Abstract
Human protothecal infection is uncommon and could be localized or systemic disease. Disseminated Prototheca algaemia tends to occur in immunocompromised patients (solid organ transplants, hematological malignancies) with high mortality. Diagnosis could be missed or delayed due to unusual clinical presentation and/or under-recognition of characteristic microscopic features of Prototheca species. Combined approach that includes removal of source of infection and intravenous amphotericin B provides the best chance of cure.
Keywords: Prototheca spp, Algaemia, Cholestatic hepatitis, Systemic lupus erythematosus
1. Introduction
Protothecosis is a rare infection caused by Prototheca species (spp.), which are considered to be algae and are ubiquitous in nature; in trees, lakes, rivers, sewage treatment plants, soil, and household garbage [1]. They cause infections in both humans and animals. Human protothecosis is uncommon and mostly causes cutaneous infections and olecranon bursitis from repeated traumatic inoculation. In immunocompromised hosts, it can disseminate to viscera causing life-threatening sepsis [4]. As a further contribution, we report a patient on immunosuppressive therapy for systemic lupus erythemaotosus (SLE) and thrombotic thrombocytopenic purpura (TTP) who presented with sepsis and cholestatic hepatitis from Prototheca wickerhamnii algaemia. To our best knowledge, it is the first case report of disseminated Prototheca algaemia in a patient with SLE who presented as cholestatic jaundice and hepatitis as the atypical clinical presentation of systemic protothecosis and she was successfully treated with intravenous amphotericin B. We review reported cases of Prototheca algaemia in the literature and analyze those patients' characteristics, treatment modalities and their outcomes.
2. Case
A 38-year-old woman was transferred from an outside facility for management of refractory autoimmune thrombotic thrombocytopenic purpura (TTP). The patient had a history of hemodialysis-dependent chronic kidney disease due to systemic lupus erythematosus. She routinely received hemodialysis through an arterio-venous fistula (AVF) in the right forearm. The patient received high dose corticosteroids, plasma exchange, and rituximab for TTP. On physical examination, she appeared fatigued with icteric sclera but normal skin and musculoskeletal findings. Remainder of physical examination was normal.
Her hospital course was complicated by persistent fever 102 °F (38.9 °C) and jaundice on hospital day 7. The white blood cell count was 11,200 cells/mm3 (reference range 4000–11,000) with neutrophilia of 82%. Liver function tests revealed total bilirubin 27.5 mg/dL (reference range 0.4–1.4), direct bilirubin 19.4 mg/dL (reference range 0.1–0.3), with elevated alkaline phosphatase 934 units/L (reference range 39–117), alanine aminotransferase 205 units/L (reference range 10–44) and aspartate aminotransferase 219 units/L (reference range 14–40). International normalization ratio (INR) was elevated at 1.5. Blood cultures and serologic studies were submitted. CT scan of abdomen illustrated normal hepatobiliary and gastrointestinal system. A set of blood cultures was positive of Enterococcus faecalis and Pseudomonas aeruginosa and intravenous piperacillin–tazobactam and gentamicin were started. The patient underwent both transthoracis and transesophageal echocardiograms which did not reveal vegetations.
The same blood cultures were also positive for few colonies of yeasts after 72 h of incubation. Intravenous micafungin was initiated while awaiting further identification. Microscopic examination of slide cultures from Sabouraud's Dextrose Agar (SDA) plates demonstrated 2–8 tightly packed endospores within a sporangium resembling a daisy (Fig. 1). These features were compatible with Prototheca wickerhamii which was confirmed by phenotypic analysis. Since only 2 colonies of Prototheca organisms were seen on the SDA culture plate, the possibility of contamination could not be ruled out. However, several subsequent sets of blood cultures over a period of 5 days were also positive of organisms with similar features of P. wickerhamii. Intravenous amphotericin B deoxycholate (1 mg/kg/d) was started on day 10 of hospitalization with clearance of Prototheca from the blood cultures followed by steady clinical improvement. Intravenous micafungin was discontinued. Abnormal liver function values were markedly improved following administration of amphotericin B (Fig. 2). Skin and musculoskeletal examination showed normal findings. No central venous catheter was noted. Ultrasonogram of AVF did not reveal fluid collection as a source of protothecal sepsis. Stool cultures were negative for Prototheca spp. Intravenous piperacillin–tazobactam, gentamicin and amphotericin B deoxycholate were continued for total 4 weeks. However, she eventually succumbed to multi-organ failure from central venous catheter-related multi-drug resistant Pseudomonas aeruginosa and vancomycin-resistant Enterococcus faecium bacteremia on day 78 of hospitalization. P. wickerhamii was not re-isolated after 60 days from the initial sterile blood cultures. An autopsy was not performed.
Fig. 1.
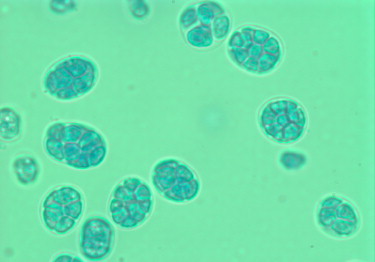
Lactophenol cotton blue stain of blood isolate showing 2–8 tightly packed endospores within a sporangium—the hallmark morula form or a daisy appearance of Prototheca wickerhamii (original magnification 1000 times).
Fig. 2.
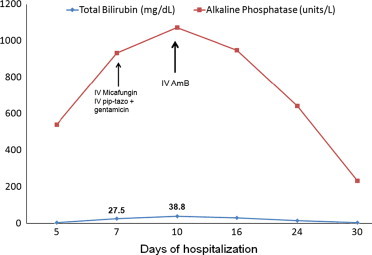
Trend of patient's serum total bilirubin and alkaline phosphatase levels before and after administration of intravenous amphotericin B. AmB—amphotericin B deoxycholate; pip–tazo—piperacillin–tazobactam.
3. Discussion
Prototheca spp. are achlorophyllous saprophytic algae and are ubiquitous in nature, being commonly isolated from grass, soil, water, and both wild and domesticated animals [1,3]. They also colonize the human skin, fingernails, respiratory tract and digestive system [3,4]. Protothecosis is endemic in animals, especially in cattle with bovine mastitis being the most commonly recognized manifestation [5]. In humans, there are 3 recognized forms of protothecosis: cutaneous (66%), olecranon bursitis (15%), and disseminated infections (19%) [2]. Among Prototheca spp., P. wickerhamii is the most common cause of human infections, followed by P. zopfii. The main underlying conditions are solid organ transplantation, hematological malignancies with/without stem cell transplants, alcoholism, diabetes mellitus, chronic glucocorticoid use, peritoneal dialysis, HIV/AIDS, and cancers [2]. Our patient is the first report in which systemic protothecosis has been associated with systemic lupus erythematous (SLE). There is one previous report of a localized cutaneous protothecal infection in a patient with SLE [6]. It is also the third reported case of cholestatic hepatitis as clinical manifestation from disseminated protothecosis infection.
The first case report of human protothecosis was described in 1964 in a Sierra Leonean rice farmer presenting with a rash on the foot following repeated trauma [7]. Subsequently more than 100 human cases have been reported [2,8]. The typical skin manifestation is a slowly progressive well-circumscribed plaque or vesiculobullous lesions which may progress to develop a necrotic crust. Some lesions develop a purulent discharge [9–11]. Predisposing factors include accidental local trauma or post-operative wounds. Prototheca infection of the olecranon bursa probably results from repeated trauma. Clinical presentations of olecranon bursitis are induration, erythema, and tenderness of the bursa [12–14].
Disseminated protothecosis occurs in immunocompromised hosts, and most notably involves blood, meninges, lymph nodes, lung, intestines, gall bladder, liver, spleen, and peritoneum [2,15]. There have been 18 reported cases of disseminated Prototheca algaemia as listed in Table 1. Prototheca zopfii algaemia accounts for only 2 patients. All patients received a wide range of immunosuppressants including MOPP (mechlorethamine, vincristine, procarbazine, prednisone), prednisone, cytosine arabinoside, mitoxantrone, azathioprine, cyclosporine A, tacrolimus, mycophenolate mofetil, gemtuzumab and infliximab. Twelve out of 18 patients (65%) with disseminated Prototheca algaemia died. On reviewing reported cases, solid organ transplant recipients notably had the highest mortality of 100%, followed by patients with hematological malignancies (50% mortality). Intravenous amphotericin B alone, either as deoxycholate or lipid formulation, was the most commonly used therapy in disseminated protothecal infection. All 6 patients, who did not receive amphotericin B therapy, died. On the other hand, among 12 patients treated with intravenous amphotericin B, only 6 patients survived (50% mortality), which includes 4 patients with hematological disorders, 1 patient with myasthenia gravis and 1 patient with an unknown defect in cellular immunity. It is of interest that both patients infected with P. zopfii died including one who was treated with intravenous amphotericin B.
Table 1.
List of reported cases of patients with disseminated Prototheca algaemia.
| Underlying conditions | Prototheca spp. | Co-infections | Treatment | Outcome | Reference |
|---|---|---|---|---|---|
| Solid organ transplants | |||||
| Heart | P. wickerhamii | C. glabrata, CMV viremia | Capsofungin | Died | Nwanguma et al. [16] |
| Heart | P. wickerhamii | None | LAmB | Died | McMullan et al. [17] |
| Kidney | P. wickerhamii | None | NA | Died | Mohd et al. [18] |
| Liver | P. wickerhamii | VRE. faecium, E. coli; CMV viremia | AmB | Died | Narita et al. [19] |
| Lung | P. zopfii | CMV viremia | Not mentioned | Died | Kwok and Schwartz [20] |
| Hematologic diseases | |||||
| SCTa, GVHD | P. wickerhamii | K. pneumoniae | LAmB | Died | Khoury et al. [21] |
| CLL | P. wickerhamii | E. coli | Voriconazoleb | Died | Lanotte et al. [22] |
| MDS, SCT | P. wickerhamii | None | AmB | Died | Hariprasad et al. [23] |
| AML, allogenic SCT | P. zopfii | None | LAmB | Died | Lass-Flörl et al. [24] |
| AML, allogenic SCT | P. spp. | E. faecalis, Leuconostoc spp. | LAmB | Cured | Torres et al. [10] |
| AML | P. wickerhamii | None | AmB | Cured | Kunovà et al. [25] |
| AML | P. wickerhamii | VRE. faecium, E. coli | LAmB+voriconazole | Cured | Gaur et al. [26] |
| Hodgkin's lymphoma | P. wickerhamii | S. epidermidis, C. glabrata | AmB | Cured | Heney et al. [27] |
| Others | |||||
| Myasthenia Gravis, prednisone, cyclosporine | P. wickerhamii | C. glabrata | AmB, AmBLC | Cured | Mohabeer et al. [28] |
| Cell-mediated immune defect | P. wickerhamii | None | AmB, transfer factor | Cured | Cox et al. [15] |
| Colon cancer | P. wickerhamii | None | Fluconzole | Died | Marr et al. [29] |
| AIDS | P. wickerhamii | None | Itraconazole, AmB | Died | Pascual et al. [31] |
| Sheehan's syndrome, chronic prednisone use | P. wickerhamii | None | Cefazolinc | Died | Joubert et al. [32] |
| SLE | P. wickerhamii | E. faecalis, Pseudomonas aeruginosa | AmB | Diedd | Our index patient |
AML—acute myeloid leukemia; SCT—stem cell transplant; GVHD—graft-versus-host disease; CLL—chronic lymphocytic leukemia; MDS—myelodysplastic syndrome; SLE—systemic lupus erythematosus; AIDS—acquired immune deficiency syndrome.
AmB—amphotericin B deoxycholate; LAmB—liposomal amphotericin B; AmBLC—amphotericin B lipid complex.
VRE. fecium—vancomycin-resistant Enterococcus faecium; E. faecalis—Enterococcus faecalis; E. coli—Escherichia coli; K. pneumoniae—Klebsiella pneumoniae; S. epidermidis—Staphylococcus epidermidis; C. glabrata—Candida glabrata; CMV—Cytomegalovirus.
NA—not available, patient died a day after admission before initiation of antifungal therapy.
No information on underlying hematological malignancy.
For possible pulmonary aspergillosis.
The patient died before the diagnosis was made.
Died from Pseudomonas and VRE septicemia.
Diagnosis of protothecosis is dependent on histological findings or microbiological isolation of the organism from affected sites or blood. Colony characteristics of Prototheca spp. resemble to other yeast-like organisms such as Candida or Cryptococcus [20,32]. There have been case reports that mis-identified P. wickerhamii as “non-albicans Candida spp.” which resulted in delayed or inappropriate therapy [16,17]. There were also reported cases in which a diagnosis could not be made ante-mortem due to severity of the disease [18,22,32]. Prototheca spp. are unicellular, oval organisms that reproduce asexually by internal septation and irregular cleavage to produce 2–20 sporangiospores which are arranged in a pathognomonic “morula” form or spoked wheel appearance (Fig. 1). Characteristic histological features in cutaneous disease are chronic granulomatous inflammation with giant cells, histiocytes, lymphocytes and plasma cells accompanied by the presence of abundant Prototheca organisms [10,31,33]. Cox et al. demonstrated cholestatic hepatitis on liver biopsy in a jaundiced patient with disseminated Prototheca sepsis [15]. Chan et al. also reported a patient with hepatobiliary protothecosis who presented as obstructive jaundice with chronic granulomatous lesions on the liver, gall bladder and duodenum [30]. In our patient, we believe that the cholestatic jaundice she developed was a consequence of granulomatous hepatitis due to systemic protothecosis, and she had a remarkable clinical and biochemical response to intravenous amphotericin B therapy.
Interestingly, as in our patient, it is not uncommon to identify blood stream infections with other co-pathogens in patients (50%). Most common isolates were Enterococcus faecalis [10, our patient], vancomycin-resistant Enterococcus faecium (VRE) [19,26], Escherichia coli [19,22,26], cytomegalovirus (CMV) [16,19,20] and Candida glabrata [16,27,28]. As in our patient, it is noted that there was more than one organism in 5 patients of whom 2 of them died. The concomitant polymicrobial infection did not seem to correlate with increased mortality but it was related to the presence of indwelling central venous catheters. Nevertheless, the significance of clinical impact of this mixed infection is unclear. The mortality of all reported patients was secondary to the direct effect of protothecal algaemia whereas our patient died from bacterial septicemia.
The other observation is the source of disseminated infection which was only identified in 50% of patients. Central venous catheters (Groshong or Hickman catheters) [10,26,27] and cutaneous lesions [23,24,26,28,29,31,32] are proved to be the most common infective nidus of protothecal algaemia. Among patients with cutaneous lesions, one patient also had protothecal olecranon bursitis [29] and there was simultaneous protothecal septic arthritis and synovitis of the left ankle in another patient [31]. Unfortunately, we could not identify the source of infection in our patient.
There is no consensus on treatment of protothecosis due to the rarity of the disease. Optimal drugs and duration of therapy are not standardized. However, proposed therapeutic strategies derived from case reports and case series include combined surgical and medical therapies. Surgical approaches include surgical debridement of involved skin, and other affected tissues when possible. Bursectomy for olecranon bursitis, and removal of central venous and peritoneal dialysis catheters can be important in recovery [2]. Reports of successful medical therapy with amphotericin B, gentamicin, amikacin, doxycyline, fluconazole, voriconazole and itraconazole suggest a broad array of potentially effective agents [2,34,35]. In vitro susceptibility tests of Prothoteca spp. can be performed but are not routinely available. It is noticed that there is no strong correlation with in vitro activity and clinical response [18]. Prototheca spp. possess cell membranes with 4% ergosterol that could be the reason for susceptibility to antifungal agents such as polyenes and azoles [2,35,36]. Among antifungals, amphotericin B has the best in vitro activity against Prototheca spp. Absence of d-glucans in their algal cell walls is likely responsible for resistance to echinocandins [37]. There is a synergistic effect between intravenous amphotericin B and oral tetracycline demonstrated by checkerboard technique [38]. By using this information, there have been reported cases of successful treatment with combined intravenous amphotericin B and oral doxycycline in patients with cutaneous and peritoneal protothecosis [9,38,39]. However, this combination has not been applied in systemic algaemia from Prototheca spp., in which intravenous amphotericin B alone is the only systemic antifungal therapy that has been shown to be effective in case series.
4. Conclusion
To the best of our knowledge, this is the first reported case of P. wickerhamii algaemia in a patient with SLE presenting as cholestatic hepatitis. It highlights to clinicians that cholestatic jaundice is part of the variable clinical presentations in patients with systemic visceral protothecosis. Laboratory technicians should also be aware of the pathognomonic microscopic features of Prototheca spp. (“morula” appearance) that would definitely help in the accurate diagnosis and optimal treatment. Intravenous amphotericin B with removal of the source of infection is the most effective approach in systemic disseminated protothecosis. Our case adds to the limited evidence of the role of amphotericin B in the treatment of algaemia from P. wickerhamii. However, the clinical cure rate of systemic Prototheca algaemia is noted to be only 50% in reported case series in which solid organ transplant recipients have the highest mortality.
Conflict of interest statement
There are no competing interests.
Acknowledgments
We would like to extend our thanks to Drs. Victoria Johnson and Edward W. Hook III for their support and critical suggestions on this submitted manuscript.
References
- 1.Pore R.S., Barnett E.A., Barnes W.C., Jr., Walker J.D. Prototheca ecology. Mycopathologia. 1983;81:49–62. doi: 10.1007/BF00443909. [DOI] [PubMed] [Google Scholar]
- 2.Lass-Flörl C., Mayr A. Human protothecosis. Clinical Microbiology Reviews. 2007;20:230–242. doi: 10.1128/CMR.00032-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huerre M., Ravisse P., Solomon H., Ave P., Briquelet N., Maurin S. Human protothecosis and environment. Bulletin de la Societe de Pathologie Exotique. 1993;86:484–488. [PubMed] [Google Scholar]
- 4.Wirth F.A., Passalacqua J.A., Kao G. Disseminated cutaneous protothecosis in an immunocompromised host: a case report and literature review. Cutis. 1999;63:185–188. [PubMed] [Google Scholar]
- 5.Jensen H., Aalbaek B., Bloch B., Huda A. Bovine mammary protothecosis due to Prototheca zopfii. Medical Mycology. 1998;36:89–95. [PubMed] [Google Scholar]
- 6.Tsuji K., Hirohara J., Fukui Y., Fujinami S., Shiozaki Y., Inoue K. Protothecosis in a patient with systemic lupus erythematosus. Internal Medicine. 1993;32(7):540–542. doi: 10.2169/internalmedicine.32.540. [DOI] [PubMed] [Google Scholar]
- 7.Davies R.R., Spencer H., Wakelin P.O. A case of human protothecosis. Transactions of the Royal Society of Tropical Medicine and Hygiene. 1964;58:448–451. doi: 10.1016/0035-9203(64)90094-x. [DOI] [PubMed] [Google Scholar]
- 8.Krcméry V., Jr Systemic chlorellosis, an emerging infection in humans caused by algae. International Journal of Antimicrobial Agents. 2000;15:235–237. doi: 10.1016/s0924-8579(00)00150-3. [DOI] [PubMed] [Google Scholar]
- 9.Venezio F.R., Lavoo E., Williams J.E., Zeiss C.R., Caro W.A., Mangkornkanok-Mark M. Progressive cutaneous protothecosis. American Journal of Clinical Pathology. 1982;77:485–493. doi: 10.1093/ajcp/77.4.485. [DOI] [PubMed] [Google Scholar]
- 10.Torres H.A., Bodey G.P., Tarrand J.J., Kontoyiannis D.P. Protothecosis in patients with cancer: case series and literature review. Clinical Microbiology and Infection. 2003;9:786–792. doi: 10.1046/j.1469-0691.2003.00600.x. [DOI] [PubMed] [Google Scholar]
- 11.Lu S., Xi L., Qin W., Luo Y., Lu C., Li X. Cutaneous protothecosis: two new cases in China and literature review. International Journal of Dermatology. 2012;51(3):328–331. doi: 10.1111/j.1365-4632.2011.05019.x. [DOI] [PubMed] [Google Scholar]
- 12.Ahbel D.E., Alexander A.H., Kleine M.L., Lichtman D.M. Protothecal olecranon bursitis. A case report and review of the literature. Journal of Bone and Joint Surgery, American Volume. 1980;62(5):835–836. [PubMed] [Google Scholar]
- 13.Nosanchuk J., Greenberg R. Protothecosis of the olecranon bursa caused by achloric algae. American Journal of Clinical Pathology. 1973;59:567–573. doi: 10.1093/ajcp/59.4.567. [DOI] [PubMed] [Google Scholar]
- 14.de Montclos M., Chatte G., Perrin-Fayolle M., Flandrois J. Olecranon bursitis due to Prototheca wickerhamii, an algal opportunistic pathogen. European Journal of Clinical Microbiology & Infectious Diseases. 1995;14:561–562. doi: 10.1007/BF02113444. [DOI] [PubMed] [Google Scholar]
- 15.Cox G.E., Wilson J.D., Brown P. Protothecosis: a case of disseminated algal infection. Lancet. 1974;2(7877):379–382. doi: 10.1016/s0140-6736(74)91760-7. [DOI] [PubMed] [Google Scholar]
- 16.Nwanguma V., Cleveland K., Baselski V. Fatal Prototheca wickerhamii bloodstream infection in a cardiac allograft recipient. Journal of Clinical Microbiology. 2011;49(11):4024. doi: 10.1128/JCM.05305-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McMullan B., Muthiah K., Stark D., Lee L., Marriott D. Prototheca wickerhamii mimicking yeast: a cautionary tale. Journal of Clinical Microbiology. 2011;49(8):3078–3081. doi: 10.1128/JCM.00487-11. [Epub 2011 Jun 8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohd R., Sabaratnam P., Salleh M.A., Abd Razak M.F., Ahmad N. Characterization of Prototheca wickerhamii isolated from disseminated algaemia of kidney transplant patient from Malaysia. Mycopathologia. 2012;173(2–3):173–178. doi: 10.1007/s11046-011-9469-8. [Epub 2011 Sep 24] [DOI] [PubMed] [Google Scholar]
- 19.Narita M., Muder R.R., Cacciarelli T.V., Singh N. Protothecosis after liver transplantation. Liver Transplantation. 2008;14(8):1211–1215. doi: 10.1002/lt.21565. [DOI] [PubMed] [Google Scholar]
- 20.Kwok N., Schwartz S.N. Prototheca sepsis in a lung transplant patient. Clinical Microbiology Newsletter. 1996;18:183–184. [Google Scholar]
- 21.Khoury J.A., Dubberke E.R., Devine S.M. Fatal case of protothecosis in a hematopoietic stem cell transplant recipient after infliximab treatment for graft-versus-host disease. Blood. 2004;104:3414–3415. doi: 10.1182/blood-2004-07-2720. [DOI] [PubMed] [Google Scholar]
- 22.Lanotte P., Baty G., Senecal D., Dartigeas C., Bailly E., Duong T.H. Fatal algaemia in patient with chronic lymphocytic leukemia. Emerging Infectious Diseases. 2009;15(7):1129–1130. doi: 10.3201/eid1507.090373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hariprasad S.M., Prasad A., Smith M., Shah G.K., Grand M.G., Shepherd J.B. Bilateral choroiditis from Prototheca wickerhamii algaemia. Archives of Ophthalmology. 2005;123(8):1138–1141. doi: 10.1001/archopht.123.8.1138. [DOI] [PubMed] [Google Scholar]
- 24.Lass-Flörl C., Fille M., Gunsilius E., Gastl G., Nachbaur D. Disseminated infection with Prototheca zopfii after unrelated stem cell transplantation for leukemia. Journal of Clinical Microbiology. 2004;42:4907–4908. doi: 10.1128/JCM.42.10.4907-4908.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kunovà A., Kollàr T., Spànik S., Krcméry V. First report of Prototheca wickerhamii algaemia in an adult leukemic patient. Journal of Chemotherapy. 1996;8:166–167. doi: 10.1179/joc.1996.8.2.166. [DOI] [PubMed] [Google Scholar]
- 26.Gaur S., Marrin C., Barnes R.A. Disseminated protothecosis following traumatic Hickman line removal in a patient with leukemia. Medical Mycology. 2010;48(2):410–412. doi: 10.1080/13693780903188698. [DOI] [PubMed] [Google Scholar]
- 27.Heney C., Greef M., Davis V. Hickman catheter-related protothecal algaemia in an immunocompromised child. Journal of Infectious Diseases. 1991;163:930–931. doi: 10.1093/infdis/163.4.930. [DOI] [PubMed] [Google Scholar]
- 28.Mohabeer A.J., Kaplan P.J., Southern P.M., Gander R.M. Algaemia due to Prototheca wickerhamii in a patient with myasthenia gravis. Journal of Clinical Microbiology. 1997;35:3305–3307. doi: 10.1128/jcm.35.12.3305-3307.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marr K.A., Hirschmann J.V., Thorning D., Raugi G.J. Photo quiz. Protothecosis. Clinical Infectious Diseases. 1998;26(3):756–757. doi: 10.1086/514564. [575] [DOI] [PubMed] [Google Scholar]
- 30.Chan J., Jeffers L., Gould E., Hutson D., Martinez O., Reddy K. Visceral protothecosis mimicking sclerosing cholangitis in an immunocompetent host: successful antifungal therapy. Review of Infectious Disease. 1990;12:802–807. doi: 10.1093/clinids/12.5.802. [DOI] [PubMed] [Google Scholar]
- 31.Pascual J., Balos L., Baer A. Disseminated Prototheca wickerhamii infection with arthritis and tenosynovitis. Journal of Rheumatology. 2004;31:1861–1865. [PubMed] [Google Scholar]
- 32.Joubert M.F., Ferguson T.G., Pankey G.A. Prototheca wickerhamii algaemia. Infectious Diseases in Clinical Practice. 1993;2:428–430. [Google Scholar]
- 33.Modly C., Burnett J. Cutaneous algal infections: protothecosis and chlorellosis. Cutis. 1989;44:23–24. [PubMed] [Google Scholar]
- 34.Shahan T., Pore S. In vitro susceptibility of Prototheca spp. to gentamicin. Antimicrobial Agents and Chemotherapy. 1991;35:2434–2435. doi: 10.1128/aac.35.11.2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sheikh-Ahmad M., Goldstein S., Potasman I. Prototheca wickerhamii hand infection successfully treated by itraconazole and voriconazole. Journal of Travel Medicine. 2006;13:321–323. doi: 10.1111/j.1708-8305.2006.00062.x. [DOI] [PubMed] [Google Scholar]
- 36.Sud I., Feingold D. Lipid composition and sensitivity of Prototheca wickerhamii to membrane-active antimicrobial agents. Antimicrobial Agents and Chemotherapy. 1979;16:486–490. doi: 10.1128/aac.16.4.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tortorano A.M., Prigitano A., Dho G., Piccinini R., Daprà V., Viviani M.A. In vitro activity of conventional antifungal drugs and natural essences against the yeast-like alga Prototheca. Journal of Antimicrobial Chemotherapy. 2008;61(6):1312–1314. doi: 10.1093/jac/dkn107. [DOI] [PubMed] [Google Scholar]
- 38.Lee W., Lagios M., Leonards R. Wound infection by Prototheca wickerhamii, a saprophytic alga pathogenic for man. Journal of Clinical Microbiology. 1975;2:62–66. doi: 10.1128/jcm.2.1.62-66.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sands M., Poppel D., Brown R. Peritonitis due to Prototheca wickerhamii in a patient undergoing chronic ambulatory peritoneal dialysis. Review of Infectious Disease. 1991;13:376–378. doi: 10.1093/clinids/13.3.376. [DOI] [PubMed] [Google Scholar]


