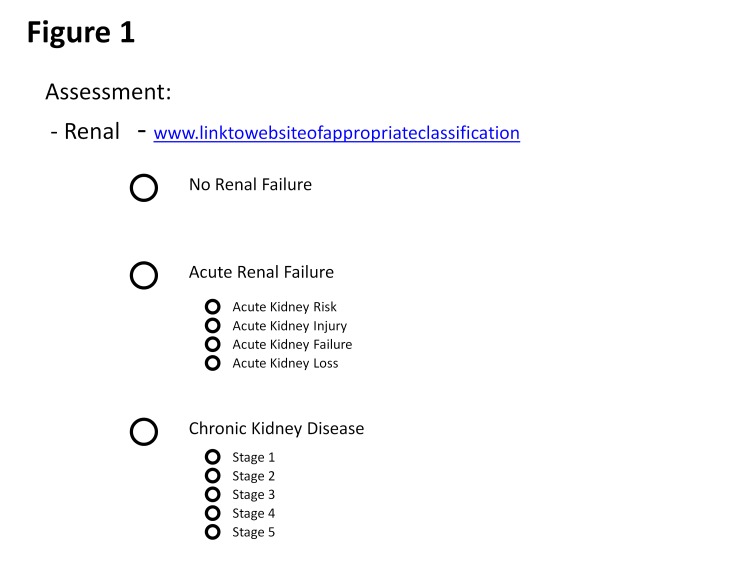
The renal template note developed with embedded clinical decision support was designed by members of the Division of Nephrology and Hypertension, Department of Medicine, and in conjunction with the Department of Medical Informatics. The study was initiated in January of 2012. At that time the majority of the inpatient documentation was paper-based with the exception of a group of approximately 10 voluntary providers who were piloting a computerized progress note, none of which were study participants. The EMR vendor at the time of this work was Siemens Medical Solutions (Malverne, PA). The pilot computerized progress note was a structured note entry application containing both clickable structured elements and free text elements. Vital signs and laboratory results are imported as structured data from the EMR into the note. Data from structured and free text elements such as the assessment and plan can be carried forward to subsequent patient days with validation by the documenting provider on each element brought forward. The study note template was incorporated into the existing computerized progress note template and prompted residents to click the appropriate classification of their patient’s kidney disease. Patients could be classified as having no kidney disease, acute kidney injury (AKI), chronic kidney disease (CKD) or acute on chronic kidney disease (► Figure 1). In patients with acute on chronic kidney disease both the AKI and CKD classifications could be clicked at that same time. When the AKI or CKD box was clicked, residents were prompted to sub-classify AKI into risk, injury, failure or loss categories based on the Acute Dialysis Quality Initiative (ADQI) – Risk, Injury, Failure, Loss or End Stage Renal Disease (RIFLE) classification scheme [3] and/or to sub-classify CKD into stages based on the Kidney Disease Improving Global Outcomes (KDIGO) guidelines [4]. The renal template note was designed to minimize disruptions in workflow and required only one to four extra clicks in the documentation process while providing clinical decision support at the point of note entry. There were no drop down menus associated with the template note and all components of the note were visible on the electronic page after clicking. Clinical decision support for the template note consisted of a link embedded into the progress note to an intranet webpage where residents could obtain RIFLE classification guidelines, CKD staging guidelines and a simplified 4-variable Modification of Diet in Renal Disease (MDRD) estimated glomerular filtration rate (GFR) calculator. The MDRD calculator would calculate the GFR of the patient for study participants based on entered age, gender, race and creatinine, and would also assign an appropriate CKD stage. This calculator provided a point of care aid for classifying patients with chronic kidney disease into the appropriate stage. The study participants were given a 30 minute tutorial on documentation with electronic notes, as they all were documenting in the paper chart prior to this study. The tutorial included a brief lesson on using the renal template note and the importance of renal failure documentation. They were then encouraged to use the renal template note for all of their follow-up documentation, regardless of renal diagnosis, for a period of one-month.
Fig 1.
The study note incorporated into the computerized progress note template. Residents were prompted to click on the appropriate classification of their patient’s kidney disease. When the AKI or CKD box was clicked, residents were prompted to sub-classify AKI into risk, injury, failure or loss categories based on the Acute Dialysis Quality Initiative (ADQI) – Risk, Injury, Failure, Loss or End Stage Renal Disease (RIFLE) classification scheme [3] and/or to sub-classify CKD into stages based on the Kidney Disease Improving Global Outcomes (KDIGO) guidelines [4]. Clinical decision support for the template note consisted of a link embedded in the progress note to an intranet webpage where residents could obtain RIFLE classification guidelines, CKD staging guidelines and a simplified 4-variable Modification of Diet in Renal Disease (MDRD) estimated glomerular filtration rate (GFR) calculator.
2.3 Measures
2.3.1 Pre-study survey
The pre-study survey consisted of basic demographic questions, a question related to prior nephrology training and a question regarding future career plans.
2.3.2 Quiz
The kidney disease quiz was an 11–question, fill in the blank quiz that tested knowledge of CKD staging, AKI classification and variables affecting the MDRD GFR calculation (Appendix 1). The questions for the quiz were based on the CDS link that residents could access during the intervention period. Grading of the quiz was performed by a blinded investigator that did not participate in study recruiting, study consent or study procedures. Partial credit was given for incomplete answers. The pre-study quiz was distributed immediately after participants were consented for the study. This corresponded to the afternoon prior to starting their month on the ward service, i.e., the intervention period. The post-study quiz, which comprised the exact same questions as the pre-study quiz, was distributed during sign-outs on the last day of the intervention period (after a one-month period of time). This quiz was designed based on the experience of the lead author (a board certified nephrologist).
2.3.3 Post-study survey
The post-survey consisted of questions related to resident confidence with using the renal template note and resident confidence in their knowledge of kidney disease. The majority of survey questions were framed according to a 5 point Likert scale with 1 = Strongly Agree, 2 = Agree, 3 = Neutral, 4 = Disagree, and 5 = Strongly Disagree.
2.4 Assessment of Appropriate Documentation
At the end of the study period appropriate documentation of kidney disease in the study notes was determined by study investigators based on standard RIFLE and KDIGO classifications. The lead author instructed other investigators on how to determine appropriate documentation. Of note, urine output criteria was not used to determine the RIFLE stage and if a baseline serum creatinine (creatinine from >3 months prior) was not available, the note was not classified. Documentation of kidney disease was considered appropriate only if the correct stage of CKD or the correct RIFLE classification of AKI appeared in the note. Attempts at classification that noted CKD without the appropriate stage or AKI without the appropriate RIFLE classification were not counted as appropriate documentation.
2.4.1 Renal Template Notes
All renal template notes written during the 2 one-month study periods were extracted from the electronic medical record in the order in which the patient for which the note was written was admitted to the hospital. The result was 2435 renal template progress notes. Of these 2435 renal template notes, only the first renal template progress note written for a particular patient was included in the evaluation for appropriate documentation leaving 550 notes completed for individual patients. Notes were excluded from evaluation of appropriate documentation if:
the study participants determined that the patient did not have renal failure
a baseline creatinine (creatinine from >3 months prior) could not be determined by investigators based on the existing record, as this is necessary for determination of acute or chronic status of kidney disease
estimated glomerular filtration rate ≥60 mL/min/1.73m2 for patients with CKD (stage 1 and stage 2) because the investigators felt they could not reliably determine the presence of urinary abnormalities or renal structural abnormalities for greater than 3 months in the inpatient record.
Renal template notes were evaluated for appropriate documentation in order based on the extraction list. No notes were skipped during this process. There were no prior studies to guide choosing an appropriate sample size of notes to analyze. We decided as a group that for this pilot study it would be appropriate to review enough notes so that approximately 100 would be classified for individual patients. 230 notes were analyzed to arrive at 100 classifications based on the above inclusion and exclusion criteria. The notes that were classified were written by 12 of 15 (80%) study participants, with a range of 7–16 classified notes per participant.
2.4.2 Historical Notes
Documentation using the renal template notes was compared to historical progress notes written approximately one year prior by PGY-1 residents with similar medical ward experience as the study population. These historical notes were obtained from paper based inpatient charts scanned into the electronic medical record of patients seen by the nephrology department in consultation from November 1st 2011 to February 29th 2012. This time period was selected to ensure that PGY-1 residents had a similar work experience as our study population. Comparative charts had ICD 9 coding designating AKI or stage 3, 4 or 5 chronic kidney disease (stage 1 and 2 CKD were excluded from data extraction because they could not be reliably determined in notes as explained above). A list of identifying information for these charts was generated by the billing department at our institution. The result was a list of 381 charts. Only those charts that contained an intern progress note written for a patient on the general medicine service were considered for analysis, and only the first progress note written on an individual patient was considered. Historical notes were excluded from classification if:
a baseline creatinine could not be determined by investigators based on the existing record,
if multiple charts existed for the identifying information that was extracted,
if the patient did not have AKI or CKD.
The majority of historical charts that were not classified did not have an intern progress notes for a patient on an internal medicine ward service. All historical charts that were extracted were analyzed and based on the above inclusion and exclusion criteria 112 notes were classified.
2.5 Statistical Analysis
The results were expressed as mean (± standard deviation) for continuous data and frequency (percent) for categorical data. Comparisons of means for quiz scores pre- and post-intervention were performed using paired t-tests. Comparisons of appropriate documentation between renal template notes and historical notes were performed using Fischer’s exact test. Statistical significance was defined as p<0.05.
3. Results
3.1 Survey Results for Resident Experience with the Renal Template Note with CDS
Of the 15 PGY-1 residents who used the patient note for documentation during the study period, the average age was 28; 8 were male, 6 of 15 (40%) had taken a prior nephrology elective and only one was planning a career in nephrology. 14 of 15 (93%) agreed or strongly agreed that they were more aware of kidney failure and 11 of 15 (73%) agreed or strongly agreed that the design of the renal template note was user friendly. 14 of 15 (73%) thought that it took less or the same amount of time to document a patient with kidney disease. 10 of 15 (67%) agreed or strongly agreed that the renal template note improved their knowledge of ARF and 11 of 15 (73%) agreed or strongly agreed that the renal template note improved their knowledge of CKD. At the end of the study period 14 of 15 (93%) residents agreed or strongly agreed that it was important to document outpatients as having CKD. These data are summarized in ► Tables 1 and ► Table 2.
Table 1.
Demographic Characteristics of PGY1 Residents (n = 15). Note. MD = Medical Doctor. DO = Doctor of Osteopathy. MBBS = Bachelor of Medicine and Bachelor of Surgery.
| Characteristic | Mean (± SD) or No. (%) |
|---|---|
| Age | 28 (±3) |
| Male | 8 (53) |
| Degree | |
| • MD | 13 (87) |
| • DO | 1 (7) |
| • MBBS | 1 (7) |
| Prior nephrology elective (Yes) | 6 (40) |
| Plan career in Nephrology | |
| • Yes | 1 (7) |
| • No | 10 (67) |
| • Unsure | 4 (27) |
Table 2.
Post-Intervention Survey Results (n = 15). Survey data were collected according to a 5 point Likert scale with 1 = Strongly Agree, 2 = Agree, 3 = Neutral, 4 = Disagree, and 5 = Strongly Disagree. Note. CDS = Clinical decision support, RTN = Renal template note, AKI = Acute kidney injury, CKD = Chronic kidney disease.
| Survey Item | Mean (±SD) or No. (%) |
|---|---|
| The intervention made you more aware of renal failure. | 1.8 (±0.56) |
| The operability of the CDS was user friendly. | 2.27 (± 0.70) |
| Compared to pre-RTN, Length of documentation time. | |
| • Less | 4 (26.7) |
| • Same | 7 (46.7) |
| • More | 4 (26.7) |
| Do you plan to pursue a career in Nephrology? | |
| • Yes | 1 (6.7) |
| • No | 13 (86.7) |
| • Unsure | 1 (6.7) |
| The intervention improved your knowledge of AKI. | 2.47 (± 0.91) |
| The intervention improved your knowledge of CKD. | 2.2 (± 0.94) |
| You feel it is important to document outpatients with CKD. | 1.4 (± 0.67) |
3.2 Knowledge Assessment via Kidney Disease Quiz
Prior to implementation of the renal template note, the average kidney disease scores were 21.2% (±14.1%). This included an average score of 4.7% (±12.4%) on the AKI section and 32.2% (±23.2%) on the CKD section. Post-intervention there was an improvement in renal failure knowledge (33.3% ±24.1%), however this improvement did not reach statistical significance. There was an improvement in both AKI (18%±31.5%) and CKD knowledge (44.6%±23.1%) post intervention, however again these differences did not reach statistical significance. When post intervention quiz scores for residents who completed a renal template note for every follow-up encounter were examined they were higher than the entire cohort (33.3%±24.1%, vs. 36.9%±25.8%), however this improvement did not reach statistical significance.
3.3 Appropriate Documentation of Kidney Disease
The distribution of kidney disease diagnoses in 100 renal template notes and 112 historical notes is shown in Table 3. Using the renal template note, there was an improvement in appropriate documentation of both stage 3–5 CKD (35.8% vs. 20.5%) and AKI (30.3% vs. 17.9%), however these differences did not reach statistical significance. Patients with CKD were sub-classified based on stage. In historical notes there were no patients with stage 3 or 4 CKD who were documented using a stage-based classification scheme. In the renal template notes there were 11 patients with stage 3 and stage 4 CKD who were documented correctly by stage. This improvement reached statistical significance for stage 3 CKD (19.6% vs. 0%, p<0.01). Patients with AKI were subclassified into risk, injury, failure or loss levels of injury based on the RIFLE criteria, however there was not a statistically significant improvement in RIFLE classification at any level of injury.
Table 3.
Appropriate Documentation of Renal Failure. Definitions: Stage III CKD: eGFR between 30–59 mL/min/1.73 m2 for ≥ 3 months; Stage IV CKD: eGFR between 15–29 mL/min/1.73 m2 for ≥ 3 months; Stage V CKD: eGFR 15< mL/min/1.73 m2 for ≥ 3 months or dialysis dependence; Risk: Increased creatinine X 1.5 or eGFR decrease >25%; Injury: Increased creatinine X 2 or eGFR decrease >50%; Failure: Increased creatinine X 3 or eGFR decrease >75% or creatinine ≥ 4mg per 100ml (acute rise of ≥ 0.5 mg per 100ml). Note: RTN = Renal Template Note, eGFR = estimated glomerular filtration rate
| Note Classification | Historical Correct (%) | RTN Correct (%) | P value |
|---|---|---|---|
| Chronic Kidney Disease | 15/73 (20.5) | 24/67 (35.8) | |
| Stage III CKD | 0/33 (0) | 9/46 (19.6) | <0.01 |
| Stage IV CKD | 0/17 (0) | 2/6 (33.3) | 0.06 |
| Stage V CKD | 15/23 (65.2) | 13/15 (86.7) | 0.26 |
| Acute Kidney Injury | 7/39 (17.9) | 10/33 (30.3) | |
| Risk | 0/24 (0) | 2/16 (12.5) | 0.15 |
| Injury | 1/5 (20) | 1/6 (16.7) | 1 |
| Loss | 6/10 (60) | 7/11 (63.6) | 1 |
4. Discussion
Despite the development of guidelines for the staging and classification of AKI and CKD, kidney disease remains under-recognized by physicians in the United States [15]. This under-recognition has been attributed to the use of creatinine levels rather than GFR by physicians to define kidney disease (leading to an under-estimation), and to a failure of physicians to recognize guideline specific definitions of kidney disease [16]. In this study we introduced a renal template note into the computerized documentation process for volunteer PGY1 residents at our institution and studied its effect on resident knowledge and documentation of kidney disease, surrogate measures of recognition. This template note was designed to be user friendly, with minimal disruption to workflow. The majority of study participants did find the renal template note to be user friendly with approximately ¾ of study participants stating that the template note did not prolong their documentation time. This finding is consistent with previous studies of template based notes that have not shown increased documentation times with their use [17, 18].
We found slight improvements in kidney disease knowledge with the use of the renal template note though this improvement did not reach statistical significance. When knowledge of kidney disease was broken down into CKD or AKI knowledge, again improvements with the renal template note were seen, but these also did not reach statistical significance. This was a disappointing finding, and given that the post study quiz was administered immediately after the intervention period, any improvements in knowledge were likely attributable to recall bias. Due to this result, we do not plan on re-testing kidney disease knowledge at any time period, as lasting significant improvements in kidney disease knowledge are unlikely to be seen. In order to determine reasons for the failure of our intervention to improve resident knowledge, the investigators had informal discussions with some study participants regarding the renal template note. These participants suggested additional educational interventions throughout the month to supplement kidney disease knowledge that had been acquired by using the template note.
With regards to documentation rates, we found improvements in CKD but not AKI documentation with use of the renal template note. This improvement was realized in the staging of early CKD. Despite the implementation of guidelines for classification by CKD stage in 2002, PGY1 resident notes from one year prior did not document any cases of stage 3 or stage 4 CKD. This finding is consistent with previous studies that have shown low inpatient rates of appropriate stage 2 through 4 CKD documentation [19]. With the implementation of the renal template note, the frequency of appropriate documentation of stage 3 CKD significantly improved. This is of particular importance given the need for early recognition and treatment of patients with chronic kidney damage. By improving early recognition of CKD, early treatment can be initiated that has been shown to improve mortality and slow and even prevent progression of kidney disease to end stage [20]. AKI documentation remained poor despite use of the renal template note, a finding that is consistent with existing literature [21]. Interestingly, the documentation rates of ARF and stage 5 CKD in both renal template notes and historical notes were higher than other diagnoses. For ARF, we hypothesized that was due to a familiarity with the term ARF and not related to a clear classification decision. This familiarity likely resulted because the term ARF was previously used to describe any abrupt change in renal function. Since 2007, the new term to describe an abrupt change in renal function is AKI with ARF being a subset of AKI in which there is a tripling of creatinine or a 75% reduction in GFR [13]. For stage 5 CKD, we hypothesized that increased rates of documentation were due to the inclusion of the term ESRD as part of appropriate classification of these patients and the ease with which dialysis patients are recognized.
The strengths of the study include the use of the template note for a large number of inpatient encounters (2,435 renal template notes generated), and the perceived ease of use of the note. Our study also included a range of measures included a pre and post intervention surveys and quizzes as well as in depth analysis of appropriate documentation rates. Our study is limited by its small sample size and non-randomized nature possibly leading to selection bias. Study participants could choose to use the renal template note for documentation or to continue to document in the paper chart, and because of this option, 6 study participants chose to continue paper documentation. It is thus possible that our study selected for a more diligent resident population than would be expected otherwise. In addition, the investigators only analyzed 230 of 550 renal template notes written on individual patients, and because these notes were extracted in order of the date of patient admission, only notes from 12 of 15 (80%) study participants, all from the 1st intervention cohort, were analyzed. Thus although this cohort compromised 80% of the study participants, the possibility of selection bias still exits (these residents may have been more diligent in documenting with the template note than the three from the second cohort). Despite this, we feel our significant difference in documentation patterns for early stage CKD is valid because all extracted historical notes were analyzed and not one note appropriately documented stage 3 CKD. Another limitation of the study is that we could not assess how often study participants clicked the CDS link during the intervention period. Unfortunately, we were not able to use technology such as a counter in our study. For future studies, we plan to enable a counter that lets investigators know how often and by whom the CDS link is clicked during the study period. Another limitation of our study was that although historical notes were written by PGY-1 residents with similar ward medical experience as the study participants (given that notes were from a comparable time period in the academic year), these residents may have had a different knowledge base than the study participants, making interpretations drawn from the comparison of their notes difficult. Another limitation of our study was the use of non-validated quizzes and surveys. There are no universally validated surveys to assess confidence and perceived importance of kidney disease knowledge for providers, and there is also no universally validated quiz to test the kidney disease knowledge of providers. We plan to use the results from this pilot survey to create a validated quiz and survey for a future large-scale study. Finally our study is limited by the fact that all study participants were writing their progress notes in the paper chart prior to implementation of this study and not electronically documenting these notes. Thus, any improvements in documentation may be attributed to the use of an electronic note rather than the particular template.
5. Conclusions
In conclusion, a renal template note with clinical decision support did not significantly improve resident knowledge of kidney disease, but did lead to an improvement in appropriate staging of early stage CKD (stage 3) and an appreciation of kidney disease documentation by residents. Future studies should focus on the use of template notes to augment resident learning in the context of other educational interventions and possibly didactic sessions. These studies should also focus on documentation of CKD which appears to be more feasible for residents.
Clinical Relevance Statement
A renal template note with clinical decision support was well received by residents and did not prolong their documentation time. A renal template note with clinical decision support can lead to an improvement in appropriate staging of early stage CKD. If kidney disease is recognized early, treatment can be implemented to delay or even prevent progression to end stage renal disease, a highly morbid and costly condition. Practioners should consider embedding template notes with supplemental educational interventions into their existing EMR to improve resident documentation of chronic conditions.
Conflict of Interest
The authors declare no conflicts of interest in this research
Protection of Human and Animal Subjects
The study was approved by the Institutional Review Board of our hospital and was conducted in accordance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research involving Human Subjects.
APPENDIX 1
Renal Failure Quiz (100 points)
Define Acute Kidney Risk by change in kidney function and urine output elements (10 points)
Define Acute Kidney Injury by change in kidney function and urine output elements (10 points)
Define Acute Kidney Failure by change in kidney function and urine output elements (10 points)
Define Acute Kidney Loss by change in kidney function and urine output elements (10 points)
List the 4 variables needed to calculate GFR using the 4-variable MDRD equation (20 points)
Define Stage 1 CKD by GFR criteria and urine findings (10 points)
Define Stage 2 CKD by GFR criteria and urine findings (10 points)
Define Stage 3 CKD by GFR criteria (5 points)
Define Stage 4 CKD by GFR criteria (5 points)
Define Stage 5 CKD by GFR criteria (5 points)
Define End Stage Renal Disease (5 points)
References
- 1.Collins AJ, Foley RN, Chavers B, Gilbertson D, Herzog C, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Guo H, Gustafson S, Heubner B, Lamb K, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. ’United States Renal Data System 2011 Annual Data Report: Atlas of chronic kidney disease & end-stage renal disease in the United States. Am J Kidney Dis 2012; 59(1 Suppl 1): A7, e1–420 [DOI] [PubMed] [Google Scholar]
- 2.Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, Powe NR. The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med 2002; 137(6): 479–486 [DOI] [PubMed] [Google Scholar]
- 3.Levinsky NG. Specialist evaluation in chronic kidney disease: too little, too late. Ann Intern Med 2002 Sep; 137(6): 542–543 [DOI] [PubMed] [Google Scholar]
- 4.Rothberg MB, Kehoe ED, Courtemanche AL, Kenosi T, Pekow PS, Brennan MJ, Mulhern JG, Braden GL. Recognition and management of chronic kidney disease in an elderly ambulatory population. J Gen Intern Med 2008; 23(8): 1125–1130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chase HS, Radhakrishnan J, Shirazian S, Rao MK, Vawdrey DK. Under-documentation of chronic kidney disease in the electronic health record in outpatients. J Am Med Inform Assoc 2010; 17(5): 588–594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Navaneethan SD, Kandula P, Jeevanantham V, Nally JV Jr., Liebman SE. Referral patterns of primary care physicians for chronic kidney disease in general population and geriatric patients. Clin Nephrol 2010; 73(4): 260–267 [DOI] [PubMed] [Google Scholar]
- 7.Plantinga LC, Boulware LE, Coresh J, Stevens LA, Miller ER 3rd, Saran R, Messer KL, Levey AS, Powe NR. Patient awareness of chronic kidney disease: trends and predictors. Arch Intern Med 2008; 168(20): 2268–2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox CH, Swanson A, Kahn LS, Glaser K, Murray BM. Improving chronic kidney disease care in primary care practices: an upstate New York practice-based research network (UNYNET) study. J Am Board Fam Med 2008; 21(6): 522–530 [DOI] [PubMed] [Google Scholar]
- 9.Patel TG, Pogach LM, Barth RH. CKD screening and management in the Veterans Health Administration: the impact of system organization and an innovative electronic record. Am J Kidney Dis 2009; 53(3 Suppl 3): S78–S85 [DOI] [PubMed] [Google Scholar]
- 10.Litvin CB, Davis KS, Moran WP, Iverson PJ, Zhao Y, Zapka J. The use of clinical decision-support tools to facilitate geriatric education. J Am Geriatr Soc 2012; 60(6): 1145–1149 [DOI] [PubMed] [Google Scholar]
- 11.Riggio JM, Sorokin R, Moxey ED, Mather P, Gould S, Kane GC. Effectiveness of a clinical-decision-support system in improving compliance with cardiac-care quality measures and supporting resident training. Acad Med 2009; 84(12): 1719–1726 [DOI] [PubMed] [Google Scholar]
- 12.Keenan CR, Nguyen HH, Srinivasan M. Electronic medical records and their impact on resident and medical student education. Acad Psychiatry 2006; 30(6): 522–527 [DOI] [PubMed] [Google Scholar]
- 13.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004; 8(4): R204–R212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stevens PE, Levin A. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013; 158(11): 825–830 [DOI] [PubMed] [Google Scholar]
- 15.Lewington AJ, Cerda J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int 2013; May 1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fox CH, Brooks A, Zayas LE, McClellan W, Murray B. Primary care physicians’ knowledge and practice patterns in the treatment of chronic kidney disease: an Upstate New York Practice-based Research Network (UNYNET) study. J Am Board Fam Med 2006; 19(1): 54–61 [DOI] [PubMed] [Google Scholar]
- 17.Marill KA, Gauharou ES, Nelson BK, Peterson MA, Curtis RL, Gonzalez MR. Prospective, randomized trial of template-assisted versus undirected written recording of physician records in the emergency department. Ann Emerg Med 1999; 33(5): 500–509 [DOI] [PubMed] [Google Scholar]
- 18.Mulvehill S, Schneider G, Cullen CM, Roaten S, Foster B, Porter A. Template-guided versus undirected written medical documentation: a prospective, randomized trial in a family medicine residency clinic. J Am Board Fam Pract 2005; 18(6): 464–469 [DOI] [PubMed] [Google Scholar]
- 19.Ferris M, Shoham DA, Pierre-Louis M, Mandhelker L, Detwiler RK, Kshirsagar AV. High prevalence of unlabeled chronic kidney disease among inpatients at a tertiary-care hospital. Am J Med Sci 2009; 337(2): 93–97 [DOI] [PubMed] [Google Scholar]
- 20.Stack AG. Impact of timing of nephrology referral and pre-ESRD care on mortality risk among new ESRD patients in the United States. Am J Kidney Dis 2003; 41(2): 310–318 [DOI] [PubMed] [Google Scholar]
- 21.Grams ME, Plantinga LC, Hedgeman E, Saran R, Myers GL, Williams DE, Powe NR. Validation of CKD and related conditions in existing data sets: A systematic review. Am J Kidney Dis 2011; 57(1): 44–54 [DOI] [PMC free article] [PubMed] [Google Scholar]