ABSTRACT
Objectives
The iliac crest is the standard site for harvesting bone; however, this procedure may require another specialist and a general anaesthetic. The proximal tibial bone harvest has gained popularity for harvesting autogenous bone. An analysis of the clinical literature regarding the various regions for harvesting bone demonstrates that the use of the proximal tibia led to shorter hospital stays, lower morbidity rates, and a shorter learning curve for the surgeon. The purpose of this study was to analyze the clinical anatomy of a proximal tibial bone harvest graft to provide the anatomical architecture supporting a safe procedure.
Materials and Methods
Dissection of 58 lower limbs from embalmed cadavers was conducted to determine the anatomy of a proximal tibial bone harvest (PTBH).
Results
Dissection revealed that the medial approach has fewer clinically relevant neurovascular structures in harms way, and a larger surface area, providing the clinician a confident surgical window to perform the procedure.
Conclusions
The anatomical basis of this study suggests that the medial proximal tibial bone harvest approach would have fewer serious structures in harm's way compared to the lateral; however, the lateral approach may be preferred for a subgroup of patients.
Keywords: bones and bone tissue, augment bone graft, tibia, bone transplantation.
INTRODUCTION
In 1682, the first documented case of bone grafting was recorded in the Anecdotal Case History of Church Literature [1]. Harvesting bone techniques and grafts are used to treat a myriad of pathologies including skeletal trauma, congenital defects, infectious diseases, and conditions associated with cancer. Harvesting techniques and grafts can also be used in reconstructive and restorative surgery, in particular in the head and neck region by Oral Maxillofacial and Plastic surgeons. Bone grafts provide a honeycombed matrix for in-growth by host bone and provide osteogenic cells and growth factors to the host. There are three classic harvesting areas conducted on bone: 1) cortical, 2) cancellous, and 3) cortical-cancellous [2-5]. Approximately 200,000 autogenous bone grafts are harvested annually within the United States [6,7]. In 1992, Catone, et al. [8] described a bone harvesting technique from the proximal tibia published in the Journal of Oral Maxillofacial Surgery. There have been modifications since the technique was described [5-14].
The "gold standard" for harvesting cancellous bone has long been the iliac crest site [15,16]. For procedures requiring a bone graft involving head and neck pathologies, multiple clinicians may be needed to coordinate bone harvesting and final graft placement [2-6].
The proximal tibial bone harvest site is becoming a popular alternative to the iliac crest harvest site [3-5,15,16]. There are two recognized approaches or techniques used at the anterior proximal tibial region: lateral and medial [5]. This study focused on comparing the clinical anatomy of the two approaches.
In other countries (United Kingdom, Germany, Sweden, etc.), the proximal tibial harvest is now being conducted in clinical trials as an outpatient procedure [15-18]. The morphology of the anterior aspect of the tibia has it positioned so that the most anterior structure is a sharp and well-defined border. There are two flat surfaces that angle posteromedially and posterolaterally, which allow access for collection of cancellous bone. These two flat surfaces have been referred to in clinical studies as the medial and lateral approaches to the anterior proximal tibial bone harvest [11,12,18-23]. There are no studies to date that compared the detailed anatomical structures encountered from the two approaches.
The purpose of this study was to analyze the clinical anatomy of a proximal tibial bone harvest graft to provide the anatomical architecture supporting a safe procedure.
MATERIAL AND METHODS
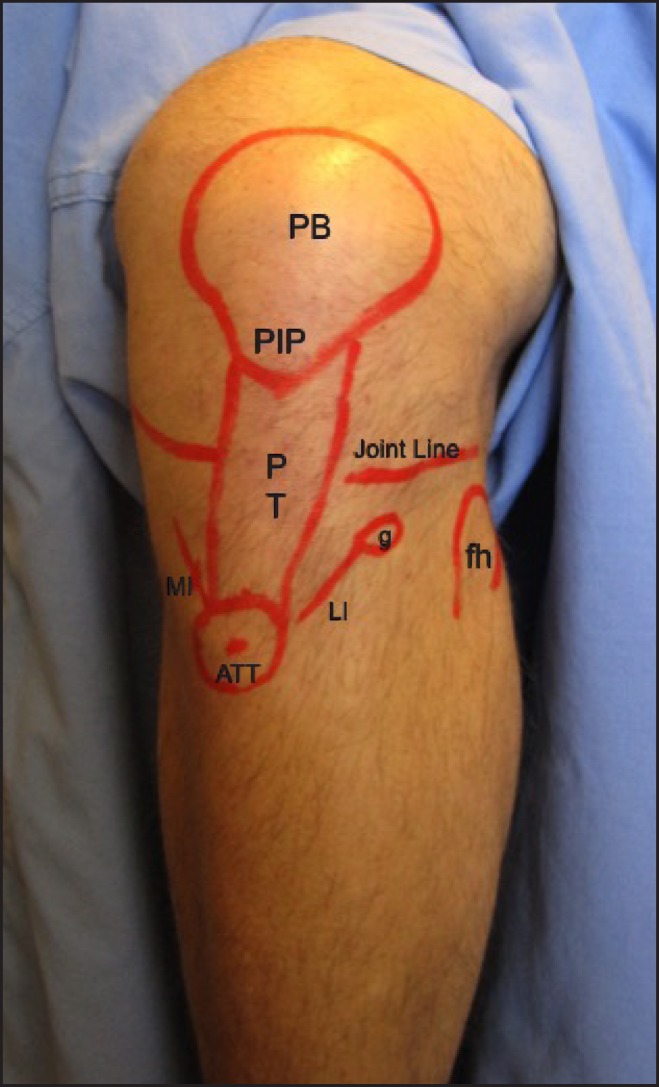
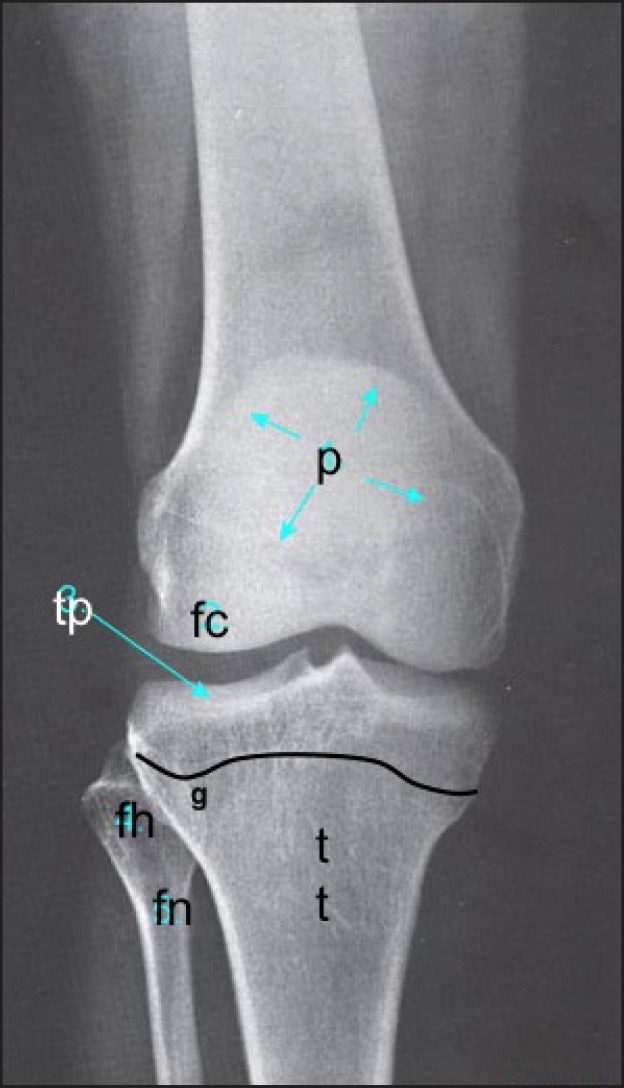
A literature search of proximal tibial bone graft/harvest techniques was conducted and the anatomy was analyzed. Fifty radiographic images (roentograms of the proximal tibia) and dry tibial bones were examined to assess the epiphyseal line. Thirty cadavers (58 sides, 30 right and 28 left, age 45 – 89, average: 76.3) were dissected to reveal the anatomy witnessed during a proximal tibial bone harvest. Exclusion criteria included below knee amputation and/or severe trauma to the proximal tibia. Both the medial and lateral approaches consisted of placing the cadaver in a supine position with the knee flexed between 30 - 45 degrees. Surface anatomy palpation was performed to identify bony landmarks, which were highlighted with a skin marker pen. Prior to incision palpated surface bony landmarks of the medial approach were as follows: patella, medial border of patella tendon, apex of a single tibial tuberosity or the distal prominence of a double apex tibial tuberosity (ATT), medial tibial condyle and medial tibiofemoral space. Using a calliper, a measurement point of 1.5 cm proximal to the ATT (p-ATT) was identified and 1.5 cm medial (m-ATT) to the p-ATT point was marked with an 'X' ('X' represents the midpoint of the 1 to 2 cm oblique incision). Prior to incision palpated surface bony landmarks of the lateral approach were as follows: patella, lateral border of patella tendon, tibial tuberosity (TT), Gerdy's tubercle (GT), fibular head, lateral condyle of tibia and lateral tibiofemoral space. Classically, the midpoint between the TT and the fibular head reveals Gerdy's tubercle. An oblique incision from GT was made towards the ATT. The medial and lateral incisions were made through connective tissue from skin down to periosteum (Figure 1 and Figure 2). Deep dissection was then conducted to identify any connective tissue layers and/or neurovascular structures (Figure 4). Trephine needle was used to penetrate the cortex and a 1cm window was created within the cortex. Spoon spatula was used to harvest cancellous bone.
Figure 1.
Surface markings of left proximal tibial region: PB = body of patella; PT = patella tendon; fh = head of fibula, PIP = inferior pole of patella; MI = medial approach incision; LI = lateral approach incision; ATT = apex of tibial tuberosity, g = gerdy's tubercle.
Figure 2.
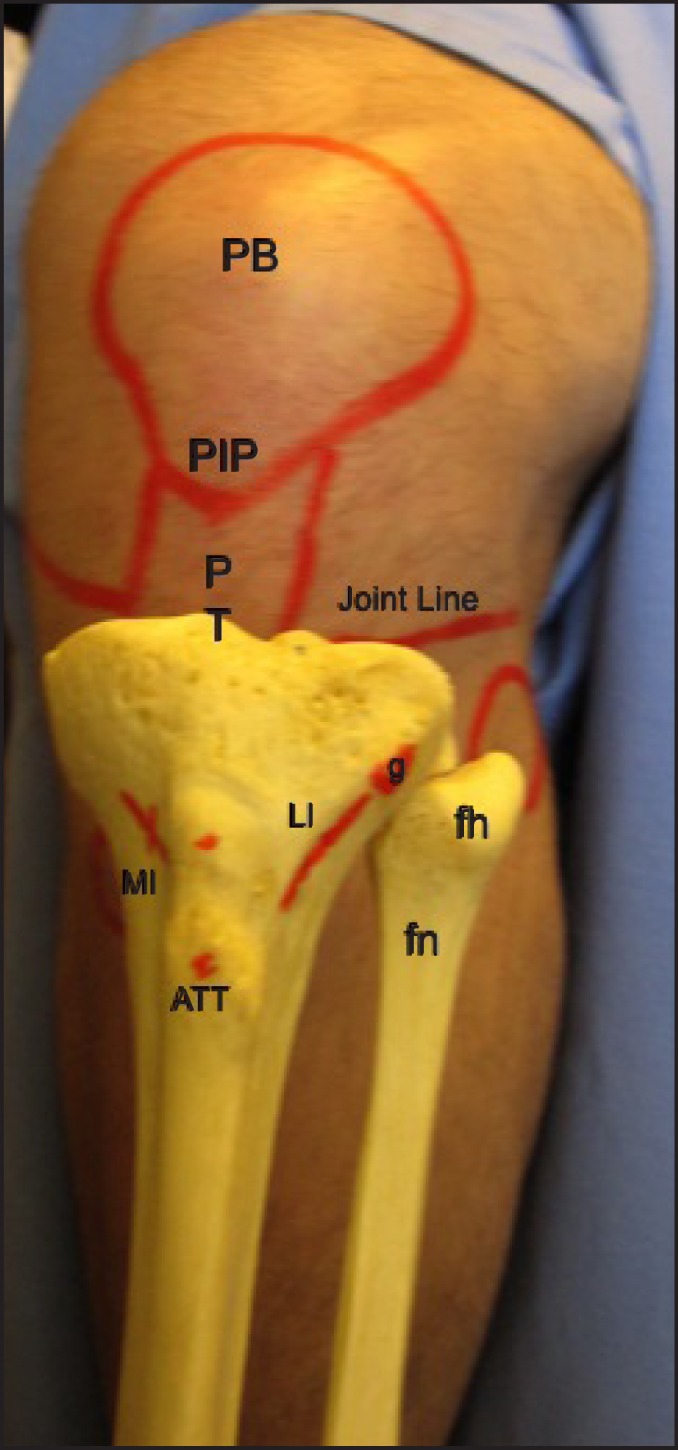
Surface and osseous proximal tibial anatomy: PB = body of patella; PT = patella tendon; PIP = inferior pole of patella; MI = medial approach incision; LI = lateral approach incision; ATT = apex of tibial tuberosity; g = gerdy's tubercle; fh = head of fibula, fn = neck of fibula.
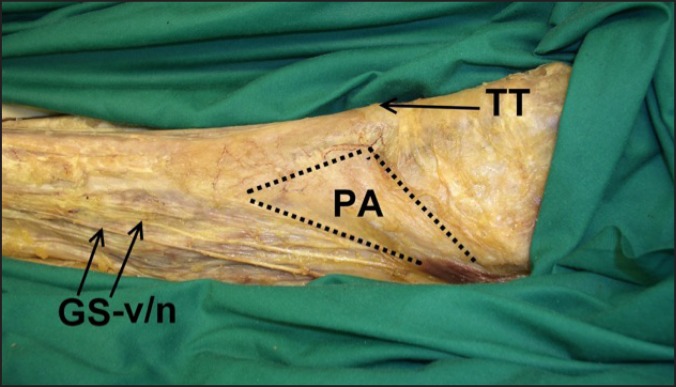
Figure 4.
Superficial dissection of the proximal tibial bone graft: medial approach. TT = tibial tuberosity; PA = pes anserinus; GS-v/n = Great saphenous vein and nerve.
RESULTS
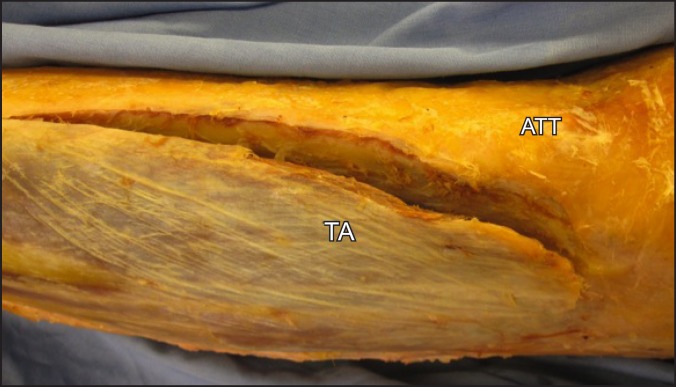
In previous studies, the primary focus was based on techniques and morbidity of the above procedures. No single study adequately integrated detailed anatomy with these techniques. Radiographic images and dry tibial bone examination revealed that the proximal tibial epiphyseal line remained within 2 cm of the medial and lateral plateaus of the tibia. Prior to dissection, all palpable landmarks were identified. The medial approach incision (tibial tuberosity 1.5 cm x 1.5 cm grid incision) successfully allowed entry through the cortex to harvest cancellous bone avoiding the epiphyseal line (Figure 3). Dissection from this incision revealed (superficial to deep connective tissue) dermis, subcutaneous tissue, pes anserinus tendon, and the medial collateral ligament (Figure 4, Figure 5 and Figure 6). Neurovascular structures encountered were the infrapatellar branch and medial crural cutaneous branch of the saphenous nerve, the saphenous nerve; the saphenous branch of the descending genicular artery and the medial inferior genicular artery; the great saphenous vein and branches from the infrapatellar region (Figure 7). The lateral approach using an oblique incision from Gerdy's tubercle to ATT (GT-ATT incision) successfully allowed entry through the cortex to harvest cancellous bone avoiding the epiphyseal line. Dissection from this incision revealed (superficial to deep) dermis, subcutaneous tissue, iliotibial tract or band (anterolateral ligament), anterior tibialis muscle, and extensor digitorum longus muscle. Neurovascular structures encountered were the lateral sural cutaneous nerve, recurrent deep peroneal nerve, common fibular nerve, superficial fibular nerve, and deep fibular nerve; anterior tibial artery and its recurrent branch; anterior tibial vein.
Figure 3.
X-ray of anterior proximal tibia and fibula landmarks prior to harvest: p = patella; fc = femoral condyle; tp = tibial plateau; curved line = epiphyseal line; g = gerdy's tubercle; tt = tibial tuberosity; fh = head of fibula; fn = neck of fibula.
Figure 5.
Superficial dissection of proximal tibial bone graft: lateral approach. TA = Tibialis anterior muscle; ATT = apex of tibial tuberosity.
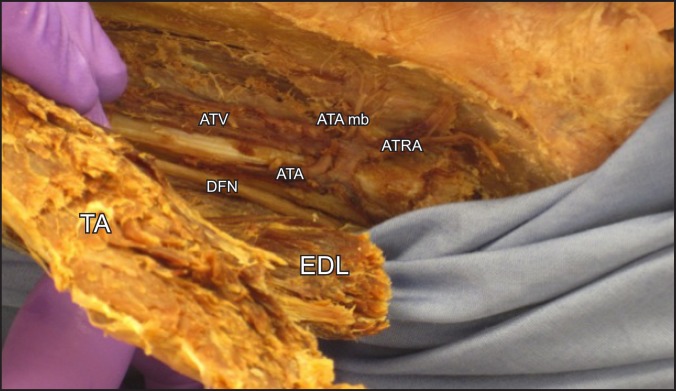
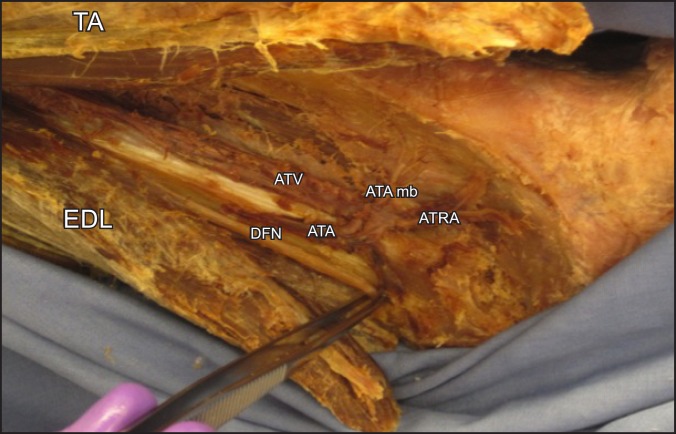
Figure 6.
Deep dissection of proximal tibial bone graft: lateral appraoch. Tibialis anterior muscle and extensor digitorum longus muscle reflected. TA = tibialis anterior muscle; EDL = extensor digitorum longus muscle; ATA = anteiror tibial arterior; ATV = anterior tibial vein; ATA mb = anterior tibial artery muscular branches; ATRA = anterior tibial recurrent artery; DFN = deep fibular nerve.
Figure 7.
Deep dissection of proximal tibial bone graft: lateral approach. Tibialis anterior muscle and extensor digitorum longus muscles reflected and separated displaying the deep fibular nerve between the forceps. TA = tibialis anterior muscle; EDL = extensor digitorum longus muscle; ATA = anteiror tibial arterior; ATV = anterior tibial vein; ATA mb = Anterior tibial artery muscular branches; ATRA = anterior tibial recurrent artery; DFN = deep fibular nerve.
DISCUSSION
Proximal tibial bone harvesting is a recognized, important surgical procedure, harvesting bone for acute and chronic pathological defects. Anatomical structures from superficial to deep of the proximal medial and lateral regions of the tibia are not described or illustrated comprehensively in contemporary anatomy texts or atlases [24-39]. Although the majority of these structures appear within texts individually, they are generally dispersed amongst multiple chapters and may have some of the smaller structures omitted completely.
Several investigations describe two techniques for harvesting cancellous bone from the proximal tibia [12,17]. In general, the proximal tibial bone harvest was considered as an acceptable alternative to the previous "gold standard" iliac crest harvest [3,16]. The proximal tibial bone harvest technique demonstrated some benefits that make it preferable to the iliac crest. Benefits include: decreased hospitalization, potentially fewer required clinicians, lower morbidity, and adequate harvest volume. As such, it could stimulate clinicians to opt for this approach, rather than the iliac crest. Nevertheless, individual investigations have focused on technique and inadequately addressed the detailed anatomy for the surgeon.
Comparing the medial to the lateral approach can aid surgeons in their choice of approach regarding structures that potentially could be compromised or for specific patient sub groups. The medial approach consistently had fewer structures demonstrated from cadaveric dissection, specifically, a small surface-supplying artery (branch of descending genicular) and cutaneous nerves (saphenous branches of the infrapatellar and medial crural) (Table 1). The lateral approach has significant arterial structures and motor nerves potentially in harm's way.
Table 1.
Anatomy of proximal tibial bone harvest. Medial vs. lateral approaches
| Medial approach | Lateral approach | |
|---|---|---|
| Nerve | Infrapatellar branch of saphenous nerve; Medial crural cutaneous branch of saphenous nerve; Saphenous nerve |
Lateral sural cutaneous nerve; Recurrent deep peroneal nerve; Common fibular nerve; Superficial fibular nerve; Deep fibular nerve |
| Artery | Saphenous branch of descending genicular artery; Medial inferior genicular artery |
Anterior tibial artery; Anterior tibial recurrent artery |
| Vein | Great saphenous vein; Great saphenous vein: branches from Infrapateller region |
Anterior tibial vein branches; Anterior tibial vein |
| Compartment | Pes anserinus complex | Tibialis anterior muscle; Extensor digitorum longus muscle; Extensor hallucis longus muscle |
Using the lateral approach, it could be postulated that the anterior tibialis (+/- extensor digitorum longus) muscle will cover the harvest site defect, which may increase healing and decrease morbidity in diabetic or compromised patients. It is a known fact that the moderate to severe diabetic patient has compromised arterial supply, therefore an approach where a highly vascular structure, such as a muscle, covering the defect, would expedite healing. Thus, it may be the approach of choice for this group of patients. Studies of the medial harvest procedure reveal that the "trap-door" from the extraction can result in an aesthetic depression-deformity and demonstrates insignificant morbidity [20]. Further, compartment syndrome would not be an issue with the medial approach whereas it could be problematic with the lateral approach. The architecture of the compartment(s) of the anterolateral aspect of the proximal leg can be compromised from the surgical insult due to increased pressure within the investing fascia. This study is not suggesting that one approach is better than the other. Rather, each approach can benefit different patient sub-groups and each have unique anatomical considerations.
CONCLUSIONS
The medial approach would have fewer serious structures in harm's way compared to the lateral approach; however, the lateral approach would have the benefit of muscle coverage and therefore healing might be expedited in particular patient sub-groups. From an anatomical point of view, this study suggests that the novice clinician might prefer the medial approach, while the more experienced clinician may choose to use the lateral approach when appropriate. However, the approach may be more specific to patient sub-groups and/or co-morbid factors. For example, the lateral approach may be more prudent for diabetic patients, whereas the medial approach may be preferable for a person whose healing is not compromised.
Acknowledgments
ACKNOWLEDGMENTS AND DISCLOSURE STATEMENTS
Internal Review Board (IRB) approval was granted for this study. There was not any external funding for this study. The authors did not have any conflict of interest with this study. Authors retain all rights to images.
REFERENCES
- 1.Susumu T, Masamichi U, Takae Y, editors Experimental and Clinical Reconstructive Microsurgery. New York: Springer; 2003. p. 44.
- 2.Ilankovan V, Stronczek M, Telfer M, Peterson LJ, Stassen LF, Ward-Booth P. A prospective study of trephined bone grafts of the tibial shaft and iliac crest. Br J Oral Maxillofac Surg. 1998 Dec;36(6):434-9. [DOI] [PubMed]
- 3.Frohberg U, Mazock JB. A review of morbidity associated with bone harvest from the proximal tibial metaphysis. Mund Kiefer Gesichtschir. 2005 Mar;9(2):63-5. [DOI] [PubMed]
- 4.Hughes CW, Revington PJ. The proximal tibia donor site in cleft alveolar bone grafting: experience of 75 consecutive cases. J Craniomaxillofac Surg. 2002 Feb;30(1):12-6; discussion 17. [DOI] [PubMed]
- 5.Besly W, Ward Booth P. Technique for harvesting tibial cancellous bone modified for use in children. Br J Oral Maxillofac Surg. 1999 Apr;37(2):129-33. [DOI] [PubMed]
- 6.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res. 1997 Jun;(339):76-81. [DOI] [PubMed]
- 7.Engelstad , Mark E , Morse, Timothy. Anterior Iliac Crest, Posterior Iliac Crest, and Proximal Tibia Donor Sites: A Comparison of Cancellous Bone Volumes in Fresh Cadavers. Journal of Oral Maxillofacial Surgery 68:3015-3021, 2010. [DOI] [PubMed]
- 8.Catone GA, Reimer BL, McNeir D, Ray R. Tibial autogenous cancellous bone as an alternative donor site in maxillofacial surgery: a preliminary report. J Oral Maxillofac Surg. 1992 Dec;50(12):1258-63. [DOI] [PubMed]
- 9.Belthur MV, Conway JD, Jindal G, Ranade A, Herzenberg JE. Bone graft harvest using a new intramedullary system. Clin Orthop Relat Res. 2008 Dec;466(12):2973-80. Epub 2008 Oct 8. [DOI] [PMC free article] [PubMed]
- 10.Herford AS, King BJ, Audia F, Becktor J. Medial approach for tibial bone graft: anatomic study and clinical technique. J Oral Maxillofac Surg. 2003 Mar;61(3):358-63. [DOI] [PubMed]
- 11.Chen YC, Chen CH, Chen PL, Huang IY, Shen YS, Chen CM. Donor site morbidity after harvesting of proximal tibia bone. Head Neck. 2006 Jun;28(6):496-500. [DOI] [PubMed]
- 12.Kirmeier R, Payer M, Lorenzoni M, Wegscheider WA, Seibert FJ, Jakse N. Harvesting of cancellous bone from the proximal tibia under local anesthesia: donor site morbidity and patient experience. J Oral Maxillofac Surg. 2007 Nov;65(11):2235-41. [DOI] [PubMed]
- 13.Lezcano FJ, Cagigal BP, Cantera JM, de la Peña Varela G, Blanco RF, Hernández AV. Technical note: medial approach for proximal tibia bone graft using a manual trephine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007 Jul;104(1):e11-7. Epub 2007 May 7. Review. [DOI] [PubMed]
- 14.Mauffrey CP, Seligson D, Krikler S. Surgical techniques: How I do it? Bone graft harvest from the proximal lateral tibia. Injury. 2010 Feb;41(2):242-4. Epub 2009 May 31. [DOI] [PubMed]
- 15.Jakse N, Seibert FJ, Lorenzoni M, Eskici A, Pertl C. A modified technique of harvesting tibial cancellous bone and its use for sinus grafting. Clin Oral Implants Res. 2001 Oct;12(5):488-94. [DOI] [PubMed]
- 16.Alt V, Nawab A, Seligson D. Bone grafting from the proximal tibia. J Trauma. 1999 Sep;47(3):555-7. [DOI] [PubMed]
- 17.Miranda SL, Fonseca APZ, Guarnieri M. Evaluation and donor site morbidity of tibial bone graft in sinus lift operation. Oral Surg. 2008 Oct;1(3): 135-39. [DOI]
- 18.Gerressen M, Prescher A, Riediger D, van der Ven D, Ghassemi A. Tibial versus iliac bone grafts: a comparative examination in 15 freshly preserved adult cadavers. Clin Oral Implants Res. 2008 Dec;19(12):1270-5. [DOI] [PubMed]
- 19.Wang K, Almeida LE, Olsson AB. Volume analysis of the proximal tibial metaphysis. J Oral Maxillofac Surg. 2007 Dec;65(12):2425-9. [DOI] [PubMed]
- 20.Kirmeier R, Payer M, Lorenzoni M, Wegscheider WA, Seibert FJ, Jakse N. Harvesting of cancellous bone from the proximal tibia under local anesthesia: donor site morbidity and patient experience. J Oral Maxillofac Surg. 2007 Nov;65(11):2235-41. [DOI] [PubMed]
- 21.Marchena JM, Block MS, Stover JD. Tibial bone harvesting under intravenous sedation: Morbidity and patient experiences. J Oral Maxillofac Surg. 2002 Oct;60(10):1151-4. [DOI] [PubMed]
- 22.van Damme PA, Merkx MA. A modification of the tibial bone-graft-harvesting technique. Int J Oral Maxillofac Surg. 1996 Oct;25(5):346-8. [DOI] [PubMed]
- 23.Misch , Jensen , Cockrell Tibial cancellious autograft for sinus grafting. The Sinus Bone Graft, Quintessence Pub. Co, 1999. p. 117-26.
- 24.Abrahams P, Boon J, Spratt J, Hutchings R. McMinn's clinical atlas of human anatomy. London: Mosby Elsevier; 2008. p. 285-336. [DOI]
- 25.Gosling JA, Humpherson JR, Willan PLT, Harris PF, Whitmore I. Lower Limb. Human anatomy: color atlas and textbook. Philadelphia: Mosby Elsevier; 2008. p. 254-314.
- 26.Moses KP, Nava P, Banks J, Petersen D. Lower Limb. In: Abrahmas P, editor. Atlas of clinical gross anatomy. Philadelphia: Mosby Elsevier; 2005. p. 486-542.
- 27.Rohen JW, Yokochi C, Lutjen-Drecoll E. Lower Limb. Color atlas of anatomy: a photographic study of the human body. Baltimore; Lippincott Williams & Wilkins; 2006. p. 417-87.
- 28.Snell RS. The Lower Limb. In: Sze G, editor. Clinical anatomy. Baltimore: Lippincott Williams & Wilkins; 2004. p. 591-718.
- 29.Woodburne RT, Burkey WE. The Lower Limb. Essentials of human anatomy. New York: Oxford University Press; 1994. p. 575-652.
- 30.Chung KW, Chung HM. Lower Limb. In: Chung HM, editor. Gross anatomy. Baltimore:, Lippincott Williams & Wilkins; 2008. p. 82-128.
- 31.Tank PW, Gest TR. The Lower Limb. Atlas of anatomy. Baltimore: Lippincott Williams & Wilkins; 2009. p. 87-145.
- 32.Gilroy AM, MacPherson BR, Ross LM. Knee & Leg. Atlas of anatomy. New York: Thieme Medical Publishers; 2008. p. 380-98.
- 33.Standring S. Pelvic Girdle and Lower Limb. In: Mahadevan V, Collins P, Healy JC, editors. Gray's anatomy: The anatomical basis of clinical practice. Spain: Elsevier; 2008. p. 1327-1465.
- 34.Ranganathan TS. Lower Limb. A textbook of human anatomy. Ram Nagar, New Delhi: S Chand & Company Ltd; 1982. p. 140-243.
- 35.Sinnatamby CS. Lower Limb. Last's anatomy: regional and applied. Philadelphia: Churchill Livingstone Elsevier; 2006. p. 115-69.
- 36.Drake RL, Vogl AW. Lower Limb. In: Ilaslan H, Richmond BJ, Polster J, editors. Gray's atlas of anatomy. Philadelphia: Churchill Livingstone Elsevier; 2008. p. 272-347.
- 37.Moore KL. Lower Limb. In: Baldridge MG, editor. Clinically oriented anatomy. Baltimore: Williams & Wilkins; 2010. p. 508-656.
- 38.Drake RL. Lower Limb. In: Adinolfi AM, editor. Gray's anatomy for students. Philadelphia:, Churchill Livingstone Elsevier; 2010. p. 468-604.
- 39.Netter FH. Lower Limb. In: Hansen JT, editor. Atlas of human anatomy. Philadelphia: Saunders Elsevier; 2011. p. 469-531.