Abstract
Background
Various surgical techniques for thumb duplication have been described. The main goal in thumb reconstruction is to achieve optimal function, stability, and shape. Few publications have quantified the functional results of each surgical option and factors that may affect these outcomes.
Methods
We performed a retrospective review during the period from 1990 to 2011 of 115 surgery patients, 99 of whom had a mean postoperative follow-up of 44.1 months. They were classified according to the Wassel classification. We assessed the surgical technique, functional results, and complications, and evaluated the probable prognostic value of age and Wassel classification.
Results
This case series comprised mainly female patients (62 %) and the right hand (74 %), with a mean age at operation of 20 months. The most common group was Wassel type IV (54 %). On the basis of the Tada scoring system, we obtained 91 good results (91 %). Complications occurred in 27 patients (27 %), mainly instability and axis deformation. In a comparison of preoperative factors (age at the time of surgery and Wassel classification) with the final results (Tada score and complications), the association between older age at surgery and complications (p = 0.0001) and Wassel types III and IV and complications (p = 0.0210 and p = 0.0095) was statistically significant.
Conclusions
Following the basic concepts of anatomical reconstruction, we obtained good results in most patients. The main complications were instability and axial deformity. These were most common in patients who underwent operations at an age of more than 12 months, and patients with Wassel types III and IV deformities.
Keywords: Prognostic value, Polydactyly, Thumb duplication, Wassel classification, Tada score, Hand reconstructive surgery
Introduction
Thumb duplication is a preaxial polydactyly and, according to some authors, is the most frequent type of hand polydactyly in white patients [1–3], with also high incidence in America and many Asian populations [4, 5]. The classical theory for its etiology is a disruption of the ectoderm and preaxial mesodermal necrosis in the embryologic period, before the eighth week [6]. Recent studies describe the role of both the programmed cell death in the formation of normal preaxial digit formation [7] and the differentiation of the anterior/posterior axis of the limb [8]. To form along this polarity, the zone of polarizing activity (ZPA) is an area of mesenchyme that contains signals which instruct the developing limb bud. Sonic Hedgehog protein, which is expressed in the ZPA, plays a major role in determining radial-ulnar characteristics. Abnormal expression of other morphogens such as Hox genes, bone morphogenic proteins, and Gli-3 are involved in the development of thumb duplication [9].
To treat this pathology, various surgical techniques have been used. The Wassel classification not only refers to the pathoanatomy of the polydactyly, but also guides various surgical techniques [1, 6, 10]. In our view, more important than selecting one technique or another is ensuring two well-defined objectives [1, 6, 10–12]: thumb alignment and stability, which will allow for optimal functionality. Considering the social importance of the hand, the aesthetic aspect is also a very relevant factor.
The aims of the present study were as follows. First, to describe the surgical results of our patients in terms of function and complications. Second, to analyze the influence of the initial grade of the Wassel classification and of age at the time of surgery. These might be predictive factors affecting the final functionality and postoperative complications. Many publications have discussed the different surgical options, but only a few have addressed the factors that may affect the final results [1, 13, 14].
Materials and methods
This was a retrospective study based on a case series. Patients presenting duplicated thumb, affected or not from a syndrome, and having undergone surgery in our center between 1990 and 2011, were included. Only patients with floating thumbs and triphalangism, and patients with a history of previous surgery were excluded. The clinical files and imaging documentation of all patients were reviewed. After obtaining approval from our institution’s Human Studies Committee and informed consent from all patients whose images may appear in this article, we began the evaluation. All surgeries were performed by the same team. Of a total series of 115 patients, we achieved accurate follow-up of 99 patients. All these patients were followed until they were discharged, with proper radiological study, final Tada score evaluation, and registration of any complication. The mean postoperative follow-up period was 44.1 months (range 3–144 months). There were no differences in follow-up among the Wassel groups or in relation to other factors.
The Wassel classification and the clinical examination results were used to determine the operative technique [1, 6, 9, 11], always keeping in mind that the aim of surgical treatment is to achieve stability, mobility, alignment, and adequate size and shape of the thumb. If it is mandatory, we may accept a decrease in the range of motion to achieve joint stability, mainly on the interphalangeal (IP) and metacarpophalangeal (MCP) joints.
With these concepts in mind and with use of the Wassel classification, the optimal reconstruction technique of the dominant thumb may be determined. In general, hypoplastic radial thumbs are removed, and the remaining thumb is then reconstructed. In cases of types II and III thumbs with symmetrical radial and longitudinal sizes, the Bilhaut–Cloquet procedure is commonly recommended [1, 9, 12, 13]. Nevertheless, we do not usually use this technique because it is more technically demanding and offers results similar to those of radial resection with soft tissue reconstruction [11, 13]. We use the modified Bilhaut–Cloquet technique only in Wassel type IV thumbs with divergent MCP and convergent IP joints [10, 11].
Using zig-zag incisions, we perform deep dissection, inspecting every joint aspect. First, by establishing slight traction, the IP or MCP joint congruency is evaluated. Mainly in types II and IV, chondroplasty of the radial facet of the proximal phalanx and the metacarpus, respectively, is usually necessary to restore joint congruency [1]. Second, the IP and MCP joint stability is tested. In any case of radial resection, the radial collateral ligaments are reattached with preservation of the capsular-periosteal flaps. To reconstruct the MCP joint, soft tissue from the base of the proximal phalanx is sutured to the metacarpal neck. The thenar musculature (Fig. 1) and radial collateral capsular-periosteal flap is reattached at the same site. At this point of the procedure, if some joint instability remains, part of the extensor pollicis longus (EPL) or flexor pollicis longus (FPL) is used as a circumferential pulley around the proximal phalanx, suturing the tendon to itself [11]. In cases of connections between the FPL and extensors, they may be cut out [11]. Third, to ensure joint axial alignment, it is important to avoid eccentric tendon pull of the EPL by its insertion at the radial side of the base of the distal phalanx (Fig. 2). With that aim, the duplicated EPL of the radial thumb may be sutured to its corresponding remaining tendon of the ulnar thumb at the ulnar base of the distal phalanx. The eccentric position of the tendon is thus modified, and its deforming forces are subsequently neutralized. At this stage, in nearly all cases, these mentioned soft tissue procedures achieve proper alignment. If good alignment is not achieved with these methods, osteotomies become necessary. If so, ulnar–base head–neck junction osteotomy of the proximal phalanx is performed. Before performing the osteotomy, a 0.7-mm K-wire is introduced antegrade at the base of the distal phalanx until it appears at the tip of the thumb. The K-wire is then reintroduced in a retrograde manner from the tip of the thumb to the head of the proximal phalanx. The K-wire is then driven through the proximal phalanx and left in place for 5 weeks. Osteotomy of a proximal or distal delta phalanx is also necessary in some exceptional cases. Radial-side head–neck junction metacarpal osteotomy, however, has not been necessary in any case. Z-plasty of the first space is performed in exceptional cases in which first-space contracture limited thumb functionality.
Fig. 1.

Thenar musculature with radial insertion
Fig. 2.

Duplicated extensor pollicis longus tendons with a common origin for both thumbs
Variables evaluated in the present study were sex, age at the time of diagnosis, grade of duplication following the Wassel classification (Fig. 3), age at the time of surgery, association with other malformations/diseases/syndromes, history of the pathology in the family, and obstetrical complications. The postoperative functional outcome was measured by the Tada score [15], represented by a five-point scale that evaluates three basic areas: instability (>5º of angulation at IP joint or >20º at MCP joint when the thumb is subjected to maximal stress), axial deformity (>5º of ulnar angulation at IP joint or >20º of angulation at MCP joint), and range of motion (IP and MCP joints) [1]. This system rates the result as good (4 or 5 points), fair (2 or 3 points), or poor (0 or 1 point). In addition, postoperative complications were studied, including hypertrophic scar or pulp hypoplasia, width of nail, length (affected when <75 % of the length on the normal side), stiffness (loss of >25 % of the sum of the active IP and MCP joint ranges of movement with reference to the normal side), and first-space contracture (loss of >25 % of the IP angle between the first and second metacarpal bones) [1]. In cases of bilateral polydactyly (three patients affected), the less-affected thumb was considered to be the normal side for comparison. We also evaluated patients who required repeated surgery. Further surgery was elective in cases of late axial deformity or instability. These parameters were collected from the patients’ notes, as all this information had been previously collected during their follow-up in clinics.
Fig. 3.
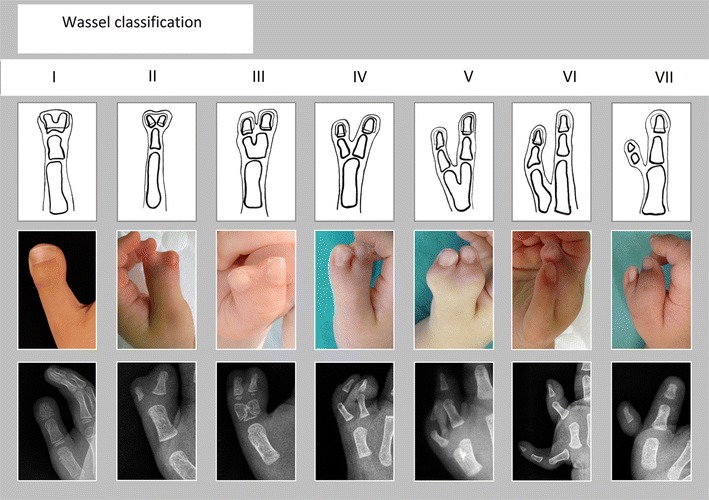
Wassel classification
Prognostic factors for the presence of complications were evaluated. The association between the initial Wassel classification and late complications was evaluated, comparing the different groups using Fisher’s test and categorizing one group against the rest. Moreover, the probable connection between age at the time of surgery and posterior complications was studied. With the help of the Mann–Whitney test, we compared the mean ages in every group, with and without complications (the results were considered statistically significant when p < 0.05).
Prognostic factors for the final functional results (Tada score) were also evaluated, as described in the next section.
Results
Of all hands operated on, 74 were right hands (74 %) and 25 were left hands (25 %). There were 62 female (62 %) and 37 male (37 %) patients. The mean age at the time of surgery was 20 months.
Seventeen patients suffered from other malformations (17 %). Among them, only one patient was affected by Treacher Collins syndrome. There was a family history of thumb duplication in 25 patients (25 %).
Some type of obstetrical history was present in 11 patients (11 %), including growing retardation (n = 1), maternal treatment with fluoxetine (n = 1), treatment with amoxicillin (n = 1), prematurity (n = 4), maternal tobacco smoking habit (n = 1), twins (n = 1), fetal anoxia (n = 1), and bleeding at the sixth month of pregnancy (n = 1).
The most frequent Wassel type was IV (n = 54, 54 %), followed by II (n = 14, 14 %) (Table 2).
Table 2.
Relationship between Wassel classification and complications
| Wassel classification | n | % | Complications | % in each group |
|---|---|---|---|---|
| I | 3 | 3 | 0 | 0 |
| II | 14 | 14 | 2 | 14 |
| III | 10 | 10 | 5 | 50 |
| IV | 54 | 54 | 19 | 35 |
| V | 2 | 2 | 0 | 0 |
| VI | 5 | 5 | 1 | 20 |
| VII | 11 | 11 | 0 | 0 |
| Total | 99 | 100 | 27 |
The most frequent type was Wassel type IV with 54 patients (54 %), followed by type II with 14 patients (14 %)
Most of the patients with complications belonged to types III (50 %) and IV (35 %). This greater average of complications was statistically significant (Chi-square test, p = 0.0210 and p = 0.0095)
Results of the surgical technique
As mentioned above, thumb reconstruction must obtain stability, mobility, alignment, and proper size and shape. The Wassel classification helps to determine the optimal surgical technique with which to achieve these aims [1, 6, 9, 11].
Radial thumb excision was performed in almost all cases, including cases of equal radial and longitudinal size. Although the Bilhaut–Cloquet procedure (combining longitudinal parts of the skeleton of each thumb) is widely recommended in cases of symmetrical size in types I, II, and III deformities [1, 6, 9, 11–13], we do not use it as a common technique. As mentioned above, we believe that it is a much more demanding surgical technique and offers final functional results similar to those of radial resection, in addition to late nail deformity if the unmodified version is used [13, 16]. The unmodified Bilhaut–Cloquet procedure was applied in only three cases of type II deformities [12]. Although the modified Bilhaut–Cloquet technique has been described as suitable in Wassel type IV thumbs with divergent MCP and convergent IP joints [10, 11], rigorous studies have not been published. For this reason and because we do not see any significant advantage, we prefer not to commonly use this technique.
To achieve joint congruency, resection of the redundant articular surface of the proximal phalanx or of the metacarpal head was performed in 52 patients (52 %): one with Wassel type I, nine with type II, four with type III, 36 with type IV, one with type V, and one with type VI. It was mainly used in type II (proximal phalanx chondroplasty, 9 patients, 16 %) and type IV (metacarpal head chondroplasty, 36 patients, 67 %) [1]. Nevertheless, it might be useful in other Wassel types when joint congruency is not achieved.
Ulnar–base head–neck junction osteotomy of the proximal phalanx was necessary to achieve axial alignment in five patients (0.05 %). In three of them (types II and IV), osteotomy was necessary to correct delta phalanx-associated deformity [17]. It was maintained with a K-wire for 5 weeks. One patient had Wassel type II, three had type IV, and one had type V deformities.
Associated Z-plasty was only necessary in two patients (type IV). A second Z-plasty was necessary in four of the seven patients affected by types V and VI deformities, in which adduction contracture is more common [13].
Complications were present in 27 patients (27 %). The most frequent complication was axial deformity (19 patients, 19 %), followed by instability (8 patients, 8 %), stiffness (6 patients, 6 %), atrophic pulp (3 patients, 3 %), hypertrophic scar (2 patients, 2 %), and first-space narrowing (1 patient, 1 %).
Repeat surgery was necessary in 12 patients (12 %). All these patients were included in the complications. Five patients (types III and IV) presented with late axial deformity, and seven patients (types III, IV, and V) presented with simultaneous clinodactyly and instability. Secondary procedures included collateral ligament reconstruction (9 patients, 75 %), tendon reattachment (4 patients, 33 %), and arthrodesis of the IP joint (12 patients, 100 %) [16]. All these patients had good final results, functionally and aesthetically, after that second surgical procedure.
Prognostic significance of Wassel classification/age at the time of surgery in the final functional results/complications
Relationship between prognostic factors and complications
Age at the time of surgery and the existence of complications seemed to show some association. The mean age in the group without complications was 17 months, while it was 29 months in the group with complications. The statistical analysis, applying an unpaired t-test, showed a significant difference (p = 0.0001). By groups, the risk of presenting complications increases proportionately from the youngest group (0–6 months) to the older groups (7–12 months, 13–18 months, 19–24 months). The statistical analysis using Fisher’s Exact Test for Count Data also shows a significant difference (p = 0.0002). Only the oldest group (>24 months) shows a slightly decreasing risk of presenting complications in the future compared to the group aged between 19 and 24 months. According to these results, the best range of age to avoid complications would be between 0 and 6 months (Table 1). Considering the most common complications, namely, deformity and instability, the only difference was in the mean age of patients who suffered from clinodactyly. In these selected patients, the mean age was 35 months with deformity and 17 months without deformity (p = 0.0035). Surgery was postponed because of the variable waiting list or due to external factors. There was no selection bias.
Table 1.
Relationship between range of age and complications
| Range of age (months) | n | % | Complications | % in each group |
|---|---|---|---|---|
| 0–6 | 11 | 11 | 0 | 0 |
| 7–12 | 42 | 42 | 8 | 19 |
| 13–18 | 17 | 17 | 6 | 35 |
| 19–24 | 6 | 6 | 5 | 83 |
| >24 | 23 | 23 | 8 | 34 |
| Total | 99 | 100 | 27 |
Most of the patients with complications belonged to the age group between 19 and 24 months. This greater average of complications was statistically significant (Fisher’s Exact Test for Count Data, p = 0.0002)
Classification and complications also had some correlation. Most patients with complications had type III (5 of 10, 50 %) and type IV deformities (19 of 54, 35 %). In these two groups (types III and IV), the average number of patients with complications was significantly greater than that in the other groups (using the Chi-square test, p = 0.0210 and p = 0.0095) (Table 2).
Relationship between prognostic factors and final functional result (Tada score)
According to the Tada score [10, 12], the results were good in 91 patients (91 %), of which 72 had 5 points and 19 had 4 points; fair in 8 patients (8 %); and poor in none. No correlation was found between different groups or age at the time of surgery or in the final outcomes. There was a very variable number of patients in each group. Moreover, there were no poor results. We can conclude that the surgical techniques used in our center offer good results in the Tada score system in almost all the patients treated (91 %) (Table 3).
Table 3.
Relationship between Wassel classification and functional results
| Wassel classification | Tada 5 | Tada 4 | Tada 3 | Tada 2 |
|---|---|---|---|---|
| I | 3 | 0 | 0 | 0 |
| II | 12 | 2 | 0 | 0 |
| III | 3 | 5 | 1 | 1 |
| IV | 38 | 11 | 5 | 0 |
| V | 1 | 1 | 0 | 0 |
| VI | 4 | 0 | 1 | 0 |
| VII | 11 | 0 | 0 | 0 |
| Total | 72 | 19 | 7 | 1 |
Results were 91 % good (4 and 5), 8 % fair (3 and 2), and none poor. Despite the good outcomes overall, there was a tendency toward more patients with 4 points in group III and more fair results in group IV
Discussion
All current publications about this pathology are retrospective [1, 7–9], as is ours. Our group comprised 99 patients, a number very similar to that in reviews by Wassel [10] and Ogino et al. [14]. With the exception of Tada [12], the remaining studies involved significantly smaller groups. Nevertheless, we must admit that as one of the limitations of our study.
The Tada score is the functional scale used in the present study. We believe that this is a very appropriate score because it takes into account the most common and limiting complications, namely, clinodactyly and stability, and because it evaluates range of motion [16]. In the literature, only Abid et al. [11] used another scale (Koichi’s scale).
To achieve good thumb function, surgery may allow for preservation of the thumb with improved development of intrinsic and extrinsic structures. Generally, excision of the radial thumb is recommended, as in our protocol [1, 9, 13, 14]. Otherwise, the Bilhaut–Cloquet technique may be put into practice in types I, II, and III deformities when the sizes of the two thumbs are similar and with restricted IP joint motion but good MCP/carpometacarpal (CMC) joint motion [1, 6, 9, 12, 13, 18, 19]. We do not use this technique because, first, the aesthetic results are only fair, and, second, it is a much more demanding technique with final functional results equivalent to those of other techniques. For type IV, subtype D defects (divergent MCP joint and convergent IP joint), a modified technique has been developed [10, 11, 20]. This technique allows for axis correction and stabilization of the IP joint while avoiding nail dystrophy because a single nail is preserved. The article by Abid refers to only four patients [11]. We expect that larger studies with more reliable results will be performed.
As the literature makes clear, when operating on these patients, it is very important to also focus on the bone–capsule–ligament reconstruction of the remaining thumb [6]. Moreover, it is important to evaluate the realignment of the extensor apparatus and the extrinsic FPL tendon. Finally, it is critical to reattach the intrinsic musculature to obtain an aligned, stable, and functional thumb [6, 12]. Proximal phalanx or metacarpal osteotomies may be necessary. From a global standpoint, our therapeutic protocol closely takes after the internationally published and accepted studies.
The results obtained from these methods have been good as measured with the Tada score [16]. These results are similar to those of other studies that used the same score. Nevertheless, it would be relevant to add an aesthetic component, which is not defined in the Tada score.
The final complication rate was 27 %, slightly lower than that in the Ogino et al.’s review (34 %) [14], and significantly less than that obtained by Yen et al. (77 %) [1]. For Yen et al. [1], the most common complication was instability (69 %). In contrast, in our study, instability was present in only 8 % of patients. Our most common postoperative problem was axial deformity, which occurred in 19 % of cases, similar to Ogino et al.’s series [14]. Comparing follow-ups, Ogino et al. [14] refer to a mean follow-up of 49 months (range 12–135 months) and Yen et al. [1] to a mean follow-up of 63.6 months (range 24–120 months). This last author presents not only a slightly longer follow-up than ours, which is 44.1 months (range 3–144 months), but also an older mean age for surgery, 33 months. Probably, one of these two factors or both of them adds up so as to significantly affect the presence of complications in Yen et al.’s review.
In terms of prognostic factors, this study contributes very interesting and statistically significant results. There are no specific recommendations in the literature regarding age at the time of the operation. In general, it is known that a floating thumb must be removed as soon as possible. When thumb duplication is more complex, it might be operated on when the anatomy is more viewable and structures can be identified. Despite this, thumb duplication must not be operated on after 3 years of age to allow the patient to develop a normal body image, and to facilitate the social integration of the patient when they start school. In our study, the risk of complications was higher when the patient was older (p = 0.0001), particularly in patients with clinodactyly (p = 0.0035). Although the mean age of our patients was 20 months, similar to that in the literature, most of our patients were operated at ages between 6 and 12 months (42 % of our patients). Most authors [13, 14, 18, 21–23] operate at around 12–18 months of age. The difference in age between our mean age (20 months) and that in other studies may be due to our long waiting list, which delays surgery. Exceptionally, only one author group, Tada et al., recommends operating at 6 months [16]. Yen et al. [1] postpone surgery and operate at a mean age of 33 months. The complications that they describe add up to 77 %. According to our results, as mentioned before, the lowest rate of complications happens in patients operated before 6 months of age (0 % complications) or between 7 and 12 months of age (19 % complications). Following these statistical results and also taking into consideration the demanding surgical technique performed before 6 months, we would recommend operating on patients between 7 and 12 months of age.
The relationship between the final functional result after treatment of this pathology and the patient’s classification is not well defined. There were good results in all groups; thus, it was not possible to establish a relationship between these two factors, and we did not clearly identify the prognostic value of the Wassel classification. Nevertheless, we observed a tendency toward more type III patients with a Tada score of 4 and more fair results in type IV patients. In these groups, complications were also more concentrated (p = 0.0210 and p = 0.0095); therefore, the functional result is probably more closely associated with the presence of complications than with the initial classification.
Most patients who had one complication showed a decrease in their Tada score of only one point (from 5 to 4). Only patients who suffered from severe deformity or instability, or both, showed a significant impact in their final functional classification (dropping two or more points).
About the limitations of this study, we would mention its retrospective nature. Data were only collected from the charts. The other limitation is the short follow-up. With a mean follow-up of 44 months, most of our patients are lost before adolescence. For this reason, we may have missed some joints problems derived from the increased demands in use in adolescence and at older ages. Future prospective studies and with longer follow-ups may be developed in order to provide more information.
Acknowledgments
We would like to thank Carlos Aláez (Department of Photography, University Children’s Hospital Sant Joan de Déu, Barcelona) for his help with the preparation of the images, and also to Jorge Briceño and Macarena Valdés (Unit of Investigation, Department of Traumatology of School of Medicine, Pontificia Universidad Católica de Chile) and to Raquel Iniesta (Research and Development Unit, Sant Joan de Déu Foundation, Universitat de Barcelona) for their help with the statistical analysis.
We have not received funding for this work from any organization.
References
- 1.Yen CH, Chan WL, Leung HB, et al. Thumb polydactyly: clinical outcome after reconstruction. J Orthop Surg (Hong Kong) 2006;14(3):295–302. doi: 10.1177/230949900601400312. [DOI] [PubMed] [Google Scholar]
- 2.Ezaki M. Radial polydactyly. Hand Clin. 1990;6(4):577–588. [PubMed] [Google Scholar]
- 3.Watson BT, Hennrikus WL. Postaxial type-B polydactyly. Prevalence and treatment. J Bone Joint Surg Am. 1997;79:65–68. doi: 10.2106/00004623-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Graham TJ, Ress AM. Finger polydactyly. Hand Clin. 1998;14:49–64. [PubMed] [Google Scholar]
- 5.Leung PC, Chan KM, Cheng JC. Congenital anomalies of the upper limb among the Chinese population in Hong Kong. J Hand Surg Am. 1982;7:563–565. doi: 10.1016/S0363-5023(82)80102-0. [DOI] [PubMed] [Google Scholar]
- 6.Song KM. Thumb duplication. In: Song KM, editor. Orthopaedic knowledge update: pediatrics 4. New York: American Academy of Orthopaedic Surgeons (AAOS); 2011. pp. 134–151. [Google Scholar]
- 7.Kimura S, Yamada S, Naruse I. Normal location of thumb/big toe may be related to programmed cell death in the preaxial area of embryonic limb. Anat Rec (Hoboken) 2011;294(8):1352–1359. doi: 10.1002/ar.21434. [DOI] [PubMed] [Google Scholar]
- 8.Scott FG. Developmental biology. 9. Sunderland: Sinauer Associates, Inc.; 2010. [Google Scholar]
- 9.Tonkin MA. Thumb duplication: concepts and techniques. Clin Orthop Surg. 2012;4:1–17. doi: 10.4055/cios.2012.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wassel HD. The results of surgery for polydactyly of the thumb. Clin Orthop Relat Res. 1969;64:175–193. [PubMed] [Google Scholar]
- 11.Abid A, Accadbled F, Knorr G, et al. Type IV-D thumb duplication: a new reconstruction method. Orthop Traumatol Surg Res. 2010;96(5):521–524. doi: 10.1016/j.otsr.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 12.Dobyns JH, Lipscomb PR, Cooney WP. Management of thumb duplication. Clin Orthop Relat Res. 1985;195:26–44. [PubMed] [Google Scholar]
- 13.Maillet M, Fron D, Martinot-Duquennoy V, et al. Results after surgical treatment of thumb duplication: a retrospective review of 33 thumbs. J Child Orthop. 2007;1:135–141. doi: 10.1007/s11832-007-0019-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ogino T, Ishii S, Takahata S, et al. Long-term results of surgical treatment of thumb polydactyly. J Hand Surg Am. 1996;21(3):478–486. doi: 10.1016/S0363-5023(96)80366-2. [DOI] [PubMed] [Google Scholar]
- 15.Goldfarb CA, Patterson JM, Maender A, et al. Thumb size and appearance following reconstruction of radial polydactyly. J Hand Surg Am. 2008;33:1348–1353. doi: 10.1016/j.jhsa.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Tada K, Yonenobu K, Tsuyuguchi Y, et al. Duplication of the thumb. A retrospective review of two hundred and thirty-seven cases. J Bone Joint Surg Am. 1983;65:584–598. [PubMed] [Google Scholar]
- 17.Ozalp T, Coşkunol E, Ozdemir O. Thumb duplication: an analysis of 72 thumbs. Acta Orthop Traumatol Turc. 2006;40(5):388–391. [PubMed] [Google Scholar]
- 18.Samson P, Salazard B, Magalon G. The “Bilhaut–Cloquet” technique for treatment of thumb duplication. Handchir Mikrochir Plast Chir. 2004;36:141–145. doi: 10.1055/s-2004-817888. [DOI] [PubMed] [Google Scholar]
- 19.Horii E, Hattori T, Koh S, et al. Reconstruction for Wassel type III radial polydactyly with two digits equal in size. J Hand Surg Am. 2009;34:1802–1807. doi: 10.1016/j.jhsa.2009.07.018. [DOI] [PubMed] [Google Scholar]
- 20.Kozin SH. Reconstruction of Wassel type IV thumb duplication. Tech Hand Up Extrem Surg. 2010;14:58–62. doi: 10.1097/BTH.0b013e3181d4ee47. [DOI] [PubMed] [Google Scholar]
- 21.Guero S, Haddad R, Glicenstein J. Surgical treatment of duplication of the thumb. Apropos of 106 cases. Ann Chir Main Memb Super. 1995;14:272–283. doi: 10.1016/S0753-9053(05)80406-5. [DOI] [PubMed] [Google Scholar]
- 22.Cohen MS. Thumb duplication. Hand Clin. 1998;14:17–27. [PubMed] [Google Scholar]
- 23.Martinot-Duquennoy V, Lahouel K, Herbaux B, et al. The treatment of duplication thumbs in children. About a series of 32 patients. Eur J Pediatr Surg. 1993;3:37–40. doi: 10.1055/s-2008-1063505. [DOI] [PubMed] [Google Scholar]


