Abstract
Purpose
To report the anatomic and visual results following macular buckling for patients with macular retinoschisis related to high myopia.
Methods
Thirty-nine highly myopic eyes (mean refractive error −16.7 D; range, −9 to −24 D) of 36 patients (mean age 59 years; range, 35–79 years) presenting with macular retinoschisis associated with a posterior staphyloma, who underwent combined vitrectomy and macular buckling were evaluated. Main outcome measures included best-corrected visual acuity (BCVA) and optical coherence tomography (OCT) findings. Three cases were excluded due to short follow-up (less than 3 months). The mean follow-up was 16 months.
Results
The mean BCVA increased from 0.76 to 0.43 LogMAR (p = 0.001). Visual acuity improved in 30 eyes (83.3%), remained stable in three eyes (8.3%) and decreased in three eyes (8.3%). OCT showed resolution of foveoschisis with foveal reattachment in all eyes. None of the evaluated patients developed a macular hole during follow-up.
Conclusion
Macular buckling associated with vitrectomy results in good anatomic and visual outcomes in patients with myopic foveoschisis.
Keywords: High myopia, Posterior staphyloma, Retinoschisis, Myopic foveoschisis, Macular detachment, Lamellar macular hole, Optical coherence tomography, Macular buckling, Pars plana vitrectomy
Introduction
High myopia is defined as a refractive error equal to or higher than −6 D or an axial length greater than 26 mm.1 The prevalence of high myopia is variable, showing some ethnic variability. The estimated prevalence in the USA is approximately 2% of the population, whereas it is 10% in countries such as China or Japan.1 This may be due to genetic and external factors that remain unknown. In addition, the posterior staphyloma that develops as a result of the progressive elongation of the eye affects all layers: sclera, choroid, retina and vitreous.2
Myopic macular retinoschisis (also called myopic foveoschisis) is one of the macular complications that may develop in highly myopic eyes. It is characterized by a splitting of the layers of the neurosensory retina. The pathogenesis of myopic foveoschisis remains debatable. The most common pathogenesis model is that it is caused by antero-posterior traction due to a staphyloma and tangential traction caused by stretched retinal vessels and an abnormally rigid inner limiting membrane.1
Myopic foveoschisis is difficult to assess by fundus biomicroscopy due to the scarcely pigmented fundus of myopic eyes.3,4 However, optical coherence tomography (OCT) allows detailed imaging of myopic foveoschisis to an almost histological resolution, which has led to a better understanding and characterization of this pathology.3,5,6 The prevalence of foveoschisis in highly myopic eyes with posterior staphyloma ranges from 9% to 34% depending on the series.2,7–9
OCT is useful for diagnosis, follow-up and evaluation of surgical outcomes.10 OCT can also be used to detect possible complications such as foveal detachment, lamellar macular hole or full-thickness macular hole and retinal detachment secondary to macular hole.3,6 These findings have suggested that myopic foveoschisis is a predisposing factor for retinal detachment secondary to macular hole in myopic eyes.11 Loss of visual acuity or progressive metamorphopsia detected by the patient12 can be correlated to changes in the tomographic images, such as progression of foveoschisis, foveal detachment or development of a macular hole, not visible by biomicroscopy.
Surgical management of myopic foveoschisis is still a controversial issue. Pars plana vitrectomy, encircling scleral buckle, episcleral macular buckling or a combination of procedures has been reported in the literature.
In the present study, we evaluate the functional and anatomic outcomes of macular buckling with vitrectomy for the treatment of myopic foveoschisis.
Methods
This study is a retrospective analysis of all cases of myopic foveoschisis treated with the macular buckling technique (either hard silicone implant or Ando plombe) at our institution. Surgeries were performed by the same surgeon (CM) between July 2004 and October 2012. Informed consent was obtained from all patients prior to surgery. The Institutional Review Board of our institution approved this study. The study and data collection were performed in conformity with Spanish and European laws and adhered to the tenets of the Declaration of Helsinki.
Inclusion criteria for this study were, high myopia defined as a refractive error of −6 D or higher or an axial length greater than 26 mm, myopic foveoschisis, with or without associated foveal detachment and with or without inner macular hole (full-thickness macular holes were excluded), progressive visual loss (or loss of reading ability) or progressive metamorphopsia due to foveoschisis (once other possible causes had been excluded) and minimum postoperative follow up of 3 months.
Data collection, follow-up and outcome measures
Data were obtained by chart review of all patients presenting with myopic foveoschisis who underwent macular buckling surgery. Data were collected on, demographic characteristics, best-corrected visual acuity (BCVA), reading ability (the reference was Arial point-12 text), preoperative and postoperative axial length, anterior segment biomicroscopy, dilated fundus examination, intraocular pressure measurement, color retinography, optical coherence tomography (OCT) and postoperative complications.
Patients were divided into four groups based on preoperative OCT findings as follows: isolated foveoschisis; foveoschisis with associated foveal detachment; foveoschisis and inner lamellar macular hole; mixed cases, combining any of the above.
Surgical techniques
All cases underwent combined vitrectomy and macular buckling. The macular buckling technique was performed using a hard silicone implant (6 mm wide) in the first six cases. Since this technique is complex and time-consuming, we chose to switch to a less complex technique, using an Ando plombe instead of a hard silicone band to achieve the buckling effect. Both techniques have been previously described elsewhere.13 During surgery, pars plana lensectomy was performed in 23 of the 25 phakic eyes, in order to improve visualization during vitrectomy. These 23 eyes were left aphakic due to low vision in the fellow eye. The two remaining phakic eyes were left phakic to avoid postoperative anisometropia.
Statistical analysis
Best corrected visual acuity (BCVA) in LogMAR (logarithm of the minimum angle of resolution) notation and the spherical equivalent were the main data used for the statistical analysis. Three cases were excluded from statistical analysis due to follow-up less than 3 months.
Data were compared with the paired t-test. These analyses were performed with SPSS for Windows version 17.0 (IBM Corp., Armonk, NY, USA). A p value less than 0.05 was considered statistically significant.
Results
Patient demographics and clinical data
Thirty-nine eyes of 36 patients were included (29 females and 7 males) with a mean refractive error of −16.7 D (range, −9 to −29 D) and a mean axial length of 30.77 mm (range, 26.3–34.5 mm). Patient demographics and clinical data are presented in Table 1. Mean age of the patients was 59 years (range, 35–79 years). The minimum follow-up required for this study was 3 months, with a mean follow-up of 16 months (range, 3–42 months). Three patients underwent bilateral surgery.
Table 1.
Preoperative and postoperative details of patients undergoing macular buckling.
| Case | Age | Sex | Eye | Preoperative OCT findings | Type of macular buckling | BCVA initial (logMAR) | BCVA final (logMAR) | Reading ability | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 58 | F | OS | FD | Sil. band | 1.3 | 0.5 | Yes | 18 |
| 2 | 56 | M | OD | LMH | Sil. band | 1 | 0.5 | No | 36 |
| 3 | 56 | F | OD | FD | Sil. band | 1.1 | 1.3 | No | 24 |
| 4 | 59 | F | OS | FD | Sil. band | 0.7 | 0.2 | Yes | 42 |
| 5 | 64 | F | OS | FD + LMH | Sil. band | 0.7 | 0.2 | Yes | 13 |
| 6 | 42 | F | OD | FD + LMH | Sil. band | 1 | 0.5 | Yes | 6 |
| 7 | 56 | F | OD | FD | Plombe | 1 | 0.2 | Yes | 36 |
| 8 | 62 | F | OD | FD | Plombe | 0.5 | 0 | Yes | 17 |
| 9 | 63 | M | OD | FD | Plombe | 0.7 | 0.2 | Yes | 29 |
| 10 | 63 | F | OS | FD | Plombe | 0.5 | 0.2 | Yes | 27 |
| 11 | 67 | F | OD | FD | Plombe | 0.5 | 0.7 | No | 29 |
| 12 | 72 | F | OS | FD | Plombe | 0.8 | 0.6 | No | 30 |
| 13 | 54 | M | OS | LMH | Plombe | 0.7 | 0.4 | Yes | 8 |
| 14 | 47 | F | OD | LMH | Plombe | 0.8 | 0.2 | Yes | 27 |
| 15 | 79 | M | OS | FD | Plombe | 0.8 | 0.6 | No | 10 |
| 16 | 52 | F | OS | FD | Plombe | 0.7 | 0.4 | Yes | 21 |
| 17 | 62 | F | OD | FD | Plombe | 0.7 | 0.5 | Yes | 20 |
| 18 | 63 | F | OS | FD + LMH | Plombe | 0.5 | 0.2 | Yes | 14 |
| 19 | 45 | M | OS | FD | Plombe | 0.3 | 0.2 | Yes | 3 |
| 20 | 63 | F | OD | MS | Plombe | 0.5 | 0.3 | Yes | 24 |
| 21 | 53 | F | OD | FD | Plombe | 1.3 | 0.3 | Yes | 12 |
| 22 | 61 | F | OS | FD | Plombe | 1.3 | 0.5 | Yes | 12 |
| 23 | 64 | M | OS | FD | Plombe | 0.5 | 0.5 | No | 8 |
| 24 | 47 | F | OS | FD | Plombe | 0.3 | 0.2 | Yes | 14 |
| 25 | 64 | F | OD | FD | Plombe | 1 | 1 | No | 17 |
| 26 | 60 | F | OS | LMH | Plombe | 0.5 | 0.2 | Yes | 16 |
| 27 | 65 | F | OD | FD | Plombe | 0.5 | 0.3 | Yes | 11 |
| 28 | 74 | F | OD | FD | Plombe | 0.4 | 0.2 | Yes | 11 |
| 29 | 70 | F | OD | FD | Plombe | 0.4 | 0.5 | No | 12 |
| 30 | 60 | F | OD | LMH | Plombe | 0.8 | 0.3 | Yes | 12 |
| 31 | 52 | F | OS | FD+LMH | Plombe | 0.5 | 0.4 | Yes | 8 |
| 32 | 64 | F | OD | FD | Plombe | 1.3 | 1.3 | No | 8 |
| 33 | 48 | F | OS | MS | Plombe | 1 | 0.7 | No | 4 |
| 34 | 45 | F | OD | MS | Plombe | 0.8 | 0.5 | Yes | 4 |
| 35 | 72 | F | OD | FD | Plombe | 1.3 | 1 | No | 4 |
| 36 | 35 | M | OD | FD | Plombe | 0.7 | 0.2 | Yes | 3 |
Abbreviations: BCVA, best corrected visual acuity; OCT, optical coherence tomography; F, female; M, male; OD, right eye; OS, left eye; FD, foveal detachment; LMH, lamellar macular hole; MS, macular schisis; Sil.band, silicone band.
Functional results
Functional results are presented in Figure 1. Mean preoperative and postoperative BCVA are presented in Table 1. Mean preoperative visual acuity was 0.76 ± 0.3 LogMAR (range, 0.3–1.3 LogMAR) and mean postoperative BCVA was 0.44 ± 0.3 LogMAR (range, 0 to 1.3 LogMAR). Compared to preoperative BCVA, the final BCVA improved significantly (p = 0.001). Preoperative and postoperative BCVA according to initial OCT findings are presented in Figure 2.
Figure 1.
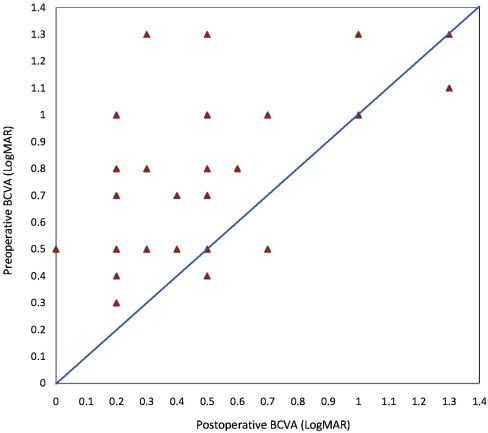
Comparison of preoperative best corrected visual acuity (BCVA) and postoperative BCVA in logarithm of the minimal angle of resolution (LogMAR) units for 36 eyes. The improvement in BCVA was statistically significant (p < 0.05; paired t-test).
Figure 2.
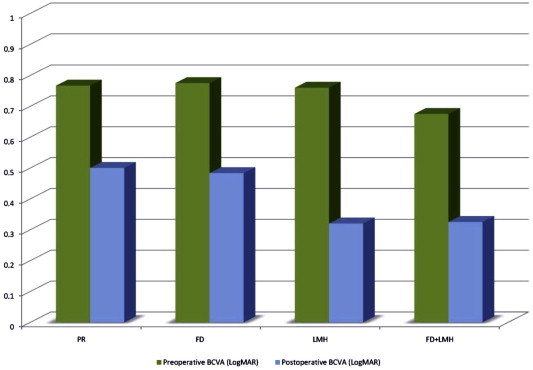
Comparison between mean pre- and postoperative best-corrected visual acuity (LogMAR) in relation to preoperative OCT findings (MS, macular schisis; FD, foveal detachment; LMH, lamellar macular hole).
Thirty of 36 (83.3%) eyes treated, had visual improvement with a mean improvement of 0.32 ± 0.3 LogMAR. Twenty-five of 36 (69.4%) eyes achieved reading ability postoperatively. Three (8.3%) of 36 eyes, all treated with Ando plombe, showed stabilization of BCVA at the end of follow-up (patients 23, 25 and 32). Patient 25 had an amblyopic eye. Three patients (8.3%) showed a decrease in visual acuity postoperatively (patients 3, 11 and 29). The first two patients developed macular retinal pigment epithelium (RPE) disturbances while the third patient developed subfoveal choroidal neovascularization that required treatment with intravitreal anti-VEGF therapy.
Anatomic outcomes
The outcomes of the macular buckling technique for the correction of myopic macular schisis are presented as pairs of matched OCT images in Figure 3. The first six patients were treated with the silicone implant while the rest were treated with the Ando plombe. All patients presented with variable degrees of preoperative foveoschisis: isolated (3 cases; 7.7%), with associated foveal detachment (26 cases; 66.7%), associated with a macular inner lamellar hole (6 cases; 15.4%) or both (4 cases; 10.2%). Postoperative OCT shows the macular indentation as an elevation of the macular region with a reduction of retinal thickness and foveal reattachment. At the end of follow-up, no recurrence of foveoschisis was evident on OCT.
Figure 3.
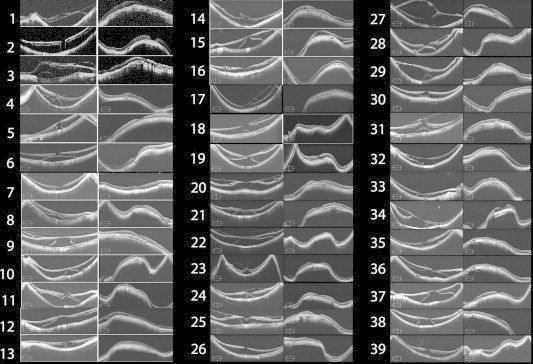
Preoperative and postoperative OCT scans.
Postoperative complications
The most frequent postoperative complications were RPE disturbances around the indented area (2 cases with hard silicone implant and 4 cases with the Ando plombe). In three cases, the buckle had to be removed, two cases due to extrusion after suture failure (one silicone implant and one Ando plombe) and one case due to secondary esotropia (silicone implant). Three cases with persistent subretinal fluid showed improvement in visual acuity at the end of follow-up. Two patients required a second surgery due to retinal detachment, one case due to a peripheral break and another case due to a posterior paravascular break. No cases in the study population developed a macular hole. During follow-up, one patient developed subfoveal choroidal neovascularization that required intravitreal anti-VEGF therapy and thus, postoperative BCVA was worse than preoperative. In one case an extrafoveal subretinal haemorrhage related to the posterior scleral suture was present though without clinical significance.
Discussion
Retinal complications related to high myopia, such as foveoschisis, are associated to several factors, of which the axial length plays a major role.14 OCT is a fundamental tool for the diagnosis and monitoring of foveoschisis3 because of its high-resolution cross-sectional imaging technique.10 Myopic foveoschisis may remain stable and asymptomatic for years. We recommend surgery when there is a proven visual loss or the patient loses reading ability.
Many surgical options for the treatment of foveoschisis have been reported throughout the years and its pathogenesis still inspires debate. Several studies have proven the benefits of vitrectomy for the resolution of foveoschisis by removing vitreoretinal traction.15–17 Benhamou et al.6 performed vitrectomy in eyes with foveoschisis and vitreoretinal traction without achieving visual gain or retinal thickness decrease, which leads us to think that other factors may also play an important role.
Zhu et al.4 used posterior scleral reinforcement in order to reduce macular retinoschisis in highly myopic patients. They achieved a visual improvement of 0.1 or more in 18 cases (75% of the patients) and complete resolution of foveoschisis in 83.33% of the cases. However, both recurrence of foveoschisis and full-thickness macular hole development were reported during the follow-up.
The combination of vitrectomy and macular buckling appears to be a safe and effective option for the treatment of myopic foveoschisis, since it addresses both internal vitreoretinal traction and the stretching effect exerted by the posterior staphyloma.
According to Gaucher,11 the natural course of myopic foveoschisis is progression towards a full-thickness macular hole (MH) and a secondary retinal detachment. Macular buckling techniques have the potential benefit of reducing the risk of MH development. In our case series, there was visual improvement in 80% of the patients and almost 70% of the patients recovered reading ability that was lost prior to the surgery. Despite the complexity of surgery, we had no intraoperative complications.
In conclusion, combining macular buckling vitrectomy is a safe and effective approach in the treatment of myopic foveoschisis, with both visual and anatomic improvement.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Ward B. Degenerative myopia: myopic macular schisis and the posterior pole buckle. Retina. 2013;3(1):224–231. doi: 10.1097/IAE.0b013e31826d3a93. [DOI] [PubMed] [Google Scholar]
- 2.Gass J.D.M. Myopic choroidal degeneration. In: Gass J.D.M., editor. Stereoscopic Atlas of Macular Diseases Diagnosis and Treatment. 4th ed. Mosby; St Louis: 1997. pp. 126–129. [Google Scholar]
- 3.Ip M., Garza-Karren C., Duker J.S. Differentiation of degenerative retinoschisis from retinal detachment using optical coherence tomography. Ophthalmology. 1999;106:600–605. doi: 10.1016/S0161-6420(99)90123-9. [DOI] [PubMed] [Google Scholar]
- 4.Zhu Z., Xueying J., Zhang J., Ke G. Posterior scleral reinforcement in the treatment of macular retinoschisis in highly myopic patients. Clin Exp Ophthalmol. 2009;37:660–663. doi: 10.1111/j.1442-9071.2009.02111.x. [DOI] [PubMed] [Google Scholar]
- 5.Takano M., Kishi S. Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthamol. 1999;128:472–476. doi: 10.1016/s0002-9394(99)00186-5. [DOI] [PubMed] [Google Scholar]
- 6.Benhamou N., Massin P., Haouchine B., Erginay A., Gaudric A. Macular retinoschisis in highly myopic eyes. Am J Ophthamol. 2002;133:794–800. doi: 10.1016/s0002-9394(02)01394-6. [DOI] [PubMed] [Google Scholar]
- 7.Akiba J., Konno S., Sato E., Yoshida A. Retinal detachment and retinoschisis detected by optical coherence tomography in a myopic eye with a macular hole. Ophthalmic Surg Lasers. 2000;31:240–242. [PubMed] [Google Scholar]
- 8.Baba T., Ohno-Matsui K., Futagami S., Yoshida T. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003;135:338–342. doi: 10.1016/s0002-9394(02)01937-2. [DOI] [PubMed] [Google Scholar]
- 9.Panozzo G., Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004;122:1455–1460. doi: 10.1001/archopht.122.10.1455. [DOI] [PubMed] [Google Scholar]
- 10.Puliafito C.A., Hee M.R., Lin C.O. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995;102:217–229. doi: 10.1016/s0161-6420(95)31032-9. [DOI] [PubMed] [Google Scholar]
- 11.Gaucher D., Haouchine B., Tadayoni R. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143:455–462. doi: 10.1016/j.ajo.2006.10.053. [DOI] [PubMed] [Google Scholar]
- 12.Kanda S., Uemura A., Sakamoto Y., Kita H. Vitrectomy with internal limiting membrane peeling for macular retinoschisis and retinal detachment without macular hole in highly myopic eyes. Am J Ophthalmol. 2003;136:177–180. doi: 10.1016/s0002-9394(03)00243-5. [DOI] [PubMed] [Google Scholar]
- 13.Mateo C., Burés-Jelstrup A., Navarro R., Corcóstegui B. Macular buckling for eyes with myopic foveoschisis secondary to posterior staphyloma. Retina. 2012;32:1121–1128. doi: 10.1097/IAE.0b013e31822e5c32. [DOI] [PubMed] [Google Scholar]
- 14.Curtin B.J. Vol. 10. Harper & Row; Philadelphia, PA: 1985. The Myopias. 237–239. [Google Scholar]
- 15.Baba T., Tanaka S., Maesawa A. Scleral buckling with macular plombe for eyes with myopic macular retinoschisis and retinal detachment without macular hole. Am J Ophthamol. 2006;142:483–487. doi: 10.1016/j.ajo.2006.04.046. [DOI] [PubMed] [Google Scholar]
- 16.Fang X., Weng Y., Xu S. Optical coherence tomographic characteristics and surgical outcome of eyes with myopic foveoschisis. Eye. 2009;23:1336–1342. doi: 10.1038/eye.2008.291. [DOI] [PubMed] [Google Scholar]
- 17.Ikuno Y., Sayanagi K., Soga K. Foveal anatomical status and surgical results in vitrectomy for myopic foveoschisis. Jpn J Ophthalmol. 2008;52:269–276. doi: 10.1007/s10384-008-0544-8. [DOI] [PubMed] [Google Scholar]



