Summary
Objective
To examine how and why the quality of clinical communication between radiologists and referring physicians was changed in the inpatient imaging process after implementation of a hospital information system (HIS).
Methods
A mixed-method study of the chest X-ray (CXR) requests and reports, and their involved processes within a pre- and post-HIS implementation setting.
Results
Documentation of patient age, patient ward, and name and signature of requesting physician decreased significantly in post-HIS CXR requests (P<0.05). However, documentation of requested position and technique increased significantly (P<0.05). In post-HIS CXR reports, documentation of patient age, patient chart number, urgent/normal status of requisition, position and technique of CXR, name of referring physician, and date of request were increased significantly (P<0.05). However, documentation of discussion for important findings was decreased significantly (P<0.05). The mean number of words in the body text of post-HIS reports was increased significantly (18.65 vs. 16.3, P = 0.00).Our qualitative findings highlighted that involving nursing and radiology staff in the communication loop between physicians and radiologists after the implementation resulted in extra steps in the workflow and more workload for them. To cope with the new workload, they adopted different workarounds that could explain the results seen in the quantitative study.
Conclusion
The HIS improved communication of administrative and identification information but did not improve communication of clinically relevant information. The reason was traced to the complications that the inappropriate implementation of the system brought to clinical workflow and communication loop.
Key words: Communication, hospital information system, chest X-ray, workflow, patient safety
1. Introduction
Imaging studies are frequently an essential component of diagnostic procedures. The expenditure on diagnostic imaging in current healthcare systems is increasing; in average they amount to more that 10% of total healthcare expenditure per capita [1,2]. Plain chest X-rays (CXR) have remained the most frequent medical imaging test, despite the advances in medical imaging technology such as CT scan, MRI, and PET scan [3]. CXRs are among the most difficult radiology images to interpret accurately too. If other sources of information such as patient history are not accessible in interpreting CXRs, there will be a great chance of missing critically important diagnosis [4,5].
The process of CXR in inpatient settings is a simple process which can be broken down into: requesting of the test (by a physician), communicating the request to the radiology department, performing the test, reading/interpreting it (by a radiologist), and finally communicating the result back. Radiologist and physician are the main participants in this process. Communication between them normally takes place through CXR requests and reports. This requisition and report is the primary yet neglected method of information exchange that enables efficient collaboration between radiologist and referring physician [6].
The information supplied from physician to radiologist and vice versa plays a prominent role in achieving maximal clinical benefit from a radiological examination. Conversely, problem in this communication can lead to error in diagnosis and treatment of patients [7]. Errors in diagnostic radiology due to communication problems are common. They have been reported as the fourth most frequent primary allegations against radiologists [8]. Evaluating patient safety events reported within a major teaching hospital in Sydney showed that almost half of the radiology related incidents had some aspect of communication breakdown [9]. Many of those errors are related to the way a test is requested or to the way its interpretation is reported back to the referring physician. The quality (i.e., the style and the content) of radiology requests and reports is of critical importance for avoiding errors and making proper clinical decisions [6,10,11]. Therefore, to minimize errors, to ensure an optimal patient care, and to make efficient use of imaging resources, communication of information by means of requests and reports must be improved [12].
Information technology (IT) has been shown to improve the quality of patient care and reduce the cost. Improving communication throughout clinical processes is among the most important areas in which IT can bring its constructive effects to fruition [13-16]. In 2010, an advanced hospital information system (HIS) was implemented in an academic hospital affiliated with Urmia University of Medical Sciences (UUMS), Urmia, Iran. Rather than evaluating the whole implementation process, we decided to look into the effects of the implementation on clinical communication. We were interested to know how communication in imaging processes was affected by this implementation. To this end, we compared the quality of CXR requests and reports and the processes involved in the pre- and post-HIS implementation periods in selected inpatient wards of this hospital. We used a mixed method study and a sociotechnical approach to understand how and why the quality of the reports and requests were changed following the HIS implementation. The study protocol was reviewed and approved by UUMS’s Review Board and Research Ethics Committee.
2. Methods
The study hospital was a 270-bed referral academic center affiliated with UUMS. All Pediatrics in-patient wards with different range of pediatric care (including neonatal ICU, Pediatric Surgery, and Hematology/Oncology, Infectious, Gastroenterology, and Nephrology) were included to this study. These wards comprised more than 70 percent of total hospital capacity. In June 2010, a HIS with the capability of requesting and reporting para-clinical diagnostic tests electronically was implemented in this hospital. The system was accessible in all inpatient and outpatient wards of the hospital. It provided flexible request and report interfaces with no mandatory fields. After implementation, the paper charts were still kept updated and printouts of all test reports were put in patients’ paper charts. In this study, we evaluated CXR requests and reports and the involved processes in Pediatric wards of the hospital. Our study was started as a quantitative study to compare the quality of information in CXR requests and reports in pre vs. post-HIS period. To explain the findings in the quantitative study, we also conducted a qualitative study of the inpatient imaging processes after the HIS-implementation.
The implementation strategy is a very important factor that determines how a ‘system frame’ collides with other frames of the implementation environment and how it works appropriately [17,18]. In the qualitative study rather than evaluating the system implementation, we focused on the post-implementation period and evaluated the effect of the implemented system on the communication process. A sociotechnical perspective was adopted. This frame of reference does not distinguish a system’s function from its implementation environment. Regardless of the technical quality of a system, the actual outcome after implemented is determined through the collision between the system frame and social, organizational, and cultural frames of its implementation environment [17]. Therefore, this study did not differentiate the system from its implementation environment when it comes to evaluate the changes in the communication process. We touched upon the implementation and its related issues only when it was needed.
2.1. Quantitative research
The quality of CXR requests and reports was defined as having necessary information contents and style. On the basis of the recommendation of the American College of Radiology [19] and reviewing the literature [6,8, 20], we developed two checklists for examining the necessary information contents and style in CXR requests and reports. The checklists were discussed and checked for their relevance with two physicians and two radiologists and modified based on their comments. The checklists then were piloted with 10 pre- and 10 post-HIS CXR requests and reports in the study hospital and further modified on the basis of the pilot test. The modified checklists were then used to collect data from the patients’ medical charts retrospectively. The items of our checklists are presented in ► Table 1 and ► Table 2. Two types of information were evaluated. The first type was demographics and identification information, e.g., patient name, age, and gender. The second type was clinical information, e.g., the reason for the test request, probable diagnosis, and proposed follow up tests. Both types of information are considered important clinically. Age, and gender for example are important information for clinicians to request proper technique or position and to report meaningful findings.
Table 1.
The information items analyzed in CXR requests using X2 test (at significance level of 0.05)
| Information items in CXR requests | df | % of pre-imp (N = 250) | % of post-imp (N = 210) | Pearson chi-square value | P value |
|---|---|---|---|---|---|
| Patient Name | 1 | 100 | 100 | * | * |
| Patient Age | 1 | 48.8 | 47.1 | 8.26 | 0.004 |
| Patient Gender | 1 | 32.8 | 32.4 | 0.05 | 0.817 |
| Patient Chart Number | 1 | 99.8 | 99.5 | 0.95 | 0.430 |
| Patient Ward | 1 | 98.4 | 85.2 | 17.91 | 0.000 |
| Urgency/Normal status of requisition | 1 | 1.2 | 0.9 | 0.04 | 0.836 |
| Request Date | 1 | 96 | 92.8 | 0.008 | 0.523 |
| Position & Technique | 1 | 68 | 79.2 | 5.59 | 0.018 |
| Medical history/Reason for request | 1 | 2.4 | 1.9 | 1.99 | 0.769 |
| Differential Diagnosis | 1 | 40.4 | 43.8 | 1.98 | 0.160 |
| Using Appropriate Terminology & Abbreviations | 100 | 96 | 0.81 | 0.450 | |
| Name & Signature of requesting physician | 1 | 82.8 | 63.3 | 16.6 | 0.000 |
* Not computable
Table 2.
The information items analyzed in CXR reports using X2 test (at significance level of 0.05
| Information items in CXR reports | df | % of pre-imp (N = 250) | % of post-imp (N = 210) | Pearson chi-square | P value |
|---|---|---|---|---|---|
| Patient name | 1 | 100 | 100 | * | * |
| Patient age | 1 | 0 | 77.6 | 399.39 | 0.000 |
| Patient gender | 1 | 100 | 100 | * | * |
| Patient chart number | 72 | 100 | 53.12 | 0.000 | |
| Urgency/Normal status of requisition | 1 | 0.4 | 34.8 | 99.82 | 0.000 |
| Position & Technique | 1 | 0 | 92.8 | 402.96 | 0.000 |
| Referring physician name | 1 | 0 | 43.8 | 136.9 | 0.000 |
| Request date | 1 | 0 | 93.3 | 406.56 | 0.000 |
| Name & signature of the reporting radiologist | 1 | 100 | 99.5 | 1.19 | 0.275 |
| General organization | 1 | 62.4 | 99 | 92.81 | 0.000 |
| Appropriate terminology & abbreviation | 1 | 1.2 | 0.5 | 2.53 | 0.111 |
| Important findings discussed | 1 | 31.6 | 17.1 | 12.72 | 0.000 |
| Negative findings reported | 1 | 2.8 | 4.3 | 0.75 | 0.386 |
| Clear & Logic conclusion | 1 | 0.4 | 0.9 | 0.53 | 0.463 |
| Final Diagnosis/ Differential Diagnosis | 1 | 0.4 | 0 | 0.35 | 0.356 |
| Proposed follow up tests | 1 | 5.2 | 8.1 | 1.56 | 0.210 |
* Not computable
We moreover counted the number of words in the body of text of the requests and reports as an extra indicator for the information being exchanged. Clinicians’ notes and request are normally written in an abstract format in which a word or an abbreviation might mean more than a sentence [16]. Therefore the number of words of clinical notes (e.g., CXR requests and reports) can be considered as an indicator of their information content.
The medical records of all patients hospitalized in pediatric wards of the study hospital in two 3-month periods before and after implementation of the HIS were included in this study. We skipped the first 6-month period after the HIS implementation (June to December 2010) to avoid the effect of “learning curve”. Therefore, two identical winter months in two consecutive years were chosen: December 22, 2009 to March 21, 2010 for the pre-HIS phase, and December 22, 2010 to March 21, 2011 for the post-HIS phase. Patients’ medical charts with at least one CXR request and report during the patients’ hospitalization were included in the study. CRX requests and reports were examined using the checklists and the number of words in the body text of the all CXR requests and reports were counted.
2.2. Qualitative research
A qualitative study of the process followed the quantitative study with the intention of understanding and interpreting the quantitative findings. This part was included three hours of observations and six interviews with one physician, two nurses, one radiologist, and two radiology staff. The observations were unstructured, non-participatory witnessing of the CXR requesting and reporting process. Notes were taken while and after the observations. The interviews were face-to-face, one-on-one, semi-structured, using pre-prepared general questions about the process such as: How do you fulfill CXR requesting/reporting process? What are the problems with the current process? How do you compare the current process with that of the pre-implementation? The interviews took 20 minutes on average and were voice recorded and transcribed accordingly.
2.3. Data analysis
The data from checklists were extracted and analyzed using X2 test (for nominal measures) and Student t-test (for evenly distributed data) to identify differences at an a-priori 0.05 level of significance. Observational notes and interview transcripts were coded and analyzed on the basis of the themes that could explain the quantitative findings. The results were discussed between the researchers to reach a shared understanding of the developments.
3. Results
3.1. The results of the quantitative study
Two hundred and fifty pairs of CXR requests and reports from pre-HIS period were compared to 210 pairs of CXR requests and reports from the post-HIS period. We had mixed results in analyzing of the data (► Table 1, ► Table 2). In the requests: While the documentation of requested position and technique was improved significantly, the documentation of patient age, patient ward, and name and signature of the requesting physician were significantly deteriorated after HIS implementation (P<0.05). No significant changes in the documentation of patient name, gender, patient chart number, the request date, urgency level of the request, medical history or reason for the request, differential diagnosis, and appropriate terminology and abbreviations were found (P>0.05) (► Table 1).
In the reports: The appearance of patient age, patient chart number, urgency level of the test, the applied position and technique for the test, the request date of the test, name of the referring physician, as well as the general organization of the reports were significantly improved in the post-HIS phase (P<0.05). However, discussion of important findings in the reports was deteriorated significantly following HIS implementation (P<0.05). No significant changes were observed in documentation of patient name, gender, name and signature of the reporting radiologist, reporting negative findings, clear and logic conclusion, final diagnosis/differential diagnosis, and proposed further follow-up tests (P>0.05) (► Table 2).
We compared the mean number of words in the body text of CXR requests and reports of pre-implementation to those of the post-implementation. Analysis showed that following the implementation of HIS, the mean number of words in the reports’ body text increased significantly (18.65 vs. 16.3, P = 0.00), while that of the requests did not change significantly (► Table 3).
Table 3.
The mean word number of CXR requests and reports evaluated using Student t test (at significance level of 0.05)
| Pre-imp. | Post-imp. | P value | 95% CI of the difference | |
|---|---|---|---|---|
| Mean number of words in the requests | 3.65 | 3.39 | 0.309 | -0.098, 0.616 |
| Mean number of word in the reports | 16.03 | 18.65 | 0.000 | -14.947, -12.691 |
3.2. Findings of the qualitative study
In analyzing the qualitative data, the following relevant themes appeared.
3.2.1. Complicated Physician-Radiologist communication loop
At the wards, physicians were not interested in working with the system. In the absence of a sense of ownership, physicians excused themselves from working with the system for having a very high clinical workload. Instead, they left the order entry task to nurses. Therefore, similar to the pre-implementation stage, physicians were writing their orders on patients’ paper charts during ward rounds. Nurses then transferred the orders into paper-based requisition forms and sent them to the radiology department together with the patients. After the implementation of the HIS, nurses moreover had to enter the CXR requests and the required information into the system.
At the radiology department, the situation was more or less the same. Radiologists were not using the system for reporting CXR results. Similar to pre-implementation workflow, radiology technicians accepted CXR paper-based requests and performed the requested CXRs accordingly. However, if there was any necessary information missing from the paper-based requests, the technicians first tried to find it with the HIS system instead of making phone calls to the nursing staff. Similar to pre-implementation, and due to the radiologists’ very high workload, except for urgent cases, the CXR images were normally sent to the wards without being reported. The next day, CXR images were sent back to the radiology department in order to be reported by one of the radiologists.
Because of the above-mentioned changes the “desired” communication process was changed. Nurses and secretaries were joined to the physician-radiologist communication loop and became directly involved parties in the “actual” communication loop (► Figure 1).
Fig. 1.
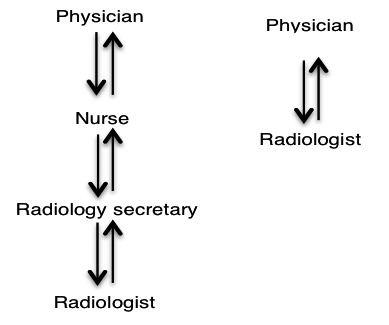
The “desired” communication loop (right) and the actual communication loop in post-HIS (left)
3.2.2. Increased workload
After the implementation of the system, the volume of work concerning CXR requests was almost doubled: nurses had to enter the requests into the system as well as prepare and send paper-based forms for the same CXR requisitions. They moreover had to make phone calls to follow up the paper-based CXR reports from the radiology department. Since in non-urgent cases, the CXR images came without reports, nurses had to return them to the radiology department for the radiologists’ reports the next day. It was possible for CXR images and their reports to be mixed up or lost on the way to or from the radiology department.
The CXR reports were first written on pieces of paper, dropped into the CXR images’ envelopes, and delivered to the secretaries. The secretaries opened the patients’ medical record in the HIS using the information on the paper-based CXR requests. This normally took time because many requests did not have enough patient specifications. They then typed the reports in the HIS, printed the reports, and delivered them to the radiologists. The radiologists read the reports and signed and stamped them, and gave them back to the secretaries for delivery to the wards (► Figure 2). A radiology staff member told us:
Fig. 2.
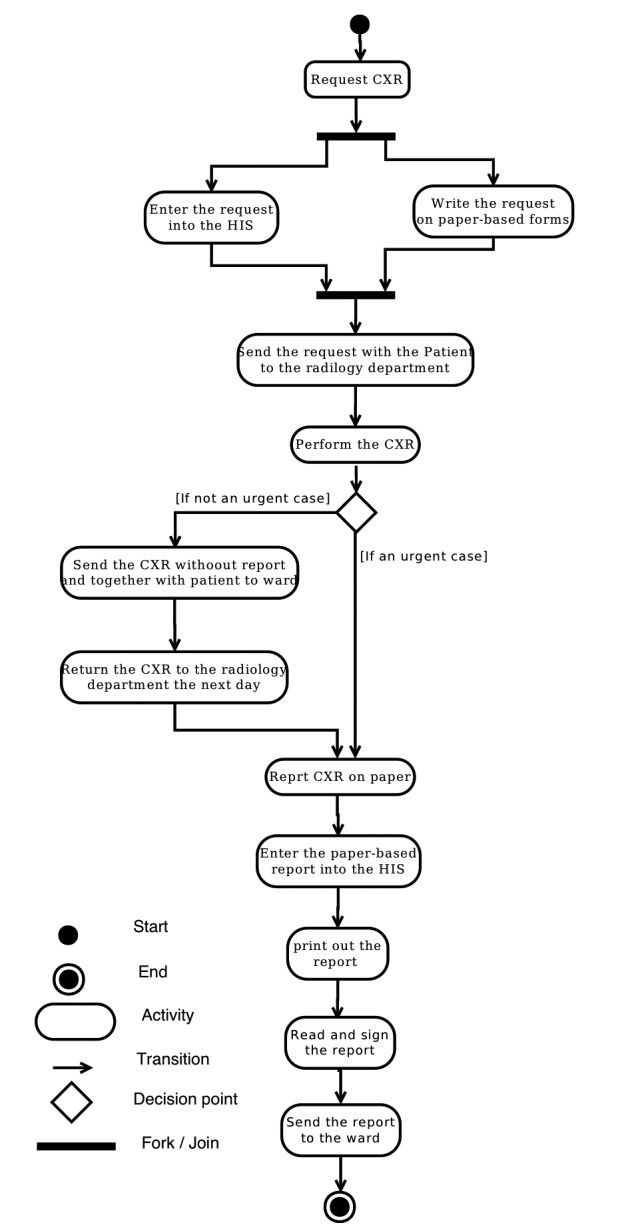
UML activity diagram of the actual post-HIS workflow process
“The workload after the HIS has multiplied especially for the secretaries. As a result of this increased workload, we had to hire two more secretaries.”
Because of the above-mentioned changes, extra activities and extra steps in the “actual” workflow comparison to the “desired” workflow were created. As a result, the actual post-implementation workflow became less efficient and more time consuming (► Figure 2 and ► Figure 3).
Fig. 3.
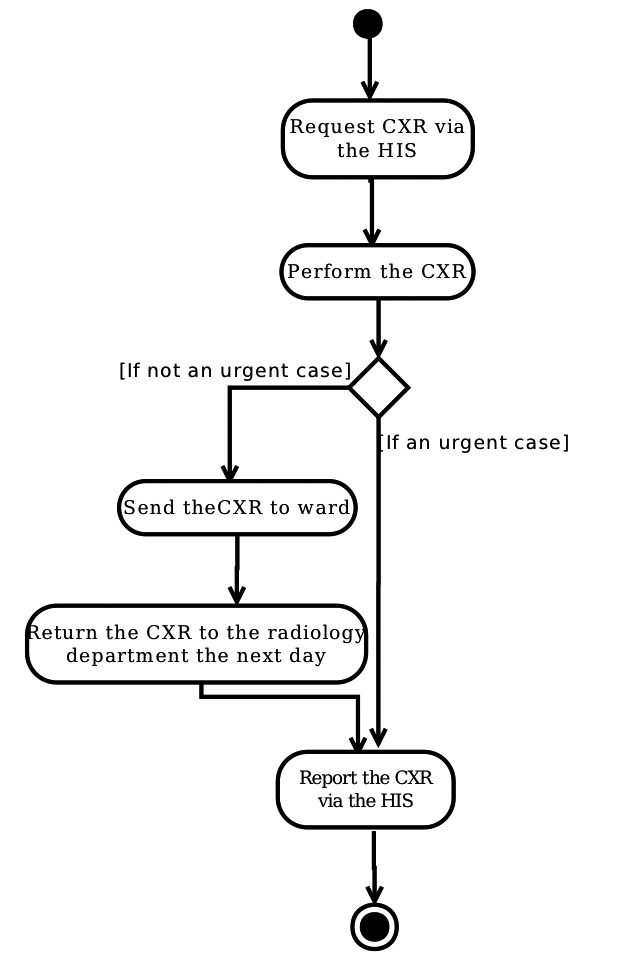
UML activity diagram of the “desired” workflow process
3.2.3. Unsupervised (risky) workarounds
At the wards, nurses compiled pre-prepared paper-based CXR requests with physicians’ signatures and stamps on them in nursing stations. Therefore, they could easily enter the patients’ identification (including patients’ name and chart number) to the pre-prepared requests and sent them to the radiology department for every CXR order. However, nurses neither have enough insight into the patients’ specific information, including clinical conditions, nor enough time to acquire this information. Thus, they left some patient specific information such as reason for the request and differential diagnosis unfilled in the requests. Similarly, in working with the HIS system, nurses did not fill in all the required information fields when they entered the CXR requests into the HIS.
At the Radiology department, the secretaries used a couple of ready-made report templates to overcome the increased workload. These templates were developed in coordination with radiologists and used for reducing the typing workload of the secretaries and for elaborating upon the concise reports of radiologists. They nevertheless put the required specification and precision of the reports in jeopardy. We observed many reports with exact similar wordings at the post-HIS period.
3.2.4. Incidental findings
The main driving force behind the implementation of the HIS was financial. Improving efficiency and quality of clinical processes in the system implementation were not prominent. The hospital was losing a great amount of money over the incomplete documentation of patients’ care required by insurance companies. The hospital authorities rushed to implement the system to improve documentation and to reduce its budget deficit. In doing so, the implementation team failed to motivate the clinical leaders and physicians to be involved in the implementation process.
At the radiology department, radiologists wrote the reports on small paper sheets. These handwritten paper reports were very concise and did not contain enough identification of the patients. Moreover, they were attached to the images in a very loose way. Thus, they could be mixed up when handled by the secretaries. One patient’s CXR report might easily go to another patient’s medical chart. This problematic part of the process existed prior to the HIS implementation. After the implementation, however, an additional risky step added to its vulnerability. The secretaries had to find and open patients’ electronic files in the system before typing the reports and printing them out. Therefore, in the context of high workload and reports with minimal identification information, the secretaries might mistakenly enter the report for one patient into the electronic file of another patient. The radiologists might miss this type of error when checking the printed reports because they had no carbon copy of their hand-written reports, and because remembering details of many CXR images was almost impossible. Moreover, after the secretaries finalized the reports in the system and printed them out, they were accessible by clinicians at the wards. This increased the risk that unchecked CXR reports might be used in patient care clinical management.
4. Discussion
Our quantitative study showed how the documentation of information in CXR requests and reports changed after implementation of the HIS. The results indicated that the quality of CXR requests decreased. Conversely, the quality of CXR reports regarding non-clinically relevant information and the mean number of words in the reports’ body text increased after the HIS implementation. However, the quality of CXR reports concerning clinically relevant information (such as discussion of important findings and differential diagnoses) either did not change or decreased.
Our qualitative study showed that the system was not supporting communication of the imaging process; physicians and radiologists became passive users of the system. They could not communicate directly (through the “desired” communication loop). To compensate, nursing and radiology staff were involved in the communication loop. This involvement of nursing and radiology staff resulted in an increased workload for them. Striving to reduce the extra workload, the staff members devised workarounds that undermined safe communication and increased the risk of error in clinical practice. Since nurses were using ready-made, paper-based requisition forms, important information was not included in the CXR requests. As filling the fields was not mandatory, information was also missing when CXR requests were entered into the HIS. Although the workarounds could reduce nurses’ workload to some extent, they increased the radiology staff’s workload. They had to gather missing necessary (mainly administrative and identification) information from different sources and enter them into the HIS system. This additional information produced HIS system reports that were much more complete compared to pre-HIS reports. However, in most cases the radiology staff failed to gather information about patients’ clinical condition. Therefore, the presence of patients’ clinical information in the post-HIS CXR reports either did not change or decrease. Using ready-made report templates increased the length (number of words) of the reports. Despite the increase in number of words, we observed that the reports’ quality did not improve with respect to documenting clinical information. In fact, the increase in the body of text of the post-HIS reports were mostly related to an increase in general and non-specific, explanatory words.
High workload is inherent to clinical practice and has frequently been referred to as an important drawback in adopting information technology in clinical practice [21,22]. Previous studies reported that recruiting nurses and secretaries as communication mediators between information systems and physicians can decrease physicians’ workload and increase appropriate use of information systems and may even reduce the possibility of medical errors [23]. However, our study showed such recruitment involves more parties in the communication loop and increases the complexity of the communication process and workflow. The increased workflow complexity can propagate unsafe workarounds and hence increase the chance of error in medical practice. For those parties involved inadvertently in the communication loop, the purpose of the workarounds was to reduce workload, never realizing that those workarounds could undermine clinical communication processes and put patient safety in jeopardy [24].
Implementation strategy is perhaps the most important step in applying IT in healthcare [18]. The driving force and motivation behind the implementation determines how a system frame collides with other frames of its implementation environment and finally how a system is adopted and used [25]. In our case, the main motivation behind the HIS implementation was mainly financial. Focusing too much on improving financial aspect of the hospital care, the implementation team overlooked the multidimensional nature of IT intervention and failed to address those dimensions in their implementation strategy. As a result the documentation of financially important information improved while the documentation of clinical important information did not improve. However, if improving the efficiency and safety of the care processes were at the center stage, the physicians’ involvement and better documentation of clinical information would be expected.
In depth qualitative study of the implementation process is required to understand what exactly went wrong and how it could be prevented. However, our findings in this study show how some of those unintended effects of the implementation could be prevented. It sounds that in rushing to implement the system, the implementation team did not assess required changes properly and failed to be prepared to mange them. They did not allow for adequate training and buy-in time for the users. Physician involvement and leadership was not considered essential and their concerns in system implementation were not valued. As a result physicians did not have sense of ownership towards the system. The implementation team had to study the workflow processes that were going to be affected by the implementation. Through mapping and comparing the ‘desired workflow’ with the existing ‘actual workflow’, necessary adjustments to the actual workflow could be recognized and implemented before the system implementation. Those adjustments had to focus on reducing the number of involved steps and necessary synchronizations throughout the processes.
The importance of good communication during imaging procedures is beyond question. Diagnosis and treatment in the modern healthcare practice depend more and more on imaging procedures. The financial burden of these procedures on healthcare systems is of increasing trend [1,2]. If for any reason referring physicians and radiologists cannot communicate the necessary information correctly and efficiently, the result would not only be extra financial burden on healthcare system, but also unnecessary exposure of patients to ionizing radiation, delayed diagnosis and treatment, and patient disappointment [26]. Therefore improving the quality of physician-radiologist communication should be considered alongside the other plans for reducing the financial burden of diagnostic imaging expenditure. We argue that in applying information technology, it is critically important that the communication loop and the involved processes are kept as simple as possible. If an implementation requires involving more parties in the communication loop, workflow changes should be recognized and the devised workarounds should be supervised and managed closely to avoid unintended side effects. Moreover, for reducing communication related errors, it is critically important to close the communication loop between physician and radiologist [27]. There is always possibility for error in a hybrid system of electronic and paper-based. In our case, the communication loop could not be closed unless a digital radiography system and a Picture Archiving and Communication system (PACS) were implemented and integrated into the HIS.
This study had many limitations. The retrospectively collected data left much room for confounding factors that were difficult to manage. For example, we could not determine if the CXR requests and reports (in patients’ charts) were completed in the course of normal clinical care or later for insurance reimbursement purposes. Moreover, a singular record review is always vulnerable to error. Some of the workflow problems and patient safety issues may have already existed and the HIS system implementation simply made them more visible. We did not evaluate the implementation process; therefore, our study was unable to provide a complete overview on different aspects of this important issue. A large-scale in-depth qualitative study is required to understand what actually went wrong during the implementation process.
5. Conclusions
The HIS improved communication of administrative and identification information, but did not improve communication of clinically relevant information. The reason was traced to the complications that the inappropriate implementation of the system brought to clinical workflow and communication loop. Therefore, in implementing IT, the implementation team should strive to keep the communication loop between the clinicians as simple and as direct as possible. If an implementation requires involving more parties in the communication loop, workflow changes and devised workarounds should be supervised and managed closely.
Clinical Relevance Statement
For improving clinical communication by IT:
Communication improvement should be addressed in IT implementation strategies.
The actual clinical workflow processes should be mapped to the workflow designed into the system and necessary changes to the processes’ frame should be adopted before the implementation.
IT should be applied to simplify and to close communication loop between clinicians.
Conflict of Interest
The authors declare that they have no conflicts of interest in the research. The ideas discussed here are the authors’ opinion and do not reflect their organization’s position.
Human Subjects Protections
This study did not involve human subjects. The Ethical aspects of the study in accessing patients data was reviewed and approved by the Research Ethical Committee of Urmia University of Medical Sciences.
Acknowledgments
We would like to thank Dr. Davood Khorasani for his kind assistance in the study and Dr. Nassrollah Jabbari for commenting on the developed checklists.
References
- 1.Canadian Institute for Health Information, Hospital Cost Drivers Technical Report – What Factors Have Determined Hospital Expenditure Trends in Canada? (Ottawa, Ont.: CIHI, 2012). Available from: http://www.cihi.ca/CIHI-ext-portal/pdf/internet/HOSPITAL_COSTDRIVER_TECH_EN.(Cited on 5 April 2013) [Google Scholar]
- 2.The Health Care Cost and Utilization Report: 2011 tracks changes in health care prices, utilization, and spending on people younger than 65 covered by employer-sponsored private health insurance (ESI). Available from: http://www.healthcostinstitute.org/files/HCCI_HCCUR2011.pdf (Cited on 5 April 2013) [Google Scholar]
- 3.Mehrotra P, Bosemani V, Cox J. Do radiologists still need to report chest x rays? Postgrad Med J 2009; 85(1005): 339–341 [DOI] [PubMed] [Google Scholar]
- 4.Moncada DC, Rueda ZV, Macías A, Suárez T, Ortega H, Vélez LA. Reading and interpretation of chest X-ray in adults with community-acquired pneumonia. Braz J Infect Dis 2011; 15(6): 540–546 [PubMed] [Google Scholar]
- 5.Turkington P M, Kennan N, Greenstone M A. Misinterpretation of the chest x ray as a factor in the delayed diagnosis of lung cancer. Postgrad Med J 2002; 78: 158–160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wallis A, McCoubrie P. The radiology report – Are we getting the message across? Clinical radiology. Clin Radiol. 2011; 66(11): 1015–1022 [DOI] [PubMed] [Google Scholar]
- 7.Donnelly LF, Dickerson JM, Goodfriend MA, Muething SE. Improving patient safety in radiology. Am J Roentgenol 2010;194(5): 1183–1187 [DOI] [PubMed] [Google Scholar]
- 8.Cascade PN, Berlin L. Malpractice issues in radiology. American College of Radiology Standard for Communication. Am J Roentgenol 1999;173(6): 1439–1442 [DOI] [PubMed] [Google Scholar]
- 9.Stewart MJ, Georgiou A, Hordern A, et al. What do radiology incident reports reveal about in-hospital communication processes and the use of health information technology? Stud Health Technol Inform 2012; 178: 213–218 [PubMed] [Google Scholar]
- 10.Naik SS, Hanbidge A, Wilson SR. Radiology reports: examining radiologist and clinician preferences regarding style and content. Am J Roentgenol 2001; 176(3): 591–598 [DOI] [PubMed] [Google Scholar]
- 11.Song KS, Song HH, Park SH, Ahn KJ, Yang IK, Byun JY, Jeon JS, Kim JY, Kim BS, Lim GY, Kim YJ, Kim HS, Kim CY, Bahk YW. Impact of clinical history on film interpretation. Yonsei medical journal 1992; 33(2): 168–172 [DOI] [PubMed] [Google Scholar]
- 12.Garvey CJ, Connolly S. Radiology reporting--where does the radiologist’s duty end? Lancet 2006; 367(9508): 443–445 [DOI] [PubMed] [Google Scholar]
- 13.Alkasab TK, Alkasab JR, Abujudeh HH. Effects of a computerized provider order entry system on clinical histories provided in emergency department radiology requisitions. J Am Coll Radiol 2009; 6(3): 194–200 [DOI] [PubMed] [Google Scholar]
- 14.Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc 2011; 18(2): 169–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prevedello L, Khorasani R. Enhancing quality assurance and quality control programs: IT tools can help. J Am Coll Radiol 2009; 6(12): 888–889 [DOI] [PubMed] [Google Scholar]
- 16.Pirnejad H, Niazkhani Z, Berg M, Bal R. Intra-organizational communication in healthcare--considerations for standardization and ICT application. Methods Inf Med 2008: 47(4): 336–45 [PubMed] [Google Scholar]
- 17.Berg M. Implementing information systems in health care organizations: myths and challenges. Int J Med Inform 2001; 64(2-3): 143–156 [DOI] [PubMed] [Google Scholar]
- 18.Ammenwerth E, Talmon J, Ash JS, et al. Impact of CPOE on mortality rates--contradictory findings, important messages. Methods Inf Med 2006; 45(6): 586–593 [PubMed] [Google Scholar]
- 19.ACR ACR standard for communication: diagnostic radiology. In: Practice guidelines and technical standards. Reston, VA USA 1991, updated in 1995, 1999, 2001, and 2005. [Google Scholar]
- 20.Ridley LJ. Guide to the radiology report. Australas Radiol 2002; 46(4): 366–369 [DOI] [PubMed] [Google Scholar]
- 21.Poon Eric G, Blumenthal David Jaggi, Tonushree Honour Melissa M, Bates David W, Kaushal Rainu. Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals. Health Aff (Millwood) 2004; 23(4): 184–190 [DOI] [PubMed] [Google Scholar]
- 22.Aarts J, Berg M. Same systems, different outcomes – comparing the implementation of computerized physician order entry in two Dutch hospitals. Methods Inf Med 2006; 45(1): 53–61 [PubMed] [Google Scholar]
- 23.Kazemi A, Fors UG, Tofighi S, Tessma M, Ellenius J. Physician order entry or nurse order entry? Comparison of two implementation strategies for a computerized order entry system aimed at reducing dosing medication errors. J Med Internet Res 2010; 12(1): e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Niazkhani Z, Pirnejad H, van der Sijs H, Aarts J. Evaluating the medication process in the context of CPOE use: the significance of working around the system. International journal of medical informatics 2011; 80(7): 490–506 [DOI] [PubMed] [Google Scholar]
- 25.Novak LL, Holden RJ, Anders SH, et al. Using a sociotechnical framework to understand adaptations in health IT implementation. Int J Med Inform 2013; Apr 2. pii: S1386-5056(13)00020-8. doi: 10.1016/j.ijmedinf.2013.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amis ES Jr, Butler PF, Applegate KE, et al. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol 2007; 4(5): 272–284 [DOI] [PubMed] [Google Scholar]
- 27.Pirnejad H. Computerization of Healthcare Communication: On applying information technology to improve healthcare communication and concerns for patient safety. (PP: 126–130); VDM Verlag (24 Jul 2009). ISBN 9783639158618 [Google Scholar]


