Abstract
Background
Hip dysplasia is prevalent in nonambulatory children with cerebral palsy, and may contribute to a decreased quality of life (Lonstein in J Pediatr Orthop 6:521–526, 1). Reconstructive procedures such as a femoral varus derotation osteotomy with or without a pelvic osteotomy are commonly employed with the goal of achieving and maintaining well reduced hips.
Purposes
The goals of this study are both to characterize the complications of reconstructive procedures and to identify risk factors that may contribute to these complications.
Patients and methods
A retrospective analysis was conducted among 61 nonambulatory children (93 hips) with cerebral palsy who underwent a femoral varus derotation osteotomy, with or without an open reduction and/or pelvic osteotomy, from 1992 through 2008 at our institution. The average patient age was 8.1 years (2.6–14.7) and the mean follow-up time was 5.9 years (2.1–15.9).
Results
The cumulative complication rate per patient including failures to cure was 47.6 %. Spica casting was found to be a risk factor for all complications (P = 0.023); whereas patients younger than 6 years old (P = 0.013) and children with a tracheostomy (P = 0.004) were found to be risk factors for resubluxation following surgery.
Conclusions
Although reported complication rates of hip reconstructive procedures performed upon children with cerebral palsy have varied considerably, those with more severe disease have experienced more complications. We report our tertiary referral center’s complication rate and our institutional experiences with risk factors for complications and failures to cure.
Level of evidence
IV, Retrospective case series.
Keywords: Cerebral palsy, Nonambulatory, Complications, Hip surgery
Introduction
Hip dysplasia is identified in up to 57 % [1] of nonambulatory patients with spastic quadriplegic cerebral palsy (CP). Reconstructive procedures are commonly performed to treat hip subluxation or dislocation, most commonly soft tissue releases and a femoral varus derotation osteotomy (VDRO) with or without an open reduction and/or pelvic osteotomy. The goal of these procedures is to retain located, mobile, and painless hips [2, 3].
While the reported complication rates for hip reconstructive surgery in patients with CP have varied considerably (0–81 %), [4–17] it is difficult if not impossible to compare studies since all but one [18] are based upon mixed populations of ambulators and nonambulators with no uniformity in defining a complication. Severity of disease, as indicated by limited ambulatory ability, the presence of a tracheostomy or gastrostomy, and Gross Motor Function Classification System (GMFCS), has been shown to be an important determinant for both the incidence of hip displacement and the risk of complications [16]. These previous studies have reported perioperative complications, but have not considered longer term problems such as resubluxation or redislocation as a complication. Our impression is that those patients with a dislocation, and those with subluxation in whom the natural history would result in dislocation, can be viewed as “failures to cure”, a long term complication.
With the goal of achieving better consistency in defining and categorizing complications, adaptations of the Clavien classification [19] have been reported, including the Clavien–Dindo [20]. The Clavien–Dindo scheme was adapted by Sink et al. [21] for use in orthopaedics (Table 1).
Table 1.
Modified Clavien-Dindo Classification according to Sink et al
| Modified Clavien–Dindo classification according to Sink et al. | ||
|---|---|---|
| I | Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, and radiological interventions. Allowed therapeutic regimens are: drugs as antiemetics, antipyretics, analgesics, diuretics, electrolytes, and physiotherapy. This grade also includes wound infections opened at the bedside. | |
| II | Requiring pharmacological treatment with drugs other than such allowed for grade I complications. Blood transfusions and total parenteral nutrition are also included. | |
| III | Requiring surgical, endoscopic or radiological intervention | IIIa: Intervention not under general anesthesia |
| IIIb: Intervention under general anesthesia | ||
| IV | Life-threatening complication (pulmonary embolus, admission to intensive care unit) or complication with the potential to result in permanent dysfunction/long term orthopaedic disability (permanent nerve injury, osteonecrosis) | |
| V | Death | |
For this study we define subluxation or dislocation (RMI >60 % at latest follow-up) as a Grade IIIb complication (Failure to cure)
The goals of this retrospective review are to (1) document the spectrum of complications following reconstructive hip procedures in nonambulatory patients with spastic quadriplegia (GMFCS 4,5) while these complications according to Sink’s modification of the Clavien–Dindo scheme, and (2) identify risk factors for these complications.
Methods
After obtaining approval from our Institutional Review Board, we performed a retrospective chart review of patients with spastic quadriplegic CP (GMFCS 4,5) treated with reconstructive hip surgery (soft tissue release and femoral varus derotational osteotomy with or without a pelvic osteotomy) for progressive subluxation or dislocation of the hip between 1/1/1992 and 12/31/2008, and a minimum follow-up of 2 years. Patients were identified through CPT codes (27258, 27259, 27165, 27146, 27147, 27151, 27156, and 27001).
The information collected for each patient is shown in Table 2, and the peri-operative, post-operative, and long term complications documented are shown in Table 3. With regard to the radiographic evaluation, the migration index of Reimer (RMI) was used to evaluate hip outcomes because of its reproducibility and its relationship to prognosis [22]. We defined a normal hip as having a RMI ≤30 %, mildly subluxated as 30 % < RMI < 60 %, severely subluxated as 60 % ≤ RMI < 90 %, and dislocated as RMI ≥90 %. Severely subluxated hips with an unfavorable prognosis based on migration index (>60 %) were considered failures to cure, since we would predict that all of these would become dislocated over the long term [23].
Table 2.
Variables collected for each VDRO performed
| Data collection | |
|---|---|
| Preoperative variables | Age |
| Gender | |
| CP Physiologic classification | |
| CP Geographic classification | |
| Ambulatory status | |
| Side of involvement | |
| Presence of tracheostomy | |
| Presence of gastrostomy tube | |
| Medical comorbidities (GERD, MR, epilepsy, heart defects, cardiac arrhythmias, asthma, CF, hematologic conditions) | |
| Operative data | Procedure performed & complications (see Table 3) |
| Postoperative data | Type and length of immobilization |
| Need for additional procedures | |
| Complications during admission and through latest followup (see Table 3) | |
| Radiographic data (preop, postop, followup) | Neck shaft angle (NSA) |
| Acetabular index (AI) | |
| Type of acetabulum (I, II) | |
| Migration index (RMI): (Normal = <30 %, mild subluxation = 30–60 %, Severe subluxation = 60–90 %, Dislocation = >90 %) | |
GERD gastroesophageal reflux disease, MR mental retardation, CF cystic fibrosis, ASA American Society of Anesthesiologists
Table 3.
Complications sought
| Complications following reconstructive hip surgery | |||
|---|---|---|---|
| Perioperative (intraoperative and during early postoperative period prior to discharge) | Infection | ||
| Nerve injury | |||
| Artery injury | |||
| Wound (dehiscence) | |||
| Pressure sore | |||
| Medical | Pulmonary | Atelectasis | |
| Pneumonia | |||
| Respiratory failure | |||
| Gastrointestinal (Ileus) | |||
| Deep vein thrombosis | |||
| Urinary tract infection | |||
| Postoperative (after discharge, within 1 month of procedure) | Infection | ||
| Fracture | Away from Implant | ||
| Adjacent to Implant | |||
| Wound (dehiscence) | |||
| Implant (loss of correction or fixation) | |||
| Cast related (sores, skin breakdown) | |||
| Neurologic deficit | |||
| Vascular | |||
| Long term complications (more than 1 month following discharge) | Heterotopic ossification | ||
| Avascular necrosis | |||
| Nonunion | |||
| Implant related | Fracture (adjacent to implant) | ||
| Prominent/painful | |||
| Loss of fixation | |||
| Failure to cure | Hip subluxation with poor prognosis (migration percentage >60%) | ||
| Hip dislocation (migration percentage >90%) | |||
Statistical methods
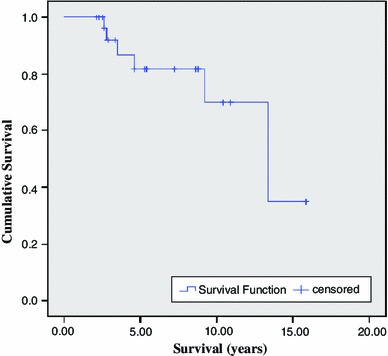
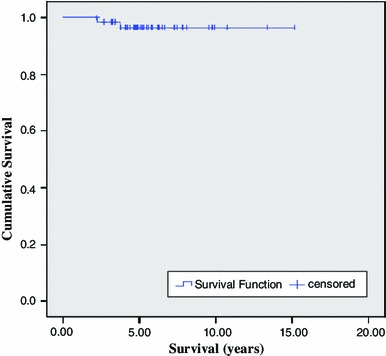
Comparison of complication rates was performed by using Chi square analysis in cases where variables were dichotomous and there were >5 events per cell. In cases where there were <5 events per cell, a Fisher’s exact test was used. Survival was plotted via Kaplan–Meier analysis as survival to redisplacement. A p value of <0.05 was considered to be statistically significant. Each hip was considered a separate point of analysis for the purposes of statistical analysis except where specified as number of patients. Statistics were calculated with the SPSS processor version 19.0. (SPSS Inc, Chicago, IL).
Results
Our initial search of CPT codes identified 156 surgical procedures (VDRO ± pelvic osteotomy) in 124 patients. Sixty-three patients were excluded because they were ambulatory (30), lost to follow-up (19), had inadequate follow-up (8), or were treated by a salvage procedure such as valgus osteotomy or proximal femoral resection (6). Our final study group therefore included 93 hips in 61 patients (Fig. 1).
Fig. 1.
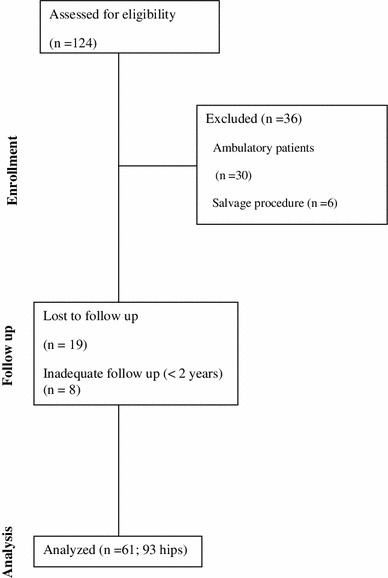
CONSORT diagram outlining the determination of the final study population
The average age at surgery was 8.1 years (range 2.6–14.7). 31 patients (51 %) were male and 30 (49 %) were female. Twenty-eight patients (45.9 %) had bilateral surgery and a pelvic osteotomy was performed on 38 hips (40 %). The average follow-up was 5.9 years (range 2.1–15.9). A summary of findings is provided in Appendix 1. The surgeries were performed at our institution by one of five attending surgeons.
Of the 61 patients (with a total of 93 hips) who underwent a unilateral or bilateral VRDO ± a Dega osteotomy, 29 patients had at least one complication in the period from surgery to final follow-up for a total complication rate of 47.6 % per patient and 32.3 % per VDRO performed. Excluding failures to cure (RMI ≥60 % at final follow-up) the total complication rate was 41 % per patient or 26.8 % per VDRO performed. Due to three patients having multiple complications each, there were 35 cumulative complications. To reduce redundancy, we report complication grades according to Sink et al’s complication grading scheme with percentages corresponding to complications per patient. There were a total of eight grade I complications (13 %) consisting of three decubitus ulcers, one case of heterotopic ossification (HO), two cases of severe pain, and two cases of atelectasis. Of the eleven grade II complications (18 %) there were eight femur fractures, one case of intraoperative malignant hyperthermia, one superficial wound infection, and one urinary tract infection. The only grade IIIa complication (2 %) was a case of respiratory failure that occurred intraoperatively. The 14 grade IIIb complications (23 %) included two resubluxations with a RMI ≥60 % but <90 %, six redislocations with a RMI >90 %, five symptomatic implants requiring removal, and one loss of implant fixation. The lone grade IV complication (2 %) was a case of avascular necrosis (AVN).
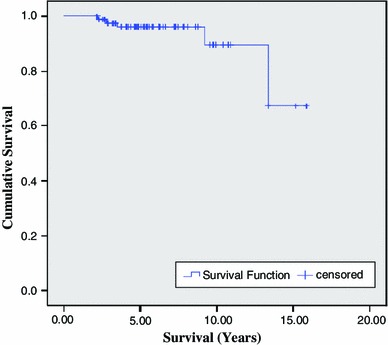
Of the pre-, peri-, and post-operative variables collected, only post-operative immobilization with a spica cast positively correlated with future complications (P = 0.023). Furthermore, surgeries performed on children under the age of 6 years of age and children with tracheostomies were the only factors that predisposed to failures to cure (P = 0.013 and P = 0.004, respectively). Survival plots for time until resubluxation for the total study population, for patients with and without a tracheostomy, and for patients below and above the age of six are displayed below as Figs. 2, 3, 4, 5 and 6, respectively.
Fig. 2.
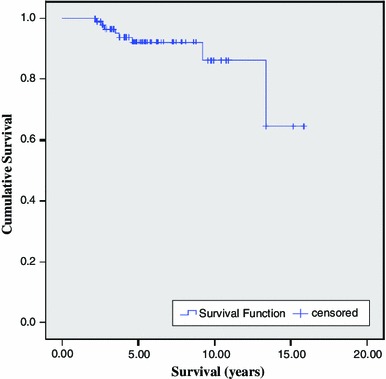
Survival function for composite population
Fig. 3.
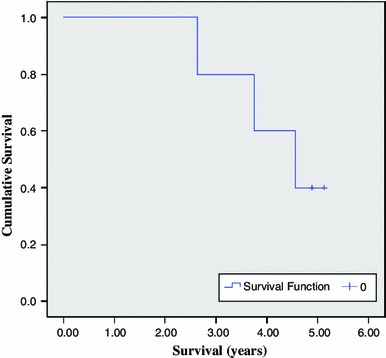
Survival function for patients with a tracheostomy
Fig. 4.
Survival function for patients without a tracheostomy
Fig. 5.
Survival function for patients younger than 6 years
Fig. 6.
Survival function for patients older than 6 years
Discussion
Neuromuscular hip dysplasia is common in nonambulatory patients with spastic quadriplegia, and reconstructive surgical procedures are often performed to address progressive subluxation or dislocation. Children with a greater severity of neurologic impairment have been shown to have a greater prevalence and severity of hip dysplasia [3] in addition to the highest complication rates [16].
Our first goal was to document the spectrum of complications following reconstructive surgery for neuromuscular hip dysplasia. The complication rate in this series (47.6 % per patient) falls nearly in the center of the range reported in the literature (Table 4) [4–17]. Our rate may also be elevated by the choice to include the category of “failure to cure” as a complication, rather than the more common practice to review the patient’s perioperative course for complications related to the procedure.
Table 4.
Summary of findings of related studies
| Author | Pt | Hips | Age (range) | Non-amb | Technique | Side unilateral/bilateral | Imm | FU (years) |
|---|---|---|---|---|---|---|---|---|
| Hoffer [6] | 20 | 25 | 8.9 (4.5–15) | 65 % | VDRO | 15 (75 %)/5 (25 %) | 2–8 weeks | 11.5 |
| Sturm [17] | 21 | 28 | 19 (3.3–31) | 75 % | Procedure not specified | 14 (67 %)/7 (33 %) | 6–12 weeks | NR |
| Brunner [4] | 47 | 64 | 10.3 (3.4–19.4) | 68 % | VDRO + OR | 30 (47 %)/17 (53 %) | 6 weeks | Clin (6.8) Rad (3) |
| Root [12] | 31 | 35 | 12 (4–23) | 71 % | VDRO + OR + PO (26 Salter, 5 Chiari, 3 Shelf, 1 Pem) | 27 (87 %)/4 (13 %) | 6 weeks | 7 |
| Gordon [5] | 44 | 52 | 8.8 (4.4–16.4) | 75 % | PO (Pemberton) ± VDRO (50) ± femur shortening (15) ± STR (37) ± OR (13) | 36 (82 %)/8 (18 %) | 6–10 weeks | 4 |
| Miller [23] | 51 | 70 | 9.9 (3.3–20) | 86 % | VDRO ± PO (59) ± OR (6) VDRO (11) | 42 (82 %)/9 (18 %) | None | 2.77 |
| Shea [21] | 15 | 19 | 7.75 (3.4–12.2) | 27 % | PO (Pemberton) ± STL (9) ± VDRO (13) ± OR (3) | 11 (73 %)/4 (17 %) | 6 weeks | 10.75 |
| Song [15] | 39 | 55 | 8.8 (3–15) | 79 % | VDRO (31) VDRO + PO (24) | 23 (59 %)/16 (41 %) | 6 weeks | 4.5 |
| Stasikelis [16] | 79 | 119 | 7.3 (2–17.8) | 84 % | VDRO + STR ± PO (25) | 39 (49 %)/40 (51 %) (9 staged, 31 at index) | NR | 2.4 |
| McNerney [9] | 75 | 104 | 8.1 (1.1–19.2) | 96 % | Index side: VDRO + STR ± OR (69) + PO Other side: VDRO (55) ± PO (2 Salter) | 20 (27 %)/55 (73 %) | 4–6 weeks | 6.9 |
| Noonan [11] | 65 | 79 | 7.6 (3.1–16.8) | 92 % | VDRO (30) VDRO + OR (49) | 51 (78 %)/14 (22 %) | NR | 5.2 |
| Sankar [13] | 12 | 14 | 10.6 | 75 % | VDRO + STR + Obt Neur + OR + PO | 10 (83 %)/2 (17 %) | 4–6 weeks | 16.7 |
| Al-Ghadir [18] | 39 | 52 | 8.1 + 3.6 years | 100 % | A: VDRO (16) B: VDRO + PO (36) | 26 (67 %)/13 (33 %) | NR | 4.4 |
| Luegmair [8] | 19 | 19 | 14.6 (12–17.9) | 68 % | Shelf (19) ± VDRO (5) ± STR (11) ± OR (1) | 19 (100 %)/0 | 6 weeks | 5.4 |
| Khalife [7] | 50 | 89 | 7.4 (4–15) | 46 % | VDRO ± PO (40 Dega, 17 Salter) ± OR (20) | 11 (22 %)/39 (78 %) | 3 weeks | 6 |
| Canavese [24] | 27 | 27 | 6.8 (2–15) | 93 % | VDRO + STR (22) VDRO + STR +PO (5) | 27 (100 %)/0 | NR | 2 |
| N = 16 | 634 | 851 | ||||||
| Current study | 61 | 93 | 8.1 (2.6–14.7) | 100 % | VDRO + STR ± PO | 34 (55 %)/28 (45 %) | 8.9 |
| Author | NSA (°) Preop/FU | AI (°) Preop/FU | RMI (%) Preop/FU | Complications | Compl Rate* (%) | Resubluxate/redislocate | Sink grades (% of complications) |
|---|---|---|---|---|---|---|---|
| Hoffer [6] | 155/125 | 28/27 | NR | AVN (1), Pin drainage (4), Excessive varus angulation (3) | 65 | 4/1 | I (8, 57 %) IIIb (5, 36 %) IV (1, 7 %) |
| Sturm [17] | NR | NR | NR | Fx (10) | 48 | NR | II (10, 100 %) |
| Brunner [4] | NR | NR | NR | Fx (3), Inf (1) | 47 | 15/3 | II (4, 18 %) IIIb (18, 82 %) |
| Root [12] | NR | 50/40 | 74/25 | AVN (10), Technical error pelvic osteotomy (1), Fx (3), HO (2), Trochanteric bursitis (1) | 68 | 4/0 | I (14, 67 %) II (3, 14 %) IIIb (4, 19 %) |
| Gordon [5] | NR | NR | NR | Delayed union (2), Pneum (2), Skin ulcer (2) | 14 | None | I (4, 67 %) II (2, 33 %) |
| Miller [23] | Nonamb: 150/104 Amb: 148/115 | NR | VDRO: 43/9 VDRO + PO: 74/5 | Pneum (1), HO (1), PTX (1), UTI (1), Inf (3), Fx (3), Skin breakdown (6), AVN (6) | 51 | 2/2 | I (13, 50 %) II (5, 19 %) IIIa (4, 15 %) IIIb (4, 15 %) |
| Shea [21] | NR | 28/11 | 55/12 | None | 0 | None | None |
| Song [15] | VDRO: 157/133 VDRO + PO: 159/132 | VDRO: 28/24 VDRO + PO: 29/18 | VDRO: 54/27 VDRO + PO: 63/11 | Fx (10), Implant failure (2), AVN (2), HO (1) | 67 | 9/2 | I (1, 4 %) II (10, 38 %) IIIb (13, 50 %) IV (2, 8 %) |
| Stasikelis [16] | NR | NR | NR | Death (3), Fx (25), Decub ulcers (5) | 42 | NR | I (5, 15 %) II (25, 76 %) V (3, 10 %) |
| McNerney [9] | NR | 26/11 | 66/14 | Technical error pelvic osteotomy (1), AVN (8), Wound infection (3), HO (7), Coxa vara (2), Death (1), Severe windblown hips (1) | 37 | 5/0 | I (11, 39 %) II (3, 11 %) IIIb(5, 18 %) IV (8, 29 %) V (14 %) |
| Noonan [11] | 153/131 | 32/25 | 82/28 | HO (1),Infection (2), Delayed unions (2), Pressure sore (6), Windswept hips (6), Abduction contracture (4), Fx (9), Incongruent/DJD (16), AVN (4) | 81 | 18(with RMI > 35 %)/3 | I (29, 40 %) II (17, 24 %) IIIb (22, 31 %) IV (4, 6 %) |
| Sankar [13] | NR | NR | 100/11 | Fx (8), Arthritis (1) | 75 | None | I (1, 11 %) II (8, 89 %) |
| Al-Ghadir [18] | A: 153/120 B: 159/121 | A: 24/11 B: 24/20 | A: 62/10 B: 63/18 | HO (1) | 13 | 4/0 | I (1, 20 %) IIIb (4, 80 %) |
| Luegmair [8] | NR | 51/35 | 64/10 | Hematoma (1), Stiffness (1) Graft resorption (1) Windblown hip (1) Arthritis (1) | 42 | 0/3 | I (5, 63 %) IIIb (3, 37 %) |
| Khalife [7] | 145/130 | VDRO: 30/30 VDRO + PO: 21/21 | 19/22 | HO (1), Fx (1), AVN (33) | 94 | 12/0 | I (1, 2 %) II (1, 2 %) IIIb (12, 26 %) IV (33, 70 %) |
| Canavese [24] | NR | I/L: 52/44 C/L: 51/43 | I/L: 48/18 C/L: 53/23 | NR | NR | 6/0 | IIIb (6, 100 %) |
| N = 16 | |||||||
| Current study | NR | NR | NR/27 | Decubitus ulcers (3), HO (1), Pain (2), Atelectasis (2), Fx (8), Malignant hyperthermia (1), Inf (1), UTI (1), Respiratory failure (1), Sympt implant (5), loss of fixation (1), AVN (1) | 47 | 2/6 | I (8, 23 %) II (11, 32 %) IIIa (1, 3 %) IIIb (14, 41 %) IV (1, 3 %) |
Age is reported in years
Pt patient, Imm length of immobilization in weeks, NSA femoral neck shaft angle, AI acetabular index (angle formed by line from lateral triradiate cartilage to acetabulum edge and Hilgenrieners line), FU follow up, VDRO varus derotation osteotomy, OR open reduction, PO pelvic osteotomy, NR not reported, AVN avascular necrosis, Fx fracture, HO heterotopic ossification, Pneum pneumothorax, DJD degenerative joint disease, Clin clinical follow up, Rad radiological follow up
* Complication rate is calculated [(total complications + failures to cure)/total patients]
Our review of the literature identified 16 studies reporting on 851 hips (3.3–20 years, 46–100 % nonambulators) followed for 4–16 years (Table 4). Most of these studies have reported complications during the perioperative period, have included a subset of ambulatory patients, and have varied in their definition of a complication. Among these studies there were 534 VDRO’s and 439 VDRO’s and a pelvic osteotomy with or without open reduction of the hip. Unilateral procedures were performed for 401 hips, and bilateral in 233. The most common complication was a femur fracture (9.4 % of hips), which mirrors our experience (8.6 % of hips). Fractures have been linked to immobilization in a spica cast, although in our study both the casted and non-casted groups totaled four fractures each. Other complications included pressure sores (3.3 % of cumulative patients), infection (2 %), AVN (10 %), HO (2.3 %), arthritis from an incongruent joint (2.7 %), implant failure (0.9 %), and symptomatic implants (0.8 %). Medical complications mostly involved the pulmonary system (respiratory failure, pneumothorax, pneumonia, or atelectasis).
In our study persistent instability was identified in 9 % of cases [2 % severe subluxation (RMI >60 %), 7 % redislocation]. Most studies have not considered “failure to cure” as a complication, namely redislocation or a RMI which would predict progressive subluxation leading to dislocation. In previous studies, which have included a subset of ambulatory patients, resubluxation was reported in 76 of 678 hips (11 %, range 2–14 %, 14/16 studies), while redislocation was observed in 20/678 hips (3 %, range 0–16 %, 14/16 studies). With regard to radiographic outcomes, the average RMI at follow-up was 17 % (12/16 studies), while the acetabular index was 21.2 (10/16 studies). The neck-shaft angle was only reported in 5/16 studies, and ranged from 104 to 133 degrees at follow-up.
According to Sink’s modification of the Clavien–Dindo scheme, 19 of our 35 complications were mild (Grade I or II). Of the remaining 16 complications, 8 were failures to cure and 5 involved symptomatic implants. We found that the single grade IV complication was an asymptomatic case of avascular necrosis. AVN was reported as a complication in 64 cases (7/16 studies), 33 of which were observed in a single series (Khalife). As AVN varies in severity, and is usually asymptomatic in the nonambulatory population with cerebral palsy, it remains questionable whether AVN should be classified as a grade IV unless long term symptoms are present or would be predicted. Noonan et al. reported a complication rate of 81 % in 65 patients (92 % nonambulatory), including 15 cases of “incongruent hips”, a radiologic finding for which we did not report.
As demonstrated in Table 5, incorporating these “failures to cure” into the literature review[4–17] raises the composite complication rate from 38 % up to 54 %, while at the same time skewing the complication grades towards the more severe. The proportion of grade IIIb complications alone jumps from 24 to 43 %. We believe that this reclassification helps to better estimate the true risks associated with this intervention.
Table 5.
Proportion of complications according to grade comparing the present series to the cumulative total from the studies represented in Table 4
| Classification according to Sink modification of Clavien-Dindo | ||
|---|---|---|
| Complication grade | Literature review | Present series (%) |
| I (deviation from normal postoperative course) | 14 % (44/324) | 23 |
| II (requiring pharmacologic treatment) | 29 % (94/324) | 31 |
| IIIa (intervention not under general anesthesia) | 0.01 % (2/324) | 3 |
| IIIb (intervention under general anesthesia) | 32 % (104/324) | 40 |
| IV (life threatening or long term orthopaedic dysfunction) | 24 % (79/324) | 3 |
| V (death) | 0.03 % (1/324) | 0 |
Our second goal was to identify the risk factors for these complications. Only spica cast immobilization (P = 0.023) was linked to all-cause complications, while patients younger than 6 years old (P = 0.013) and children with a tracheostomy (P = 0.004) were linked to failures to cure. Previous studies have shown that spica immobilization is associated with an increased risk of fractures [17]. Taking a closer look at the complications associated with spica casting in our current series, the distribution of specific complications is mostly equivalent among the spica and non-spica groups (four femur fractures in each) with the exception of the CD type I complications, of which, six of eight were related to the cast: three decubitus ulcers, one cases of heterotopic ossification, and two cases of severe pain with one definitely related to the cast requiring cast removal. With regard to the other risk factors, the presence of a tracheostomy indicates a greater severity of neurologic involvement, likely increasing the risk of recurrent instability. Furthermore, as progression of neuromuscular hip dysplasia is in part due to muscle imbalance within the setting of rapid growth, it seems plausible that younger patients would be at greater risk for recurrence of instability.
There are several limitations of our study, including the fact that patients were treated by a number of different surgeons over a 10 year period, and the data is retrospective. One important variable that likely relates to complications following surgical procedures in the neuromuscular population is nutritional status, which was not controlled in our study. Our current practice includes a preoperative nutritional consultation prior to reconstructive procedures for neuromuscular hip dysplasia, and while many patients are suitable candidates with oral supplementation, a more limited number have even required placement of a gastrostomy tube to achieve appropriate nutritional parameters for these procedures.
Conclusions
While complications are frequent in nonambulatory patients with CP following reconstructive hip surgery, the vast majority are minor and do not result in permanent problems. Immobilization in a spica cast should be avoided if possible due an increased risk for cast-related complications. Furthermore, younger patients with greater levels of neurologic impairment are at the greatest risk for a complication. We suggest that “failure to cure” be considered a long term complication. While adopting a uniform classification scheme for complications of surgical procedures is a worthy goal, our impression is that systems used in the general surgical literature must be adapted to characterize the nuances of orthopaedic complications.
Appendix
See Table 6.
Table 6.
Raw patient data
| Hip # | Pt # | Age at surgery (years) | Sex | Hip side | Trach/G-tube | Weight (kg) | ASA status | Procedure | Surgery total | EBL (mL) |
|---|---|---|---|---|---|---|---|---|---|---|
| 2 | 2 | 13.9 | M | R | N | 42.4 | 2 | 5 | 2:17 | 150 |
| 3 | 2 | 13.4 | M | L | N | 38.0 | 3 | 5 | 4:36 | 200 |
| 4 | 3 | 9 | F | R | N | 34.0 | 3 | 4 | 4:52 | 150 |
| 5 | 4 | 5.3 | M | R | Both | 17.2 | 3 | 3 | 3:30 | 100 |
| 6 | 4 | 5.3 | M | L | Both | 17.2 | 3 | 3 | 3:30 | 100 |
| 7 | 5 | 10.4 | F | R | N | 16.6 | 3 | 2 | 2:45 | 100 |
| 8 | 6 | 14.6 | M | R | N | 32.7 | 2 | 2 | 2:09 | 100 |
| 9 | 7 | 8.8 | M | R | G-tube | 16.0 | 3 | 4 | 3:09 | 100 |
| 12 | 9 | 10.4 | M | L | Both | 36.0 | 3 | 2 | 2:09 | 150 |
| 17 | 14 | 7.9 | M | R | Both | 25.7 | 3 | 5 | 4:21 | 250 |
| 18 | 14 | 7.9 | M | L | Both | 25.7 | 3 | 5 | 4:21 | 250 |
| 21 | 16 | 7.1 | M | L | Both | 11.9 | 3 | 5 | 4:38 | 260 |
| 22 | 17 | 5.6 | F | L | N | 19.0 | 2 | 2 | 2:30 | 225 |
| 23 | 18 | 13.3 | F | R | N | 26.0 | 3 | 3 | 2:57 | 150 |
| 24 | 18 | 13.3 | F | L | N | 26.0 | 3 | 3 | 2:57 | 150 |
| 26 | 20 | 4.6 | F | R | G-tube | 16.6 | 3 | 3 | 2:53 | 50 |
| 27 | 20 | 4.6 | F | L | G-tube | 16.6 | 3 | 3 | 2:53 | 50 |
| 29 | 22 | 7.7 | F | R | N | 23.6 | 3 | 5 | 5:27 | 475 |
| 30 | 22 | 7.7 | F | L | N | 23.6 | 3 | 5 | 5:27 | 475 |
| 33 | 24 | 5.9 | M | R | G-tube | 10.7 | 3 | 3 | 3:29 | 100 |
| 34 | 24 | 5.9 | M | L | G-tube | 10.7 | 3 | 3 | 3:29 | 100 |
| 36 | 26 | 10.3 | F | R | N | 20.1 | 3 | 5 | 2:57 | 100 |
| 37 | 26 | 7.1 | F | L | N | 15.3 | 3 | 5 | 2:55 | 150 |
| 41 | 29 | 13.9 | F | R | N | 37.6 | 3 | 3 | 4:10 | 600 |
| 42 | 29 | 13.9 | F | L | N | 37.6 | 3 | 3 | 4:10 | 600 |
| 43 | 30 | 4.9 | M | R | G-tube | 19.0 | 3 | 2 | 2:33 | 100 |
| 46 | 33 | 6.8 | M | R | N | 24.3 | 3 | 5 | 3:28 | 100 |
| 47 | 33 | 8 | M | L | N | 31.4 | 3 | 5 | 2:38 | 100 |
| 48 | 34 | 3.8 | F | R | G-tube | 15.2 | 3 | 3 | 4:09 | 250 |
| 49 | 34 | 3.8 | F | L | G-tube | 15.2 | 3 | 3 | 4:09 | 250 |
| 51 | 36 | 6.1 | F | R | G-tube | 26.2 | 3 | 3 | 2:33 | 50 |
| 52 | 36 | 6.1 | F | L | G-tube | 26.2 | 3 | 3 | 2:33 | 50 |
| 53 | 37 | 9.7 | M | R | N | 18.7 | 3 | 7 | 3:39 | 150 |
| 54 | 37 | 11.5 | M | L | N | 20.2 | 3 | 7 | 4:07 | 200 |
| 55 | 38 | 6.7 | M | L | G-tube | 24.0 | 3 | 4 | 2:18 | 100 |
| 56 | 39 | 10.8 | M | L | N | 33.5 | 3 | 2 | 2:38 | 100 |
| 57 | 40 | 4.4 | M | L | G-tube | 15.1 | 3 | 4 | 3:31 | 125 |
| 58 | 41 | 12.3 | M | R | N | 33.8 | 3 | 4 | 3:36 | 200 |
| 60 | 43 | 11 | F | R | N | 38.0 | 2 | 2 | 2:34 | 100 |
| 61 | 44 | 13.4 | M | L | N | 61.1 | 3 | 2 | 2:47 | 200 |
| 63 | 46 | 5.7 | M | R | N | 16.4 | 3 | 4 | 2:34 | 50 |
| 65 | 48 | 10.9 | M | L | N | 35.4 | 2 | 4 | 3:11 | 150 |
| 66 | 49 | 9.4 | F | L | G-tube | 23.6 | 3 | 3 | 2:55 | 100 |
| 67 | 49 | 9.4 | F | R | G-tube | 23.6 | 3 | 3 | 2:55 | 100 |
| 70 | 52 | 5 | F | R | G-tube | 13.0 | 2 | 3 | 2:28 | 100 |
| 71 | 52 | 7.1 | F | L | G-tube | 15.3 | 2 | 3 | 2:09 | 200 |
| 72 | 53 | 12.2 | F | R | N | 21.0 | 2 | 7 | 3:35 | 300 |
| 73 | 53 | 11.8 | F | L | N | 20.5 | 3 | 7 | 3:59 | 200 |
| 76 | 56 | 10.7 | F | R | N | 17.2 | 3 | 2 | 2:12 | 100 |
| 77 | 57 | 9.6 | F | R | N | 18.1 | 2 | 3 | 3:31 | 500 |
| 78 | 57 | 9.6 | F | L | N | 18.1 | 2 | 3 | 3:31 | 500 |
| 81 | 59 | 8.2 | M | L | N | 17.7 | 3 | 4 | 3:45 | 100 |
| 82 | 60 | 6.2 | F | R | G-tube | 11.0 | 3 | 7 | 4:52 | 150 |
| 83 | 60 | 6.2 | F | L | G-tube | 11.0 | 3 | 7 | 4:52 | 150 |
| 84 | 61 | 8.9 | F | R | G-tube | 16.0 | 2 | 4 | 2:51 | 150 |
| 85 | 62 | 7 | F | L | N | 22.5 | 3 | 4 | 3:33 | 150 |
| 88 | 65 | 8.6 | M | L | G-tube | 17.7 | 3 | 4 | 3:07 | 100 |
| 89 | 66 | 3.1 | F | R | Both | 13.6 | 3 | 3 | 2:54 | 200 |
| 90 | 66 | 3.1 | F | L | Both | 13.6 | 3 | 3 | 3:54 | 200 |
| 91 | 67 | 12.3 | F | R | N | 28.0 | 3 | 3 | 2:53 | n/a |
| 92 | 67 | 12.3 | F | L | N | 28.0 | 3 | 3 | 2:53 | n/a |
| 97 | 71 | 4.7 | F | L | G-tube | 16.1 | 3 | 4 | 3:46 | 100 |
| 100 | 74 | 3.5 | F | R | G-tube | 10.9 | 3 | 2 | 3:51 | 250 |
| 102 | 76 | 9.3 | M | R | N | 46.2 | 3 | 3 | 3:44 | 250 |
| 103 | 76 | 9.3 | M | L | N | 46.2 | 3 | 3 | 3:44 | 250 |
| 104 | 77 | 5.3 | M | R | G-tube | 15.0 | 3 | 3 | 3:02 | 100 |
| 105 | 77 | 5.3 | M | L | G-tube | 15.0 | 3 | 3 | 3:02 | 100 |
| 106 | 78 | 7 | M | R | N | 21.0 | 3 | 3 | 3:36 | 300 |
| 107 | 78 | 7 | M | L | N | 21.0 | 3 | 3 | 4:36 | 300 |
| 110 | 80 | 8.3 | F | L | N | 19.0 | 3 | 4 | 3:51 | 75 |
| 116 | 84 | 9.7 | M | R | N | 31.2 | 3 | 5 | 2:05 | 250 |
| 117 | 84 | 9.7 | M | L | N | 24.9 | 2 | 5 | 3:11 | 100 |
| 127 | 91 | 7.2 | F | R | G-tube | 18.0 | 3 | 3 | 3:48 | 100 |
| 128 | 91 | 7.2 | F | L | G-tube | 18.0 | 3 | 3 | 3:48 | 100 |
| 129 | 92 | 3.3 | F | R | G-tube | 16.3 | 2 | 3 | 2:47 | 150 |
| 130 | 92 | 3.3 | F | L | G-tube | 16.3 | 2 | 3 | 2:47 | 150 |
| 131 | 93 | 7.4 | M | R | G-tube | N/a | n/a | 5 | n/a | n/a |
| 132 | 93 | 7.4 | M | L | G-tube | n/a | n/a | 5 | n/a | n/a |
| 133 | 94 | 10.8 | M | R | N | 25.0 | 3 | 5 | 2:56 | 150 |
| 134 | 94 | 11.6 | M | L | N | 25.0 | 3 | 5 | 2:56 | 150 |
| 135 | 95 | 11.1 | M | R | N | 24.0 | 2 | 5 | 4:59 | 300 |
| 136 | 95 | 11.1 | M | L | N | 24.0 | 2 | 5 | 5:59 | 300 |
| 140 | 98 | 6.1 | M | L | N | 18.0 | 3 | 4 | 3:44 | 250 |
| 147 | 103 | 8 | F | L | N | 25.0 | 3 | 4 | 4:38 | 100 |
| 150 | 105 | 4.3 | M | R | N | 20.1 | 2 | 3 | 2:28 | Minimal |
| 151 | 105 | 4.3 | M | L | N | 20.1 | 2 | 3 | 2:28 | Minimal |
| 153 | 107 | M | R | G-tube | 14.0 | 2 | 3 | 1:35 | 125 | |
| 158 | 110 | 11.7 | F | L | N | 19.5 | 3 | 4 | 3:32 | 100 |
| 160 | 112 | 5 | F | R | G-tube | 11.2 | 2 | 3 | 4:13 | 30 |
| 161 | 112 | 5 | F | L | G-tube | 11.2 | 2 | 3 | 4:13 | 30 |
| 169 | 118 | 2.6 | M | R | N | 9.2 | 2 | 2 | 2:26 | 100 |
| 170 | 119 | 6.3 | F | L | N | 17.0 | 2 | 2 | 5:33 | 150 |
| Hip # | Transfusion | Periop complications | Post-op Hgb | Immob type | Hospital complications | Length of stay CHOP (days) | Postop complications | Complication treatment | Follow-up (years) | FFU RMI |
|---|---|---|---|---|---|---|---|---|---|---|
| 2 | Y | N | 7.8 | abd pillow | N | 8 | N | 5.03 | 0.05 | |
| 3 | Y | N | 9.9 | abd pillow | respiratory failure | 7 | Femur fracture | Spica cast | 5.54 | 0.05 |
| 4 | N | N | 6.7 | abd pillow | N | 6 | AVN femoral head & femur fracture | Spica cast | 6.46 | 0.05 |
| 5 | N | N | 8.3 | abd pillow | N | 3 | N | 4.56 | 0.95 | |
| 6 | N | N | 8.3 | abd pillow | N | 3 | N | 4.56 | 0.51 | |
| 7 | N | N | 10.8 | abd pillow | N | 4 | N | 8.09 | 0.05 | |
| 8 | N | N | 13 | abd pillow | N | 4 | N | 3.79 | 0.05 | |
| 9 | N | N | 10.2 | abd pillow | N | 3 | N | 4.66 | 0.26 | |
| 12 | N | N | 9.9 | abd pillow | N | 6 | N | 4.89 | 0.19 | |
| 17 | N | N | 12.4 | Spica cast | N | 3 | N | 3.73 | 1.00 | |
| 18 | N | N | 12.4 | Spica cast | N | 3 | N | 3.73 | 0.05 | |
| 21 | Y | N | 11.7 | Spica cast | N | 5 | N | 5.13 | 0.05 | |
| 22 | N | N | 9.6 | abd pillow | N | 4 | N | 3.33 | 0.59 | |
| 23 | N | N | 8.8 | Spica cast | N | 6 | Sacral decubitus ulcer | Wound care | 7.84 | 0.11 |
| 24 | N | N | 8.8 | Spica cast | N | 6 | Sacral decubitus ulcer | Wound care | 7.84 | 0.27 |
| 26 | N | N | 10.2 | abd pillow | N | 4 | N | 2.53 | 0.22 | |
| 27 | N | N | 10.2 | abd pillow | N | 4 | N | 2.53 | 0.24 | |
| 29 | Y | N | 9.7 | Spica cast | N | 5 | N | 6.21 | 0.43 | |
| 30 | Y | N | 9.7 | Spica cast | N | 5 | N | 6.21 | 0.05 | |
| 33 | Y | N | 9.6 | Spica cast | N | 6 | N | 2.81 | 0.05 | |
| 34 | Y | N | 9.6 | Spica cast | N | 6 | Femur fracture | Spica cast | 2.81 | 0.05 |
| 36 | N | N | 11 | abd pillow | N | 6 | Femur fracture | Splint | 4.11 | 0.27 |
| 37 | N | N | 13.9 | abd pillow | N | 3 | N | 7.30 | 0.05 | |
| 41 | N | N | 9 | Spica cast | N | 2 | N | 3.40 | 0.17 | |
| 42 | N | N | 9 | Spica cast | N | 2 | N | 3.40 | 0.22 | |
| 43 | N | N | 10.3 | abd pillow | N | 2 | Femur fracture | Spica cast | 2.89 | 0.35 |
| 46 | N | N | 9.5 | abd pillow | N | 4 | N | 4.35 | 0.30 | |
| 47 | N | N | 10.8 | abd pillow | N | 3 | N | 3.20 | 0.19 | |
| 48 | Y | N | 10.4 | Spica cast | N | 3 | HO | 2.29 | 0.58 | |
| 49 | Y | N | 10.4 | Spica cast | N | 3 | HO | 2.29 | 0.45 | |
| 51 | N | N | n/a | Spica cast | N | 2 | N | 8.63 | 0.52 | |
| 52 | N | N | n/a | n/a | N | 2 | N | 8.63 | 0.17 | |
| 53 | N | N | 8.56 | abd pillow | N | 4 | N | 4.11 | 0.55 | |
| 54 | Y | N | 7.8 | abd pillow | N | 6 | N | 2.23 | 0.78 | |
| 55 | Y | N | 12.9 | abd pillow | N | 4 | N | 3.18 | 0.34 | |
| 56 | N | N | n/a | abd pillow | N | 5 | N | 5.77 | 0.36 | |
| 57 | N | Hyperthermic intraoperatively | 8.8 | Spica cast | Malignant hyperthermia | 3 | N | 3.51 | 0.82 | |
| 58 | N | N | 11.6 | abd pillow | N | 3 | N | 2.70 | 0.28 | |
| 60 | N | N | 9.1 | abd pillow | N | 3 | Severe pain | Exam under anesthesia | 5.83 | 0.25 |
| 61 | N | N | 10.7 | abd pillow | N | 4 | N | 4.82 | 0.05 | |
| 63 | Y | N | 9.6 | abd pillow | Skin breakdown in groin area | 4 | N | 2.13 | 0.24 | |
| 65 | N | N | 9.9 | abd pillow | N | 4 | N | 5.44 | 0.15 | |
| 66 | Y | N | 6 | Spica cast | N | 6 | N | 4.90 | 0.05 | |
| 67 | Y | N | 6 | Spica cast | N | 6 | n/a | 4.90 | 0.26 | |
| 70 | N | N | 7.3 | abd pillow | N | 4 | N | 5.43 | 0.54 | |
| 71 | N | N | 8.4 | abd pillow | Seizure | 4 | N | 3.39 | 0.05 | |
| 72 | Y | N | n/a | Spica cast | Sacral decubitus ulcer | 8 | N | 4.88 | 0.05 | |
| 73 | N | N | 8.7 | Spica cast | N | 3 | N | 5.28 | 0.05 | |
| 76 | N | N | 9.8 | abd pillow | N | 2 | N | 5.16 | 0.05 | |
| 77 | Y | N | 6.5 | Spica cast | Severe pain requiring spica change | 5 | N | Spica cast change | 6.22 | 0.43 |
| 78 | Y | N | 6.5 | Spica cast | Severe pain requiring spica change | 5 | N | Spica cast change | 6.22 | 0.05 |
| 81 | N | N | 8.8 | abd pillow | N | 6 | N | 2.21 | 0.05 | |
| 82 | Y | N | n/a | abd pillow | N | 2 | N | 2.66 | 0.47 | |
| 83 | Y | N | n/a | abd pillow | N | 2 | N | 2.66 | 0.05 | |
| 84 | N | N | 9.1 | abd pillow | N | 4 | N | 4.58 | 0.38 | |
| 85 | N | N | 10.1 | abd pillow | N | 7 | Symptomatic implant | Hardware removal | 6.67 | 0.21 |
| 88 | N | N | 9.1 | abd pillow | N | 3 | N | 4.75 | 0.25 | |
| 89 | Y | N | 7.4 | abd pillow | N | 8 | Loss of implant fixation | Refixation | 2.63 | 0.86 |
| 90 | Y | N | 7.4 | abd pillow | N | 8 | N | 2.63 | 0.51 | |
| 91 | N | N | 9.8 | Spica cast | N | 3 | N | 4.83 | 0.08 | |
| 92 | N | N | 9.8 | Spica cast | N | 3 | N | 4.83 | 0.09 | |
| 97 | N | N | 10.2 | Spica cast | N | 3 | Infection | PICC line placement & antibiotics | 5.28 | 0.46 |
| 100 | N | N | n/a | Spica cast | Atalectasis | 3 | Femur fracture | Splint | 2.79 | 1.00 |
| 102 | N | N | 8.7 | abd pillow | N | 4 | N | 4.21 | 0.47 | |
| 103 | N | N | 8.7 | abd pillow | N | 4 | N | 4.21 | 0.05 | |
| 104 | N | N | 11.4 | Spica cast | N | 3 | Symptomatic implant | Hardware removal | 7.22 | 0.19 |
| 105 | N | N | 11.4 | Spica cast | N | 3 | Symptomatic implant | Hardware removal | 7.22 | 0.50 |
| 106 | N | N | 12.6 | Spica cast | N | 5 | None | 10.75 | 0.05 | |
| 107 | N | N | 12.6 | Spica cast | N | 5 | None | 10.75 | 0.35 | |
| 110 | N | N | 13 | Spica cast | N | 5 | Femur fracture | Spica cast | 7.49 | 0.18 |
| 116 | N | N | 9.1 | abd pillow | N | 4 | Symptomatic implant | Hardware removal | 7.81 | 0.05 |
| 117 | N | N | 11.1 | abd pillow | N | 4 | None | 9.56 | 0.05 | |
| 127 | N | N | 13.5 | Spica cast | Skin breakdown | 57 | None | 9.91 | 0.05 | |
| 128 | N | N | 13.5 | Spica cast | Skin breakdown | 57 | None | 9.91 | 0.05 | |
| 129 | N | N | 10.8 | Spica cast | Atalectasis | 3 | None | 8.78 | 0.05 | |
| 130 | N | N | 10.8 | Spica cast | Atalectasis | 3 | None | 8.78 | 0.05 | |
| 131 | N | N | n/a | abd pillow | N | n/a | None | 7.26 | 0.19 | |
| 132 | N | N | n/a | abd pillow | N | n/a | None | 7.26 | 0.19 | |
| 133 | N | N | 13.6 | abd pillow | N | 3 | None | 6.27 | 0.39 | |
| 134 | N | N | 13.6 | abd pillow | N | 3 | None | 5.44 | 0.05 | |
| 135 | N | N | 11.7 | Spica cast | UTI | 5 | None | Bactrim | 4.65 | 0.05 |
| 136 | N | N | 11.7 | Spica cast | UTI | 5 | None | Bactrim | 4.65 | 0.05 |
| 140 | N | N | 8.5 | abd pillow | N | 4 | None | 9.21 | 1.00 | |
| 147 | N | N | 14.1 | Spica cast | N | 7 | None | 9.77 | 0.05 | |
| 150 | N | N | 10.3 | Spica cast | N | 6 | None | 10.42 | 0.05 | |
| 151 | N | N | 10.3 | Spica cast | N | 6 | Femur fracture | Spica cast | 10.42 | 0.14 |
| 153 | Yes | N | 11.4 | Spica cast | N | 3 | None | 13.34 | 1.00 | |
| 158 | N | N | 14.2 | Spica cast | N | 3 | None | 10.89 | 0.24 | |
| 160 | N | N | 14.5 | Spica cast | N | 3 | None | 10.89 | 0.43 | |
| 161 | N | N | 14.5 | Spica cast | N | 3 | None | 15.86 | 0.43 | |
| 169 | N | N | n/a | Spica cast | N | 3 | None | 15.17 | 0.05 | |
| 170 | N | N | 11.1 | Spica cast | N | 3 | Symptomatic implant | Hardware removal | 5.86 | 0.16 |
Pt #, patient number, Trach/g-tube, presence of tracheostomy, gastrostomy tube, or both; Procedure: 2, unilateral VDRO; 3, bilateral VDRO; 4, unilateral VDRO and unilateral pelvic osteotomy; 5, bilateral VDRO and unilateral pelvic osteotomy; 7, bilateral VDRO and bilateral pelvic osteotomy
ASA American Society of Anesthesiologists, immob immobilization, abd pillow abduction pillow
References
- 1.Lonstein JE, Beck K, Lonstein JE, Beck K. Hip dislocation and subluxation in cerebral palsy. J Pediatr Orthop. 1986;6:521–526. doi: 10.1097/01241398-198609000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Flynn JM, Miller F, Flynn JM, Miller F. Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg. 2002;10:198–209. doi: 10.5435/00124635-200205000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Spiegel DA, Flynn JM, Spiegel DA, Flynn JM. Evaluation and treatment of hip dysplasia in cerebral palsy. Orthop Clin North Am. 2006;37:185–196. doi: 10.1016/j.ocl.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Brunner R, Baumann JU. Clinical benefit of reconstruction of dislocated or subluxated hip joints in patients with spastic cerebral palsy. J Pediatr Orthop. 1994;14:290–294. doi: 10.1097/01241398-199405000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Gordon JE, Capelli AM, Strecker WB, Delgado ED, Schoenecker PL. Pemberton pelvic osteotomy and varus rotational osteotomy in the treatment of acetabular dysplasia in patients who have static encephalopathy. J Bone Joint Surg Am. 1996;78:1863–1871. doi: 10.2106/00004623-199612000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Hoffer MM, Stein GA, Koffman M, Prietto M. Femoral varus-derotation osteotomy in spastic cerebral palsy. J Bone Joint Surg Am. 1985;67:1229–1235. [PubMed] [Google Scholar]
- 7.Khalife R, Ghanem I, El Hage S, Dagher F, Kharrat K. Risk of recurrent dislocation and avascular necrosis after proximal femoral varus osteotomy in children with cerebral palsy. J Pediatr Orthop B. 2010;19:32–37. doi: 10.1097/BPB.0b013e3283320c31. [DOI] [PubMed] [Google Scholar]
- 8.Luegmair M, Vuillerot C, Cunin V, Sailhan F, Berard J, Luegmair M, Vuillerot C, Cunin V, Sailhan F, Berard J. Slotted acetabular augmentation, alone or as part of a combined one-stage approach for treatment of hip dysplasia in adolescents with cerebral palsy: results and complications in 19 hips. J Pediatr Orthop. 2009;29:784–791. doi: 10.1097/BPO.0b013e3181b7699e. [DOI] [PubMed] [Google Scholar]
- 9.McNerney NP, Mubarak SJ, Wenger DR, McNerney NP, Mubarak SJ, Wenger DR. One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop. 2000;20:93–103. [PubMed] [Google Scholar]
- 10.Miller F, Girardi H, Lipton G, Ponzio R, Klaumann M, Dabney KW. Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop. 1997;17:592–602. doi: 10.1097/01241398-199709000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Noonan KJ, Walker TL, Kayes KJ, Feinberg J. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in cerebral palsy: statistical analysis in 73 hips. J Pediatr Orthop B. 2001;10:279–286. [PubMed] [Google Scholar]
- 12.Root L, Laplaza FJ, Brourman SN, Angel DH. The severely unstable hip in cerebral palsy. Treatment with open reduction, pelvic osteotomy, and femoral osteotomy with shortening. J Bone Joint Surg Am. 1995;77:703–712. doi: 10.2106/00004623-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Sankar WN, Spiegel DA, Gregg JR, Sennett BJ, Sankar WN, Spiegel DA, Gregg JR, Sennett BJ. Long-term follow-up after one-stage reconstruction of dislocated hips in patients with cerebral palsy. J Pediatr Orthop. 2006;26:1–7. doi: 10.1097/01.bpo.0000190842.77036.d0. [DOI] [PubMed] [Google Scholar]
- 14.Shea KG, Coleman SS, Carroll K, Stevens P, Van Boerum DH. Pemberton pericapsular osteotomy to treat a dysplastic hip in cerebral palsy. J Bone Joint Surg Am. 1997;79:1342–1351. doi: 10.2106/00004623-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Song HR, Carroll NC. Femoral varus derotation osteotomy with or without acetabuloplasty for unstable hips in cerebral palsy. J Pediatr Orthop. 1998;18:62–68. [PubMed] [Google Scholar]
- 16.Stasikelis PJ, Lee DD, Sullivan CM. Complications of osteotomies in severe cerebral palsy. J Pediatr Orthop. 1999;19:207–210. doi: 10.1097/01241398-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Sturm PF, Alman BA, Christie BL. Femur fractures in institutionalized patients after hip spica immobilization. J Pediatr Orthop. 1993;13:246–248. [PubMed] [Google Scholar]
- 18.Al-Ghadir M, Masquijo JJ, Guerra LA, Willis B. Combined femoral and pelvic osteotomies versus femoral osteotomy alone in the treatment of hip dysplasia in children with cerebral palsy. J Pediatr Orthop. 2009;29:779–783. doi: 10.1097/BPO.0b013e3181b76968. [DOI] [PubMed] [Google Scholar]
- 19.Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. 1992;111:518–526. [PubMed] [Google Scholar]
- 20.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sink EL, Beaule PE, Sucato D, Kim YJ, Millis MB, Dayton M, Trousdale RT, Sierra RJ, Zaltz I, Schoenecker P, Monreal A, Clohisy J (2011) Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg Am [DOI] [PubMed]
- 22.Scrutton D, Baird G, Smeeton N. Hip dysplasia in bilateral cerebral palsy: incidence and natural history in children aged 18 months to 5 years. Dev Med Child Neurol. 2001;43:586–600. doi: 10.1017/S0012162201001086. [DOI] [PubMed] [Google Scholar]
- 23.Miller F, Bagg MR. Age and migration percentage as risk factors for progression in spastic hip disease. Dev Med Child Neurol. 1995;37:449–455. doi: 10.1111/j.1469-8749.1995.tb12028.x. [DOI] [PubMed] [Google Scholar]
- 24.Canavese F, Emara K, Sembrano JN, Bialik V, Aiona MD, Sussman MD. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in GMFCS level III to V patients with unilateral hip involvement. Follow-up at skeletal maturity. J Pediatr Orthop. 2010;30:357–364. doi: 10.1097/BPO.0b013e3181d8fbc1. [DOI] [PubMed] [Google Scholar]


