Abstract
Background
Studies of pediatric and adolescent fractures in general report a significant increase in the incidence of upper-extremity fractures as well as in their surgical treatment. The aim of this study was to determine the trends of the incidence and treatment of distal humeral fractures in hospitalized 0- to 18-year-old patients in Finland.
Method
The study included the entire pediatric and adolescent (<19 years) population in Finland during the 24-year period from 1 January 1987 to 31 December 2010. Data on hospitalized patients were obtained from the nationwide National Hospital Discharge Registry where information is collected from all hospital categories (private, public, and other). Surgical treatment was categorized into three groups; (1) reposition with casting; (2) reposition or reduction and osteosynthesis; (3) reposition or reduction and external-fixation and other fixation methods. Patients were classified into three groups according to age: 0–6 years, 7–13 years, and 14–18 years. Annual incidences were calculated using the annual mid-year population census obtained from the Official Statistics of Finland.
Results
During the 24-year study period, there were a total of 12,590 hospitalizations with a main or secondary diagnosis of distal humeral fracture. In children aged 0–12 years the overall incidence of hospitalization increased 30 % during the 24-year study period, from 4.5 per 10,000 person-years in 1987 to 5.8 per 10,000 person-years in 2010. There were a total of 5,548 operations. During the study period, surgical treatment by repositioning or reduction with osteosynthesis due to a distal humeral fracture increased by fivefold in patients aged <6 years and by twofold in patients aged 7–12 years of age. The incidences of fracture and treatment in children older than 13 years did not change.
Conclusion
The incidence of distal humeral fractures and the incidence of repositioning with osteosynthesis increased remarkably in prepubertal children during the 24-year study period in Finland.
Keywords: Distal humeral fracture, Incidence, Pediatric, Treatment
Introduction
Distal humeral region fractures account for up to 5 % of all fractures in skeletally immature children [1–3]. Supracondylar fractures comprise up to 80 % of distal humeral region fractures [1–4], while fractures of the medial and lateral humeral condyles are much less common, representing 20 % of distal humeral fractures [1, 2]. Upper-arm fractures are often sustained during a fall as children attempt to protect themselves with an outstretched hand [1, 2]. A previous Finnish population-based study revealed a 23 % increase in the incidence of all upper-extremity fractures over the past 10 years and an increase of up to 28 % in the incidence of surgical treatment [5]. The type of upper-extremity fracture that has increased the most, however, is not known.
Unlike other anatomic areas in the growing skeleton, most distal humeral fractures are treated surgically by closed or open repositioning and osteosynthesis, usually by pinning [6–8]. Percutaneous pinning is a popular method of choice for supracondylar fractures [6–8] and has been reported to be a safe and cost-effective method that provides good functional results [7–10]. Even dislocated supracondylar fractures can be treated by repositioning and casting with an excellent functional outcome [11]. Most complex fractures require open reduction [6, 12]. An open procedure, based on a good technical understanding, has been reported to be as safe as a closed procedure [12, 13]. However, especially with an open technique, the treating physician should be aware of the potential complications, including iatrogenic neurovascular injury, elbow stiffness, malunion, and the development of cubitus varus or valgus deformity [14–16]. To reliably provide adequate functional results, it is recommended that a surgeon gain experience by operating on a minimum of 15 fractures under the supervision of an attending surgeon [17].
The aim of this study was to assess population-based changes in the incidence of hospitalization and treatment of distal humeral fractures among children aged 0–18 years in Finland between 1987 and 2010.
Materials and methods
This study covered the entire pediatric and adolescent population (aged <19 years) in Finland during a 24-year period, from 1 January 1987 to 31 December 2010. Distal humeral fracture data were obtained from the statutory, computer-based National Hospital Discharge Register of Finland (NHDR) that was founded in 1967 and collects information from all hospital categories (i.e., private, public, and others). The NHDR contains data on the age, sex, and domicile of a patient, length of hospital stay, primary and secondary diagnosis, and operations performed during the hospital stay. The validity of the NHDR is excellent with respect to both coverage and accuracy of the database [18–20].
The main outcome variable for this study was the number of patients hospitalized as inpatients with a main diagnosis of distal humeral fracture (ICD-9 codes 8124A and 8125A from 1987 to 1996; ICD-10 code S42.4 from 1997 to 2010). The procedural codes changed during the 24-year study period. The procedures carried out for patients with ICD-9 codes included in the study were reposition and cast (9,123 patients), closed or open reposition and osteosynthesis (9,128 patients), external-fixation (9,130 patients), and other distal humeral fracture operations (9,139 patients). The corresponding ICD-10 codes were NBJ41 (reposition and cast), NBJ64 (reposition or reduction and ostesynthesis), NBJ70 (external-fixation), and NBJ91 (other distal humeral fracture operation).
To analyze the incidence trends during the entire study period from 1987 to 2010, the ICD-10 procedures codes were pooled with the ICD-9 codes. Surgical treatment was categorized into three groups: Group 1, reposition with casting; Group 2, reposition or reduction with osteosynthesis; Group 3, external fixation and other fixation method. The patients were also stratified into three age groups: from 0 to 6 years, from 7 to 13 years, and from 14 to 18 years.
To calculate the incidence of distal humeral fractures leading to inpatient hospital treatment, we obtained the annual mid-year population census from the Official Statistics of Finland, an electronic national population register [21]. Statistical analysis was performed using PASW ver. 19.0 (SPSS, Chicago, IL). The incidence figures were thus the true results concerning the entire adolescent population in Finland rather than cohort-based estimates during the study period; as such 95 % confidence intervals were not calculated.
Results
A total of 12,585 hospitalizations were registered for patients aged <19 years with a main or secondary diagnosis of distal humeral fracture during the 24-year study period. Boys comprised the majority of the patients (7,487, 60 %), with girls accounting for 40 % (5,098). There were a total of 5,548 surgical procedures (44 %). The most common surgical treatment method was reposition or reduction with osteosynthesis (4,703, 85 %), followed by closed reposition with casting (619, 11 %). Other types of surgical management, such as external-fixation (38, 1 %) and others (185, 3 %) were quite rare. Most of the patients were not treated in an operating room (7,040, 56 %). The mean age of the hospitalized children was 7.8 years (boys 8.2 years; girls 7.3 years; p = 0.003). Mean hospital stay for the entire study population was 1.9 days; for patients with reposition or reduction and osteosynthesis, mean hospital stay was 1.9 days, and for those with reposition and casting it was 3.0 days.
In this patient cohort,, the overall person-based hospitalization incidence for distal humeral shaft fractures was 5.6 per 10,000 person-years. In patients of both sexes aged 13–18 years, the incidence of fractures remained low and did not change during the 24 years of the study. In patients aged 0–6 years and 7–12 years, however, the incidence of fractures increased markedly in both sexes after the early 1990s. Girls aged 0–6 years showed the highest increase in the incidence of fractures, from 2.3 per 10,000 person-years in 1987 to 6.4 per 10,000 person-years in 2010 (Fig. 1). The same trend was detected in boys aged 0–6 years—from 3.7 per 10,000 person-years in 1987 to 6.8 per 10,000 person-years in 2010 (Fig. 2).
Fig. 1.
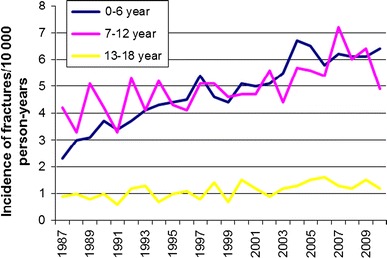
Incidence of distal humeral fractures between 1987 and 2010 among girls aged 0–18 years
Fig. 2.
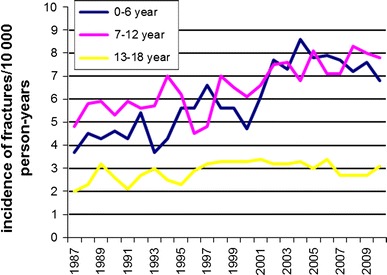
Incidence of distal humeral fractures between 1987 and 2010 among boys aged 0–18 years
The overall incidence of reposition and casting remained steady during the study period, decreasing slightly in patients aged 7–12 years (Fig. 3). The incidence of reposition or reduction and osteosynthesis increased markedly after 1996, especially in patients aged 0–6 years, from 0.6 per 10,000 person-years in 1987 to 3.0 per 10,000 person-years in 2010; in patients aged 7–12 years, this incidence increased from 1.4 per 10,000 person-years in 1987 to 3.4 per 10,000 person-years in 2010 (Fig. 4).
Fig. 3.
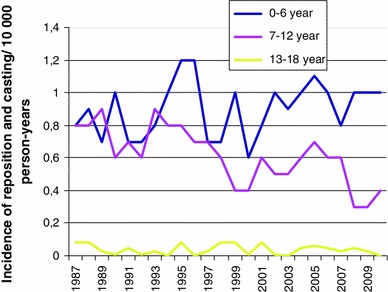
Incidence of repositioning with casting between 1987 and 2010 among girls and boys aged 0–18 years
Fig. 4.
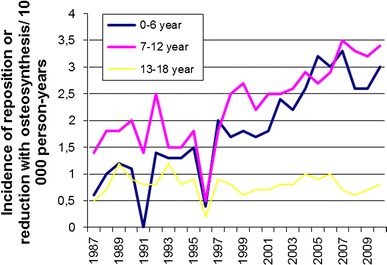
Incidence of repositioning or reduction with osteosynthesis among girls and boys aged 0–18 years between 1987 and 2010
The incidence of external-fixation was very low, with the highest incidence being 0.09 per 10,000 person-years (6 patients) in 1997 in patients aged 0–6 years. Surgical treatment with external-fixation was not related to a longer hospitalization period (mean 1.4 vs 1.9 days in all patients).
Discussion
The two principal aims of this study were to describe the incidence of distal humeral fractures leading to hospitalization and the trends in the surgical management of children and adolescents aged 0–18 years in Finland between 1987 and 2010. The main findings were that the incidence of fractures and surgical treatment increased markedly in preteen children beginning towards the end of the 1990s.
The overall incidence of pediatric fractures has increased since the 1950s, but according to Mäyränpää et al.’s population-based study the trend changed has during the last two decades [4, 22], with the incidence of all but upper-extremity fractures significantly decreasing [22]. In their Finnish population-based study on the incidence of hospital-treated upper-extremity fractures, Helenius and co-workers [5] reported a 23 % increase in fractures and 28 % increase in operative management during the past 10 years. These findings are supported by those of other studies, but there has been little focus on which type of fractures has increased. Cooper et al. [23] reported that approximately one-third of children sustain at least one fracture before 17 years of age, further suggesting that the overall increasing incidence of fractures may be due to changes in children’s activity patterns over time. In addition, new leisure-time physical activities, such as motor vehicle activities, and the popularity of trampolines and skateboards have led to an increase in the incidence of distal humeral fracture, especially supracondylar fractures [24–27]. Distal humeral fractures, especially supracondylar fractures, are usually extension fractures sustained during a fall on an outstretched hand in a child’s attempt to protect him/herself [28]. The injury mechanism is quite common and is usually related to low injury energy [28]. In children aged <3 years, the injury mechanism is often a fall from a household object, and in children aged >4 years, it is likely to be due to a fall from playground equipment, as reported by Fransworth et al. [29]. Park et al. [30] presented a playground safety score and suggested that improvements in the playground infrastructure may reduce the incidence of humerus fractures, especially supracondylar fractures. Safety precautions should be implemented in both homes and playgrounds, and the safety aspects of various sport activities should be improved.
Our analysis was based on accurate NHDR data and the annual mid-year population census in Finland. The change in the ICD-classification during the follow-up time had no impact on the collected data, and the trend of increasing incidence of fractures was linear. The collected data cover the entire Finnish population over a 24-year period, and the follow-up time was sufficiently long to estimate the trends of fracture incidence over the long term. Annual incidence rates provide precise information and can be used to detect even small changes in incidence. The findings of our study suggest that the increase in upper-extremity fractures is strongly related to increases in distal humeral fractures. The reason for the increase in these fractures, especially in younger children, may be explained by an increased activity pattern in the children’s home. In their study on preschool children, Valerio et al. [31] reported that upper extremity fractures caused by a low-energy injury most often occur at home (42 %) in this age group, followed by accidents on playgrounds and footpaths (26 %). There has been an increased participation of preschool-age children in activities associated with physical risks, such as jumping on a trampoline without a safety net and playing with motor vehicle toys, which may also contribute to the increased incidence of these types of fractures.
The incidence of repositioning and casting remained low and constant during the study period in the youngest and oldest age groups. In patients aged 7–13 years, however, the incidence of repositioning with casting decreased and at the same time the incidence of repositioning or reduction and osteosynthesis (mostly pinning) increased markedly. Based on previous studies, most distal humeral fractures are supracondylar fractures, so we assumed that changes in the incidence of fractures and treatment mostly included supracondylar fractures. Based on their evidence-based study, Mulpuri et al. [6] recommended surgical treatment for dislocated, unstable fractures (Willkins II and III). Foead et al. reported that surgical treatment with repositioning and pinning with a minimally invasive incision is a safe and effective surgical procedure, regardless of how the pinning is performed [32]. The low complication rates and several advantages, including simple operative procedures, quick recovery time, and good functional results, support surgical treatment [8–10, 12, 13, 32]. On the other hand, Spencer et al. [11] claim that some less severe, stable (Gartland type II) supracondylar fractures can be successfully treated without surgical intervention if close follow-up is possible. Based on the results of our 24-year study, it would appear that both the incidence of fractures and the incidence of surgical treatment have increased. These changes require more economical recourses in terms of planning and preparing pediatric wards and hospitals. The reason for the increased incidence of surgical treatment may be partly explained by the overall increased tendency toward operative treatment for upper extremity fractures [33]. According to Fletcher et al. [34], supracondylar fractures in patients older than 8 years of age are probably caused by higher energy injury and are more severe than those in younger age groups in which the injury energy is usually low. Supracondylar fractures with relatively poor remodeling potential require precise and stable treatment to obtain a satisfactory outcome, which may increase the willingness of the surgeon to ensure the stability of the fracture by pinning, especially in Gartland II type fractures, although such fractures could also be managed by reposition and close follow-up. The increased concern associated with these fractures may partly explain the increase in operative treatment rather than changes in hospitalization standards.
One strength of this study is the use of data from the Finnish NHDR, which provides an excellent database of patients treated in hospitals during the last 24 years. In addition, treatment is equally accessible at a comparable standard to all Finnish citizens, and thus patients can be followed in the hospital discharge register based on their personal identification number. The accuracy and coverage of the NHDR are reported to be excellent, and the validity of the data has confirmed in several studies [18–20]. The NHDR also covers private hospitals, which are very uncommon in Finland.
A limitation of this study includes the lack of separation between supracondylar, later-, and medial epicondylar fractures due to the fact that they were classified under the same ICD-10 code. This is a general limitation, however, that is commonly related to hospital discharge register data. Further, the incidence reported in our study is based on hospitalized patients. Patients treated by casting as outpatients were not included in this study. A child or adolescent often requires pain management in the hospital, however, and based on our experience approximately 56 % of these patients are hospitalized. In the Finnish healthcare system, there are no financial incentives that could drive to admission rather than outpatient treatment, and private hospitals do not treat pediatric fracture patients needing overnight care. In conclusion, financial benefit does not explain the increased interest towards operative treatment.
To summarize, the increase in the overall incidence of pediatric upper arm fractures seems to be partially accounted for by an increase in distal humeral fractures, especially in preteen children. Over the last two decades, young children have begun to participate in more risky activities, such as jumping on a trampoline and playing with motor vehicle toys. In the older age group, the severity of fractures may have also increased due to higher energy injuries caused by motor vehicles. This change in activities during a child’s everyday life and the simple fracture mechanism by falls on an outstretched hand may explain the increased incidence in0 fractures. It is unlikely that changes in hospitalization policies have caused this increase in our country. The incidence of surgical treatment by pinning also increased at the same time and may be explained by the overall increased trend toward selecting operative treatment for upper extremity fractures. Distal humeral fractures with low bone remodeling potential require precise and stable reduction, which may increase the willingness of the surgeon to ensure the stability of the fracture by pinning.
Conflict of interest
None.
References
- 1.Beekman F, Sullivan JE. Some observations on fractures of long bones in children. Am J Surg. 1941;51:722–738. doi: 10.1016/S0002-9610(41)90207-6. [DOI] [Google Scholar]
- 2.Weise K, Schwab E, Scheufele TM. Elbow injuries in childhood. Unfallchirurg. 1997;100(4):255–269. doi: 10.1007/s001130050117. [DOI] [PubMed] [Google Scholar]
- 3.Hanlon CR, Estes WL. Fractures in childhood: a statistical analysis. Am J Surg. 1954;87:312–323. doi: 10.1016/S0002-9610(54)90128-2. [DOI] [PubMed] [Google Scholar]
- 4.Hedström EM, Svensson O, Bergström U, Michno P. Epidemiology of fractures in children and adolescents. Acta Orthop. 2010;81(1):148–153. doi: 10.3109/17453671003628780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Helenius I, Lamberg TS, Kääriäinen S, Impinen A, Pakarinen M. Operative treatment of fractures in children is increasing. A population-based study from Finland. J Bone Jt Surg Am. 2009;91(11):2612–2616. doi: 10.2106/JBJS.H.01519. [DOI] [PubMed] [Google Scholar]
- 6.Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop. 2012;32(2):143–152. doi: 10.1097/BPO.0b013e318255b17b. [DOI] [PubMed] [Google Scholar]
- 7.Wilkins KE. The operative management of supracondylar fractures. Ortop Clin North Am. 1990;21:269–289. [PubMed] [Google Scholar]
- 8.Green DW, Widmann RF, Frank JS, Gardner MJ. Low incidence of ulnar nerve injury with crossed pin placement for pediatric supracondylar humerus fractures using a mini-open technique. J Ortop Trauma. 2005;19(39):158–163. doi: 10.1097/00005131-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Mazda K, Boggione C, Fitoussi F, Pennecot GF. Systematic pinning of displaced extension-type supracondylar fractures of the humerus in children: a prospective study of 116 consecutive patients. J Bone Jt Surg Br. 2001;83:888–893. doi: 10.1302/0301-620X.83B6.11544. [DOI] [PubMed] [Google Scholar]
- 10.Zionts LE, Woodson JC, Manjra N, Zalavras C. Time of return of elbow motion after percutaneous pinning of pediatric supracondylar humerus fractures. Clin Ortop Relat Res. 2009;469(8):2007–2010. doi: 10.1007/s11999-009-0724-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spencer HT, Dorey FJ, Zionts LE, Wong MA, Moazzaz P, Silva M. Type II supracondylar fractures: can some be treated nonoperatively? J Pediatr Ortop. 2012;32(7):675–681. doi: 10.1097/BPO.0b013e318269c459. [DOI] [PubMed] [Google Scholar]
- 12.Onder E, Emel G, Ahmed A, Uygar D, Yalim A. Treatment of supracondylar fractures of the humerus in children through an anterior approach is a safe and effective method. Int Ortop. 2009;33(5):1371–1375. doi: 10.1007/s00264-008-0668-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reitman RD, Waters P, Millis M. Open reduction and internal fixation for supracondylar humerus fractures of the humerus in children. J Pediatr Ortop. 2001;21:157–161. [PubMed] [Google Scholar]
- 14.Bub FR, Schulz AP, Lill H, Voigt C. Supracondylar osteotomies of posttraumatic distal humeral deformities in young adults—technique and results. Open Ortop J. 2011;5:389–394. doi: 10.2174/1874325001105010389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bashyal RK, Schoenecker PL, Dobbs MB, Luhmann SJ, Gordon JE. Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop. 2009;29(7):704–708. doi: 10.1097/BPO.0b013e3181b768ac. [DOI] [PubMed] [Google Scholar]
- 16.Mehlman CT, Crawford AH, Mcmillion TL, Toy DR. Operative treatment of supracondylar fractures of the humerus in children: the Cincinnati experience. Acta Orthop Belq. 1996;62(1):41–50. [PubMed] [Google Scholar]
- 17.Liu RW, Roocroft J, Bastrom T, Yaszay B. Surgeon learning curve for pediatric supracondylar humerus fractures. J Pediatr Orthop. 2011;31(8):818–824. doi: 10.1097/BPO.0b013e3182306884. [DOI] [PubMed] [Google Scholar]
- 18.Salmela R, Koistinen V. Is the discharge register of general hospitals complete and reliable? Sairaala. 1987;49:480–482. [Google Scholar]
- 19.Keskimäki I, Aro S. Accurate of data on diagnosis, procedures and accidents in the Finnish Hospital Discharge Register. Int J Health Sci. 1991;2:15–21. [Google Scholar]
- 20.Mattila VM, Sillanpää P, Iivonen T, Parkkari J, Kannus P, Pihlajamäki H. Coverage and accuracy of diagnosis of cruciate ligament injury in the Finnish Hospital Discharge Register. Injury. 2008;39:1373–1376. doi: 10.1016/j.injury.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Statistics Finland (2012) Official Statistics of Finland. Statistics Finland, Helsinki
- 22.Mäyränpää MK, Mäkitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: a population-based study. J Bone Miner Res. 2010;25(12):2752–2759. doi: 10.1002/jbmr.155. [DOI] [PubMed] [Google Scholar]
- 23.Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res. 2004;19:1976–1981. doi: 10.1359/jbmr.040902. [DOI] [PubMed] [Google Scholar]
- 24.Hurson C, Browne K, Callender O, O’Donell T, O’Neill A, Moore DP, Fogarty EE, Dowling FE. Pediatric trampoline injuries. J Pediatr Orthop. 2007;27(7):729–732. doi: 10.1097/BPO.0b013e318155ab1. [DOI] [PubMed] [Google Scholar]
- 25.Villarin LA, Beck KE, Freid R. Emergency department evaluation and treatment of elbow and forearm injuries. Emerg Med Clin North Am. 1999;17:844–858. doi: 10.1016/S0733-8627(05)70100-0. [DOI] [PubMed] [Google Scholar]
- 26.Leksan I, Nicolic V, Mrela T, Lovric I, Kristek J, Selthofer R. Supracondylar fractures of the humerus in children caused by traffic. Coll Antropol. 2007;31(49):1009–1013. [PubMed] [Google Scholar]
- 27.Nysted M, Drogset JO. Trampoline injuries. Br J Sports Med. 2006;40(12):984–987. doi: 10.1136/bjsm.2006.029009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carson S, Woolridge DP, Colletti J, Kilgore K. Pediatric upper extremity injuries. Pediatr Clin North Am. 2006;53(1):41–67. doi: 10.1016/j.pcl.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 29.Fransworth CL, Silva PD, Mubarak SJ. Etiology of supracondylar humerus fractures. J Pediatr Orthop. 1998;18(1):38–42. [PubMed] [Google Scholar]
- 30.Park MJ, Baldwin K, Weiss-Laxer N, Christian JB, Mello MJ, Eberson C, Spiegel DA. Composite playground safety measure to correlate the rate of supracondylar humerus fractures with safety. An ecologic study. J Pediatr Orthop. 2010;30(2):101–105. doi: 10.1097/BPO.0b013e3181d07689. [DOI] [PubMed] [Google Scholar]
- 31.Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg. 2004;1:76–82. doi: 10.1177/230949900401200114. [DOI] [PubMed] [Google Scholar]
- 32.Valerio G, Gallè F, Mancusi C, Di Onofrio V, Colapietro M, Guida P, Liguori G. Pattern of fractures across pediatric age groups: analysis of individual and lifestyle factors. BMC Public Health. 2010;30(10):656. doi: 10.1186/1471-2458-10-656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Flynn JM, Jones KJ, Garner MR, Boebel J. Eleven years experience in the operative management of pediatric forearm fractures. J Pediatr Orthop. 2010;30(4):313–319. doi: 10.1097/BPO.0b013e3181d98f2c. [DOI] [PubMed] [Google Scholar]
- 34.Fletcher ND, Schiller JR, Garg S, Weller A, Larson AN, Kwon M, Browne R, et al. Increased severity of type III supracondylar humerus fractures in the preteen population. Pediatr Ortop. 2012;32(6):567–572. doi: 10.1097/BPO.0b013e31824b542d. [DOI] [PubMed] [Google Scholar]


