Summary
Objective
Antimicrobial stewardship programs (ASPs) help meet quality and safety goals with regard to antimicrobial use. Prior to CPOE implementation, the ASP at our pediatric tertiary hospital developed a paper-based order set containing recommendations for optimization of dosing. In adapting our ASP for CPOE, we aimed to preserve consistency in our ASP recommendations and expand ASP expertise to other hospitals in our health system.
Methods
Nine hospitals in our health system adopted pediatric CPOE and share a common domain (Cerner Millenium™). ASP clinicians developed sixty individual electronic order sets (vendor reference PowerPlans™) to be used independently or as part of larger electronic order sets. Analysis of incidents reported during CPOE implementation and medication variances reports was used to determine the effectiveness of the ASP adaptation.
Results
769 unique PowerPlans™ were used 15,889 times in the first 30 days after CPOE implementation. Of these, 43 were PowerPlans™ included in the ASP design and were used a total of 1149 times (7.2% of all orders). During CPOE implementation, 437 incidents were documented, 1.1% of which were associated with ASP content or workflow. Additionally, analysis of medication variance following CPOE implementation showed that ASP errors accounted for 2.9% of total medication variances.
Discussion
ASP content and workflow accounted for proportionally fewer incidents than expected as compared to equally complex and frequently used CPOE content.
Conclusion
Well-defined ASP recommendations and modular design strengthened successful CPOE implementation, as well as the adoption of specialized pediatric ASP expertise with other facilities.
Key words: Medical order entry system, clinical decision support systems, clinical pharmacy information systems, workflow
Background
In 2007, the Infectious Diseases Society of America (IDSA) published a guideline for development of an institutional antimicrobial stewardship program (ASP), specifically identifying pediatric clinical settings as a priority [1]. ASPs have demonstrated improvement in validated quality metrics for adult and pediatric populations [2,3,4]. Two core strategies have been identified: prospective-audit with feedback, and formulary restriction and preauthorization. Although the abbreviation ‘ASP’ may also refer to ‘active server pages’ in computer programming literature, for most citations in medical literature ‘ASP’ refers to ‘antimicrobial stewardship program’.
As ASPs become more widespread, implementing ASPs for pediatric patients in community or general settings remains a challenge. Lack of funds as well as experienced personnel have impeded widespread implementation [5,6], particularly in pediatrics. Children have unique needs, particularly with regards to optimization of dosing, which are best served by the expertise of a pediatric infectious disease physician or clinical pharmacist. Additionally, barriers to communication and logistical obstacles can lead to prolonged approval times and possible delay in care [7]. In clinical settings where these important personnel are not present, clinical decision support (CDS) has been identified as one way that key elements of ASPs can be enabled in clinical settings [1].
Our pediatric hospital developed an ASP in 2008 to promote antimicrobial treatment optimization. The ASP team utilizes a preauthorization and restriction program, audits select antimicrobials, and provides feedback based on targeted audits. An extensive paper-based order form was required for antimicrobial ordering, which provided decision support through the recommendation of optimal dosing per pharmacokinetic and pharmacodynamic principles. Agents which required authorization by ASP team members prior to ordering (“restricted agents”) were clearly identified on the paper based order form. Pediatric patients at other hospitals in the health system were supported by adult antimicrobial stewardship programs or by phone consultation with pediatric infectious disease physicians at the specialty hospital or other pediatric infectious disease specialists in the community.
In 2011, a multidisciplinary team was tasked with implementing computerized prescriber order entry (CPOE) for pediatrics across nine facilities in a single health system. The inpatient facilities had ancillary services installed, exchange capabilities, nursing documentation, closed loop medication administration, physician documentation, and moderate data continuity across facilities at the time of CPOE implementation. These services had been implemented over the preceding 10 years, starting with admission and registration system in 2003. A subset of the development team was tasked to expand certain elements of the already-existing antimicrobial stewardship program (ASP) to all facilities through utilization of CPOE capabilities. The team included the pharmacists and physicians at the tertiary children’s hospital who support the ASP, as well as the informatics team.
Objectives
Our primary objectives in the implementation were to preserve consistency in our ASP recommendations within the pediatric academic center and share some ASP elements with other facilities in our health system, improve the ability of the ASP to monitor and audit restricted agents, and promote consistent communication with ASP team members providing approvals. Secondary objectives included education and support to physicians in their initial antimicrobial choices as well as identifying successful features of our design that could potentially be applied to electronic ordering of other medications and interventions.
Methods
System background and CPOE design intervention
The nine facilities that adopted pediatric CPOE share a common domain within the electronic health record (EMR) platform (Cerner Millenium™), and all facilities care for neonatal and/or pediatric patients. Major design goals for devising a strategy to adapt components of the existing paper-based ASP for use at several facilities using the established EMR system included:
share robust, evidence-based dosing information and best empiric choice for specific conditions among pediatric practitioners across multiple services at all facilities
devise a way to efficiently and consistently update information within the electronic order sets and
establish an electronic means to restrict ordering of specific antimicrobials.
Based on established paper-based order forms from our ASP, we designed a series of sixty individual electronic PowerPlans™ within our EMR. The content of the PowerPlans™ included recommended weight based dosing, as well as empiric indication-based recommendations. Content experts (infectious disease physicians and clinical pharmacists) provided guidance on adding to the existing paper based order forms and converting them to electronic PowerPlans™, providing dosing recommendations based on indication, age, weight, and other drug-specific factors. (► Figure 1). The Power-Plans™ were inserted into larger electronic order sets where suggested empiric antimicrobials were appropriate. This allowed the ASP team to provide the same utilization recommendations across multiple facilities and provided a way to efficiently update information.
Fig. 1.
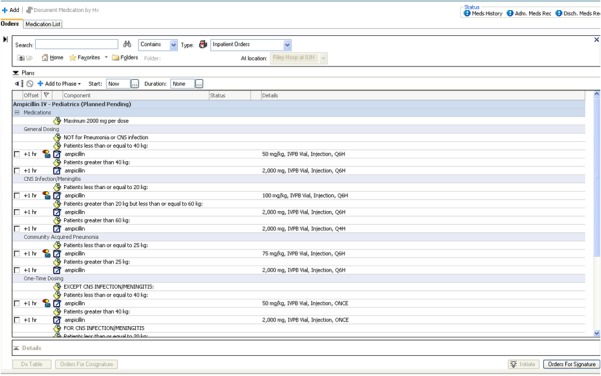
ASP PowerPlan™ providing recommendations based on indication, age, and weight
The management of restricted agents within antimicrobial stewardship is variable across the facilities in our health system, reflecting the differing staffing levels, specialty training and overall operations among our facilities. Preserving the operational efficiency of the pediatric ASP resources and allowing appropriate guidance for the outlying facilities was important. An additional challenge was to preserve the integrity of the shared domain of the Cerner EMR and uncluttered views in predominantly adult clinical settings.
Special verbiage and ordering instructions were used for restricted agent PowerPlans™ (► Figure 2) and are enhanced by a series of alerts that allowed for closer monitoring by ASP staff. The customizable alerts (vendor reference Discern™ alerts) are enabled only at the tertiary pediatric facility – other facilities manage their restriction program separately from the pediatric hospital. The alerts identify the restricted agents (► Figures 3 and ► Figure 4) and require the ordering prescriber to document the type of approval obtained to complete the order (i.e. by protocol, recommended by written ID consultation, or approved by an ASP team member). Upon order verification, the pharmacist may access and review the alert history to confirm approval of the drug prior to it being dispensed.
Fig. 2.
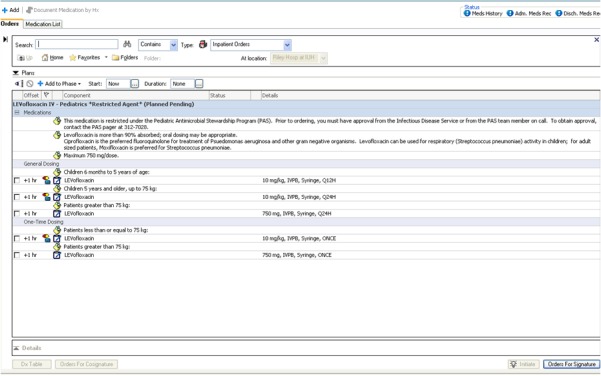
PowerPlan™ for restricted agent
Fig. 3.
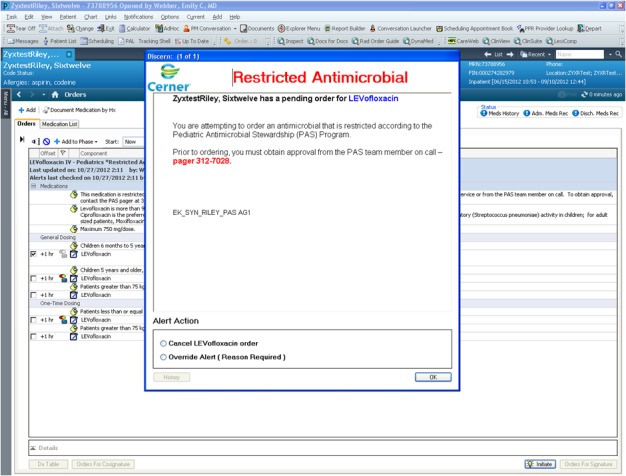
Alert for restricted antimicrobial.
Fig. 4.
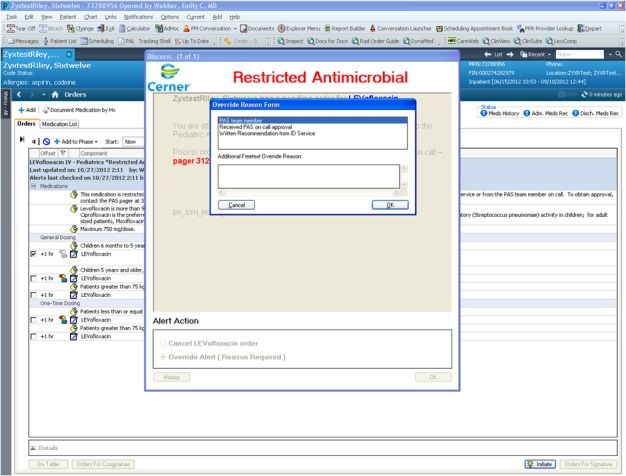
Alert requesting reason for override of restricted antimicrobial agent.
This design also allows changes to all ASP content to be made efficiently at a single point in the EMR by the ASP team. For example, if an agent is restricted due to a medication shortage, the restriction can be lifted after the agent becomes more widely available via adjustment of the alert settings. If best practice around infusion time or indications changed, the orders can be modified centrally, even those embedded in other order sets.
Measures of CPOE implementation
Changes in ASP Workflow
Following CPOE implementation, the ASP team generates reports based on alert reports that identify and evaluate the specifics of each restricted agent alert activation instance. ASP team members utilize alerts that fire on a daily basis and confirm that prescribers sought approval, as well as make recommendations on appropriate choice and duration of therapy. Prior to CPOE, this information was contained within a larger report and took additional time to manually evaluate. In cases where approval is not appropriately obtained, members of the ASP team can follow up with individual prescribers who are not in compliance with the ASP approval requirements.
Evaluation of implementation
As the facilities outside of the pediatric tertiary care hospital did not have the restriction alert enabled, the ASP team relied on voluntary reports of difficulty with PowerPlan™ usability or content at those facilities. We retrospectively reviewed three sets of data from the pediatric tertiary care hospital to determine the effectiveness of the implementation of the ASP within CPOE.
First, we reviewed the reports on frequency of ASP PowerPlans™ and restricted agents during implementation, using the reports of Discern™ alerts fired. These reports are automatically generated and helped determine whether the content was being utilized as frequently and easily as anticipated. We reviewed reports for a total of 60 days encompassing the immediate implementation period.
Second, a group of clinical pharmacists (an ASP program clinical pharmacist, a non-ASP clinical pharmacist, and an informatics pharmacist) and physicians (a pediatric hospitalist and an infectious disease specialist) performed independent reviews of the incident reports gathered during implementation. The incident reports for the first 21 days after CPOE implementation were collected in a multidisciplinary command center using phone calls, emails, and in-person reports collected by information services (IS) support staff. Incidents and reports after that point returned to regular practice and were collected through a central help desk using phone calls and emails. The reviewing group further classified the incidents into technical issues, content issues, or interface issues. Incidents that met multiple criteria were reviewed by all 5 reviewers and placed into the most appropriate category by group decision.
Third, review of medication variances in the months following implementation were also analyzed to identify issues associated with implementation arising after initial implementation was complete. Medication variances regarding any problems pertaining to safety and clinical care are self-reported by physicians, pharmacists and nurses. They are collected in an online incident reporting system and pertain to “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer.” [8] Clinical pharmacists analyzed 30 days of medication variance reports collected after implementation and after the command center closed as a sample to identify what proportion of these reports implicated ASP content, versus other CPOE-related issues. This provided information about the period of time immediately after the command center closed.
Results
ASP content utilization
During the study period, 769 PowerPlans™ were used, 43 of which were PowerPlans™ included in the ASP design. ASP plans were used a total of 1149 times, accounting for 7.23% of all orders placed. This frequency was similar during the time of the medication variance reports analysis (698 Power-Plans™ used, ASP content accounting for 7.37% of all orders).
Incidents reported to command center during implementation
Of the 437 tickets submitted during the evaluation period, 378 were incidents directly related to CPOE and only 4 (1.1%) were related to ASP content or workflow (► Table 1).
Table 1.
Incident tickets cataloged in CPOE implementation command center.
| Incident or Issue Reported | Occurrence % (n) |
|---|---|
| Content issues | |
| Request to change or correct order sentences, non-ASP content | 47(204) |
| Request to change or correct order sentences, ASP content | 1(4) |
| Technical issues | |
| Hardware issues, security access | 18 (79) |
| Documentation, printing of reports and forms not pertaining to CPOE | 14 (59) |
| Interface issues | |
| Monitoring System Change (Dashboard, Tracking Board) | 7 (30) |
| Training gap, requests for one-on-one assistance | 7 (29) |
| Workflow issue in specific units or with patient transfer | 7 (32) |
| Total | 100 (437) |
Of the number of requests for change in content, ASP PowerPlansTM accounted for 2 out of 60 requests (3.3%). Of the number of incidents surrounding alerts, ASP alerts accounted for 1 of 3 (33.3%) requests. This incident was related to notification of a duplicate gentamicin order, not content of the ASP PowerPlan™ itself.
Medication errors reported during implementation
Medication variance reports encompassing the first full month after implementation and subsequent months were reviewed (► Figure 5). The number of all medication variances during implementation (August), was higher than compared to subsequent months. None of the CPOE related medication variances contributed to harm to the patient and or required intervention. The 30 day period after the command center closed was reviewed in-depth by a team of 3 clinical pharmacists to examine the role of ASP content. Of the total 165 medication variances documented that month, 68 medication variances were CPOE related. Further review identified 2 of the errors related to ASP content design, accounting for 1.2% of the total reports that month.
Fig. 5.
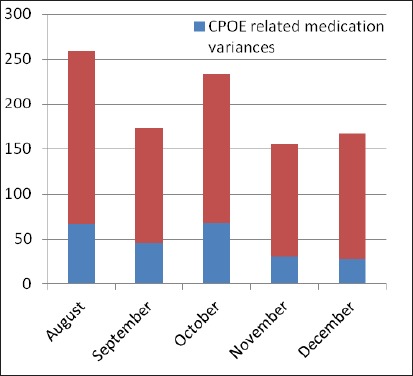
Proportion of CPOE-related incidents to all medication variance incidents.
Discussion
As a result of multidisciplinary design and adaptation process, the ASP content and workflow was widely adopted during CPOE and accounted for proportionally fewer incidents at our institution than other elements of CPOE during the implementation process and in subsequent months. ASP content accounted for approximately 7% of all orders during implementation but did not account for that proportion of CPOE-related problems. Incidents documented in our command center and voluntary medication variances reported in our incident reporting system both reflect a range of CPOE-related issues but fewer related to ASP content and workflow than other plans of similar complexity and frequency. We contend that this reflects an effective design for ASP implementation utilizing a vendor EMR at a pediatric academic center with clinical support, as well as a potential means to expand ASP support to other facilities within our health system.
Adoption of the ASP to CPOE within our common domain had many positive gains. Similar to previous studies [9], CPOE entry allows for ASP reports to be generated for select populations, eliminating much of the manual review necessary prior to CPOE. The improved transparency for prescribers regarding restricted antimicrobial agents at our pediatric hospital has promoted collaboration between the ASP team and other clinicians as well. The modular structure of inserting Power-Plans™ into larger order sets, as well as serving as “stand alone” orders, allowed our ASP content (chiefly dosing recommendations and recommendations for empiric indications) to be “shared” at other facilities that treat pediatric patients; however, not all have pediatric pharmacists and infectious disease specialists to provide support. Lack of these specialized resources is a problem highlighted as a key future direction of ASP efforts [1]. Community and general hospital settings in our health system can now use pediatric ASP PowerPlans™ containing indication based optimum dosing, even without access to a pediatric infectious disease physician or clinical pharmacist.
Additionally, as the PowerPlans™ for individual antibiotics are embedded in indication based PowerPlans™, adjustments and updates made to a single PowerPlan™ can be immediately disseminated within the appropriate order sets, providing another layer of CDS and allowing for efficient and widely disseminated changes. Since implementation, there has also been a subjective improvement in collaboration. Neonatologists and pharmacists collaborated on reordering the gentamicin orders to promote the most frequently used and effective dosing. Additionally, facilities have viewed additional content from the pediatric ASP PowerPlans™ in surgery and emergency department settings.
Using CDS to augment appropriate antibiotic use and selection was documented over a decade ago [10], and efforts to optimize the use of CDS continue [11,12]. Assessment of an antimicrobial decision support tool showing a reduction in costs due to unnecessary or inappropriate antibiotics has also been widely documented [13-17]. However, most clinical informaticians are still experimenting and improving on the most effective application of CDS tools to support the tenets of antimicrobial stewardship.
Identifying the best clinical decision support for a specific scenario that allows for incorporation requires clinical knowledge, awareness of workflow, and informatics literacy. A recent review of EMR vendor products identified 53 types of front end clinical decision support tools [18] that could be applied.
Cloud or web-based hosting is an emerging and intriguing area of development. In 2008, Agwu and colleagues [8] described a web-based application for antimicrobial stewardship support at a pediatric tertiary care hospital. The preapproval ASP system was a repository of information, as well as a communication tool, hosted on a secure server and allowed prescribers to submit requests with rationale for restricted agents. Implementation of this system in paper-order based environment produced a decrease in restricted agents ordered, a decrease in missed or delayed doses, and cost savings of $370,000 in the first year. The system was immensely useful, and was designed to encourage communication and discussion with pediatric infectious disease specialists. This did prove difficult to export to other systems without similar resources to support it. Despite this limitation, the web-based antimicrobial stewardship program showed sustained savings [17]. The data gathered also demonstrated that restricted antimicrobials have a higher cost per capita, accounting for 26% of the total doses and 81% of the antimicrobial charges, the majority of which was due to 5 restricted drugs.
Effectively and efficiently adopting antimicrobial stewardship into an inpatient EMR requires providing the prescriber with the best choices for the patient, adhering to clinical guidelines for empiric choices, and using restricted agents with caution. This results in many different institutions struggling to recreate the content for ASPs, particularly as more providers adopt predominantly vendor EMR systems and struggle to balance information accessibility and security issues.
Hermsen et al describe use of a retrospective query in TheraDocTM to augment and increase intervention attempts by ASP personnel [19]. Their prospective audit with intervention ASP highlighted importance of effective clinical decision support to be integrated into clinical workflow. Although this method is widely thought to be more effective than restriction models of ASP [20], implementing such a system requires significant resources beyond the means of many hospitals. The authors concluded, “The introduction of a CDS[S] allowed systematic performance of prospective audit with intervention and feedback.”
We faced similar circumstances as previous authors [9,19,21] when integrating our ASP into our EMR; however, there were some notable differences. One advantage was that CPOE implementation occurred several years after a widely accepted ASP program was established, rather than concurrently. Additionally, the design of our ASP included significant, directive front-end clinical decision support at the level of the physician, as well as a structure utilizing system queries that allowed for expedited audits by our ASP team. The paper based order form (supporting a formulary restriction and preauthorization structure) lent itself well to CPOE design, and the ASP team has also sustained ongoing improvements. Finally, we faced the challenge of expanding parts of our ASP (dosing and indication recommendations) for pediatric patients at 8 general hospital settings. Making our ASP content generalizable within our health system meant developing and sharing content with community and non-pediatric providers.
One unanticipated consequence of the modular design was its impact on our surgery workflow. In the paper process, multiple order sets appeared in a single stack of papers; transitioning to separate order sets for antimicrobials required additional and ongoing education. Understanding workflow is necessary to success, since a single workflow can impact multiple processes.
There are limitations to our ASP program as well as the evaluation of the implementation. Since this study focused on the design and implementation of ASP in CPOE, the long-term impact will need to be examined long term. Our review of incidents during the implementation as well as the medication variances in following months were both voluntarily reported, which could have produced a biased selection. Retrospective review does not always identify whether an incorrect medication dose selection or other CPOE-related incident is due to provider knowledge, workflow, or confusion from the ASP design. As most incidents related to errors may be multi-factorial, this could underestimate the number of incidents attributed to ASP content and program implementation. Finally, we reviewed PowerPlan™ use and medication variances from the pediatric hospital only. Although the other facilities using the ASP content submitted their concerns during implementation to the command center, we did not have other comprehensive markers for the usability and implementation of the ASP content by outside groups during the implementation period.
Future initiatives planned for the ASP program CPOE intervention include assessing reduction in time from order to drug administration, evaluating barriers to efficient use of the PowerPlans™, and utilizing the ASP program for more prospective audit opportunities across the health system.
Conclusions
Customizing our vendor EMR provided an effective design strategy to preserve and enhance our existing pediatric ASP at our tertiary care hospital and allowed the extension of some elements of the ASP support to other hospitals in our health system. Although these facilities may not have pediatric pharmacy or ID resources to fully operationalize a pediatric ASP team, they were able to use the ASP-recommended content. When compared to similarly complex PowerPlans™ that are used with the same frequency, the incident reports and medication variations related to the ASP design was proportionally less. We conclude that this reflected an effective adaptation and enhancement of existing ASP workflow into a vendor EMR with minimal disruption.
This adaptation may serve as a model for future endeavors to implement new elements of the EMR, as well as improve existing processes. Like most CPOE implementations, new problems arose; however, the increased transparency in prescribing practices, ability to control recommended dosing and choices centrally, and the ability to make expedited improvements were desirable benefits.
Clinical Relevance
As more health care providers implement vendor products, success in implementation and improvements will depend on workflow, clinical expertise, and the usability and adaptability of the EMR platform. The design, adaptation, and implementation of our existing pediatric antimicrobial stewardship resources to our vendor EMR product was successful because of careful planning and may prove useful for other groups adopting similar EMR products or clinical programs.
Conflict of Interest
The authors declare that they have no conflicts of interest in the research.
Protection of Human and Animal Subjects
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by the Indiana University Institutional Review Board.
Contributorship
All six authors of the above authors meet criteria for authorship including 1) substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; 2) drafting the article or revising it critically for important intellectual content; and 3) final approval of the version to be published. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Newland JG, Hersh AL. Purpose and design of antimicrobial stewardship programs in pediatrics. Pediatr Infect Dis J 2010; 29: 862–863 [DOI] [PubMed] [Google Scholar]
- 2.Di Pentima MC, Chan S, Eppes SC, Klein JD. Antimicrobial prescription errors hospitalized children: role of antimicrobial stewardship program in detection and intervention. Clin Pediatr 2009; 48: 505–512 [DOI] [PubMed] [Google Scholar]
- 3.Metjian TA, Prasad PA, Kogon A, Coffin SE, Zaoutis TE. Evaluation of an antimicrobial stewardship program at a pediatric teaching hospital. Pediatr Infect Dis J 2008; 27: 106–111 [DOI] [PubMed] [Google Scholar]
- 4.Carling P, Fung T, Killion A, Terrin N, Barza M. Favorable impact of a multidisciplinary antibiotic management program conducted during 7 years. Infect Control Hosp Epidemiol 2003; 24:699–706 [DOI] [PubMed] [Google Scholar]
- 5.Hersh AL, Beekmann SE, Polgreen PM, Zaoutis TE, Newland JG. Antimicrobial stewardship programs in pediatrics. Infect Control Hosp Epidemiol. 2009: 30(12): 1211–1217 [DOI] [PubMed] [Google Scholar]
- 6.Johannsson B, Beekmann SE, Srinivasan A, Hersh AL, Laxminaravan R, Polgreen PM. Improving antimicrobial stewardship: the evolution of programmatic strategies and barriers. Infect Control Hosp Epidemiol 2211: 32(4): 367–374 [DOI] [PubMed] [Google Scholar]
- 7.Sunenshine RH, Liedtke LA, Jernigan DB, Strausbaugh LJ. Role of infectious diseases consultants in management of antimicrobial use in hospitals. Clin Infect Dis 2204: 38(7): 934–938 [DOI] [PubMed] [Google Scholar]
- 8.The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP). Accessed on September 11, 2013, http://www.nccmerp.org/ [DOI] [PubMed] [Google Scholar]
- 9.Agwu AL, Lee CK, Jain SK, Murray KL, Topolski J, Miller RE, Townsend T, Lehmann CU. A World Wide Web-based antimicrobial stewardship program improves efficiency, communication, and user satisfaction and reduces cost in a tertiary care pediatric medical center. Clin Infect Dis 2208: 47(6): 747–753 [DOI] [PubMed] [Google Scholar]
- 10.Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme JF Jr, Lloyd JF, Burke JP. A computer assisted management program for antibiotics and other antiinfective agents. N Engl J Med 1998; 338: 232–238 [DOI] [PubMed] [Google Scholar]
- 11.Linder JA, Bates DW, Williams DH, Connolly MA, Middleton B. Acute infections in primary care: accuracy of electronic diagnoses and electronic antibiotic prescribing. J Am Med Inform Assoc 2006; 13: 61–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mainous AG 3rd, Lambourne CA, Nietert PJ. Impact of a clinical decision support system on antibiotic prescribing for acute respiratory infections in primary care: quasi-experimental trial. J Am Med Inform Assoc 2013; 20: 317–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pestotnik SL, Classen DC, Evans RS, Burke JP. Implementing antibiotic practice guidelines through computer-assisted decision support: clinical and financial outcomes. Ann Intern Med 1996; 124: 884–890 [DOI] [PubMed] [Google Scholar]
- 14.McGregor JC, Weekes E, Forrest GN, Standiford HC, Perencevich EN, Furuno JP, Harris AD. Impact of a computerized clinical decision support system on reducing inappropriate antimicrobial use: a randomized control trial. J Am Med Inform Assoc 2006; 13: 378–384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sáez-Llorens X, Castrejón de Wong MM, Castaño E, De Suman O, De Morös D, De Atencio I. Impact of an antibiotic restriction policy on hospital expenditures and bacterial susceptibilities: a lesson from a pediatric institution in a developing country. Pediatr Infect Dis J 2000; 19(3): 200–206 [DOI] [PubMed] [Google Scholar]
- 16.Ozkurt Z, Erol S, Kadanali A, Ertek M, Ozden K, Tasyaran MA. Changes in antibiotic use, cost and consumption after an antibiotic restriction policy applied by infectious disease specialists. Jpn J Infect Dis 2005; 58(6): 338–343 [PubMed] [Google Scholar]
- 17.Sick AC, Lehmann CU, Tamma PD, Lee CK, Agwu Al. Sustained savings from a longitudinal cost analysis of an internet-based preapproval antimicrobial stewardship program. Infect Control Hosp Epidemiol 2213: 34(6): 573–580 [DOI] [PubMed] [Google Scholar]
- 18.Wright A, Sittig DF, Ash JS, Feblowitz J, Meltzer S, McMullen C, Guappone K, Carpenter J, Richardson J, Simonaitis L, Evans RS, Nichol WP, Middleton B. “Development and evaluation of a comprehensive clinical decision support taxonomy: comparison of front-end tools in commercial and internally developed electronic health record systems. J Am Med Inform Assoc 2011;18:232–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hermsen ED, VanSchooneveld TC, Sayles H, Rupp ME. Implementation of a clinical decision support system for antimicrobial stewardship. Infect Control Hosp Epidemiol 2012; 33: 412–414 [DOI] [PubMed] [Google Scholar]
- 20.Dellit TH, Owens RC, McGowan JE Jr, Gerding DN, Weinstein RA, Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF, Brennan PJ, Billeter M, Hooton TM. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007: 15; 44(2): 159–177 [DOI] [PubMed] [Google Scholar]
- 21.Thursky K. Use of computerized decision support systems to improve antibiotic prescribing. Expert Rev Anti Infect Ther 2006; 4: 491–507 [DOI] [PubMed] [Google Scholar]


