1. Case
A 32 years old male with history of hypertension since three years, and recent ill-defined febrile illness was admitted. He has suffered of edema and fatigue. Laboratory examination revealed increased creatinine (8.6 mg/dL), proteinuria (3230 mg/day) and negative secondary work up including HIV serologic test. The patient underwent dialysis followed by renal biopsy in the clinical context of rapidly progressive renal failure.
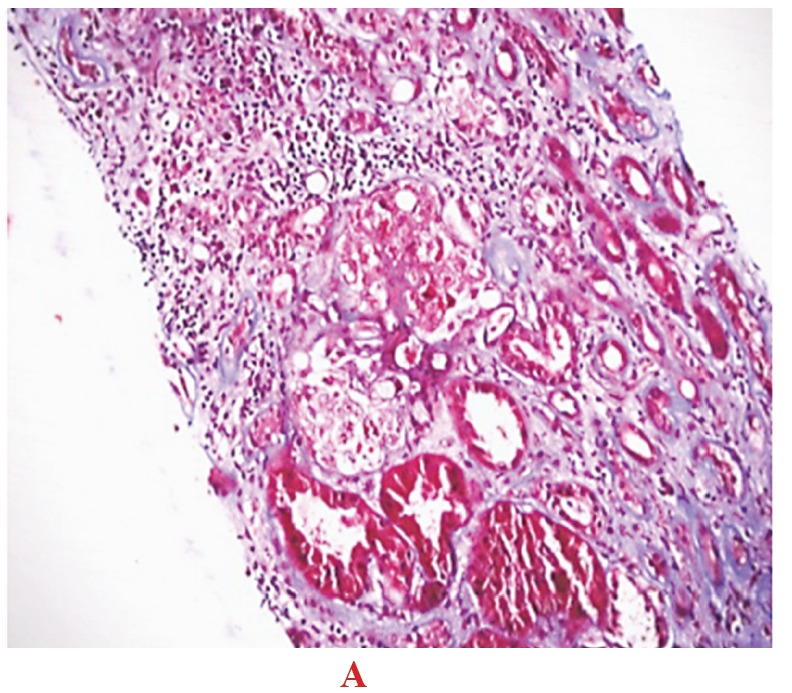
Histopathologic examination revealed positive mesangial immunoreactivity for IgM and C3 in immunoflourescence study. Light microscopic studies disclosed podocytic hypertrophy and hyperplasia that contained prominent intracytoplasmic protein resorption droplets, pseudocrescent formation, wrinkling of the glomeular basement membrane (GBM) and lobular collapse, at least in one of the glomerulus (Fig. 1;A,B,C). Out of twelve glomeruli, four were globally sclerotic. Interstitial fibrosis and cortical atrophy in about 70% of the cortical area were observed.
Fig1.A, B, C.
Focal segmental glomerulosclerosis (FSGS), collapsing variant (H&E and Jones × 200): In the collapsed tuft, the glomerular basement membranes are imploded, without appreciable increase in matrix material. The podocytes overlying the collapsed tuft are marked hyperplastic with enlarged vesicular nuclei, focal binucleated forms, and crowding of the urinary space.
A.

B.

C.

2. Discussion
The designation of collapsing variant of focal segmental glomerulosclerosis (FSGS) is applied to cases in which at least one glomerulus displays segmental or global obliteration of the glomerular capillary lumina by wrinkling and collapse of the GBMs associated with podocyte hypertrophy and hyperplasia. Collapse involving a single glomerulus is considered significant, such that the presence of any glomerular collapse pre-empts the other morphologic categories of FSGS. The term glomerular collapse was first introduced by Weiss et al., who have described an unusual clinicopathologic complex of severe nephrotic syndrome, rapidly progressive renal failure, and glomerular collapse occurring in 6 black patients. Two patients required dialysis within 10 weeks of clinical presentation and 5 had an ill defined febrile illness. Although the clinical and pathologic findings suggested possible HIV-associated nephropathy, only one of these patients subsequently developed acquired immunodeficiency syndrome. Two subsequent series have reported a similar malignant course to renal failure in patients with collapsing FSGS who lack HIV infection.
The incidence of the collapsing variant is increasing. Collapsing FSGS is comprised 11% of all primary FSGS at Columbia Presbyterian Medical Center from 1979 to 1985, 20% from 1986 to 1989, and 24% from 1990 to 1993.
3. Pathologic features
Collapsing FSGS presents a dramatic pattern of injury. Glomerular capillary lumina are occluded by an implosive wrinkling and collapse of the GBMs that is more often global than segmental, without predilection for the perihilar segments (1-5). This GBM collapse is best delineated with the use of the PAS or the Jones methenamine silver stains. The acute nature of the glomerular injury is evidenced by the lack of appreciable increase in intracapillary or mesangial matrix (3-6). The glomerular collapse must be accompanied by striking hypertrophy and hyperplasia of the overlying podocytes, which have enlarged, open vesicular nuclei with frequent nucleoli, occasional binucleated forms, and rare mitotic figures (4-8). Podocytes may be so crowded as to fill the urinary space, forming pseudocrescents, and often contain prominent intracytoplasmic protein resorption droplets (Fig. 2, A &B).
Fig 2.A, B.
FSGS, collapsing variant: Trichrome and PAS stain (× 200) delineates the collapsed blue-staining tuft and the abundant hyperplastic podocytes forming a pseudocrescent containing many intracytoplasmic fuchsinophilic protein resorption droplets. The podocyte hyperplasia lacks the spindled cellular morphology and pericellular matrix seen in true crescents of parietal cell origin.
A.
B.

Unlike FSGS (NOS), glomeruli with collapsing sclerosis usually lack of hyalinosis, endocapillary foam cells, and adhesions to Bowman’s capsule. Mesangial hypercellularity, glomerulomegaly, and arteriolar hyalinosis are un-common disease. Tubulointerstitial disease is an important component of this condition and often appears out of proportion to the degree of glomerular sclerosis (2-6). In addition to tubular atrophy, interstitial fibrosis, edema, and inflammation, there are widespread tubular degenerative and regenerative changes. These include tubular epithelial simplification with enlarged hyperchromatic nuclei, nucleoli, mitotic figures, and focal apoptosis. About 40% of cases may have tubular microcysts that contain loose proteinaceous casts.
Collapsing glomerulopathy may be confused with forms of crescentic glomerulonephritis (3-9). The proliferating podocytes in collapsing FSGS lack the spindled morphology and pericellular matrix seen surrounding the proliferating parietal cells of true crescents. Crescentic glomerulonephritis is also distinguished by the usual presence of necrotizing lesions in the underlying tuft and breaks in the GBM (8-12).
4. Clinical-pathologic correlations
Once a diagnosis of collapsing FSGS has been reached, the possibility of HIV-associated nephropathy must be ruled out. Exclusion of HIV-associated nephropathy is based on the demonstration of negative HIV serologies, and is supported by the absence of endothelial tubuloreticular inclusions. Moreover, these patients have a higher presenting serum creatinine level (3.5 versus 1.3 mg/dL and 4.2 versus 2.0 mg/dL) despite a shorter time course from clinical onset to biopsy examination. Primary FSGS with collapsing features typically has a rapid course to renal failure and is often unresponsive to steroid therapy.
Conflict of interest
The author declared no competing interests.
Funding/Support
None declared.
Acknowledgments
None declared
Implication for health policy/practice/research/medical education:
Collapsing focal segmental glomerulosclerosis presents a dramatic pattern of injury. Glomerular capillary lumina are occluded by an implosive wrinkling and collapse of the glomeular basement membranes (GBMs) that is more often global than segmental, without predilection for the perihilar segments. This GBM collapse is best delineated with the use of the PAS or the Jones methenamine silver stains.
Please cite this paper as: Mohammadi Torbati P. Focal segmental glomerulosclerosis; collapsing variant. J Nephropathology. 2012; 1(2): 87-90. DOI: 10.5812/nephropathol.7515
References
- 1.Weiss MA, Daquioag E, Margolin EG, Pollak VE. Nephrotic syndrome, progressive irreversible renal failure, and glomerular “collapse”: a new clinicopathologic entity? Am J Kidney Dis . 1986;7(1):20–8. doi: 10.1016/s0272-6386(86)80052-x. [DOI] [PubMed] [Google Scholar]
- 2.Detwiler RK, Falk RJ, Hogan SL, Jennette JC. Collapsing glomerulopathy: a clinically and pathologically distinct variant of focal segmental glomerulosclerosis. Kidney Int . 1994;45(5):1416–24. doi: 10.1038/ki.1994.185. [DOI] [PubMed] [Google Scholar]
- 3.Valeri A, Barisoni L, Appel GB, Seigle R, D’Agati V. Idiopathic collapsing focal segmental glomerulosclerosis: a clinicopathologic study. Kidney Int . 1996;50(5):1734–46. doi: 10.1038/ki.1996.493. [DOI] [PubMed] [Google Scholar]
- 4.Barisoni L, D’Agati V. The changing epidemiology of focal segmental glomerulosclerosis in New York City. Mod Pathologica . 1994;7:156A. [Google Scholar]
- 5.Barisoni L, Kriz W, Mundel P, D’Agati V. The dysregulated podocyte phenotype: a novel concept in the pathogenesis of collapsing idiopathic focal segmental glomerulosclerosis and HIV-associated nephropathy. J Am Soc Nephrol . 1999;10(1):51–61. doi: 10.1681/ASN.V10151. [DOI] [PubMed] [Google Scholar]
- 6.Shankland SJ, Eitner F, Hudkins KL, Goodpaster T, D’Agati V, Alpers CE. Differential expression of cyclin-dependent kinase inhibitors in human glomerular disease: role in podocyte proliferation and maturation. Kidney Int . 2000;58(2):674–83. doi: 10.1046/j.1523-1755.2000.00213.x. [DOI] [PubMed] [Google Scholar]
- 7.Barisoni L, Mokrzycki M, Sablay L, Nagata M, Yamase H, Mundel P. Podocyte cell cycle regulation and proliferation in collapsing glomerulopathies. Kidney Int . 2000;58(1):137–43. doi: 10.1046/j.1523-1755.2000.00149.x. [DOI] [PubMed] [Google Scholar]
- 8.Bariety J, Nochy D, Mandet C, Jacquot C, Glotz D, Meyrier A. Podocytes undergo phenotypic changes and express macrophagic-associated markers in idiopathic collapsing glomerulopathy. Kidney Int . 1998;53(4):918–25. doi: 10.1111/j.1523-1755.1998.00845.x. [DOI] [PubMed] [Google Scholar]
- 9.Bariety J, Bruneval P, Hill G, Irinopoulou T, Mandet C, Meyrier A. Posttransplantation relapse of FSGS is characterized by glomerular epithelial cell transdifferentiation. J Am Soc Nephrol . 2001;12(2):261–74. doi: 10.1681/ASN.V122261. [DOI] [PubMed] [Google Scholar]
- 10.Laurinavicius A, Hurwitz S, Rennke HG. Collapsing glomerulopathy in HIV and non-HIV patients: a clinicopathological and follow-up study. Kidney Int . 1999;56(6):2203–13. doi: 10.1046/j.1523-1755.1999.00769.x. [DOI] [PubMed] [Google Scholar]
- 11.Cameron JS, Turner DR, Ogg CS, Chantler C, Williams DG. The long-term prognosis of patients with focal segmental glomerulosclerosis. Clin Nephrol . 1978;10(6):213–8. [PubMed] [Google Scholar]
- 12.Markowitz GS, Appel GB, Fine PL, Fenves AZ, Loon NR, Jagannath S. et al. Collapsing focal segmental glomerulosclerosis following treatment with high-dose pamidronate. J Am Soc Nephrol . 2001;12(6):1164–72. doi: 10.1681/ASN.V1261164. [DOI] [PubMed] [Google Scholar]


